![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back

A 26-year-old pregnant woman who by examination is small for gestational age.
|
Key measurements: At times, the various routine
measurements of the fetus ( femur length, biparietal diameter, head circumference, and abdominal circumference) can vary a great deal from each other. The critical step is to look for key measurements (abdominal circumference [AC] and sonographic measurements) to fall below a significant threshold. This can only be done with reasonable certainty when the gestational age has been determined by a prior ultrasound before 24-26 weeks or there is good clinical proof of gestational age (e.g., ovulation induction). • Abdominal circumference: A smaller than expected AC can be a result of technical error, fetal diaphragmatic hernia, or gastroschisis. The most common cause is that the fetus is smaller than average . • Estimated fetal weight (EFW): The EFW is a calculation generated from routine measurements. The measurements used will vary with the formula chosen, but usually the head circumference, femur length, and AC are used. Small fetal weights are seen in a variety of circumstances. If seen early in pregnancy, the possibility of an early intrauterine infection or a chromosomal abnormality should be considered. |
|
A 32-year-old woman who by examination is "large for dates."
|
Placental enlargement: This is one manifestation of
hydrops. It is also seen with intrauterine infections and certain chromosomal abnormalities (triploidy most commonly) and in some patients with diabetes. • Polyhydramnios: This is another manifestation of hydrops. It is also seen in a large number of conditions, including twins, diabetic mothers, and various fetal abnormalities including high gastrointestinal obstructions, central nervous system abnormalities, cardiac abnormalities ( both structural and arrhythmias), and in a host of miscellaneous conditions including certai.il types of limb-shortening syndromes. Many cases of polyhydramnios have no known cause. • Skin edema: This is a common feature of hydrops. A similar appearance is seen in lymphangiectasia, which is often present in association with cystic hygromas. Infants of diabetic mothers with severe macrosomia are often mistaken for babies with skin edema. • Fluid collections: Collections of fluid within the fetus are frequently seen as an indicator of hydrops. Isolated fluid collections can be seen as a result of local inflammation, obstruction, or unknown mechanisms in conditions other than hydrops. For example, obstruction of the moracic duct can lead to pleural fluid, and meconium peritonitis can lead to peritoneal fluid, as can rupture of an obstructed bladder or ureter. |
|

A 29-year-old woman who by examination is small for gestational age.
|
Oligohydramnios: The appearance is characteristic for
oligohydramnios with little else to consider. The real issue is the cause of the oligohydramnios. • Abdominal pregnancy: One feature of a rare abdominal pregnancy is the lack of amniotic fluid. This is variable and can be simply a manifestation of the unusual distribution of amniotic fluid. More typically, the fetus is in an extended position and the fetal limbs are spread rather than crowded. The diagnosis in this condition is made by tracing the myometrium from the cervix. + DIAGNOSIS: Oligohydramnios from premature rupture of membranes, not clinically suspected. + KEY FACTS CLINICAL • Fetal renal function becomes the primary determinant of amniotic fluid volume at about the eighteenth week of pregnancy. • Normal amniotic fluid volume increases steadily until about 32 to 34 weeks of pregnancy, then decreases slightly until 42 weeks, then decreases more rapidly. • The normal variability of amniotic fluid volume at any gestational age is high. |
|

A 29-year-old pregnant woman referred for a routine fetal ultrasound.
|
Chiari II malformation: This is by far the most likely
diagnosis. False-positive "lemon" signs occur with some frequency, but false-positive "banana" signs have not been reported. • Meningocele: This is the likely reason for the small echogenic focus at the distal spine, but a skin lesion such as a hemangioma could have a similar appearance. • Sacrococcygeal teratomas: These may occur in the distal spine, but they are not so directly posterior because they originate anterior to the spine. Furthermore, they tend to be much larger. + DIAGNOSIS: Chiari I I malformation with small sacral meningocele. + KEY FACTS CLINICAL • Chiari II malformation is characterized by a small posterior fossa with downward displacement of the brainstem, resulting in protrusion of the tonsils and vermis below the cisterna magna. • Secondary features seen prenatally include meningocele or encephalocele in about 90% of cases and partial or complete absence of the corpus callosum in about 40% of cases. • Hydrocephalus is commonly seen by sonography as the first indication of Chiari II, but it is not always present early as in this case. |
|

A 5 1 -year-old woman presents to the emergency room with weight loss, loss of
appetite, and vague abdominal pain. |
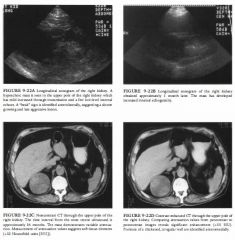
Dilated intrahepatic bile ducts: These have a relatively
specific pattern. On occasion, very large hepatic arteries can produce a similar appearance . This is sometimes seen with alcoholic cirrhosis or portal hypertension. Color Doppler imaging is useful for excluding this unusual possibility. Compared to portal veins, bile ducts may demonstrate posterior acoustical enhancement because bile is noncellular and not moving. • A mass in the head of the pancreas: This could be associated with either pancreatitis (acute or chronic) or carcinoma of the pancreas. • A single calcification of the pancreas: This diagnosis is not helpful. Multiple calcifications, especially in the pancreatic ducts, are strongly suggestive of chronic pancreatitis. Microcystic adenomas of the pancreas often contain calcifications, but many other pancreatic tumors, including islet cell tumors, may also calcify. +DIAGNOSIS: Pancreatic abscess in a patient with recurrent and chronic pancreatitis. +KBY FACTS CLINICAL • Pancreatic lithiasis occurs in 20% to 40% of patients with chronic pancreatitis and is highly associated with alcohol-induced pancreatitis. These are true stones lying within the ductal system of the pancreas. • Calcification of the mass is rare in ductal adenocarcinoma, but calcifications in the pancreas may occur in as many as 25% of patients. |
|
A 35-year-old woman presents with vague right upper quadrant pain.
|
Gallstone: A gallstone is unlikely because the abnormality
is adherent to the wall and nonmobile, and because of the absence of posterior acoustical shadowing. • Cholesterol polyp: These polyps are common intraluminal masses that are most often multiple. The polyps tend to be small, usually <5 mm in size, and almost always < 1 cm in size. They are not associated with acoustical shadowing. • Adenoma or papilloma: These lesions are almost always singular and are much less common than cholesterol polyps. These masses can be sessile and broad based (adenomas) or pedunculated and lobulated (papillary adenomas) . Masses are usually <l cm. • Primary gallbladder carcinoma: Carcinomas are most often seen as a large, solid mass replacing the gallbladder in the gallbladder fossa. Occasionally, in earlier stages focal intraluminal masses are seen, but these are usually > 1 cm in size. Associated findings include wall calcification, biliary duct dilatation, gallstones (80%), and evidence for metastatic spread, particularly to the liver. • Tumefactive sludge: This echo genic bile is not usually adherent to the wall but rather shifts location as the patient is repositioned. + DIAGNOSIS: Cholesterol polyp. + KEY FACTS CLINICAL • Cholesterolosis results from the accumulation of cholesterol within the wall of the gallbladder. This accumulation can either be diffuse or polypoid. |
|

