![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
469 Cards in this Set
- Front
- Back
|
What is normal motor nerve conduction studies?
|
generally upper extremity 50
lower ext. 42 |
|
|
what is a complex repetitive discharge?
|
it is spontaneous firing of multiple muscle fibers by ephaptic spread and one fiber acting as the "pacemaker"
|
|
|
What is a fibrillation?
|
a fibrillation is spontaneous firing of a single muscle fiber, always pathologic
|
|
|
What is a positive sharp?
|
a downward deflection, on a spectrum with fibrillations, firing of a group of muscle fibers, pathologic
|
|
|
What is a fasciculation
|
spontaneous firing of a motor unit, can be benign
|
|
|
What is the significance of complex repetitive discharges?
|
They denote chronic denervated muscle
|
|
|
What is Schwartz Jampel syndrome?
|
neuromuscular disease characterized by dysmorphic facies, hypertrichosis of eyelids, puckered faciesa, blepharophimosis, motor weakness, small muscle mass, osseous deformities pecturs
|
|
|
What is the significance of Schwartz Jampel syndrome in EMG?
|
in differential diagnosis for complex repetitive discharges
|
|
|
What is Becker myotonia?
|
It is one of the myotonia congenita, characterized by more muscle weakness than Thompson's and later onset in childhood
|
|
|
What is a fasciculation?
|
popcorn sound
spontaneous discharge of a single motor unit irregular, sig depends on company it keeps |
|
|
What are doublets and triplets?
|
they are essentially two or three fasciculations in succession, IRREGULAR
|
|
|
what is the sound associated with myokymia?
|
marching soldiers
|
|
|
What is myokymia?
|
single or multiple motor unit firings more regular, repetitive in succession
|
|
|
What is the significance of myokymia in evaluating a post-cancer plexopathy?
|
distinguish between radiation induced vs. tumor induced plexopathy, usually myokymia present in radiation induced
|
|
|
what are 3 causes of facial myokymia?
|
GBS, pontine tumor, MS
|
|
|
What is insertional activity?
|
brief bursts of muscle fiber firing when the needle is moved through muscle
|
|
|
What sounds is associated with endplate noise?
|
seasheel
|
|
|
What nosie is associated with endplate spike?
|
sputtering fat/frying pan
|
|
|
What noise is associated with fibrillation?
|
rain but crisp
|
|
|
What noise is associated with positive sharp waves?
|
rain and plop
|
|
|
what noise is associated with myotonia?
|
revving engine/dive bomber
|
|
|
what noise is associated with complex repetitive discharge?
|
machine/airplane in steady flight
|
|
|
what noise is associated with fasciculation
|
popcorn
|
|
|
what noise is associated with doublets/triplets?
|
horse trotting
|
|
|
what noise is associated with myokymia?
|
marching soldiers
|
|
|
what noise is associated with neuromyotonia?
|
pinging/racecars on racetrack
|
|
|
What is a motor unit?
|
a motor unit consists of the anterior horn cell, axon, nmj and all the muscle fibers it innervates
|
|
|
Why does a neurogenic motor unit potential have long duration and high amplitude?
|
Long duration occurs because of the sprouting of nerve fibers which take longer to transmit the impulse
|
|
|
Why does a neurogenic motor unit potential have high amplitude?
|
high amplitude occurs because of the sprouting and adoption of other muscle fibers?
|
|
|
Why does a neurogenic motor unit potential have polyphasic activity?
|
polyphasics occur because usally an impulse spreads in an orderly fashion from all the pre-ordained muscle fibers. This orderly fashion is lost with the sprouting and then leads to polyphasics
|
|
|
Why does a myogenic motor unit potential have small amplitude?
|
the small amplitude occurs because of the loss of muscle fibers (late finding and depends on the number of muscle fibers involved)
|
|
|
Why does a myogenic motor unit potential have short duration?
|
short duration is usually first and occurs because of the loss of muscle fibers that the nerve usually innervates
|
|
|
Can statin myopathy be irreversible?
|
Yes- usually reversible but if the muscle becomes necrotic and inflamed it can be irreversible
|
|
|
What are the characteristic symptoms of spinal stenosis?
|
The symptoms of spinal stenosis usually occurs upon walking when the spinal canal is compressed and then is relieved with sitting
|
|
|
What are some of the features of fascioscapulohumeral dystrophy?
|
Certain subtypes including:
facial sparing scapuloperoneal marked asymmetry |
|
|
What is the inheritance and chromosome affected in FSH?
|
Chromosome 4q35 deletion autosomal dominant
|
|
|
What other features can be associated with FSH?
|
MR, retinal telangiectasias
|
|
|
physiologically what is the etiology of end plate noise?
|
a single quanta of acetylcholine can be release spontaneously leading to miniature end plate potential without depolarization
|
|
|
What is the differential diagnosis associated with pseudomyotonia?
|
hyperkalemic periodic paralysis, glycogen storage disorders, myositis
|
|
|
What is the characteristic EMG finding on RNS in LEMS?
|
facilitation with rapid RNS (rapid is determined by the quantity of time it takes calcium to diffuse out of the cell which is 100-200ms) therefore rapid is more than 5 hertz
|
|
|
What is the characteristic EMG finding in GBS?
|
loss of F-wave and H-reflex early.. conduction block, temporal dispersion
|
|
|
What is the characteristic EMG finding in MG?
|
decrement with slow RNS at 3 HZ of >10%
|
|
|
What is SFEMG?
|
the needle records from 2 separate muscle fibers and jitter represents cross talk between the two muscles; sensitive but non specific
|
|
|
What is the normal duration, amplitude and phase of a normal voluntary motor unit potential?
|
duration 5-15 ms, amplitude 0.5 to 3 mv and phase is 2-4 phases
|
|
|
why do myogenic motor units start to develop polyphasics?
|
this occurs because although the nerve is healthy with time the changes in muscle fibers (replacement with fat and fibrous tissue) change the usual conductance of the system
|
|
|
Explain the safety factor and how it relates to myasthenia gravis.
|
The safety factor is that each depolarization of a muscle nerve causes a supra-therapeutic EPP. The amount of ACH released into the synpatic cleft and binding to the AchR is 3 times more than a normal person. In MG, the AchR are all bound and therefore there is a shorter safety factor and eventually the EPP will not fire with RNS
|
|
|
Explain the entire process of how a muscle fires
|
Voluntary muscle activity starts with energy in 3 mechanisms 1) creatine phosphokinase 2) glycogenolysis 3) Kreb's cycle. With voluntary movement ant horn cell will become depolarized travel down the axon, in the axon terminal voltage gated Ca channels open which cause ACh vesicles (pre-packaged) to be exoctyosed in to the synpatic cleft. The Ach vesicles bind to the AchR made up of 5 proteins (2 alpha, 1 beta, 1 delta, 1 gamma) the Ach vesicles bind to 2 alpha subunits which leads to a conformation change and allows multiple positive ions though (most numerous being Na). The entry of Na into the muscle fiber allows the ap to spread in the muscle fibers, through the transverse t-tubules, sarcoplasm to stimulate release of Ca from SR the release of Ca from SR then binds to troponing complex of actin (also made up of tropmyosin which covers the active site and F-actin & G-actin). The binding of calcium uncovers the active site. The myosin heads with their ATP-ase are cocked and already broken down. They connect to the active site, power stroke.
|
|
|
Explain the structure of a muscle fiber
|
Each muscle fiber is made up of multiple myofibrils suspended in sarcoplasm. The myofibrils are made up of actin and myosin attached to a Z band. EM the muscle fiber has an A band - all myosin and light I band- actin. The myosin is made up of a double helix with cocked heads with ATPase fixed. These interdigitate with actin.
|
|
|
What is a full pattern of muscle activity also called?
|
interference pattern
|
|
|
When do fibs and positive sharps usually appear in denervation?
|
7 to 14 days maximal at 3 weeks and can take up to 6 weeks
|
|
|
What do fibs and positive sharps usually indicate?
