![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
SOB: initial assessment |
Vitals- special attention to respiratory rate and pulse ox PEARL- A respiratory rate of 16, 18, or 20 in an adult probably means that it wasn’t counted accurately- it says “I think the respiratory rate is normal”- think of anything over 20 as tachypenic
Rapid assessment- look at the patient’s work of breathing and make a decision as to whether they have increased work of breathing
PEARL- The decision to intubate is based on clinical situation- not numbers- a severe COPD patient may live at a pCO2 of 70 and a pulse ox of 92- if they are talking without distress they probably don’t need a tube. Its about mental status and work of breathing- not numbers
|
|
|
SOB: history |
History- ask standard OPQRST questions about when the SOB started Important associated symptoms- Chest pain (PE or MI), fever (pneumonia), lower extremity edema (CHF), increased sputum (COPD) Aggravating factors- dyspnea on exertion or orthopnea (SOB with rest) PEARL- bad bronchitis or COPD can cause some blood tinged sputum- clarify the amount- blood tinged or dime sized is not as worrisome- “nothing but blood” is worrisome
Medical history- focus on asthma, COPD, cardiovascular history. Ask about hx of MI, strokes, CABG, catherizations. Ever intubated for COPD or asthma? Medications- recently on antibiotics or steroids? Recent med changes? Social history- most important is tobacco use
|
|
|
SOB: exam |
Work of breathing- may have to take down the patient’s gown. Look for accessory muscle use (clavicles) or retractions (usually). Retractions- paradoxical contraction of muscles with inspiration HEENT- assess the upper airway for foreign bodies and for predictors of difficult intubation (poor mouth opening, visibility of soft palate, etc.) Heart- Listen to it first before lungs (better exam that way), listen for valve disorders (aortic stenosis most common in older patients) Lungs- Assess both sides all of the way up, full lung sounds vs. quiet chest?, listen for crackles, rhonchi, and wheezing PEARL- In young children- count out respiratory rate while you listen to lung sounds- easier than counting by watching- do it for a full minute!
Abdomen- assess for tenderness- don’t miss a perotinitis Extremities- lower extremity edema, calf tenderness (DVT?)
|
|
|
SOB: differential dx |
Tubes- upper airways- airway obstruction or burns, dental or neck abscess, foreign body, croup, epiglottitis Lower airways- bronchitis, asthma, COPD, bronchiolitis (kids <2 y.o.) Lungs- Pneumonia Pipes- Pulmonary embolism Pump- Congestive heart failure, valve disorders Outside the lungs- pneumo/hemothorax, pleural effusion, abdominal process
Dental or neck abscess- most worrisome is Ludwig’s angina- deep space neck infection- classically in diabetics with poor dentition, look toxic, have brawny edema of floor of the mouth, drooling- need broad spectrum antibiotics and OR emergently with ENT to drain infection and secure airway
Foreign Body- most common in kids- sudden onset of stridor without a cough and no other viral symptoms
Croup- Viral infection in kids caused by parainfluenza, causes upper airway swelling and “barking seal” cough, worse at night, stridor at rest is more severe (see below)
Epiglottitis/tracheatitis- upper airway infections, usually in children but today is more seen in adults (waning vaccine immunity), toxic appearing, drooling, hoarse voice. Don’t agitate- get immediately to the OR Lower airway Asthma- usually a younger patient with wheezing and shortness of breath, on outpatient inhalers COPD- usually an older patient with a history of smoking, wheezing, and on outpatient inhalers
Bronchiolitis- viral syndrome, wheezing, respiratory difficulty, bilateral runny nose in a child <2 years old
Lungs Pneumonia- cough, fever, SOB, +/- hypoxia, chest x-ray with an infiltrate
Pipes (blood vessels) Pulmonary embolism- sudden onset of pleuritic chest pain, shortness of breath, risk factors include OCPs, immobilization, recent surgery, etc.