A 53-year-old man presents with acute abdominal pain and vomiting.
|
• Normal appendix: The normal appendix should have
a diameter of 5 to 6 mm and should be compressible. In addition, there should be no evidence of inflammatory changes in the periappendiceal fat. • Crohn's disease: Hypoechoic, uniform thickening of the bowel wall in the terminal ileum would surround compressed echogenic mucosa centrally. Furthermore, the terminal ileum would not have a blind end. • Appendicitis: This is the best diagnosis for a rigid tubular structure located in the right lower quadrant at the site of maximal tenderness. The diameter measurement from the outer wall to the outer wall of the structure exceeds 6 mm. The structure is noncompressible and blind-ended. On the longitudinal view, a region of increased echogenicity surrounding the appendix suggests inflammation in the periappendiceal fat. • Mesenteric adenitis: With this disease process, enlarged lymph nodes and mural thickening of the terminal ileum will be evident. Peristalsis should also be present in the terminal ileum. Inflamed lymph nodes would be unlikely to have such a smooth tubular contour, or the layering of hyperechoic and hypoechoic strata that constitute the gut signature . • Pelvic inflammatory disease (PID): Though PID is a possible pitfall, fmdings should be located more in the pelvis than the right lower quadrant. A hydrosalpinx would not have the same echopattern as the bowel. |
|

A 32-year-old pregnant woman presents with a discrepancy in her size and dates.
|
Monoamniotic, monochorionic twinning: When
no separating membrane is seen, the possibility that the twins occupy the same amniotic sac must be considered. In this case, the separating membrane can be seen, although it closely covers portions of twin B . • Twin transfusion syndrome: This condition usually results in a small, anemic twin and a hydropic cotwin . Severe fluid discrepancies can occur, as in this case . • Stuck twin phenomenon: The phenomenon results from severe fluid discrepancy between twins in different gestational sacs. The stuck twin is rendered immobile within its oligohydramniotic sac. • DIAGNOSIS: Stuck twin phenomenon. KEY FACTS CLINICAL • The stuck twin phenomenon results when there is a severe amniotic fluid discrepancy between the two gestational sacs. The fetus in the severely oligohydramniotic sac appears attached to the uterine wall and will not change location with patient repositioning. Moreover, this twin's movements are restricted. • The co-twin is frequendy seen in a polyhydramniotic sac. • Frequently there is a discrepancy in fetal growth . • The stuck twin phenomenon may be a consequence of the twin transfusion syndrome, but dle transfusion syndrome is not a necessary precondition. • Both twins have a poor prognosis. Most pregnancies result in the deadl of both fetuses. Presentation after 26 weeks, however, has been associated witl1 inlproved survival . |
|
A 26-year-old woman presents for routine obstetric ultrasound.
|
Cystic adenomatoid malformation: This entity is
typically seen as multiple large cysts or an echogenic mass. Occasionally it can occur with a diaphragmatic hernia. • Congenital diaphragmatic hernia ( CDH): A hernia of this type is a likely possibility given the displacement of the stomach into the chest and the apparent discontinuity of the hypoechoic diaphragm. • Bronchogenic and esophageal duplication cyst: It is possible that the fluid-filled structure in the left chest could be a foregut abnormality; however, the stomach is not present in its expected location. • Cystic teratoma: These are typically complex masses with cystic and solid components arising in the mediastinum. • Eventration of the diaphragm: It is difficult to exclude eventration with certainty considering how difficult it is to demonstrate the full contour of the diaphragm in the normal fetus. DIAGNOSIS: Congenital diaphragmatic hernia. KEY FACTS CLINICAL • Herniation of bowel or solid organs can occur through defects in the diaphragm that form from incomplete closure during embryologic development. Most are Bochdalek defects, which occur posteriorly, usually on the left side. • Bowel herniating through the left-sided defect will cause displacement of thoracic structures, particularly the heart, to the right. • When hernias occur on the right side, the liver may be involved. • Patients sometimes present because their fundal size is greater than their dates. This results when there is associated polyhydramnios, which most often develops in the third trimester. |
|

A 28-year-old woman has vaginal bleeding and a positive beta-human chorionic
gonadotropin ( B-HCG) level. |
The differential diagnosis includes conditions found in
patients with a positive serum HCG but no ultrasound evidence of an intrauterine pregnancy: • Early intrauterine pregnancy: This is unlikely because there are abnormal findings in both the adnexa and the cul-de-sac. • Spontaneous abortion: Tlus condition is also unlikely because of the abnormalities in the adnexa and the cul-de-sac. • Gestational trophoblastic disease: This disease is unlikely because the endometrial stripe is normal. There is no evidence of an echo genic intrauterine mass with multiple internal cysts, the finding usually seen in patients with gestational trophoblastic disease. • Ectopic pregnancy: This is the best diagnosis because demonstration of an "adnexal ring sign" in conjunction with sonographicaliy demonstrable hemoperitoneum is highly suggestive of ectopic pregnancy in a patient with a positive HCG and no intrauterine pregnancy. DIAGNOSIS: Left ectopic pregnancy. KEY FACTS CLINICAL • The spectrum of clinical symptoms ranges from pelvic pain and vaginal bleeding (often clinically indistinguishable from spontaneous abortion) to catastrophic intra-abdominal hemorrhage . • A HCG is necessary to interpret the ultrasound findings: a negative serum HCG effectively excludes an ectopic pregnancy. • The "classic clinical triad" suggesting ectopic pregnancy is amenorrhea, pain, and palpable adnexal mass. This triad, however, is often not present. • All women with positive HCG should be considered at risk for ectopic pregnancy. The following groups are at especially high risk: history of pelvic inflammatory disease, intrauterine contraceptive device, prior ectopic pregnancy, tubal reconstructive surgery, prior tubal ligation, or in vitro fertilization. • A nlinority of patients with ectopic pregnancy are critically ill and hemodynanlically unstable due to massive intra-abdominal hemorrhage . They require rapid fluid resuscitation and immediate laparotomy, and there may be no time for ultrasound imaging in this group. |
|

A 38-year-old pregnant woman presents with third-trimester bleeding.
|
Placenta previa should be considered whenever placental tissue overlies the region of the cervix at ultrasonography. False-positive diagnoses of placenta previa are common and must be considered prior to making a definitive diagnosis.
• False-positive due to distended urinary bladder: This is unlikely, because the bladder does not appear distended on the ultrasound images. • False-positive due to uterine contraction: A contraction is unlikely because there is no evidence of a lower uterine contraction on either of the images. A uterine contraction might be associated with an elongated cervix that is distorted in its overall appearance . The cervix in this patient is normal in length and configuration. • Subchorionic hematoma overlying the cervix: This condition would be possible if the hematoma were imaged in an acute stage, because the sonographic pattern of an acute hematoma can be remarkably similar to that of placental tissue. It may be possible to appreciate a subtle difference in the echo pattern of the hematoma versus the echo pattern of placental tissue. At times, the distinction is only made at the time of fo llow-up sonography because a subchorionic hematoma will show evolution in its appearance. • Fibroid overlying cervix: Such a fibroid is unlikely because the tissue overlying the cervix is continuous with placental tissue and does not have a sonographic pattern typical fo r a leiomyoma. • Complete placenta previa: This is the best diagnosis because placental tissue completely overlies the internal os. DIAGNOSIS: Complete placenta previa. KEY FA CTS CLINICAL • Painless vaginal bleeding is the clinical hallmark of placenta previa. Bleeding most commonly occurs in the third trimester but can also occur during the second trimester. • Va ginal delivery can result in disastrous complications, including either or both maternal and fe tal death due to massive bleeding. • A cesarean section is required in patients with complete placenta previa. Some patients with milder degrees of placenta previa can deliver vaginally. • There is a high association between placenta previa and abnormalities of placental attachmen t, such as placenta accreta, increta, and percreta. Cesarean hysterectomy may be necessary in some patients with these disorders. RADIOLOGIC • Ultrasound is the imaging method of choice fo r placental localization. • It is necessary to see both the lower edge of the placenta and the cervix to assess placenta previa accurately. Visualization of just the lower edge of the placenta excludes a placenta previa due to tlle main mass of the placenta but does not exclude an accessory lobe of the placenta overlying the cervix. • Ultrasound fo r placenta previa should be done witll an empty urinary bladder. If tlle bladder is full and ultrasound suggests placenta previa, scanning should be repeated after voiding. • If the cervix cannot be seen using a transabdominal approach, alternate methods such as transperineal or endovaginal scanning can be attempted. In most cases, endovaginal scanning can be avoided by using transperineal scanning. If endovaginal scanning is done, it should be performed with caution, because bleeding is a well-recognized complication of manual examination of the cervix in patients with placenta previa. Nevertheless, a substantial risk fr om endovaginal imaging has not been documented in patients with placenta previa |
|