|
Usually neurogenic pattern however some muscular dystrophy, acid maltase, myositis and hyperkalemic periodic paralysis can have this
|
|
|
When is nerve conduction lost after nerve transection?
|
Distal nerve conduction is usually lost 3-5 days after nerve transection because of wallerian degeneration
|
|
|
Why do neurogenic unit potentials show a dropout of recruitment?
|
loss of motor unit
|
|
|
What is the H reflex and what does prolongation or absence of the H reflex indicate?
|
S1 afferent- efferent arc, loss or prolongation can indicate neuronopathies, sciatica, radiculopathies and early neuropathies
|
|
|
Which muscles are highest yield to test in MG for RNS?
|
proximal trapezius stimulate spinal accessory nerve
|
|
|
How can the EMG help prognosticate in GBS?
|
After 7-14 days you should be able to see decreased amplitude consistent with axonal loss. This can be a prognostic indicator of how long recovery would take
|
|
|
What are some muscles supplied by the C8 root?
|
1. 1st DI 2) ADQ 3) APB 4) ECU (radial) 7) FCU (ulnar) 8)EDC 9)EIP 10) EPB 11)FPL 12)PQ 13) FDP 14)Adductor pollicis
|
|
|
How would you distinguish between a C8 root and a plexus lesion
|
test the C8 paraspinous muscle, ulnar nerve would have decreased SNAP in plexus while normal in C8 radiculopathy unless multiple roots involved
|
|
|
What is the key muscle in differentiating a radial nerve palsy from a C7 radiculopathy?
|
flexor carpi radialis which is innervated by the median nerve
|
|
|
How could a suprascapular nerve lesion be differentiated from a C5-C6 radic?
|
test C5/6 cervical paraspinous, deltoid, biceps, brachioradialis, rhomboids
|
|
|
What does the suprascapular nerve innervate?
|
supraspinatus 1st 15 degrees of shoulder abduction; infraspinatus external rotation of the elbow
|
|
|
Differentiate a long thoracic nerve palsy and C5-C6 radic
|
spared biceps, deltoids in long thoracic n. and would involve serratus anterior
|
|
|
How can you differentiate a peroneal nerve palsy from a L4-L5 radic?
|
Inversion (tibialis posterior) is spared in a peroneal nerve palsy but involved in an L4-5 radic
|
|
|
What are the C5-C6 muscles?
|
1) biceps
2) supraspinatus 3) infraspinatus 4) rhomboids 5) deltoids |
|
|
How would you differentiate a femoral nerve palsy from an L3 radiculopathy?
|
check the hip adductors which would be affected in an L3 radic (obturator nerve) but not a femoral nerve palsy
|
|
|
What nerve supplies the hip adductors?
|
obturator nerve
|
|
|
How can you localize a femoral nerve lesion in the pelvis rather than inguinal region?
|
a femoral nerve lesion in the pelvis would involve the iliacus muscles while inguinal would not
|
|
|
What is the significance of having anti-striational antibodies?
|
in patients yonger than 50 years old with anti-striational antibodies 60% of them will have thymoma
|
|
|
What percentage of patients with MG have a presenting complaint of ocular symptoms?
|
50% have as presenting complaint, 85-90% have ocular involvement at some time in their disease
|
|
|
What is the action of the ryanodine receptor?
|
the ryanodine receptor acts to help the release of calcium in the sarcoplasmic reticulum
|
|
|
What percentage of so-called seronegative MG patients have anti-MUSK antibodies?
|
40-71%
|
|
|
What is the pattern of weakness in anti-MUSK MG?
|
usually involves bulbar and cranial muscles, respiratory is affected, limbs are spared
|
|
|
What percentage of MG patients get weaker when started on steroids?
|
10-20%
|
|
|
What happens in patients with LEMS who undergo lower frequency 3 HZ RNS?
|
decrement
|
|
|
What happens in patients with LEMS who undergo high frequency 12 HZ RNS?
|
facilitation
|
|
|
How does 3,4 diaminopyridine work as therapy in patients with LEMS?
|
3,4 diaminopyridine acts to block the potassium channels, which keeps the cells depolarized longer and allows longer Ca entry into cells leading to more quantal Ach Release
|
|
|
What is the action of infraspinatus?
|
external rotation and adduction of the arm
|
|
|
What is the action of supraspinatus?
|
abduction of the arm for the first 15 degrees
|
|
|
What nerve supplies coracobrachialis?
|
musculocutaneous nerve
|
|
|
Which trunk is injured by thoracic outlet syndrome?
|
lower trunk
|
|
|
What are the 3 adductor muscles?
|
adductor longus, brevis and magnus
|
|
|
what are the roots that supply iliopsoas muscle?
|
l2, l3, l4
|
|
|
What is the name of the muscle that extends the toes?
|
extensor digitorum longus
|
|
|
What is the name of the muscle that extends the big toe?
|
extensor hallucis longus
|
|
|
What muscles are innervated by the tibial nerve?
|
tibialis posterior-inversion, plantar flexion-gastrocnemius/soleus and big toe flexion/flexor hallucis longus
abductor hallucis longus |
|
|
What are the roots of the sciatic nerve that supplies knee flexion?
|
L5, S1, S2
|
|
|
What nerve is involved in foot eversion?
|
superficial peroneal nerve
|
|
|
What nerve innervates brachioradialis?
|
radial nerve
|
|
|
what does the anterior interosseous nerve supply?
|
flexor pollicus longus, flexor digitorum profundus, pronator quadratus
|
|
|
What trunk does Erb Duchenne palsy injur?
|
upper trunk during birth injury
|
|
|
Injury to what nerve in the brachial plexus would cause pure motor findings?
|
suprascapular nerve
|
|
|
What muscle flexes the four lateral toes of the foot?
|
flexor digitorum longus
|
|
|
What muscle flexes the large toe of the foot?
|
flexor hallucis longus
|
|
|
Which trunk is injured in Klumpke's palsy?
|
lower trunk
|
|
|
What innervates gastrocnemius and soleus?
|
Tibial Nerve
|
|
|
What is the root for innervation of Gastrocnemius/Soleus?
|
S1, S2
|
|
|
What is the definition of conduction block on EMG?
|
drop in the CMAP amp by >50% and drop in CMAP area by more than 50%
|
|
|
What physiologic features of myelinated axons assist with rapid saltatory conduction of nerve impulses?
|
The myelin itself acts as insulator to keep the impulse from leaving the axon. Additionally there is a concentration of Na channels at the node of ranvier
|
|
|
What is neurapraxia?
|
First degree nerve injury, normal distal nerve conduction wioth conduction block, recovery in 1-3 months
|
|
|
What axonotmesis?
|
focal damage to axon with secondary wallerian degneration
2nd degree: axon loss assoc. with intact endoneurial tubes, perineurium and epineurium 3rd degree: axons, schwann cell and endoneurium damaged (axonal regeneration misdirected, can lead to neuroma) 4th degree: perineurium, endoneurium and axons are disrupted, poor prognosis requiring surgery |
|
|
neurotmesis
|
severe type of nerve injury, complete nerve disruption, no chance for improvement
|
|
|
Why is a CMAP longer duration and and decreased amplitude at a site of proximal EMG stimulation compared to distal?
|
CMAP changes because of temporal dispersion and positive/negative phase overlap or cancellation (but CMAP less affected than SNAP) EMG cases p. 21
|
|
|
What is phase cancellation?
|
when you have differing morphology of 2 waveforms secondary to intrinsic differences in the nerve fiber this can lead to cancellation when the positive and negative phases overlap
|
|
|
What is temporal dispersion?
|
Each type of nerve fiber will transmit action potential at a specified velocity. The different velocities will summate and lead to "temporal dispersion" more noticeable over a longer length of nerve
|
|
|
What are some reasons that may lead to an erroneous diagnosis of conduction block on emg?
|
submaximal percutaneous stimulation (proximal sites, obesity, edema)
long peripheral nerves (tibial, tall pt.) anomalous innervation Martin-Gruber anastomosis |
|
|
Why is it important to perform EMG/NCS at least 10-11 days after injury?