Pump (heart) Congestive heart failure- dyspnea on exertion with lower extremity edema, orthopnea, crackles on lung exam, “wet” chest x-ray MI- chest pain, diaphoresis, nausea, EKG changes
Outside the lung (space occupying) Pneumothorax- spontaneous (thin tall young patient or bad COPD/asthma) or traumatic, air in chest cavity on CXR Hemothorax- traumatic- seen as a white out on the CXR Pleural effusion- layering fluid at bases on CXR Abdominal process- perotinitis, free air under diaphragm
|
|
|
SOB: workup |
EKG- low threshold especially on older patients and in anyone with CHF or MI as a consideration (most patients over 40 should get one) Chest x-ray- Low threshold but can withhold it if it seems like an obvious asthma exacerbation or clear cut bronchiolitis PEARL- If patient is in distress or has chest pain, get a 1 view portable CXR at the bedside, otherwise send for a 2 view PA and lateral, 2 view is better, can’t tell cardiomegaly from 1 view CT Pulmonary Angiogram- if considering PE Workup- Labs
In general- if you are going to send the patient home, don’t get labs (or at least don’t order them and send them), if you admit, get labs
Venous blood gas- can be helpful in cases of severe SOB but don’t base airway interventions on those numbers alone
CBC/Chem 10- in COPD and pneumonia patients that you are going to admit Blood cultures x2- Only in pneumonia patients, ? quality measure but this seems to change everyday, don’t order them unless you are admitting the patient to avoid culture callbacks. Can tell your nurse/tech to draw and hold if you are unsure whether the patient will be admitted
CBC, chem 10, coags- PE workup patients (check creatinine for IV contrast, platelets and coags for possible anticoagulation) Cardiac Enzymes- Cardiac workup- CK, CK-MB, Troponin, +/- myoglobin BNP- secreted by the heart in response to increased ventricular stretch, <100- probably not CHF, >400- probably CHF 100-400 indeterminate |
|
|
SOB: treatment |
Treatment
Non-invasive Ventilation (CPAP and BiPAP)- can use to avoid intubation and reduce work of breathing, start at 10/5 and titrate upwards
Asthma and COPD Beta Agonists- albuterol- 2.5 mg unit dose or 5mg continuous (child) or 10mg continuous (adult) Anticholinergic- ipatroprium (atrovent)- 1 dose during ED stay (1 dose lasts 4-6 hours, no benefit from higher dosing)
Steroids- for both asthma and COPD Prednisone- 50mg PO for adults (5 day total course) Orapred (oral prednisolone)- 1 mg/kg PO BID for kids (5 day course) Solumedrol (IV prednisolone)-125 mg IV or 2mg/kg for kids PEARL- Bioavailability is the same PO vs. IV- only reason to give IV is if the patient is too tachypenic to take PO COPD flares- add antibiotics (anti-inflammatory effects) Outpatient- Azithromycin (Z-pack)- 500mg on day 1, 250 for days 2-5 Inpatient- Azithromycin or Levaqiun (levofloxacin)- 500mg IV
Bronchiolitis treatment- mostly supportive Treatment- nasal suctioning and oxygen as needed PEARL- Beta agonists don’t help bronchiolitis PEARL- High risk bronchiolitis patients (need admission for apnea monitoring)- 12 bed PICU- <12 weeks old, Premature, Immunodeficient, Cardiac anomaly (congenital)
Croup- mostly supportive Decadron (dexamethasone)- 0.6 mg/kg PO, max 10mg Racemic Epi neb- only for kids with stridor at rest (i.e. when NOT agitated or crying)- requires 4 hour observation period after neb
The lungs Pneumonia- most common cause is strep pneumonia Treatment- antibiotics, oxygen as needed Adults- Community Acquired- outpatient- Azithromycin (Z-pack) Adults- Community Acquired- inpatient- ceftriaxone 1 gram IV and Azithromycin 500mg initial dose in ED Children- Community Acquired- outpatient- amoxicillin 45 mg/kg BID PEARL- Amoxicillin 400mg/5ml= 1 teaspoon for every 10 kg (like children’s acetiminophen/ibuprofen) Children- Community Acquired- inpatient- Ceftriaxone 50 mg/kg IV and azithromycin 10 mg/kg Hospital Acquired- see sepsis podcast
The Pipes (blood vessels) Pulmonary embolism- heparin/enoxaparin - see chest pain podcast The Pump (heart) Congestive Heart Failure (CHF)- nitrates, Lasix Nitroglycerin- start with sublinguals (0.4 mg q 5 minutes= 80 mcg per minute), can do IV drip for more severe cases Lasix- loop diuretic- takes 4-6 hours for diuresis but is a weak venodilator (nitro much better)- 20mg IV or usual outpatient PO dose given IV.