A 38-year-old woman referred for obstetric ultrasound at 27 menstrual weeks.
|
The "double bubble" sign implies duodenal obstruction,
but it must be distinguished from other sources of extra cysts in the fetal abdomen. • Normal stomach, imaged twice due to oblique scan plane: This is not simply a normal stomach because Figure 9- 1 2 B demonstrates a configuration consistent with the gastric antrum and pylorus emptying into a dilated duodenal bulb. • Splenic cyst: This would be unlikely because the extra cyst is located in the right, not the left upper quadrant. • Bowel duplication cyst: This is a possibility except that the extra cyst is in an ideal location for a dilated duodenal bulb. • Choledochal cyst: This entity would be consistent with the appearance in Figure 9 - 1 2A, as the location of the second cyst is appropriate for a choledochal cyst. However, it is not consistent with Figure 9 - 1 2 B because o f the connection between the stomach and the second cyst. A choledochal cyst would not connect to the fetal stomach. • Renal cyst: Because of the location of the extra cyst, a renal cyst would be unlikely. • Dilated duodenal bulb owing to duodenal atresia: This is the likely diagnosis based on the appearance and location of the two abdominal cysts, in conjunction with sonographic demonstration of fetal stomach emptying into dilated duodenal bulb. At real-time evaluation, peristalsis was observed, further confirming a bowel etiology. DIAGNOSIS: Duodenal atresia. KEY FACTS CLINICAL • Duodenal atresia is the most common type of congenital small bowel obstruction . • The likely etiology is failme to recanalize the duodenal lumen during the tenth to eleventh week of gestation. • There is a high incidence of associated anomalies in fetuses with duodenal atresia. These include esophageal atresia, congenital heart disease, imperforate anus, other small bowel atresias, biliary atresia, renal anomalies, and vertebral anomalies. • Because 20% to 30% of fetuses with duodenal atresia also have trisomy 2 1 , chromosomal analysis should be offered when duodenal atresia is suspected. RADIOLOGIC • The fluid-filled double bubble sign seen in utero is analogous to the gas-filled double bubble sign seen on postpartum radiographs of infants with duodenal atresia. • The bubbles comprising the double bubble sign consist of an overdistended stomach in the left upper quadrant and a dilated duodenal bulb in the right upper quadrant. • Polyhydramnios is common . • The double bubble sign is not specific for duodenal atresia but can occur secondary to any obstructive process at the level of the duodenum. Among the other possible causes are annular pancreas, duodenal web, duodenal stenosis, and obstruction due to an intestinal duplication. • Many fetuses with duodenal atresia have a completely normal ultrasound, without polyhydramnios or the double bubble sign, until the late second or early third trimester. |
|
A 55-year-old woman presents with a palpable pulsatile abdominal mass.
|
Adenopathy/lymphoma: Patients with lymphoma
and retroperitoneal or mesenteric adenopathy could present with the soft-tissue mass seen in but i t would not b e expected to have the configuration seen laterally on Figure 9- 1 3C . • Other primary retroperitoneal neoplasm: Again, tIus could explain the configuration in Figure 9- 1 3B but not the configuration in Figure 9 - 1 3C. • Retroperitoneal fibrosis: This is likely to be more circumferential than the soft-tissue mass shown in It does not explain the configuration in Figure 9 - 1 3C. • Horseshoe kidney: This is the best diagnosis. The soft-tissue mass seen anterior to the aorta corresponds to the isthmus of a horseshoe kidney. The explanation for the palpable pulsatile abdominal mass at physical examination is pulsations transmitted from the aorta to the isthmus of the horseshoe kidney. DIAGNOSIS: Horseshoe kidney. KEY FACTS CLINICAL • The horseshoe kidney is a congenital renal fusion anomaly, in which the lower poles of both kidneys are joined by a fibrous or parenchymal band. • Horseshoe kidneys are a common entity, occurring in between 1 in 400 to 500 births. • Horseshoe kidneys are more susceptible to trauma compared to normally located kidneys. • Due to urinary stasis from draping of the ureters over the kidneys, there is an increased incidence of stones and infection. • Multiple renal arteries and ectopic renal arteries are common. • Patients with a horseshoe kidney are not uncommonly referred to ultrasound for evaluation of a pulsatile abdominal mass, as in tIlls case. RADIOLOGIC • Abnormal renal orientation is common in patients with horseshoe kidney. The renal pelvis is frequently directed more anteriorly than usual. • The horseshoe kidney is typically found in a relatively low position, eitl1er in the lower abdomen or the upper pelvis. A possible explanation for the low position of the horseshoe kidney is that normal ascent of the kidney is prevented by the inferior mesenteric artery. • The fused lower renal poles are commonly found at the level of the L4-L5 vertebrae. • At sonography, a soft-tissue mass may be seen anterior to the abdominal aorta. The lower poles of the kidneys can sometimes be followed into the mass by scanning in an oblique plane. The upper portions of the kidneys are not usually in their typical locations in the flanks but are relatively low in position . • In many cases, the isthmus of parenchymal or fibrous tissue connecting the two sides of the horseshoe kidney cannot be seen by ultrasound, due to overlying bowel gas. When this occurs, sonography may miss the diagnosis |
|
A 39-year-old man presents with a 2-year history of back pain and a bone scan
that shows left renal obstruction. Physical exam demonstrates a questionable left testicular mass. |
DIFFERENTIAL DIAGNOSIS
• Lymphoma: Non-Hodgkin's lymphoma is a possibility because of the large hypoechoic retroperitoneal mass and a focal testicular mass. However, the majority of malignant lymphomas manifest as diffuse testicular involvement with enlargement of the testis. • Metastatic disease: Nonlymphomatous metastases to the testis are uncommon, representing no more than 5% of all testicular neoplasms. The most frequent primary sites are the lung and prostate . Metastases are most common during the fifth and sixth decades and are more frequent than primary germ cell tumors after age 50. Metastatic lesions are commonly multiple and are bilateral in 1 5% of cases. • Primary testicular neoplasm: This is the best diagnosis from the standpoints of so no graphic fmdings and clinical likelihood. • Infarction: Testicular infarction may appear as either a focal hypoechoic mass or a diffusely hypoechoic testis of normal size. However, color Doppler would not be expected to show increased flow in the area of an infarct and the gland should not be enlarged. • Sarcoidosis: Genital involvement is uncommon, occurring in l % of patients with systemic sarcoidosis. Differentiation from a neoplasm is difficult. Occasionally, calcific foci with acoustic shadowing may be seen. DIAGNOSIS: Testicular seminoma with rare elements of choriocarcinoma metastatic to the retroperitoneum. KEY FACTS CLINICAL • Seminoma is the most common single-cell-type testicular neoplasm in adults, accounting for 40% to 50% of germ cell neoplasms. • Seminomas are more common in the slightly older age group, demonstrating a peak incidence in tlle fourth and fifth decades. They are less aggressive than other germ cell tumors, although 25% of patients will have metastases at tlle time of diagnosis. • Seminomas are relatively radiotherapy and chemotherapy sensitive. • Seminomas are the most common tumors to originate in cryptorchid testes. An increased risk of developing a seminoma remains even after orcheopexy. • Mixed germ cell tumors are the second most common testicular malignancy after seminoma, constituting 40% of all germ cell neoplasms. • Choriocarcinoma is a rare germ cell tumor. However, 2 3% of mixed germ cell tumors contain some small component of choriocarcinoma. • Choriocarcinomas secrete circulating chorionic gonadotropins and may produce gynecomastia. RADIOLOGIC • Seminomas are characteristically homogeneous, round or oval in shape, and hypoechoic. • Sonographic features of seminomas parallel their relatively homogeneous histologic features. • Seminomas may appear to be relatively well encapsulated or may be poorly marginated. They may be isolated or involve the entire testicle. • Virtually all hypoechoic, focal solid testicular masses should be considered potential neoplasms unless there is compelling clinical evidence to the contrary. • Color Doppler ultrasound carmot distinguish focal neoplasms from inflammatory lesions. However, color Doppler may be helpful in depicting subtle infiltrative lesions. Furthermore, the absence of power and color Doppler flow in a large hypoechoic mass using optimized flow settings is suggestive of an infarct. |
|
A 62-year-old man presents with a pulsatile mass and bruit in the right groin 2
days after coronary angioplasty via the right femoral artery. |
DIFFERENTIAL DIAGNOSIS
• Arterial stenosis: A stenosis of the femoral artery could cause increased diastolic flow, loss of high resistance, arterial waveform, and color Doppler bruit, but it should not alter the venous waveforms. • Arterial dissection: A dissection or flap may have features similar to atherosclerotic narrowing, but no venous waveform changes should occur. • Venous stenosis: A narrowed and stenotic vein may cause high-velocity venous flow, but no arterial changes. • Arteriovenous fistula (AVF): This is the best diagnosis because it explains both the arterial and venous waveform changes. + DIAGNOSIS: Femoral arteriovenous fistula. + KEY FACTS CLINICAL • An AVF resulting from arterial puncture and catheterization is a less common complication than a pseudoaneurysm. • An AVF is an abnormal communication between the arterial and venous systems that creates a shunt from the high-resistance arterial system into the low-resistance venous system. • An AVF is caused by simultaneous pW1Cture of the adjacent artery and vein and by simultaneous arterial and venous catheterization . • An AVF is manifest clinically by a continous bruit or thrill in the region of trauma. • An AVF may be asymptomatic or can produce localized symptoms, including pain, claudication distal to the A VF secondary to decreased arterial flow, and venous stasis due to increased venous pressure. Systemic symptoms such as high-output congestive heart failure and angina may also result. 499 • An asymptomatic AVF does not require treatment and may resolve spontaneously. • Surgical treatment or ultrasound-guided compression/ repair may be necessary. • An AVF may coexist with a postcatheterization pseudoaneurysm. RADIOLOGIC • The classic arterial pattern is high diastolic flow (a low resistance waveform) with spectral broadening just proximal to the fistula. • The classic venous pattern is increased flow velocity with pulsatile disturbed waveforms near the fistula. • Color Doppler signal in the soft tissues surrounding the AVF is caused by the transmitted thrill from disturbed flow. • A visible tract of flow connecting the artery and vein may be seen, especially with color Doppler. • There is often decreased arterial flow distal to the fistula. • Some AVFs may not demonstrate all of these features. |
|