|
Early in axonal injury, the pattern on EMG may appear like a conduction block (nl distal CMAPs) however with time to allow wallerian degernation to progress, then the EMG/NCS becomes more meaningful for prognosis.
|
|
|
When do signs of denervation such as MUAP decreased recruitment, fibrillations and positive sharps appear in denervation injury?
|
maximal at 3 weeks, up to 6 weeks can disappear after chronic
|
|
|
Why is the usual EMG pattern post RNS for MG U-shaped?
|
post-RNS decrement and then intermediate acetylcholine stores are mobilized
|
|
|
What happens in LEMS after 2-3 HZ RNS?
|
decrement in CMAP similar to MG
|
|
|
Name 5 muscles that may be useful to test for C5 myotome/radiculopathy?
|
1) Supraspinatus
2) Infraspinatus 3) Deltoid 4) Biceps 5) Brachioradialis 6) Rhomboid (sometimes involved, not always) |
|
|
Name 5 muscles that are usually involved in a C6 myotome/radiculopathy.
|
1) Biceps
2) Deltoid 3) Brachioradialis 4) Pronator Teres 5) Flexor Carpi Radialis Sometimes involved 1) Supraspinatus 2) infraspinatus 3) Extensor carpi radialis 4) Triceps |
|
|
Name 6 muscles that are usually involved in the C7 myotome/radiculopathy
|
1) Triceps
2) Flexor Carpi Radialis 3) Pronator Teres 4) Abductor Digiti Minimi 5) 1st Dorsal interossei 6) Flexor Digitorum Profundus |
|
|
If the 1st 2nd 3rd digits have hypesthesia including palm, what does that indicate for localization?
|
It has to be proximal to carpal tunnel syndrome because palmar innervation is before the median nerve enters the carpal tunnel
|
|
|
Name 6 muscles innervated by the C5 myotome
|
1. biceps
2. brachioradilis-radial n. 3. deltoid- axillary n. 4. supraspinatus- suprascapular 5. infraspinatus - suprascapular 6. rhomboid- dorsal scapular n. |
|
|
What muscle does dorsal scapular nerve innervate?
|
rhomboids
|
|
|
What 2 muscles does suprascapular nerve innervate?
|
supraspinatus and infraspinatus
|
|
|
What 2 muscles does the axillary nerve innervate?
|
deltoid and teres minor
|
|
|
What 3 muscles does the radial nerve innervate?
|
brachioradialis
supinator triceps |
|
|
What muscle does long thoracic nerve innervate?
|
serratus anterior
|
|
|
what muscle does subscapular nerve innervate
|
supraspinatus
infraspinatus |
|
|
What is meant by orthodromic recording?
|
orthodromic recording means that the action potential moves along the normal course of the sensory nerve
|
|
|
What is meant by antidromic recording?
|
antidromic recording means that the action potential is moving away from the sensory receptor such as in F or H wave studies
|
|
|
Name 2 anatomical lesions that may develop akinetic mutism clinically?
|
bilateral globus pallidus interna lesions (part of the anterior cingulate frontal subcortical circuit) and bilateral frontal lesions
|
|
|
What is the role of pedunculopontine neurons in Parkinson's disease?
|
They have shown depletion specifically of PPN in PD, plays a role in the motor circuit output from globus pallidus to the PPN
|
|
|
In the developing neural tube, what doese the basal plate become?
|
anterior horn gray matter
|
|
|
What does the alar plate of the developing neural tube become?
|
posterior horn gray matter
|
|
|
What does the anterior choroidal artery supply?
|
Discussion:
The anterior choroidal artery arises from the internal carotid artery distal to the origin of the posterior communicating artery. It has a long subarachnoid course, enters the inferior horn of the lateral ventricle through the choroidal fissure, and supplies the amygdala, hippocampal formation, globus pallidus, and the ventrolateral portion of the posterior limb and the entire retrolenticular portion of the internal capsule. Reference: Parent A. Carpenter's human neuroanatomy. |
|
|
What is the only muscle proximal to the knee innervated by the peroneal division of the sciatic nerve?
|
short head of biceps femoris
|
|
|
A lesion in the dominant inferior parietal lobule may cause what symptoms
|
Gerstmann's syndrome
1. acalculia 2. agraphia 3. right-left confusion 4. finger agnosia |
|
|
Where is the cell body of the sural nerve located?
|
dorsal root ganglion because it is a pure sensory nerve
|
|
|
Explain why conduction velocity and distal latency may be spared initially in axonal loss and affected later?
|
CV/DL generally are recorded from only the fastest fibers, with very severe axonal loss then even the fastest fibers become affected
|
|
|
What is meant by the term pseudo conduction blocK?
|
Early in nerve injury prior to wallerian degeneration NCS findings may look similar to conduction block with a drop in the amplitude
|
|
|
What is Erb's point?
|
Erb's point is the convergence of C5 and C6 lateral trunk, about 2 to 3 cm above the clavicle
|
|
|
When is the typical F wave in median and ulnar nerves?
|
32 seconds
|
|
|
When is the typical F wave in peroneal and tibial nerves?
|
56 seconds
|
|
|
What is the normal duration MUAP?
|
5 to 15 m sec
|
|
|
What is the sound of a long MUAP?
|
dull
|
|
|
What is the sound of a short MUAP?
|
crisp
|
|
|
Explain why MUAPs are large amplitude, long duration and polyphasic in neurogenic MUAPs?
|
Large amplitude b/c each AHC is feeding several fibers (same with duration) and polyphasic becuase the intrinsic synchrony of the motor unit changes with sprouting and reinnervation
|
|
|
What is the difference between activation and recruitment?
|
both ways to increase force in the body, activation allows you to increase firing rate and recruitment is self-explanatory
|
|
|
What is the normal recruitment ratio?
|
Recruitment ratio is firing rate relative to numer of units, normal should be 5:1
|
|
|
What is early recruitment?
|
The loss of motor fibers limits the generation of force. Then more units are recruited early. Myogenic
|
|
|
Which of the 2 LGMD tend to have distal onset?
|
dysferlinopathy and calveolinopathy
|
|
|
What is the pattern of inheritance of the LGMD type 1?
|
autosomal dominant
|
|
|
What is the pattern of inheritance of LGMD type 2 ?
|
autosomal recessive
|
|
|
Which LGMD may present wioth calf, tongue or other focal hypertrophy?
|
calpain, sarcoglycan, calveolin, fukutin related protein
|
|
|
Which LGMD should be considered with rigidspine and contracture?
|
calpain an lamin
|
|
|
Which LGMD tend to have scapular winging?
|
sarcoglycan and lamin
|
|
|
Which LGMD tend to have cardiac involvement?
|
lamin, sarcoglycan and fkrp
|
|
|
Which LGMD can have CPK elevated more than 10 times the upper limit normal?
|
dysferlinopathy
|
|
|
Which LGMD has inflammatory infiltrates?
|
dysferlinopathy
|
|
|
Which LGMD has rimmed vacuoles?
|
myotilinopathy
|
|
|
What is the most common LGMD?
|
calpainopathies
|
|
|
What is the sensitivity of WNV IgM in CSF on 4th day and then 7th day?
|
75% then 95%
|
|
|
What percentage of patients with MG present with ocular sx?
|
85%
|
|
|
What is the differential diagnosis for tongue fibrillations?
|
1) CN XII- base skull tumor, idiopathic hypoglossal neuropathy, brainstem lesion, radiation injury to cn xii
2) LMN d/o- ALS, SBMA, SMA, polio 3) organophosphate poisoning 4) anti-MUSK specific weakness |
|
|
What is the differential diagnosis for isolated head drop?
|
1) ALS
2) MG 3) Parkinson's dz or parkinsonism 4) isolated neck extensor myopathy 5) IBM or polymyositis 6) hypothyroidism |
|
|
What percentage of patients with MG present with oropharyngeal sx?