Outside the lungs
Pneumo/hemothorax- drain using a chest tube Pleural effusion- consider draining but most will resolve if you treat the underlying condition
|
|
|
AMS: history |
Vitals- temperature is most important (fever or hypothermia) How is the patient altered?- talk with family, EMS, nursing home Recent trauma or illness? Onset of AMS? Psychiatric history- don’t attribute it automatically to this Ingestions- legal or illegal Talk to the patient- oriented to person, place, time, situation/president? Check recent memory of events
******BIG PEARL****** ALL PATIENTS WITH AMS ARE HYPOGLYCEMIC UNTIL PROVEN OTHERWISE Check a d-stick, if below 80 give 1 amp D50 IV
|
|
|
AMS: exam |
Exam Neuro exam- Cincinnati Prehospital Stroke scale- high yield exam Face- facial droop- ask patient to smile, positive if asymmetric Arms- lift arms to shoulder level with palms up, close eyes, positive if asymmetry or one side falls to the stretcher Speech- slurred speech? “You can’t teach an old dog new tricks” Time- what was exact time of onset?
Pupils- check size and reactivity, evidence of nystagmus Axilla- if suspecting a tox cause, if axilla are dry- suggest anticholinergic exposure/ingestion Lungs- focal lung sounds suggesting pneumonia Abdomen- tenderness or pain especially in elderly Skin- GU area for infected decubitus ulcers, any rashes or petechiae?
|
|
|
AMS: Differential dx |
Differential Diagnosis (Big list- AEIOU TIPS)
A- Alcohol/acidosis E- Electrolytes I- Infection O- Oxygen (hypoxia/hypercarbia) U- Uremia
T- Toxidromes / Trauma / Temperature I- Insulin (too much)/ Ischemia P- Psych / Polypharmacy S- Stroke/Space occupying lesion / SAH |
|
|
AMS: Differential Dx detailed |
Opiates- vicodin (hydrocodone/acetaminophen), percocet (oxycodone/acetaminophen), oxycontin (oxycodone), heroin- somnolent, lethargic, respiratory depression, pinpoint pupils, treatment with Narcan (naloxone)
Benzodiazepenes- valium (diazepam), Ativan (lorazepam)- somnolent, lethargic, not as much respiratory depression, supportive care, support ABCs
Sympathomimetics (uppers)- cocaine, PCP, meth, agitated, hyper, dilated pupils, supportive care, use benzos to sedate, RSI for uncontrolled agitation
Tox workup- D-stick, EKG, CBC, Chem 10, Serum Tylenol (acetaminophen), Serum ETOH, Serum Salicylate, +/- urine drug screen (lots of false positives, doesn’t tell current intoxication)
PEARL- Unlike salicylate and ETOH use, Tylenol (acetaminophen) overdose don’t have a specific toxidrome and will likely be asymptomatic, important to get this level given it is easily missed and mortality is high
Trauma- any history of falls either recent or remotely. Non-contrast head CT is test of choice upfront
PEARL- Have a low threshold to get a head CT in AMS, especially in patients with what appears to be new onset psychiatric disease even if they don’t have neuro deficits
Infection- look for fever, hypotension, tachycardia, try to ID a source, make sure to do a thorough skin and GU exam
PEARLS -The elderly and those on immunosuppression or steroids may not mount a fever in response to infection -UTIs cause lots of AMS in the elderly -Hypothermia in the setting of infection is especially concerning
|
|
|
AMS: early workup |
Infection workup- CBC, Chem 10, blood cultures x2, UA and urine culture, chest x-ray, LP if suspecting meningitis
PEARL- You have several hours before antibiotics will affect culture results so give antibiotics early, especially if you suspect meningitis
Broad spectrum antibiotics Zosyn (piperacillin/tazobactam)- 3.375 or 4.5 grams IV Vancomycin- 15-20 mg/kg, usual dose 1 gram IV (many guidelines suggest 1st dose be 2 grams IV for faster therapeutic levels) Ceftriaxone- (in some areas better than Zosyn for urinary pathogens) 1 gram IV, 2 grams IV if suspecting meningitis (along with Vancomycin)
|
|
|
AMS: seizures/stroke |
Seizures- make sure they aren’t from hypoglycemia first, -Must have some sort of post-ictal state afterwards with AMS that slowly or quickly improves -May be intermittently agitated and then somnolent -If they have a seizure history and they didn’t hit head, support ABCs and you can allow to wake up and try to find cause (usually missed medication doses) -If new onset seizure, trauma, or other concerns, do appropriate workup