A 62-year-old man presents with a pulsatile right groin mass 24 hours after coronary
angioplasty via the right femoral artery. |
Postcatheterization hematoma: Hematomas in the
region of a puncture site can produce an anechoic or hypoechoic mass. This mass may contain flecks of color due to transmitted pulsations from the adjacent femoral artery. However, pulsed Doppler evaluation will not reveal a "to-and-fro" arterial waveform. • Arteriovenous fistula (AVF): The localized intense soft-tissue bruit associated with an AVF may sometimes mimic this color Doppler flow pattern. However, the pulsed Doppler waveforms within the adjacent artery and vein should demonstrate characteristics consistent with an AVF . • Hyperplastic lymph nodes: The increased flow i n hyperplastic lymph nodes can produce a very vascular mass on color Doppler ultrasound. However, no neck connecting the hyperplastic lymph node to the femoral artery will be observed, and the flow within the node will not have a "yin-yang" appearance . • Inguinal hernia: Particulate material within ascites in an inguinal hernia sac may produce a similar swirling color flow pattern. Pulsed Doppler evaluation will show that these swirling color changes are associated with transmitted motion from respiration and abdominal peristaltic activity rather than vascular pulsations. • Arterial pseudoaneurysm: This is the best diagnosis considering the pulsatile swirling blood flow in the mass and the waveform in the "neck" cOlmecting the artery to the pseudoaneurysm. DIAGNOSIS: Femoral artery pseudoaneurysm with successful ultrasound-guided compression repair. KEY FACTS CLINICAL • A femoral artery pseudoaneurysm is an increasingly common complication of therapeutic catheterization procedures, including percutaneous transluminal coronary angioplasty and stenting. • Occurrence rates as high as 6% have been reported. Pseudo aneurysms can produce complications including hemorrhage, pain, neuropathy, infection, local skin ischemia, peripheral embolization, and even frank rupture leading to exsanguination. • Factors that lead to pseudoaneurysm development include large catheters and sheaths, use of anticoagulant or thrombolytic agents during and following the procedure, simultaneous arterial and venous catheterizations, and suboptimal postprocedural compression. • Pcudoal uryms arc flat true aneurysms. They develop a fibrous capsule but do not have a complete arterial wall surrounding them. • Pseudoaneurysms present as pulsatile masses near the arterial puncture site. Audible systolic bruits are frequently heard but are not always present. • Pseudoaneurysms must be distinguished from overlying hematomas with transmitted pulsations. • Pseudoaneurysms may coexist with AVFs. • Although the natural history of pseudo aneurysms is variable, spontaneous tl1Tombosis is common. Unfortunately, tllere is no way of discerning which pseudoaneurysms will thrombose based on their ultrasowld appearance. • Traditional therapy for pseudoaneurysms has been surgical intervention . However, many pseudoaneurysms thrombose spontaneously. Furthermore, nonsurgical ultrasound-guided compression repair ( UGCR) has been found to be a very successful interventional technique. • UGCR is slightly more effective in nonanticoagulated patients; however, successful repair can be achieved in patients with anticoagulation. Reversal of anticoagulation before UGCR is nevertheless recommended. The age of the pseudoaneurysm does not appear to affect the ability to compress and tl1rombose the lesion adequately. • Contraindications to UCGR include overlying skin ischemia or skin infection, peripheral vascular compromise, location of tlle pseudoaneurysm above the inguinal ligament, and inability to compress tlle pseudoaneurysm without simultaneous occlusion of the underlying artery. • Complications of UCGR are uncommon; they include arterial occlusion, peripheral embolization, pseudoaneurysm rupture, and thrombosis of the adjacent common femoral vein. |
|