|
18%
|
|
|
What is the false positive rate of acetylcholine receptor antibodies
|
the ach-r binding antib false pos is rare, but if the blocking or modulating antibodies occur in isolation without binding antib it is difficult to interpret
|
|
|
What is the difference between seronegative MG in clinical and treatment?
|
seronegative MG 40% have anti-MUSK antiB; more refractory to conventional treatment, more severe disease (rarely pure ocular); respond to PE, MMF, prednisone, rituximab; thymectomy is questionable benefit, azathioprine/pyridostigmine little benefit
|
|
|
What is the difference in the treatment of ocular MG compared to classic MG?
|
ocular MG has a pretty good dramatic response to low doses of oral steroids
|
|
|
What is the clinical presentation of Kennedy's dissease?
|
limb girdle weakness
facial fasciculations, bulbar weakness spares respiratory muscles, hand tremor, sensory symptoms, feminization, testicular atrophy, gynecomastia, diabetes mellitus in 10-20% |
|
|
What is the characteristic tongue finding in Kennedy's disease?
|
longitudinal midline furrow
|
|
|
What is the usual age of onset for Hirayama disease or monomelic focal amyotrophy?
|
20 to 35
|
|
|
What are the characteristic findings on MRI for Hirayama disease?
|
anterior flexion may show anterior displacement of the posterior dural sac showing venous gorging
|
|
|
What is Hirayama disease?
|
focal amyotrophy of a single upper extremity in a young male progressive for a few years and then stabilizes, EMG may show bilateral involvement although only one side clinically involved
|
|
|
What is brachial amyotrophy diplegia?
|
variant of mnd restricted to the arms for 18 months without progression
|
|
|
In what subset of MG patients should repeat imaging be done if no thymoma in 3 to 6 months?
|
high risk, seropositive, generalized late onset MG patients
|
|
|
What are the most common paraneoplastic neurologic disorders?
|
MG and LEMS
|
|
|
What is the usual role of AchR modulating antibodies?
|
they decrease the presence of surface achR
|
|
|
What type of thymomas are usually associated with MG?
|
epithelial histology or type B
|
|
|
What percentage of MG patients have thymoma?
|
15%
|
|
|
What percentage of thymoma patients have MG?
|
40%
|
|
|
What are some differences between paraneoplastic MG and non-paraneoplastic MG?
|
paraneoplastic MG or MG with thymoma tends to be generalized, late onset and equal sex distribution
|
|
|
What percentage of thymomatous MG patients have positive Acetylcholine receptor antibodies?
|
100%
|
|
|
What percentage of patients with LEMS have small cell lung cancer?
|
50%
|
|
|
What occupational link has been shown to ALS in the US?
|
veterans are twice as likely to die from ALS as non-vets which is why they are now 100% SC
|
|
|
What occupational link has been shown for ALS in Italy?
|
Italian soccer players are 7 times more likely to get ALS
|
|
|
Which congenital myasthenic syndrome tends to have episodic respiratory insufficiency?
|
choline acetylcholinesterase deficiency
|
|
|
Which congenital myasthenic syndrome has been identified as the most common form of limb girdle myasthenia?
|
congenital MG DOK 7 deficiency
|
|
|
which congenital myasthenic syndrome is autosomal dominant and tends to present in late childhood or early adulthood?
|
congenital slow channel syndrome
|
|
|
Which congenital myasthenic syndrome is associated with an abnormal pupillary response to light?
|
endplate acetylcholinesterase deficiency
|
|
|
Which CMS is associated with prominent neck, wrist/digit extensor and intrinsic hand muscle weakness?
|
Slow channel congenital myasthenic syndromes
|
|
|
which cms actually worsen with administration of tensilon?
|
SCCMS, endplate Ach deficiency
|
|
|
What innervates extensor hallucis longus?
|
deep peroneal nerve
|
|
|
what is the root for EHL?
|
L4,L5, S1
|
|
|
What innervates Gluteus minimus?
|
superior gluteal nerve
|
|
|
What is the root for gluteus minimus?
|
L4,L5,S1, S2
|
|
|
What innervates EDB?
|
deep peroneal nerve
|
|
|
What roots are involved for EDB?
|
L5, S1
|
|
|
What nerve innervates flexor digitorum longus/brevis?
|
tibial, medial plantar
|
|
|
What roots innervate toe flexion?
|
L5, S1
|
|
|
What innervates trapezius?
|
CN XI
|
|
|
What root innervates trapezius?
|
C1,C2,C3
|
|
|
What nerve innervates the rhomboids?
|
dorsal scapular nerve
|
|
|
What muscle does the dorsal scapular nerve innervate?
|
rhomboids
|
|
|
What are the roots for the rhomboids?
|
C5
|
|
|
What innervates brachioradialis?
|
raidal nerve
|
|
|
What are the roots for brachioradialis?
|
C5, C6
|
|
|
What roots supply the deltoid?
|
C5, C6
|
|
|
What root supplies extensor carpi radialis?
|
C6, C7
|
|
|
What nerve supplies extensor carpi radialis?
|
radial nerve
|
|
|
What is the action of extensor pollicis brevis?
|
extends the thumb at the distal phalanx
|
|
|
What nerve supplies extensor pollicis brevis?
|
radial nerve
|
|
|
What nerve supplies flexor carpi radialis?
|
median nerve
|
|
|
What roots supply flexor carpi radialis?
|
C6,7
|
|
|
What roots supply latissimus dorsi?
|
C6,7,8
|
|
|
What nerve supplies latissimus dorsi?
|
thoracodorsal nerve
|
|
|
What nerve supplies extensor digitorum?
|
radial nerve
|
|
|
What root supplies triceps?
|
C7
|
|
|
What nerve innervates triceps
|
radial nerve
|
|
|
What root supplies flexor pollicis longus?
|
C8
|
|
|
What nerve innervates flexor pollicis longus?
|
median
|
|
|
What nerve supplies flexor carpi ulnaris?
|
ulnar
|
|
|
What root innervates flexor carpi ulnaris?
|
C8,T1
|
|
|
What nerve supplies abductor pollicis brevis?
|
median nerve
|
|
|
What root innervates APB?
|
C8, T1
|
|
|
What nerve supplies opponens pollicis?
|
median nerve
|
|
|
What 3 muscles make up the adductors?
|
adductor longus, brevis and magnus
|
|
|
What muscle everts the foot?
|
peroneus brevis
|
|
|
What innervates peroneus brevis/longus/tertius?
|
superficial peroneal nerve & deep peroneal nerve
|
|
|
What roots supply eversion?
|
L4,L5,S1
|
|
|
What nerve supplies tibialis posterior?
|
tibial nerve
|
|
|
What nerve supplies flexor hallucis longus?
|
tibial nerve
|
|
|
What root supplies flexor hallucis longus?
|
L5,S1,S2
|
|
|
What is the name of the branch of the median nerve that innervates abductor pollicis brevis?
|
recurrent thenar branch
|
|
|
What is origin of a fibrillation?
|
muscle fiber
|
|
|
What is the origin of myotonia?
|
muscle fiber
|
|
|
What is the origin of a positive wave?
|
muscle fiber
|
|
|
What is the origin of fasiculation?
|
muscle unit
|
|
|
What is the origin of myokymia?
|
muscle unit
|
|
|
What is the triad for Baltic myoclonus or Unvericcht Lundborgh?
|
progressive myoclonic epilepsy
ataxia cognitive decline |
|
|
What is the mode of inheritance and abnormality in Baltic myoclonus?
|
autosomal recessive and cystatin B gene
|
|
|
What is the usual age of onset of Baltic myoclonus?
|
9-13
|
|
|
What is the usual age of onset of Rolandic seizures?
|
9-13
|
|
|
What are the usual characteristics of Laforin body disease?
|
occipital seizures, ataxia, cognitive decline, progressive myoclonic epilepsy
|
|
|
What disease is associated with curvilinear fingerprint bodies on skin biopsy?
|
neuronal ceroid lipofuscinosis
|
|
|
What is the most common pediatric neurodegenerative disease?
