![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
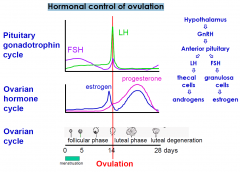
Hormonal control of ovulation
|
|
|
|
Follicular Phase
|
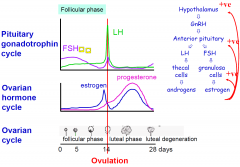
1. FSH stimulates follicle growth (15-20 grow one matures fully)
2. FSH drops due to inhibin secetion |
|
|
Luteal Phase
|
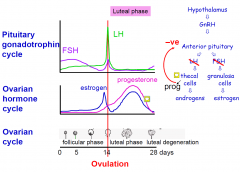
PG drops of as the corpus leutum dies and then the -ve feedback is released allowing the FSH to rise again
|
|
|
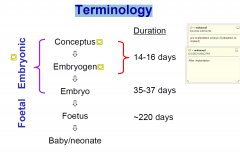
Terminology
|
|
|
|
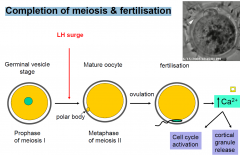
Completion of meiosis & fertilisation
|
|
|
|
Pre-implantation stages (Days 0-6)
|
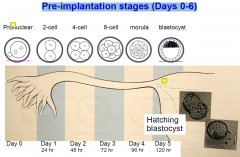
the inc. in PG relaxes the sphincter allowing passage to the blastocyst (into uterus)
|
|
|
Compaction - the start of differentiation
|
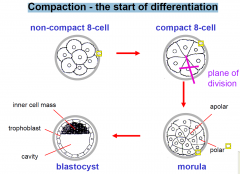
COMPACT: formation of tight junction proteins
|
|
|
Compact 8 cell
|
totipotent
|
|
|
Morula
|
- apolar cells are pluripotent
- polar cells form trophoblasts |
|
|
Function of the zona pellucida during early pregnancy
|
- surrounds conceptus from fertilisation to blastocyst stage
1. Prevents polyspermy 2. Prevents premature implantation 3. Prevents two zygotes from sticking together 4. Keeps blastomeres together until compaction |
|
|
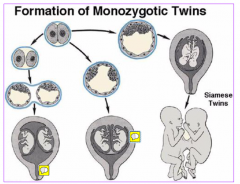
Formation of Monozygotic Twins
|
|
|
|
Receptivity of uterus to conceptus implantation
|
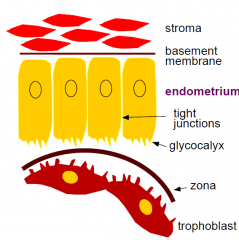
1. Pre-receptive phase
-epithelium has long apical microvilli, thick glycocalyx, -ve charge impairs attachment 2. Receptive phase - apical protrusions absorb uterine fluid decrease volume of uterine cavity - loss of -ve charge - microvilli shorten - glycocalyx thins close apposition of blastocyst to uterus attachment 3. Refractory phase - resists attachment |
|
|
Why is implantation necessary?
|
•Blastocyst - bathed in uterine secretions
»Provides O2 and metabolites required for growth and survival •Size limited •Critical for conceptus to develop its own blood supply for exchange of substances •Implantation failure - major cause of infertility due to inadequate uterine receptivity •Implantation = 1) Attachment 2) Invasion |
|
|
Attachment - day 6
|

- close apposition and adherence of trophoblast cells to endometrium
|
|
|
Attachment
|
•Zona broken down by proteases
•In a few hours »increases vascular permeability in stroma underlying contact point »Changes in stromal morphology - sprouting and ingrowth of new capillaries = primary decidua •A few days after initial attachment »Formation of new capillaries in stroma spreads to larger area |
|
|
Attachment TO invasion
|

Still within a few hours of attachment
- surface epithelium under the blastocyst becomes eroded - trophoblast processes invade between epithelial cells - isolating and digesting them |
|
|
Implantation (completed by day 9)
|

- some trophoblasts fuse to form syncytium (syncytiotrophoblast)
- others remain proliferative (cytotrophoblasts) - uterine glandular and decidual tissue is destroyed -> release of metabolic substances which can be taken up by conceptus (functions as a yolk) |
|
|
Hormones/cytokines involved in attachment
1. oestrogen: on uterus |