Stroke- New onset focal neuro deficits -D-stick first, hypoglycemia can mimic a stroke -Address ABCs then immediately get a non-contrast head CT -Don’t delay on the head CT, activate ED stroke protocol -If no intracranial bleed and within 3 hours of onset, can give TPA if no contraindications -Get a checklist of all contraindications and go through each one -Certain patients qualify for 4.5 hour time window for TPA
|
|
|
AMS: Hyponatremia and HyperK |
Hyponatremia
-Asymptomatic- water restrict -Below 120 and seizing- hypertonic saline 3%, 2-3 cc/kg over 10 minutes and repeat until seizures stop -Below 120 but not seizing- consult appropriate reference for slow replacement with hypertonic saline
Hyperkalemia
-EKG changes (peaked T waves, QRS widening)- immediately give 1 amp Calcium gluconate IV to stabilize cardiac membrane and prevent arrhythmias -Other treatments- insulin/glucose, furosemide, albuterol, dialysis
|
|
|
AMS: workup |
General AMS workup (add or subtract testing as appropriate for clinical situation)
****D-STICK**** Urine Drug Screen (with caution) EKG Serum acetaminophen (Tylenol) level CBC Serum ETOH level Chem 10 Serum salicylate level UA/Urine Culture LP if suspecting meningitis Blood culture x2 Chest x-ray VBG with lactate Non-contrast head CT
|
|
|
AMS: major points |
1) All patients with AMS are hypoglycemic until proven otherwise 2) Broad categories of AMS- TINE- Trauma/Tox, Infection, Neuro/Electrolytes 3) Have a low threshold for non-contrast head CT 4) Get a good neuro exam- quickest is Cincinnati Prehospital Stroke Scale- Face, Arms, Speech, Time
|
|
|
Syncope: Definition |
Definition of syncope- a rapid loss of consciousness followed by a rapid return to baseline -Pure syncope- usually cardiac in nature- rapid loss of bloodflow to the brain -Vasovagal syncope- stressor causes increased vagal tone that causes bradycardia and hypotension -> syncope (if the patient has other symptoms like chest pain or headache, is confused after awakening or is unconscious for an extended period of time- that is not pure syncope and demands a different workup) |
|
|
Syncope: history |
History- it’s all about the history for this chief complaint
PEARL- Dizzy does not equal syncope! Dizziness- sense of the room spinning or loss of balance (disequilibrium)= different workup than syncope workup -Ask the patient: “Was the room spinning or did you feel like you were going to pass out?” (Spinning= dizziness, pass out= syncope)
PEARL- Near syncope (or lightheadedness) is the same as Syncope (in regards to the workup)
Stressors- try to identify preceding stressors- dehydration, emotional distress, rapid temperature changes, painful condition, insufficient food or water intake
Symptoms- prodrome of feeling flushed and hot, tingling in extremities, nausea = more suggestive of vasovagal syncope
Activity- what was the patient doing? Were they exercising at the time of collapse (VERY IMPORTANT!)
Witnesses- ask them if the patient hit their head, any seizure activity (more than a few muscle jerks?), how long until the patient woke up, any confusion after waking up? PEARL- to diagnose a seizure there has to be sustained generalized tonic/clonic movements followed by a period of post-ictal confusion
Preceding symptoms and red flags
Syncope + headache= subarachnoid or intracranial hemorrhage Syncope + neuro deficit= stroke/TIA or intracranial bleed Syncope + confusion= seizure Syncope + chest pain= MI, PE, or aortic dissection Syncope + back/abdominal pain in older patient= abdominal aortic aneurysm (AAA) Syncope + positive HCG= ectopic pregnancy
Past medical history- is this recurrent syncope or is this new? Ask for history of seizures, MI, stroke/TIA, known AAA, family history of heart disease
PEARL- In younger patients say “I’m not saying this is going to happen to you but did anyone in your family die suddenly and they couldn’t find out why?” (Screen for inherited arrhythmias/cardiomyopathy) |
|
|
Syncope: physical exam |
Physical exam- check for head trauma, do a good neuro exam, listen for murmurs (both with valsalva and with standing and squatting in younger patients), abdominal/back tenderness |
|
|
Syncope: Differential Dx |
Differential diagnosis (with triggers)
Seizure- sustained generalized tonic/clonic movements with eyes open with post-ictal confusion