|
neuronal ceroid lipofuscinosis
|
|
|
What is the usual clinical characteristics of neuronal ceroid lipofuscinosis?
|
blindness, optic atrophy, ataxia, progressive cognitive decline
|
|
What is the disease characterized by myotonia/stiffness similar to Isaac's or stiffperson syndrome, with dysmorphic features and osseous deformities & CRD on emg ?
|
Schwartz Jampel- puckered facies, blepharophimosis, hypertrichosis of eyebrows, osseous deformities
|
|
|
What nerve innervates 1st DI?
|
ulnar nerve
|
|
|
What is the roots for 1st DI?
|
C8, T1
|
|
|
What is the main aciton of 1st DI?
|
abducts the second finger radially from 3rd finger
|
|
|
What innervates APB?
|
median nerve
|
|
|
What roots are involved in APB?
|
C8, T!
|
|
|
What is the main action of APB?
|
abduction of thumb with the distal phalanx flexed
|
|
|
What innervates FCR?
|
median nerve
|
|
|
What roots FCR?
|
C6, C7 > C8
|
|
|
What innervates Pronator Teres?
|
Median Nerve
|
|
|
What roots are involved in PT?
|
C6, C7
|
|
|
What roots are involved with triceps?
|
C6, 7, 8
|
|
|
What roots are involved with deltoids?
|
C5, 6
|
|
|
What is the only L4 innervated muscle below knee?
|
tibialis anterior
|
|
|
What are the roots for tibialis anterior?
|
L4, L5
|
|
|
What is the action of tibialis anterior?
|
dorsiflexion and slight inversion
|
|
|
What are the roots and innervation of Gluteus Medius?
|
Superior gluteal nerve L5, S1
|
|
|
What are roots and innervation of Gluteux maximus?
|
Inferior gluteal nerve L5, S1, S2
|
|
|
What is innervation of Sciatic Nerve?
|
L4, L5, S1, S2
|
|
|
What is another name for the lateral popliteal nerve?
|
common peroneal
|
|
|
What is another name for the medial popliteal nerve?
|
tibial nerve
|
|
|
What 3 muscles are supplied by the superior gluteal nerve?
|
Tensor fascia lata
Gluteus Medius Gluteus Minimus |
|
|
What innervates the short head of biceps femoris?
|
common peroneal nerve
|
|
|
What innervates the long head of the biceps femoris?
|
Tibial Nerve
|
|
|
How can you distinguish a femoral neuropathy in pelvis versus in inguinal ligament?
|
Involvement of iliacus. The femoral nerve innervates iliacus 4-5 cm above the inguinal ligament
|
|
|
What is the anterior crural nerve?
|
AKA femoral nerve
|
|
|
What are the 4 heads of quadriceps femoris?
|
Rectus femoris
Vastus medialis Vastus intermedius Vastus lateralis |
|
|
What 2 muscle groups are involved in hip flexion?
|
femoral nerve iliopsoas
femoral nerve quadriceps (somewhat) |
|
|
What is CMAP nadir after wallerian degeneration?
|
4-5 days
|
|
|
What is SNAP nadir after wallerian degeneration?
|
8-11 days
|
|
|
What studies differentiate a femoral neuropathy from a lumbar plexopathy or radic?
|
SNAP, involvement of tibial innervated L4/5 like tibialis anterior, paraspinals
|
|
|
Differentiate femoral nerve vs. obturator nerve in take off from lumbar plexus?
|
Femoral nerve L2,3,4 dorsal
Obturator nerve L2,3,4 ventral |
|
|
Why do necrotizing myopathis/inflammatory myopathis and dystrophinopthaies have fibrilltaion potentials?
|
Segmental necrosis -essentially denervation because of physical separation from the NMJ
|
|
|
Where do fibs originate from?
|
abnormal firing from the muscle FIBER
|
|
|
Where do fascics originate from?
|
abnormal firing from the muscle UNIT
|
|
|
How can one distinguis fibs from end plate nose?
|
Fibs are IRREGULAR, end plate noise is more REGULAR
|
|
|
Why do we recommend waiting 10-11 days to perform EMG/NCs after injury?
|
time for wallerian degeneration to complete so that CMAP can be used as a marker for axonal loss.
Early on in axonal injury it can appear like conduction block |
|
|
When do fibrillations tend to develop after nerve injury?
|
1 week full at 3 weeks
|
|
|
What are roots of gluteus medius?
|
L5/S1 innervated by superior gluteal nerve
|
|
|
Why are EDX studies limited in root lesions?
|
L1, L2, L3- no SNAPs
SNAPs are hard to get esp sural or saphenous in elderly, obese, leg edema Paraspinals may not have fibs because they are proximal and may be reinnervated If dorsal root primarily involved then exam may be normal |
|
|
Why is it that not all muscles in a myotome are involved in a radic?
|
1) Partial motor axonal loss
2) variability in myotome distribution 3) reinnervation of proximal muscles |
|
|
What SNAP is associated with L4?
|
Saphenous
|
|
|
What SNAP is associated with L5?
|
superficial peroneal
|
|
|
What SNAP is associated with S1?
|
Sural
|
|
|
Why is it that paraspinal muscles are not useful for localization?
|
the innervation of the posterior rami can travel up several vertebral levels?
|
|
|
Where does the root for C7 exit?
|
Above C7 vertebral body like all cervical roots except C8?
|
|
|
What is notable regarding the spinal cord in relation to the vertebral segments?
|
The spinal cord is usually several vertebral levels above the corresponding vertebral body
|
|
|
Why is that a single disc herniation could lead to bilateral root involvement in the lower lumbar/sacral roots?
|
The cauda equina has a long distance in the spinal canal/because of its orientaiton
|
|
|
How quickly does a nerve grow back?
|
1 mm per day or 1 inch per month
|
|
|
What roots innervate flexor digitorum longus?
|
L5, S1
|
|
|
What roots innervated EDB?
|
L5, S1/ deep peroneal nerve
|
|
|
What roots innervate abductor hallucis?
|
S1, S2, tibial nerve
|
|
|
What is the sensory innervation of the web between the first and 2nd toes?
|
deep peroneal nerve
|
|
|
What is the only distal peroneal muscle with substantial S1 innervation?
|
peroneus
|
|
|
How is the superficial peroneal SNAP affected in deep peroneal neuropathy?
|
It would be spared which is why deep peroneal neuropathy is the differential for L5 radic
|
|
|
What is the significance of complex repetitive discharges related to timing?
|
Usually denotes a chronic lesion
|
|
|
what is the size principle?
|
with voluntary contraction, smallest units with lowest threshold fire first
|
|
|
What is polyphasia?
|
measure of synchrony of depolarization of muscle fibers in a unit
|
|
|
What is meant by activation?
|
Ability to increase the firing rate
|
|
|
What is meant by recruitment?
|
Ability to add units
|
|
|
What is the normal ratio of firing: units?
|
5:1, for every 5 HZ then you should see at least 1 unit, if firing at 30 HZ, you should see 6 units
|
|
|
What is the origin of myotonia?
|
muscle fiber
|
|
|
What is the origin of neuromyotonia?
|
motor neuron or axon
|
|
|
What is meant by early recruitment with myopathies?
|
Few fibers that are remaining can not generate same force as normal motor unit, they compensate by inappropriate firing of many motor units to generate a small amt of force
|
|
|
When could a myopathy actually exhibit decreased recruitment?
|
End stage myopathy may show decreased recruitment because of decrease in # motor units as well as fibers
|
|
|
What are 2 reasons that myopathies could have fibs & positive?
|
segmental necrosis separates muscle fiber from endplate, infarction of intramuscular nerve twigs
|
|
|
Why is it that you need both proximal latency and distal latency to calculate a conduction velocity?
|
The DL & PL include also the NMJ transmission time and muscle depolarization time which have to be accounted for.
|
|
|
What is meant by antidromic recording?
|
Stimulating toward the sensory receptor
|
|
|
What is meant by orthodromic recording?
|
Stimulating away from the sensory receptor
|
|
|
Why is it that temporal dispersion and phase cancellation do not effect the CMAP as much as SNAP?