A 67-year-old woman presents with a history of intermittent left upper extremity
weakness and numbness. On physical examination there is a right carotid bruit. |
• Carotid dissection: Dissections are less common than
atherosclerotic plaque in the seventh decade. However, dissections should be considered as a cause of carotid stenosis or occlusion in YOlmger patients, particularly those with a history of traW1la, and in those with no atherosclerotic risk factors and a relative paucity of visible plaque. • Carotid stenosis: This is the best diagnosis considering the age of the patient, the intraluminal lesions, and the focal velocity elevation. • Spurious velocity elevations due to contralateral stenosis: Collateral shunting of blood to the circle of Willis on the side opposite a high-grade carotid stenosis can result in spuriously elevated velocities disproportionate to the amount of visible vessel narrowing. In this case, there was no evidence for a contralateral lesion, and the color Doppler clearly shows a large intraluminal filling defect associated with the areas of high velocity in the internal carotid artery. • Suboptimal Doppler angle: If the angle theta used to obtain velocity values exceeds 70 degrees, spurious results may be obtained that are not representative of true flow velocity. In this case, the Doppler angle theta is 60 degrees, which is an acceptable Doppler angle. Ideally, the Doppler angle should not exceed 60 degrees. DIAGNOSIS: <90% diameter stenosis of the proximal internal carotid artery with plaque ulceration. KEY FACTS CLINICAL • Stroke caused by atherosclerotic disease is the third leading cause of death in the United States. • Approxinlately 50% of these strokes are caused by atherosclerotic disease located within 2 cm of the carotid bifurcation . • Carotid sonography using duplex ultrasound has become a valuable, noninvasive screening technique to determine which patients have potentially "operable" lesions. • Carotid endarterectomy is now thought to be highly beneficial for symptomatic patients who have a 70% to 99% diameter stenosis involving the internal carotid artery. • Ongoing investigations suggest that patients with an asymptomatic >80% diameter stenosis who are scheduled to undergo cardiopulmonary bypass may also derive benefit from endarterectomy. • Other ongoing research suggests that endarterectomy may be of benefit for asymptomatic patients with a >60% diameter internal carotid artery stenosis. • Ultrasound screening allows selection of appropriate patients for angiography before surgery. There are some instances in which surgery can be performed without angiography. RADIOLOGIC • Pulsed Doppler spectral analysis and color Doppler ultrasound are approximately of equal accuracy for diagnosing >50% diameter stenoses ( >90% accuracy) . • The hallmark of a high-grade stenosis is a progressive increase in peak systolic and end diastolic velocities beginning at approximately 50% diameter stenosis and continuing until one reaches a preocclusive stenosis ( >95% diameter), at which time the peak systolic and end diastolic velocities decrease precipitously. • Peak systolic velocities >225 to 250 cm/sec are usually associated with a >70% diameter stenosis. End diastolic velocities >80 cm/sec are usually associated with the same degree of stenosis. Velocity ratios comparing the peak systolic or peak end diastolic velocities in the internal carotid artery in the region of the stenosis versus those in the more proximal common carotid artery may also be of value. • Color Doppler ultrasound allows one to display blood flow information in real time over a selected area. Stationary soft-tissue structures that lack phase or frequency shifts associated with flowing blood receive an amplitude gray scale value, while the flowing blood in the vessels receives a color assignment dependent on the direction of blood flow relative to the Doppler transducer, as well as the Doppler angle and the velocity of the flowing blood. • Color Doppler is helpful as an initial screen during the carotid examination to pinpoint areas of vascular narrowing and abnormal flow for subsequent pulsed Doppler interrogation . • Carotid plaque characterization is a controversial topic; however, plaque such as the one seen in this case, which is heterogeneous and hypo echoic and contains areas of low velocity disturbed flow within the plaque, is frequently associated with ulceration. • With an extremely high-grade stenosis or occlusion of the internal carotid artery, flow in the proximal common carotid artery may become damped with relatively low peak systolic and end diastolic velocity readings. |
|

A 26-year-old woman referred for fetal ultrasound because of uncertainty
about her dates. |
DIFFERENTIAL DIAGNOSIS
• "Hourglass membranes": This term refers to the presence of fluid in the upper vagina as a result of herniation of the amniotic membranes through the cervix. The sonographic finding is characteristic, and few conditions mimic this appearance. The important thing to recognize is the location of the uterine cervix. • Nabothian cyst: A very large nabothian cyst can have a similar appearance. In this case, the cervix is normal . DIAGNOSIS: Incompetent cervix with herniation of the amnion into the upper vagina, often referred to as "hourglass membranes." KEY FACTS CLINICAL • Preterm labor continues to be a major cause of perinatal death and morbidity. • The patients are often without symptoms and do not have a history of premature delivery. • There is no universally accepted treatment for this condition once it has progressed to this point. Various regimens have been suggested including: ( 1 ) doing nothing, ( 2 ) bed rest in the Trendelenburg position with tocolytic agents, and ( 3 ) cerclage for some patients. RADIOLOGIC • Routine images should be obtained of the cervix from 1 5 to 30 weeks of gestation. Ideally, these are done with an empty bladder. Often the transabdominal approach is adequate, but transperineal and endovaginal imaging may be needed in some cases. It is wise to examine the patient with a transabdominal scan before any endovaginal imaging to exclude the possibility of hourglass membranes. • The normal cervix is about as high as it is wide. Measurements are taken of the length of the endocervical canal from the internal to the external os. This length should exceed 3 cm up to about 30 weeks. • The normal endocervical canal can be hypoechoic or echogenic. A hypoechoic endocervical canal should not be mistaken for cervical incompetence. • Myometrial contractions can give the appearance of an elongated endocervical canal. Measurements of the length of the endocervical canal should not be taken when a contraction distorts this area. • The cervix can change in length during the course of an examination . Generally, the shortest measurement is most representative of the true clinical state. Also, "funneling" of the cervix is sometimes intermittent. The clinical consequences of intermittent fulmeling are the same in a cervix that consistently remains funneled- that is, there is a significant increase in risk for preterm labor and delivery of a premature infant. |
|
A 47-year-old man presents with intermittent episodes of right flank discomfort.
|
DIFFERENTIAL DIAGNOSIS
• Adrenal hemorrhage: Acute hemorrhage could cause a mass of markedly increased echogenicity, but it would not result in the apparent discontinuity and posterior displacement of the diaphragm behind the mass. • Renal angiomyolipoma: This hamartomatous mass is possible, although it appears more suprarenal rather than originating from the kidney. • Retroperitoneal fat-containing mass such as a liposarcoma: It would be unlikely for anatomic fat to be as well defined as this mass or be localized solely to the suprarenal area. • Adrenal myelolipoma: This is the most likely diagnosis because the apparent discontinuity and posterior displacement of the diaphragm is due to a "speed propagation artifact. " This occurs because the speed of ultrasound is slower in fatty masses than in many other soft tissues, resulting in misregistration of the location and apparent posterior displacement of the diaphragm immediately behind the fatty mass. • Adrenal carcinoma with acute hemorrhage: This could result in an echogenic mass in a suprarenal location, but it would be unlikely to cause discontinuity and posterior displacement of the diaphragm behind the mass. DIAGNOSIS: Adrenal myelolipoma. KEY FACTS CLINICAL • An adrenal myelolipoma is an uncommon, benign, nonfunctioning hamartomatous adrenal mass that contains both fatty and bone marrow elements. • Many patients with adrenal myelolipomas are asymptomatic, but some present with pain or discomfort. Discomfort can be secondary to hemorrhage, necrosis, or pressure on surrolll1ding structures. • They are most common in the fourth to sixth decades of life, and they occur with approximately equal frequency in men and women. • These lesions span a variety of sizes, ranging from microscopic to 30 cm or more in diameter. RADIOLOGIC • The ultrasound appearance depends on the relative quantities of the various tissue components. • Many myelolipomas are markedly echogenic on ultrasound. This is considered the most characteristic appearance and is more likely to be seen when there is a high fat content. • If the fat content is relatively low, a hypoechoic or heterogeneous mass may result. • In some cases the "speed propagation artifact" is subtle, seen only in certain scan planes, or not seen at all. Inability to demonstrate this particular artifact does not exclude an adrenal myelolipoma. • Even in the presence of a "speed propagation artifact," tlle diagnosis should be confirmed with a CT scan. The CT can confirm the presence of both fatty components as well as the adrenal origin of tlle mass. • Adjacent retroperitoneal fat may mask a small adrenal myelolipoma. SUGGESTED READING Musante F, Derchi LE, Zappasodi F, et al . Myelolipoma of the adrenal gland: Sonographic and CT features. AJR Am J Roentgenol 1988 ; 1 5 1 :961-964. Vick CW, Zeman RK, Malmes E, et al. Adrenal myelolipoma: CT and ultrasound findings. Urol Radiol 1984;6:7- 1 3 . |
|