|
|
|
Hormones/cytokines and attachment
Oestrogen (2) acts on blastocyst |

|
|
|
Hormones/cytokines and attachment
Corticotrophin releasing hormone (CRH) |
During implantation the endometrial response to the invading blastocyst has characteristics of an acute aseptic inflammatory response
But - once implanted the embryo suppresses this and prevents rejection Trophoblast and decidual cells produce CRH and express Fas ligand -> kills activated T cells -> prevents embryo rejection |
|
|
Maternal recognition of pregnancy
|
After ovulation the collapsed follicle transforms into corpus luteum consisting of:
Granulosa cells - secrete progesterone and oestrogen Thecal cells - secrete progesterone and androgens In non-pregnant woman - life of corpus luteum 12 -15 days - low LH level -> fall in progesterone secretion -> luteolysis |
|
|
Pregnant:
requires prolongation of luteal phase of ovarian cycle |
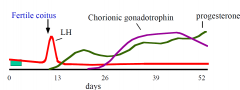
In pregnant woman
- hCG secreted by trophoblasts from 6-7 days post-fertilisation - secreted by syncytiotrophoblasts - passes into maternal circulation (measureable at 8-12 days) - binds to LH receptors on luteal cells (thecal) -> prevents luteolysis -> progesterone production maintained |
|
|
Nausea and vomiting during pregnancy
|
morning sickness !!
most common symptom of pregnancy - 50-90% of women in 35% have physical and psychosocial implications begins first trimester continues to ~12 wks gestation severe form = hyperemesis gravidarum – in <1% of women vomiting, weight loss risk dehydration, electrolyte imbalance fetal complications – fetal growth retardation |
|
|
N/V Causes
|
underlying pathophysiology - poorly understood
evolutionary adaptation? - also women with nausea during pregnancy are unlikely to miscarriage combination of factors: genetic endocrine – HCG, progesterone, thyroid hormone gastrointestinal |
|
|
Nausea and vomiting during pregnancy
Treatment: |
dietary modifications
dry, bland food !! adequate hydration decrease fatty food intake high protein diet vitamin B6 antiemetics (dopaminergic antagonists, anti-histamines, anti-cholinergics, 5-HT3 receptor antagonists) ginger, other herbal remedies |
|
|
Plasma hormones during pregnancy
DAY 40 |
By day 40 - corpus luteum no longer required
- placental trophoblasts produce progesterone - embryo produces oestrogen |
|
|
Plasma Hormones by week 6-7
|
By 6-7 weeks - hCG levels fall
-> syncytiotrophoblasts start to secrete somatomammatrophins incl. placental lactogen (placental variant of GH) -> fetal growth |
|
|
Plasma Hormones in Pregnancy
|

|
|
|
Dating of pregnancy
|

|
|
|
Developmental milestones (embryonic)
2 weeks |
– sac 2-3mm
– ectoderm, mesoderm, endoderm formed – yolk sac formed |
|
|
Developmental milestones (embryonic)
week 3 |
– brain, spinal cord and heart begin to develop
– gastrointestinal tract begins to develop |
|
|
Developmental milestones (embryonic)
week 4-5 |
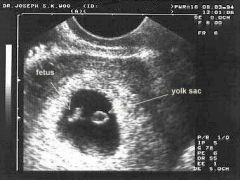
– embryo can be seen on ultrasound
– sac 20-25 mm, embryo 10 mm – arm and leg buds become visible – eyes and ear structure begin to form – formation of tissue that develops into vertebra & some other bones - further development of heart – now beats at a regular rhythm - movement of rudimentary blood through the main vessels |
|
|
Foetal heart rate
|
Measurement made from week 4-5 (ultrasound) through to labour (Doppler)
Rate increases with embryo development - week 4 = 75 beats / min - week 7-8 = 130 beats / min Foetal heart rate = 120 – 160 beats / min Low heart rate at 6-7 weeks (<90 beats / min) - used as an indicator of developmental failure and predictor of a risk of spontaneous miscarriage |
|
|
Developmental milestones (embryonic)
week 6 |

– sac 30-50 mm, embryo 20 mm
– arms and legs have grown longer – hands and feet have fingers and toes (digits) – brain continues to form - lungs begin to form |
|
|
Causes of spontaneous miscarriage
|
Miscarriage = spontaneous abortion before week 20
1.Maternal causes •Acute febrile illness •Septicaemia with infection of the foetus •Severe hypertension or renal disease •Diabetes (upto 45% if uncontrolled) •Hypothyroidism •Trauma •Drugs •Uterine fibroids •Congenital malformations of uterus •Hormone deficiency (progesterone) 2. Foetal causes •Genetic abnormalities •Congenital malformations •Faulty implantation |
|
|
Recurrent miscarriage
|

> 3 times consecutively prior to 20 weeks gestation
|
|
|
Critical periods of development -preimplantation?
|
30% fail to implant (based on IVF and animal studies)
-environment -> gene expression -> epigenetic changes -> genomic imprinting disorders -> altered metabolism -> impacts on fetal development -> impacts on child & adult health |
|
|
Critical periods of development
|
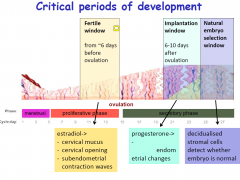
|
|
|
Critical periods of development
|
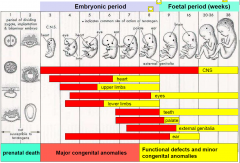
|