|
because there is a smaller range of conduction velocity (less temporal dispersion and phase cancellation)
|
|
|
What are the rules of thumb for considering a lesion axonal rather than demyelinating?
|
velocity not less than 75%
distal latency not > 130% |
|
|
What is cockayne syndrome?
|
CNS+PNS disease also with hearing loss and visual loss (pigmentary retinopathy, usually death in 1st or 2nd decade)
|
|
|
Whatis cerebrotendinous xanthomatosis?
|
intractable diarrhea, presnile cataracts, tendinous xanthomas, neurologic abnormalities; occurs in 2nd to 3rd decade of life; peripheral neuropathy/FTD/XPS/Parkinson/ Seizures/Neuropathy
|
|
|
What is metachromatic leukodystrophy?
|
Arylsulfatase A deficiency, lysosomal sulfur degradation abnormality; leads to behavior change/memory loss/decreased work performance/seizures/loss of motor skills
|
|
|
What are the roots and innervation for Gluteus medius?
|
L5-S1
|
|
|
When does early reinnervation occur?
|
at 2-3 months
|
|
|
How quickly do nerves grow back?
|
1 mm/day or 1 inch per month
|
|
|
What is the sensory innrevation for the lateral leg?
|
lateral femoral cutaneous nerve
|
|
|
How can you distinguish insertional activity from EPP?
|
If more than 300 ms
|
|
|
What is the sensory innrevation of the deep peroneal nerve?
|
web between 1st and 2nd toes
|
|
|
What is the only distal peroneal muscle with substantial innervation?
|
EDB
|
|
|
How is the superficial peroneal SNAP affected in deep peroneal neuropathy?
|
It is not affected
|
|
|
What is the SNAP for L4 dermatome?
|
saphenous
|
|
|
What is the SNAP for L5 dermatome?
|
superficial peroneal
|
|
|
What is the SNAP for S1 dermatome?
|
sural
|
|
|
How is that a SNAP could be affected in an L5 radic?
|
superficial peroneal could be affected if the DRG is intraspinal
|
|
|
What are type 1 fibers?
|
Slow, fatigue resistant
|
|
|
What are type IIA and type IIB?
|
both fast
A fatigue resistant B fatiguable |
|
|
Why do we recommend waiting 10-11 days after injury to perform EMG/NCS?
|
Wallerian degeneration to complete. Early on even axonal lesions may look like conduction block
|
|
|
What is the upper range of side to side CMAP variability?
|
30%
|
|
|
What are the myotomes for flexor digitorum longus?
|
L5, S1 tibial nerve
|
|
|
What are the myotomes for Peroneus longus & brevis?
|
tibial nerve L5, S1
|
|
|
What are the myotomes for posterior tibialis?
|
tibial nerve L5, S1
|
|
|
What muscle can help distinguish femoral nerve lesion @ pelvis vs. inguinal ligament?
|
Iliacus is innervated by femoral nerve prior to it passing underneath the inguinal ligament
|
|
|
What are the 4 heads ofthe quadriceps femoris?
|
rectus femoris, vastus lateralis, vastus intermedius and vastus medialis
|
|
|
What are the 3 terminal sensory branches of femoral nerve?
|
medial and intermediate cutanous nerves of thigh, saphenous nerve
|
|
|
What is the anterior crural nerve?
|
another name for femoral nerve
|
|
|
How long does it take for wallerian degeneration to reach its nadir for motor nerves?
|
4 to 5 days
|
|
|
How long for wallerian degen to reach it nadir for sensory nerves?
|
10-11 days
|
|
|
What 2 muscles are involved in hip flexion?
|
Both iliopsoas and quadriceps femoris assist in hip flexion p.114
|
|
|
What studies differentiate a femoral neuropathy from plexopathy or radic?
|
SNAP spared in radic, paraspinal fibs in radic
Involvement of obturator nerve suggests plexopathy or radic more than femoral neuropathy; can also test tibialis anterior |
|
|
What is anterior tarsal tunnel syndrome?
|
Entrapment of the deep peroneal nerve under extensor retinaculum
|
|
|
What is medial tarsal tunnel syndrome?
|
entrapment of hte tibial nerve under flexor retinaculum
|
|
|
What is TTS?
|
bilateral TTS only 10-20%
burning foot pain, worse with prolonged standing or walking paresthesias in sole Involvement in 1 or all of the terminal tibial branches worse with eversion |
|
|
What is diabetic amyotrophy?
|
Lumbar polyradiculoplexopathy
|
|
|
What is the time course, epidemiology?
|
subacute onset; Pain improves first, then weakness may take longer; etiology is thought to be ischemia
|
|
|
what is epidemiology of diabetic amyotrophy?
|
older adults > 50, type 2 diabetics, may be first manifestation of DM
|
|
|
What is the relationship of glycemic control to this disorder?
|
varied, some 1st manifestation some are brittle; Glycemic control does not improve rate of recovy
|
|
|
Does weight loss occur in diabetic amyotrophy?
|
Patients can lose up to 15-20 pounds
|
|
|
How often do patients with diabetic amyotrophy also have distal symmetric polyneuropathy?
|
In up to 2/3 of patients both coexist
|
|
|
What is prognosis of diabetic amyotrophy?
|
Good prognosis, improve as early as a few weeks and maximal at 12 months. Weakness starts to improve in 3-4 months but may take 3 years, recurrence occurs in 20%; usually spontaneous recovery
|
|
|
What is innervation of sciatic nerve?
|
l4,5, S1, S2
|
|
|
What is lateral popliteal nerve also known as?
|
common peroneal
|
|
|
What is medial popliteal nerve known as?
|
tibial nerve
|
|
|
What 3 muscles does superior gluteal nerve innervate?
|
tensor fascia lata, gluteus medius and minimus
|
|
|
Where does superior gluteal nerve com off?
|
Before piriformis
|
|
|
What is an accessory deep peroneal nerve?
|
An accessory deep peroneal nerve occurs when this nerve branches off superficial peroneal nerve gives rise to EDB and peroneus longus/brevis and passes behind lateral malleolus
|
|
|
How would an accessory deep peroneal nerve appear on EDX?
|
Stimulating proximally gives a higher CMAP than distally (b/c the nerve is not at the ankle), then stimulate at lateral malleolus and find the nerve running there.. add the 2 CMAPs together
|
|
|
What 3 places can you localize peroneal to?
|
fibular head, proximal thigh and deep branch
|
|
|
What is sensory innervation of superficial peroneal nerve?
|
skin of the lower 2/3 of the lateral foot and dorsum
|
|
|
What structures make up Guyon canal?
|
Pisiform bone, Pisiform hamate hiatusTransverse carpal ligamenConnective tissue
|
|
|
How would you differentiate between
An ulnar neuropathy at the elbow vs. wrist? |
elbow lesion would involve dorsal cutaneous nerve and sensory loss to 4th and 5th digits
|
|
|
How would you distinguish between a proximal/distal GC and PHH?
|
Proximal gc- all ulnar intransics Motor + sensory loss (occ sensory loss only)
Distal gc- all ulnar intrinsics no Sensory loss, deep palmar cutaneous Branch spared PHH- all ulnar intrinsics x adq/adm |
|
|
What intrinsic muscles are supplied by ulnar nerve?
|
4 dorsal interossei
3 palmar interossei Adductor pollicis ADQ/ADM FPM |
|
|
What 2 muscles above wrist are supplied by ulnar nerve?
|
FCU
FDP |
|
|
If trying to localize a distal ulnar neropathy with normal ADQ what other muscle can you try?
|
Try recording 1st DI because this most often involved in distal neuropathy
|
|
|
What would an ulnar lesion sparing ADQ, involving 1st DI and sparing sensory SNAP suggest?
|
PHH abNl
|
|
|
What is the most common cervical radiculopathy?
|
c7 in 68%, C8 in 28% C5 in 2%
|
|
|
What is the SNAP for C5?
|
no technically feasible SNAP
|
|
|
What is the SNAP for C6?