A 32-year-old pregnant woman has an elevated serum alpha-fetoprotein.
|
The differential diagnosis includes congenital malformations characterized by absence or decreased prominence of the calvarium:
• Amniotic band syndrome: This diagnosis is possible but unlikely because there is no evidence of intrauterine membranes. Additionally, the loss of the cranial vault is complete and symmetric, as opposed to amniotic band syndrome in which it is typically incomplete and asymmetric. Finally, additional lesions characteristic of amniotic band syndrome such as amputated limbs and atypical abdominal wall defects are not seen. • Severe microcephaly: It could resemble this case if the calvarium is not recognized because of its diminutive size. Microcephaly is unlikely, however, because the images demonstrate complete absence of the calvarium, rather than a small calvarium. • Exencephaly: Absence of the calvarium is consistent with exencephaly, but a larger amount of abnormally developed brain tissue would be seen in exencephaly. • Osteogenesis imperfecta: This is a consideration because it is associated with marked undermineralizationof the cranium. It is unlikely, however, because the underlying brain tissue would be normal in quantity and have a normal sonographic pattern. • Anencephaly: This is the best diagnosis because of the combination of complete symmetric absence of the calvarium in conjunction with absence of normal brain tissue above the level of the orbits. DIAGNOSIS: Anencephaly. KEY FACTS CLINICAL • Anencephaly is a neural tube defect characterized by absence of the fetal cranium and cerebral hemispheres. • Despite the implications of literal translation of the term anencephaly, there is not a complete absence of brain and head. Functioning neural tissue and calvarial structures are almost always present at the base of the skull . • The disorder is uniformly fatal. Most affected infants die in utero or within a few days of birth. • Anencephaly is often associated with additional defects, including spine anomalies, facial clefts, cardiovascular anomalies, and urinary tract malformations. 509 • After birth of one fetus with a neural tube defect, the risk of recurrence in a subsequent pregnancy is approximately 3% to 5%. RADIOLOGIC • Ultrasound changes in anencephaly are dramatic, so the detection rate approaches 1 00% by the early second trimester. • If the fetal head is low in the pelvis, directly abutting the uterine wall or cervix, the diagnosis may not be immediately obvious by transabdominal sonography. In such a case, the abnormality should still be perceived when the examiner is unable to obtain a biparietal diameter in the conventional scan plane. Endovaginal or transperineal sonography can then be used to confirm the diagnosis. • The combination of lack of cranial vault and of normal brain tissue above the level of the orbits results in a fetal head pattern that has been termed "frog-like ." • Identification of disorganized soft tissue above the level of the orbits does not exclude anencephaly. Such soft tissue is frequently seen due to the presence of angiomatous stroma. It tends to be most prominent when anencephaly is detected early in the pregnancy. • Though additional anomalies occur in up to 50% of affected fetuses, detection of these lesions is not usually considered a critical component of the ultrasound study since anencephaly is uniformly fatal. • Polyhydramnios is identified in many but not all cases. • Exencephaly is considered an embryologic precursor to anencephaly. It is characterized by complete or partial absence of the calvarium, in association with a large amount of abnormally developed brain tissue. Absence of tlle calvarium in exencephaly is postulated to expose the brain to repeated trauma and anmiotic fluid, leading to evenhlal brain destrllction and anencephaly. |
|

