![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back

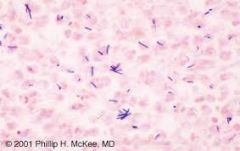
What is the aetiology of Anthrax? What species are affected? |
Acute usually fatal disease caused by bacterium Bacillus Anthracis. Mammals mainly cows and pigs in UK. Zoonotic!! |
|

Clinical signs of Anthrax? |
Any sudden or unexplained death!! If alive may get pyrexia, colic like pain, twitching, blood trickling from nostril, refusal to eat. |
|

How is anthrax transmitted? |
Spores that can survive for ages |
|

Signs of anthrax in pigs? |
More resistant than cattle. High temp, swollen, painful around throat, pyrexic then recover. If stressed relapse and die. |
|
Anthrax ddx in cattle? |
Electrocution- animals dead in a line. Hypomagnesaemia. Hypocalcaemia. Poisons. Clostridial disease. |
|
What must we not do with a anthrax suspicious case? |
Do not open it up as this will lead to sporulation!! If accidentally open the signs are consistent with septicaemia and pyrexia- congestion of the lungs and lymph nodes. Splenomegaly. |
|
|
What precautions are taken until diagnosis of anthrax? |
All sudden deaths reported to APHA! Carcase must not be opened or moved until an OV has investigated. Animals and humans kept away from the carcase pending results of investigation. Blood leaking from carcase must be treated with a DEFRA- approved disinfectant. Remove animals from an infected area if possible. In contact animals should be observed and isolated if they show symptoms. |
|
|
Can we treat anthrax? |
If got early enough crystalline penicillin. Vaccine available if on infected pasture! |
|
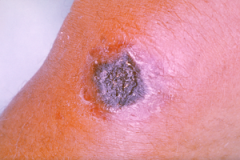
Signs of anthrax in people? |
Cutaneous form-ulcers and vesicle rings can respond to AB. Inhalation and intravenous forms are rapidly fatal. |
|

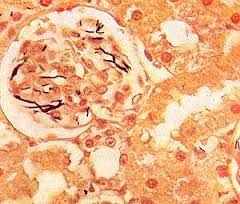
Aetiology of enzootic bovine leukosis? How is it transmitted? |
Caused by a retrovirus. Transmitted vertically mother to calf and horizontally. Causes leukemia and multiple tumors! |
|

What are clinical signs of EBL? |
Clinical signs are chronic ill health. Progressive loss of condition. Weakness. Anaemia. Anorexia. All these signs are associated with tumorous infiltration of the organs. |
|
|
How long has GB been free from bovine leukosis? |
Since July 1998 |
|
|
What age group of animal is usually effected by enzootic bovine leukosis? |
Ages 4-8 years not usually seen in animals under 2 years old. |
|
|
In all tumor in animals except for papillomas and haemangiomas what must we do? |
>2 years submitted to APHA for EBL testing. |
|
|
What surveillance schemes are in place for detection of EBL? |
Brucella milk and blood samples. All tumors. Sporadic lymphosarcoma. All imported animals. |
|
|
What treatment is there for EBL cattle? |
No treatment permitted animals must be slaughtered and those in contact |
|

What is issue with warble fly ? What is in place to stop if getting into the UK? |
Welfare issues. Extensive damage to the hide of deers, horses and cattle reducing the value of the hide. Compulsory treatment, now eradicated from GB. Notifiable in scotland. |
|

What causes warbles? Pathogenesis |
Hypoderma bovis and lineatum laying their eggs on the hair of cattle during the summer. The larvae hatch and migrate to the skin. They then move between muscle layer to the oesophagus and spinal canal. Dormant in late winter/early spring then migrate to the tissue under skin on back and mature for 30 days. Larvae exit through the skin, drop off host and pupate in the soil. Adult fly emerge in 36 days. |
|
|
Clinical signs of warbles? |
Laying eggs causes irritation and cows to run away causing injury and reduction in weight gain. Larval migration doesnt cause signs usually but may manifest as reductions in weight gain and milk production. Larvae reaching the skin cause painful swellings. Paralysis occassionally if pressure on spinal cord. Accidental or deliberate puncture of warbles can induce an allergic reaction. |
|
|
What is legislation regarding warbles? |
Imported animals except from NI to be treated for warbles within 24 hours of arrival. Warble fly order in scotland requires APHA notification, restrictions and treatments. |
|

What does brucellosis cause and what is the aetiological agent? |
Brucellosis causes abortion in cattle and undulant fever in humans. It is caused by Brucella abortus. |
|
|
Clinical signs of brucellosis? |
Second half of gestation abortions/ stillbirths. Epididymitis/orchitis in bulls. Infertility. Non pregnant animals may be assymptomatic. Subsequent pregnancies after a brucellosis abortion are usually normal. |
|
|
How is brucellosis transmitted? |
In infected abortion material- placenta. Uterine secretions. Semen- AI. Ingestion- milk. |
|
|
How long does brucella abortus survive in slurry/ urine etc? |
Slurry for 8 months. Faeces for 4 months. Urine for 4 days. Damp soil 27 days. |
|

How have we controlled brucellosis spread in GB? |
All abortions reported to APHA! Animals are sampled. Restrictions on individual pending a negative result. If infection confirmed herd restrictions, sampling, culling and compensation. All animals of non officially brucellosis free origin require testing before and after import and after first calving in GB! |
|

How do we test for brucellosis? |
Bulk milk tank sampling. Individual animal bloods for serology post import and first calving in GB. Abortion enquiries milk and vaginal swabs taken for serology and bacterial culture. |
|
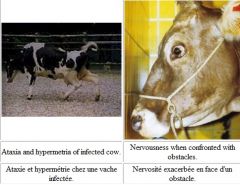
Clinical signs of BSE? Age usually seen in? |
Hypersensitivity, ataxia, changes in mental status, progresses to death. Usually seen in animals over 5 years old |
|
|
Aetiology and cause of BSE? |
Transmissable spongioform encephalopathy. Prions. |
|
How do we diagnose BSE? |
Histopath spongy brain |
|
|
How do we control BSE? |
Slaughter and compensation- identify her progeny and slaughter also. No sale on milk of suspects. Animal protein in feedstuffs banned. |
|
|
How is BSE tested now? |
Not in healthy animals for human consumption but BSE suspects, fallen cattle and emergency slaughters. |