|
lateral antebrachail cutaneous nerve
median snap from index/thumb |
|
|
What is SNAP for C7?
|
median snap ind/middle finger
|
|
|
What is SNAP for C8?
|
medial antebrachial cutaneous nerve
|
|
|
What is SNAP for T1 ?
|
medial brachial cutaneous nerve
|
|
|
Why is it that SNAP is usally normal in radic?
|
impinges on preganglionic fibers
|
|
|
What are radial nerve/C8 muscles?
|
extensor pollicis longus, extesor pollicis brevis
|
|

The hand on the viewer's left is abnormal. Explain the sign and abnormality.
|

Froment's sign
ulnar nerve palsy caused by weakness of adductor pollicis brevis, therefore, in attempting to adduct the thumb, the patient will activate FPL and make an "ok sign" |
|
|
Where does lateral antebrachial cutaneous nerve bran off?
|
Upper trunk/lateral cord
|
|
|
What is Pincer sign or abnormal ok sign?
|
A sign of anterior interiorosseous nerve weakness/dysfunction flexor pollicis longus weakness
|
|
|
How does exacerbation with valsava (cough/sneeze) help localize arm symtoms?
|
worsening with arm symptoms can suggest cervical radic
|
|
|
Where is weakness most common in neuralgic amyotrophy?
|
upper trunk
|
|
|
How often does recurrence occur in neuralgic amyotrophy?
|
Rare only 3-10%
|
|
|
Why is it that median snap is spared in a lower plexus lesion?
|
the sensory innervation is primarily through the upper and medial while the motor is in the lower plexus
|
|
|
What is SNAP for C6?
|
lateral antebrachial cutaneous nerve, median SNAP recording from thumb
|
|
|
What is SNAP for C7?
|
median SNAP recording from middle finger, index finger
|
|
|
What is SNAP for C8?
|
ulnar recording from ADM
|
|
|
What is SNAP for T1?
|
medial antebrachial cutaneous nerve in forearm
|
|
|
Why is it that median snap is spared in a lower plexus lesion?
|
the sensory innervation is primarily through the upper and medial while the motor is in the lower plexus
|
|
|
What is SNAP for C6?
|
lateral antebrachial cutaneous nerve, median SNAP recording from thumb
|
|
|
What is SNAP for C7?
|
median SNAP recording from middle finger, index finger
|
|
|
What is SNAP for C8?
|
ulnar recording from ADM
|
|
|
What is SNAP for T1?
|
medial antebrachial cutaneous nerve in forearm
|
|
|
Why is it that median snap is spared in a lower plexus lesion?
|
the sensory innervation is primarily through the upper and medial while the motor is in the lower plexus
|
|
|
What is SNAP for C6?
|
lateral antebrachial cutaneous nerve, median SNAP recording from thumb
|
|
|
What is SNAP for C7?
|
median SNAP recording from middle finger, index finger
|
|
|
What is SNAP for C8?
|
ulnar recording from ADM
|
|
|
Why is it that median snap is spared in a lower plexus lesion?
|
the sensory innervation is primarily through the upper and medial while the motor is in the lower plexus
|
|
|
What is SNAP for T1?
|
medial antebrachial cutaneous nerve in forearm
|
|
|
What is SNAP for C6?
|
lateral antebrachial cutaneous nerve, median SNAP recording from thumb
|
|
|
What is SNAP for C7?
|
median SNAP recording from middle finger, index finger
|
|
|
What is SNAP for C8?
|
ulnar recording from ADM
|
|
|
What is SNAP for T1?
|
medial antebrachial cutaneous nerve in forearm
|
|
|
Why is it that median CMAPS are spared in upper trunk lesion?
|
the motor fibers are predominantly through upper trunk
|
|
|
What findings may be seen on MRI in neuralgic amyotrophy?
|
nothing on brachial plexus except fatty changes c/w denervation in affected muscles
|
|
|
What distinguishes between sporadic and hereditary neuralgic amyotrophy?
|
hereditary neuralgic amyotrophy often recurs, can involve lower cranial nerves, can have findings such as dysmorphism (cleft palate, canthal folds, syndactyly)
|
|
|
What mutation causes hereditary neuralgic amyotrophy?
|
chromosome 17, septin 9
|
|
|
How could one distinguish HNPP from hereditary neuralgic amyotrophy?
|
HNPP usually painless
|
|
|
How much acetylcholine is in each synaptic vesicle?
|
5000 to 10000 molecules of Ach
|
|
|
After 3 years of pure ocular weakness what is the risk of developing generalized MG?
|
only 3-10 %
|
|
|
What are some features that distinguish LEMS from MG?
|
LEMS/botulism has low/borderline CMAPs, facilitates post-exercise; clinically LEMS areflexia, sensory features, dysautonomia, less/subtle involvement ocular muscles
|
|
|
Where does the greatest decrement occur in amplitude in RNS?
|
between 1st and 2nd stimulation
|
|
|
Where does the amplitude level off in RNS?
|
After 5th stimulation
|
|
|
What would an asymmetric polyneuropathy with predilection for cool skin areas such as nipples, buttocks, fingers with ulcers suggest?
|
leprous neuropathy
|
|
|
what percentage of patients with neuropathy are unknown despite extensive investigation?
|
25%
|
|
|
What 3 neuropathies may be proximal?
|
GBS, CIDP porphyria
|
|
|
What are 4 etiologies of large fibers sensory neuropathy?
|
B6 intoxication, E, paraneoplastic, Sjogrens
|
|
|
What does POEMS stand for and what type of neuropathy?
|
chronic demyelinating
Polyneuropathy Organomegaly Endocrinopathy Monoclonal gammopathy Skin Changes |
|
|
What type of neuropathy is associated with IgM spike?
|
sensory ataxia, older adults, less responsive to treatment
|
|
|
If considered a pure axonal neuropathy what is the lower limit of normal for conduction velocity?
|
70%
|
|
|
Name 10 causes of hereditary demyelinating peripheral neuropathy.
|
1. CMT 1 2. CMT 3 3. congenital hypomyelinating 4.krabbe's 5. metachromatic leukodystrophy 6. cockayne 7. adrenoleukodystrophy 8. refsums 9. tangier 10. castleman
|
|
|
What structures make up guyon canal?
|
pisiform bone, pisiform hiatus, transverse carpal ligament, connective tissue
|
|
|
How would you differentiate between an ulnar neuropathy at the elbow vs. wrist?
|
Involvement of dorsal cutaneous ulnar nerve to the 4th and 5th digits
|
|
|
How can you differentiate between lesions at proximal GC, distal GC and PHH?
|
Proximal gc- all ulnar intransics
Motor + sensory loss (occ sensory loss only) Distal gc- all ulnar intrinsics no Sensory loss, deep palmar cutaneous Branch spared PHH- all ulnar intrinsics x adq/adm |
|
|
What intrinsic muscles are supplied by ulnar nerve?
|
4 dorsal interossei 3 palmar interossei Adductor pollicis
ADQ/ADM FPM |
|
|
What 2 muscles above wrist are supplied by ulnar nerve?
|
FDP and FCU
|
|
|
What are the most common etiologies lead to ulnar neuropathy at the wrist?
|
mass lesions, ganglia, cyst, lipoma, repetitive movements, wrist fracture
|
|
|
What would an ulnar lesion sparing
ADM, inbolving 1st DI with a normal Dorsal sural snap suggest? |
PHH lesion, the most common distal ulnar neuropathy
|
|
|
What are 2 drawbacks to following aldolase in myopathies?
|
Aldolase is less sensitive/specific than CK. It is elevated in both primary muscle and hepatocellular disease
|
|
|
In PM/DM what muscle is most likely to have fibrillation potentials?
|
paraspinal muscles; Majority of these patients 50-100% of their muscles have fibs
|
|
|
What type of MUAPs are present in PM/DM?
|
normal, short dur lo amp, long duration high amp all possible. LDHA b/c of collateral sprouting, effective denervation caused by segmental myonecrosis
|
|
|
Why do myopathies get fibrillations?