A 57-year-old man presents with fever, abdominal pain, and vomiting
|
DIFFERENTIAL DIAGNOSIS
• Emphysematous cholecystitis: This is a good possibility because of the presence of brightly echogenic foci within the wall and within the lumen of the gallbladder. The acoustic noise and ring-down posterior to these foci suggests the presence of gas. • Porcelain gallbladder: The calcified wall in this condition would be expected to produce cleaner shadows without the reverberation artifacts seen in this case. • Gallbladder full of stones: The echogenic foci in tllis case appear to be located in the wall of the gallbladder itself. Intraluminal gallstones would be expected to be separated from the wall by a crescent of bile, thus producing the wall-echo-shadow sign. • Bowel gas: A loop of bowel can be displaced into the gallbladder fossa, especially after cholecystectomy. One would expect to fmd, however, the gut signature typical of bowel wall, and also continuity with an adjacent loop of bowel. DIAGNOSIS: Emphysematous cholecystitis. KEY FACTS CLINICAL • Emphysematous cholecystitis is an unusual variant of acute cholecystitis caused by gas-forming bacteria. • This is a particularly fulnlinant type of infection that is five times more likely to result in gallbladder perforation. • There is a male predilection (unlike more typical acute cholecystitis), and it is most often seen in the elderly. • There is a strong association with diabetes mellitus. • Patients often have a deceptively mild clinical presentation. RADIOLOGIC • Sonographic features of emphysematous cholecystitis depend on the relative amounts of intralunlinal and intramural gas. • Intraluminal gas is seen as an interface of highly reflective echoes. Posterior to this line, acoustic noise and ring-down reverberation are seen. • Intramural gas can be located within the thickened edematous gallbladder wall. This gas is often seen ;s a broken line of echoes (dots and dashes) that have distal reverberation artifacts. Occasionally, these echoes can be seen to float up to a non dependent portion of the gallbladder. This has been referred to as the effervescent gallbladder. • Because of the seriousness of the diagnosis, additional in1aging is indicated to confirm the suspicion of emphysematous cholecystitis. Plain film radiography, and especially CT, can confirm the presence of air. SUGGESTED READING Bloom RA, Libson E, Lebensart PD, et al. The ultrasowld spectrum of emphysematous cholecystitis. J Clin Ultrasound 1989; 1 7: 2 5 1 -256. Hunter ND, Macintosh PK. Acute emphysematous cholecystitis: An ultrasonic diagnosis. AJR Am J Roentgenol 1980; 1 34 : 592-593. emcek AA Jr, Gore RM, Vogclzang RL, Grant M . The effervescent gallbladder: A sonographic sign of emphysematous cholecystitis. AJR Am J Roentgenol 1988 ; 1 50: 575-577. Parulekar SG. Sonographic findings in acute emphysematous cholecystitis. Radiology 1 982;145 : 1 1 7- 1 1 9 . |
|
A 62-year-old man presents with abdominal pain.
|
• Simple renal cyst: The mass does not meet strict
sonographic criteria for a simple cyst, which must be anechoic, demonstrate increased through-transmission, and have a well-defined back wall. • Hemorrhagic or infected renal cyst: This is a possibility because of the predominantly cystic nature of tlle lesion, which has low-level internal echoes, only moderate wough-transmission, an imperceptible wall, and relatively smooth margination. • Renal abscess: This diagnosis is possible because of reduced through-transmission and internal echoes. The patient should have an elevated white blood cell count and localized flank pain. The ultrasound and CT appearance of an abscess does depend on me time at which it is studied, but usually more inflammatory changes are evident in both the kidney and me perinephric space. • Renal cell carcinoma: This is the most likely diagnosis because of the variable attenuation, areas of irregular wall thickening, and demonstration of significant contrast enhancement ( > 1 0 HU increase) . DIAGNOSIS: Renal cell carcinoma developing in the wall of a cyst. KEY FACTS CLINICAL • Renal cell carcinomas account for >90% of all cancers in me kidney. • The class triad of hematuria, abdominal mass, and pain is an uncommon presentation. Microhematuria is absent in up to 40% of cases. A more common presentation includes fever, malaise, anemia, weight loss, or a paraneoplastic process. Detection is frequently incidental. • These tumors are most frequent in the sixth and seventh decades, although recently an increased incidence in younger females and adolescents has been noted. The male-to-female ratio is approximately 2 to 1 . • Larger neoplasms ( > 1 0 cm) frequently are locally invasive or have metastasized at the time of diagnosis. Small neoplasms (:S:3 cm) uncommonly present with metastases. • Renal cell carcinoma commonly metastasizes to the lung, ipsilateral renal hilar lymph nodes, and paraaortic/ paracaval lymph nodes. There may also be direct extension to the perinephric and paranephric spaces. Invasion of the major renal veins and the inferior vena cava is common. Osseous metastases are usually lytic and expansile . RADIOLOGIC • A cystic mass is considered a simple cyst by ultrasound if it is: • Rounded, smoothly marginated, intraparenchymal, or exophytic with a smootll, t11in, or imperceptible wall 513 • Anechoic (a few, thin smooth septations are acceptable) • Characterized by increased wough-transmission of sound • By CT, a simple cyst will be rounded, smoothly marginated, intraparenchymal or exophytic, and have a smooth, thin, or imperceptible wall. Attenuation values should be uniformly those of water (-1 0 to +20 HU), and there should be no evidence of enhancement on immediate postcontrast images ( :S: 1 0 HU increase) . • Renal cysts can b e categorized according to the Bozniak criteria as follows: Category I : Simple uncomplicated benign cyst. These lesions need no further radiologic work-up. Category II: Minimally complicated renal cyst with specific radiologic findings that are of concern. They include all cysts wim one or more fine septations; cysts with tlUn, fine calcifications wit11in the wall or septae; and cysts that are high in attenuation ( >+20 H U ) . These cysts must not demonstrate postcontrast enhancement. They are benign and do not require surgery. Category I I I : Cysts with features also seen with malignant lesions. These features include thickened, irregular walls or septae; thickened, irregular calcifications wimin me walls or septae; some enhancement on postcontrast imaging. These cysts require surgical intervention. Category IV: Cysts that are clearly malignant. These masses will have irregular margins, vascular elements, solid tissue, and areas of necrosis. Some will be neoplasms that have grown adjacent to or in the wall of a simple cyst. These cysts require surgical intervention |
|
A 56-year-old woman 5 days status post renal transplantation presents with
increasing creatinine and no urine output. |
Acute transplant rejection: In acute transplant rejection,
venous flow should be present. However, tills condition cannot be distinguished reliably from acute tubular necrosis. • Severe acute tubular necrosis: Acute tubular necrosis and acute graft rejection have a similar appearance, and both occur frequently in tlle first few days to 1 week post transplant. Acute tubular necrosis would also show venous flow. • Subcapsular hematoma: Subcapsular hemorrhage can produce a Page kidney effect; however, there is no evidence of a large subcapsular hematoma. • Renal vein thrombosis: This is tlle best diagnosis given the Doppler arterial waveform and the conspicuous absence of venous flow. • DIAGNOSIS: Renal vein thrombosis. KEY FACTS CLINICAL • Causes of renal allograft dysfunction are myriad, including acute rejection, acute tubular necrosis, drug toxicity, obstruction, infection, subcapsular hematoma, and vascular complications. • The normal renal allograft is sin1ilar to the normal native kidney in that it has a low resistance vascular system requiring perfusion iliroughout the cardiac cycle (i.e., both systolic and diastolic flow). • Renal blood flow changes reflect the relative severity of disease by increased resistance to allograft perfusion. The more severe the renal disease, the greater the increase in resistance to arterial flow. • Vascular complications are frequent events following renal transplantation. Renal artery stenosis, arterial or venous thrombosis, arteriovenous fistulas, and pseudoaneurysms may all occur. Duplex and color Doppler ultrasound have proven useful for detecting the presence of flow as well as vascular abnormalities. Whereas renal artery stenosis/occlusion in renal transplants occurs in anywhere from 1 .6% to 1 6% of allografrs, renal vein ilirombosis as a cause of acute renal failure is uncommon. • The main role of diagnostic imaging in the immediate post-transplant period is to exclude renal obstruction, evaluate the presence of arterial and venous flow, assess the presence or absence of peritransplant fluid collections, and guide renal biopsies and fluid drainages. RADIOLOGIC • The image findings in tills renal allograft are nonspecific. The internal parenchymal texture is very heterogeneous, consistent witll any number of causes of renal transplant dysfunction. There is no evidence of obstruction or a subcapsular hematoma. • Increased resistance to allograft perfusion is reflected by a disproportionate decrease in diastolic flow. This results in an elevation of the arterial : RI ( Resistive index = (A - B )/B time averaged mean A-B where A = peak systolic velocity and B = end diastolic velocity. • Reversed end diastolic flow indicates markedly increased resistance to renal allograft perfusion. This nonspecific finding does not allow one to distinguish between acute tubular necrosis and acute rejection. However, combined abnormally elevated arterial resistance and absence of venous flow is extremely suggestive of acute renal vein ilirombosis as a cause of renal dysfunction. • Occasionally, very slow venous flow may mimic renal vein ilirombosis. In the absence of color Doppler flow, the use of power or amplitude Doppler to direct subsequent pulsed Doppler spectral analyses may alleviate these diagnostic problems. • While ultrasound can document the presence of arterial and venous flow and assess for obstruction and peritransplant fluid collections, tlle Doppler arterial waveforms are not sufficient for distinguishing between different causes of transplant dysfunction, many of which produce an increased RI. In most instances, if the clinical situation is not diagnostic of the cause of renal dysfunction, a biopsy will be necessary. Ultrasound provides a valuable service in guiding renal transplant biopsies, particularly for avoiding extrarenal vessels. |
|

A 27-year-old pregnant woman is referred for an elevated maternal serum
alpha fetoprotein level at 16 menstrual weeks. |
Omphalocele: This is a possibility, but to be the correct
diagnosis the mass should be surrounded by a membrane and the cord insertion should be into the mass, not to one side of it. The abdominal wall defect tends to be large in omphalocele, and the mass may contain liver. Ascites can be found in the fetal abdomen. • Gastroschisis: This is the most likely possibility because of the eccentric location of the mass, the insertion of the cord adjacent to the mass, the absence of a limiting membrane, and the echogenicity and lobulation of the mass resulting from the conglomeration of bowel loops that are possibly thick walled. • Limb-body wall complex: This is characterized by severe and widespread abnormalities, which can include eviscerated liver, cranial and extremity defects, and scoliosis. Eviscerated organs are often entangled with membranes. • Pentalogy of Cantrell: This is an unlikely diagnosis given that the pentalogy is defined by the presence of an omphalocele, ectopic cordis, diaphragmatic hernia, cardiac malformation, and sternal cleft. • Cloacal extrophy: This is less likely as it is diagnosed on the basis of the failure to identity a normal urinary bladder and splaying of the pubic rami. There are often additional genitourinary abnormalities. • Amniotic band syndrome: This diagnosis is suggested by an unusual collection of abnormalities that could include abdominal wall defects, limb reduction abnormalities or amputations, eccentric cephaloceles, and a cleft lip. The absence of associated membranes also argues against this diagnosis. DIAGNOSIS: Gastroschisis. KEY FACTS CLINICAL • The etiology of gastroschisis has been attributed to abnormal involution of the right umbilical vein and to omphalomesenteric artery disruption . • Though this defect was once thought to mandate a cesarean section, many obstetricians now perform vaginal delivery, at least for subsets of these fetuses. • Most cases occur sporadically, although there are reports of familial recurrence. • Most cases come to attention because of an abnormally elevated maternal serum alpha fetoprotein level. • Gastroschisis is not usually associated with chromosomal abnormality or other malformations. RADIOLOGIC • The diagnosis is based on the presence of an abdominal wall defect from which a mass protrudes that is not covered by a membrane. The defect is usually to the right of the umbilical cord, and ascites is not typically present in the fetal abdominal cavity. • Though a systematic search for other abnormalities should be performed, fetuses with gastroschisis usually do not have additional structural abnormalities. • In most cases, bowel alone is eviscerated, though portions of the genitourinary system can also be involved in the defect. Some reports have suggested that liver can rarely be involved, though these reports have been contested. • Usually the task of the sonographer is to distinguish gastroschisis from omphalocele. The two most telling features of gastroschisis are its paramedian location (lateral to the umbilical insertion ) and the absence of a limiting membrane. In contrast, an omphalocele is encased by a membrane and occurs at the umbilical cord insertion such that the cord inserts directly into the mass. • The extruded bowel can become thick walled and matted. Furthermore, the mass can become encased by fibrous bands. • Fetuses may develop evidence of bowel wall thickening, bowel obstruction, and perforation. Meconium peritonitis is suspected when tl1ere are abdominal calcifications or pseudocysts. Ischemic injury to the bowel can occur. • Intrauterine growth retardation is a frequent complication. |
|