Subarachnoid/intracranial hemorrhage- syncope plus a headache or a neuro deficit
Ruptured AAA- older patient with hypertension with back/abdominal pain or hematuria +/- unstable vital signs- stat bedside ultrasound Stroke/TIA- syncope with neuro deficit
GI Bleed- syncope plus black or bloody stools
MI/ACS- chest pain and syncope
Aortic dissection- sudden onset of ripping or tearing chest/back pain +/- pulse or neuro deficit
Aortic stenosis- older patient with a systolic ejection murmur that radiates into the carotids
Pulmonary embolism- sudden onset of dyspnea/pleuritic chest pain +/- risk factors for PE
Arrhythmia- see below- WPW/HOCM/Long QT/Brugada
Carotid sinus sensitivity- syncope with activities that put pressure on carotid sinus (tying a necktie, shaving, checking carotid pulse)
Orthostatic hypotension- medications such as alpha and beta blockers, dehydration
Hypoglyemica- diabetic patient or ingestion of diabetic medications
Tox- drugs, ETOH, environmental (carbon monoxide)- look for a toxidrome
Sepsis- fever and signs of infection
|
|
|
Syncope: workup |
Labs (if necessary, usually for older patients who are being admitted)
D-stick (some clinicians do this in all patients) CBC- (severe anemia can cause syncope) Chem 10- (electrolyte abnormalities can cause arrhythmias) UA- UTIs can cause a wide variety of symptoms in older patients Non-contrast head CT- if there is head trauma +/- C-spine CT as needed
EKG findings in syncope- look for these 4 findings on EVERY EKG on a patient with syncope- Long QT, Brugada, WPW, HOCM/LVH Pneumonic- BLOW Hard- (Brugada, LOng QT, WPW, HOCM)
Long QT syndrome- congenital disorder causing prolonging of refractory period = greater chance of R on T phenomenon (PVC on downslope of T wave causing v-fib).
EKG- Long QT defined as >440 milliseconds in males, >460 ms in females (some experts say QTs >500 are most concerning)
PEARL- to eyeball a normal QT- T wave is within the first half of the R to R interval, look for U wave that may cause EKG machine to overcall the QT interval
Dispo- no exercise until evaluated and cleared by cardiology, give seizure precautions (no driving, no swimming, shower with a chair or with someone nearby)
Wolf Parkinson White (WPW)- accessory pathway that bypasses AV node and can cause V-tach EKG- shortened PR and delta wave (slurring of Q to R transition)- Dispo- needs Cardiology/EP followup, no exercise until cleared by cardiology
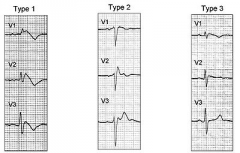
Brugada syndrome- sodium channel disorder- frequent syncope in a young and otherwise healthy patient without heart disease with a right bundle block pattern and ST elevation in V1-V3 Dispo- admit for immediate implanted defibrillator placement (high risk for sudden death)
Hypertrophic cardiomyopathy/LVH- thickened LV wall that causes outflow obstruction with exercise, classically a young athlete that collapses during exercise EKG- LVH (tall R waves in V4-V6 or AVL and deep Q waves in V4-V6) Dispo- confirm with echo + no exercise until cleared by cardiology
|
|
|
Syncope: dispo |
Young patients- normal EKG/negative HCG, no red flags, and normal EKG= discharge Older patients (50 or over- my opinion, definitely over 65)- admitted for telemetry monitoring and further workup
San Francisco Syncope rule- insufficient sensitivity to rule out need for admission (52-92% sensitivity for serious outcomes in validation studies) if positive, more reason to admit
CHF- History of CHF or current suspicion Hematocrit <30% EKG abnormalities (non-sinus rhythm or change in EKG)* Shortness of breath (with syncope episode) Systolic BP less than 90 after arrival to the ED
*Although this was excluded in the original study, most clinicians also include any T wave abnormalities in the “abnormal EKG” criteria
|
|
|
Syncope: big points |
1) Syncope= rapid loss of consciousness followed by rapid return to baseline- period, anything else demands a bigger workup 2) Syncope workup must include EKG and HCG in females, everything else dictated by clinical scenario 3) Syncope with exercise= red flag- look for WPW, Long QT, Brugada, and HOCM in young patients 4) Young patients with syncope with no red flags and negative EKG/HCG go home, older patients get admitted for further workup
|