|
segmental myonecrosis causing a physical separation from the NMJ leading to effective denervation, collateral sprouting, fibertype grouping, etc.
|
|
|
Name 3 causes of primary inflmmatory myopathy, 4 secondary inflammatory myopathy and 2 others.
|
1. PM
2. DM-juenile, adult, amyopathic 3. IBM ________________________ 1. "overlap syndrome" SLE, RA, Sjogren's 2. with ca- Br, Ov, Lung 3. Granulomatous (sarcoid) 4. Infection- cysticercosis, trichinella ____________________ 1. Eosinophilic 2. nodular myositis |
|
|
What is the source of CRDs and what do they indicate regarding timing of lesions?
|
muscle fiber, ephaptic conduction, usually either subacute or chronic
|
|
|
How could a MUAP be misleadingly long duration?
|
satellite potentials or linked potentials that are time locked but separated from the main body of the MUAP often seen in myopathy
|
|
|
What are 4 types of motor neuronopathy?
|
ALS, SMA, Polio, Monomelic amyotrophy
|
|
|
What are types of sensory neuronopathy?
|
paraneoplastic (Ant-Hu)
autoimmune (Sjogren's) Toxic Infectious |
|
|
What are 6 etiologies of plexopathy?
|
radiation induced, neoplastic, entrapment, diabetic, hemorrhagic and inflammatory
|
|
|
What is the rate of axonal growth determined by?
|
The rate of axonal regrowth after injury is determined by the rate of axonal transport 1 mm per day
|
|
|
If a patient with numbness of the little finger has a normal ulnar SNAP- what are 3 possible etiologies?
|
1) too early (incomplete) Wallerian degeneration
2) proximal demyelinating lesions 3) lesion at root level or above |
|
|
What is a type I error in EMG?
|
diagnosing a problem when there is not one present
|
|
|
What is a type II error in EMG?
|
not diagnosing a problem, but one is present
|
|
|
What are the divisions of the 31 spinal nerves?
|
8 cervical 12 thoracic 5 lumbar 5 sacral 1 coccygeal
|
|
|
What forms the blood-nerve barrier?
|
vascular endothelium supplying the nerve and connective tissue of the perineurium
|
|
|
What is the tensile strength of a peripheral nerve and a spinal root?
|
tensile strength of peripheral nerve is 20-30 kg, spinal root is 2-3 kg
|
|
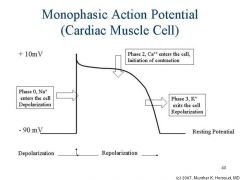
Name all the channels involved in the AP
|
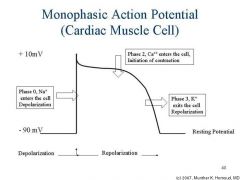
Besides those depicted, the Na channels become inactivated which can initiate repolarization
|
|
|
What are nodes of Ranvier?
|
small uninsulated gaps between Schwann cells
|
|
|
What does it mean for an action potential to be volume conducted?
|
process of an intracellular electriacal potential being transmitted through extracellular fluid and tissue is known as volume conduction
|
|
|
What is a near-field potential?
|
It can only be recoded close to its source and the characteristic of the potential depend on the distance between the recording electrodes and the electrical source
|
|
|
Explain the triphasic appearance of SNAPs as apposed to diphasic appearance of motor NCS?
|
SNAP triphasic because the initial positive is traveling toward the rec. electrode, negative deflection occurs due to potential under the electrode and then the final positive because the potential moves away. (Motor NCS are diphasic because the current is right at the recording electrode so it never moves towards it)
|
|
|
What is a far-field potential?
|
The current is instantaenous, travels in all directions and does not depend on distance
|
|
|
Why is it that conduction velocity cannot be measured by 1 stimulation for motor ncs?
|
Due to the fact that both distal latency and proximal latency will take into account time for stimulation to reach nmj, depolarize, nmj transmission and then time to depolarize the muscle. PL-DL then is measuring only the time of conduction along the nerve (distance divided by seconds)
|
|
|
How does one calculate the conduction velocity for sensory nerves?
|
distance divided by the onset latency
|
|
|
What is theadvantage to using the peak latency?
|
peak latency can be ascertained straightforward without variation and onset atency can be difficult b/c of technical factors
|
|
|
How can one differentiate a SNAP from CMA by duration?
|
SNAP duration is much shorter usually 1.5 ms while CMAP duration is usually 5-6 ms
|
|
|
why is it that peak latency cannot be used to measure conduction velocity?
|
This is because the population of fibers that represent peak latency are unknown and can't be used to calculate conduction velocities
|
|
|
What does antidromic stimulation mean?
|
toward the sensory receptor
|
|
|
What does orthodromic mean?
|
stimulation away from the sensory receptor
|
|
|
Why is it that radiculopathies do not affect SNAPs?
|
because they are proximal to the dorsal root ganglion
|
|
|
Why is it that CMAPs are not as affected by phase cancellation and temporal dispersion as SNAPs?
|
temporal dispersion is affected by a wide variety of fibers some with myeling/large diameter etc. there is less variability in motor fibers; phase cancellation the duration of muaps/cmaps are very similar and therefore are not as affected by phase
|
|
|
Why is it that motor fibers are not as affected by phase cancellation as sensory fibers?
|
Motor fibers are not as affected by phase cancellation because they are longer duration and their positive & negative phases tend not to overlap as much as the positive & negative phases of the short duration SNAPs
|
|
|
Name 10 types of hereditary demyelinating neuropathies.
|
1) CMT 1A HMSN 1
2) Dejerine Sotas HMSN 3 3) Refsum's HMSN 4 4) HNPP 5) Metachromatic Leukodystrophy 6) Adrenoleukodystrophy 7) Cockayne Syndrome 8) Cerebrotendimoatous Xanthoma 9) Krabbe's Syndrome 10) niemann-pick disease |
|
|
Name 6 types of CIDP
|
1) Idiopathic
2) Assoc. with HIV 3) Assoc. with anti-MAG 4) Assoc with osteosclerotic myeloma 5) Assoc. with waldenstrom's macroglobulinemia 6) assoc with MGUS |
|
|
Name 5 types of acquired demyelinating disease
|
1) AIDP
2) CIDP 3) Toxin (Toluene, amiodarone, arsenic) 4) Diphtheria 5) Multifocal motor neuropathy with conduction block |
|
|
What is a normal H response?
|
<34 msec
|
|
|
How could one differentiate an H response from an M wave ?
|
As stimulation intensity is increased the M wave will grow larger, but the H will get smaller
|
|
|
Differentiate the H & F based on 1)afferent-efferent 2)morphology & stability
3) normal values 4)nerves studies. |
1) H sensory 1A-motor
F motor-motor 2) H triphasic stable impersistent F polyphasic persistent (each waveform should be different) 3) H <34 F <32 in arms <56 in legs 4) H- tibial-soleus median-FCR femoral-quads F- all |
|
|
What should the gain and sweep be to evaluate an F response?
|
200 mv and 5-10msec
|
|
|
What is an F response?
|
An F response occurs because after stimulation potentials move toward AHC (antidromic) and then cause a backfiring, orthodromic potential down the nerve without synapse (not a reflex) and only has 1-5% of motor fibers; called F because it was named after foot
|
|
|
Why is it that the cathode should be more proximal when performing an F wave?
|
Theoretical risk that the potential will be blocked by the anode (anodal block) in the standard position
|
|
|
What 3 features should be studied when performing F waves?
|
1) chronodispersion (maximal - minimal latency)
2) impersistence 3) minimal latency |
|
|
What are some limitations of the F response in assessing proximal lesions?
|
1) F waves only measure C8-T1 radiculopathies (not as common site)
2) If Sensory neuronopathy then F wave would be normal (like in anti-Hu's) 3) If only a small proximal segment demyelinated F may still look normal 4) For the F to be abnormal then a lot of the motor neres would have to be affected, which doesn't necessarily happen and there is a lot of overlap in myotomes |

