![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
What is cardiac monitoring and why do it? |
- cardiac monitoring gives a ‘real time’ continuous recording of the cardiac rhythm - it detects any changes - fast or slow, regular or irregular |
|
|
What is an ECG? (Electrocardiogram) |
- 10 electrodes placed in set positions on the body - assesses the electrical activity of the heart at 12 different angles |
|
|
Practical aspects of recording an ECG |
-patient identity confirmed/gained consent -patient laid down at 30/45 degrees with arms by their side - skin may require cleaning (and drying) - modify for smaller patients - male patients may require chest hair shaving - under or over the breast? - patient should be as relaxed as possible - ECG machine set at 25mm/sec and 10mm/mV - filter button off unless absolutely necessary |
|
|
What can go wrong when recording an ECG or cardiac monitoring? - causing inaccurate results |
- patient moving around - electrical interference - patient coughing - placing the leads the wrong way around |
|

12 lead placement |
-V1: 4th intercostal space (ICS), RIGHT margin of the sternum -V2: 4th ICS along the LEFT margin of the sternum -V4: 5th ICS, mid-clavicular line -V3: midway between V2 and V4 -V5: 5th ICS, anterior axillary line (same level as V4) -V6: 5th ICS, mid-axillary line (same level as V4) |
|
|
What should be written/printed on the ECG? |
-name -nhs number -date of birth -date and time recorded -why it has been recorded -any required identifiers |
|
|
What should be written/printed on the ECG? |
-name -nhs number -date of birth -date and time recorded -why it has been recorded -any required identifiers |
|
|
What electrical charge does a ‘resting’ cardiac cell have? |
A negative electrical charge compared to their surroundings |
|
|
What happens when a cell becomes ‘depolarised’? |
When it is stimulated to do so, the cells become depolarised - they become positively charged in comparison to their surroundings |
|
|
What happens when a cell becomes ‘repolarised’? |
-after a short time, the cells become repolarised - their charge returns to the negative, resting state |
|
|
What happens when a cell becomes ‘repolarised’? |
-after a short time, the cells become repolarised - their charge returns to the negative, resting state |
|
|
What can cause the cardiac cell to contract? |
Most of the time, being depolarised can cause the cardiac cell to contract |
|
|
What happens when a cell becomes ‘repolarised’? |
-after a short time, the cells become repolarised - their charge returns to the negative, resting state |
|
|
What can cause the cardiac cell to contract? |
Most of the time, being depolarised can cause the cardiac cell to contract |
|
|
Why are some complexes positive and some negative? |
- a wave of depolarisation moving towards a lead (f causes an upward (positive deflection on the ECG - a wave of depolarisation moving away from a lead causes downward (negative) deflection on the ECG - in the absence of electrical activity the ECG trace will return to the baseline |
|
|
What are the general principles of an ECG? |
- The wider something is on the ECG, the longer it has taken (in time) to happen - The taller (or deeper) something is on the ECG, the more electrical energy is involved - which usually reflects the amount of heart muscle (myocardium) represented |
|

The P wave |
- caused by atrial depolarisation - normally upright in most leads (the notable exception is a aVR, in which the P wave is usually negative) |
|

PR interval |
- represents AV nodal delay - measured from the start of the P wave to the first QRS deflection -should be no greater then 0.2 seconds (1 large or 5 small squares) |
|

QRS complex |
- represents ventricular depolarisation - measured from first deflection after P wave, to end of S wave - should be less then 0.12 seconds (3 small squares) |
|

ST segment |
- electrically neutral period, myocardium remains contracted - represents the time between ventricular depolarisation and repolarisation |
|

T wave |
- represents repolarisation of the ventricles - usually the same orientation as the QRS complex - usually asymmetrical, with a shallow first half, steep second - if there is a QRS then there will always be a T wave |
|
|
What are the general principles of reading an ECG? |
- If the rhythm has some sort of P wave activity followed by a narrow QRS the impulse is generated in the atrium. - If it is a normal looking P wave followed by QRS it is sinus rhythm/tachycardia/bradycardia - If the QRS complexes are wide and bizarre and no P wave it is generated in the ventricles hence ventricular tachycardia/ ventricular ectopic. - If there is a normal P wave but a wide and bizarre QRS there is a conduction defect in the ventricles. But it is sinus. |
|
|
How many leads provide a 12 lead view? |
10 |
|
|
Where are the other 4 leads for a 12 lead view?
*Excluding v1-6 on the precordium |
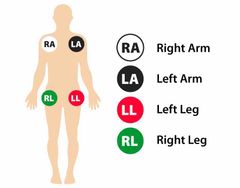
- There are 4 leads, one on all 4 limbs - right leg - left leg - right arm - left arm |
|

Where are the other 4 leads for a 12 lead view?
*Excluding v1-6 on the precordium |

- There are 4 leads, one on all 4 limbs - right leg - left leg - right arm - left arm |