A 54-year-old woman with left knee pain.
|
Metastatic disease: This is an unlikely diagnosis because
of the absence of a primary malignancy and because only a single abnormality is present. Multiple abnormalities would be expected with metastatic disease. • Osteosarcoma: This tumor usually occurs in the 1 0- to 2 5-year-old age range and is apparent radiographically at the time of presentation, making this an unlikely diagnosis. • Insufficiency fracture: This is the best diagnosis because initial radiographs commonly are normal in the face of an abnormal bone scan, with development of sclerosis at the fracture site demonstrable on radiographs a few weeks later. • Osteomyelitis: This diagnosis is unlikely because the patient is older than most patients with osteomyelitis and because of the absence of a predisposing factor. Furthermore, at least some radiographic abnormality would be expected in osteomyelitis. • Degenerative joint disease: This diagnosis is unlikely because the bone scan abnormality is not in the joint space but in the tibial metaphysis. Furthermore, the radiograph does not demonstrate changes of degenerative joint disease. DIAGNOSIS: Insufficiency fracture. KEY FACTS CLINICAL • Musculoskeletal injury accounts for 1 5% to 20% of emergency department visits and 30% of patient visits in routine orthopedic practice . • Physical examination and plain film radiography o f the site of injury are typically performed at the time of presentation. • Insufficiency fractures occur when bones weakened by osteoporosis or other metabolic bone disease are placed under normal stress. • Stress fractures occur when normal bones are exposed to abnormal stress of a repetitive type . • Pathologic fractures occur when bones weakened by tumor involvement are exposed to normal stress. RADIOLOGIC • Radiographic studies are often initially normal at the time of development of an insufficiency fracture or a stress fracture. In fact, abnormalities may not be present until 1 to 2 weeks later. • If pain is considered to be of osseous origin and the plain radiographs are normal, a radionuclide bone scan is the next imaging modality that is generally used to evaluate possible fracture. The bone scan will typically be abnormal at that time. • On a three-phase bone scan, acute fractures demonstrate increased perfusion on the dynamic phase, poorly defined abnormal radiotracer accumulation on the blood pool images, and focal abnormal accumulation on delayed images. • MRI can demonstrate cortical and marrow changes associated with fracture. • Insufficiency fractures in elderly patients with osteoporosis can mimic metastatic disease on plain films. SUGGESTED READING Holder LE. Clinical radionuclide bone imaging. Radiology 1 990;1 76:607-6 1 4 . Holder LE. Bone scintigraphy in skeletal trauma. Radiol Clin North Am 1 993;3 1 :739-78 1 . Martin P. Basic principles of nuclear medicine techniques for detection and evaluation of trauma and sports medicine injuries. Semin Nucl Med 1 9 8 8 ; 1 8 :90- 1 1 2 . |
|
A 4-year-old child with a history of recurrent urinary tract infections.
|
Neurogenic bladder: High grades of vesicoureteral
reflux can be seen in patients with neurogenic bladder, often at relatively low bladder volumes. However, in both of the cases illustrated, the patients were able to void voluntarily to complete bladder emptying, which is inconsistent with the diagnosis of neurogenic bladder. • Unilateral hydronephrosis: This entity is typically seen in the setting of obstruction and is evaluated by an antegrade study. However, the radionuclide cystogram, performed in the cases illustrated, is a retrograde examination undertaken to detect vesicoureteral reflux. • Contamination from voided radionuclide material: Such contamination pools around the external genitalia. In the cases illustrated, the distribution on voiding conforms to the shape of the ureter and intrarenal collecting system. • Vesicoureteral reflux: This is the best diagnosis for the cases illustrated. The radiotracer activity in the ureters in these patients is due to vesicoureteral reflux before and during voiding. Many different grades of vesicoureteral reflux are demonstrated in these two examinations: grades 2 ( Figure 1 0-2A, right ureter), 3 ( Figure 1 0-2B, right ureter), and 4 (Figure 1 0-2B, left ureter) . DIAGNOSIS: Vesicoureteral reflux. KEY FACTS CLINICAL • The overall prevalence of vesicoureteral reflux is < 1 % in the general population. However, 35% of children with urinary tract infections have vesicoureteral reflux, and 25% to 50% of asymptomatic siblings also have vesicoureteral reflux. • Vesicoureteral reflux spontaneously resolves in approximately 80% of cases. • Patients with vesicoureteral reflux are treated with prophylactic antibiotics and re-evaluated with annual cystograms. The goal of therapy is to avoid pyelonephritis, which can leading to renal scarring. However, vesicoureteral reflux alone, without superimposed infection, is also believed to damage nephrons. Therefore, early surgery is recommended for some cases of severe reflux, even in the absence of infection, to prevent renal insufficiency. RADIOLOGIC • The most appropriate means of evaluating pediatric urinary tract infections is a matter of controversy. Most physicians agree that the first cystogram in boys should be an x-ray voiding cystogram, in order to evaluate the urethra. In girls, a radionuclide cystogram is adequate, especially when combined with sonography, which provides adequate anatomic assessment. • The classification of vesicoureteral reflux is as follows: Grade 1 : Reflux into the ureter only Grade 2: Reflux reaching the renal pelvis and calyces, without calyceal dilation Grade 3 : Reflux reaching the calyces, with mild calyceal dilation Grade 4: Reflux reaching the calyces, with marked calyceal dilation Grade 5 : Progressive calcyceal dilation and ureteral tortuosity • Advantages of radionuclide cystography include • Approximately l/l OOth radiation exposure compared with x-ray voiding cystogram • Continuous imaging during bladder filling and voiding, unlike noncontinuous imaging using intermittent fluoroscopy with x-ray voiding cystourethrogram (VCUG) . • Radionuclide cystography technique: The radiopharmaceutical is instilled into the bladder, which is gradually filled with saline via a gravity drip . Imaging continues during bladder filling and voiding. • Filling the bladder to maximum capacity is important for optimal sensitivity. Inadequate bladder filling can produce false-negative examinations. Furthermore, reflux tends to occur at increasingly higher bladder volumes with advancing age as patients outgrow the abnormality. |
|
A 76-year-old woman with a history of coronary artery disease,
hypertension, elevated serum lipids, and atrial fibrillation presents with increasing shortness of breath. |
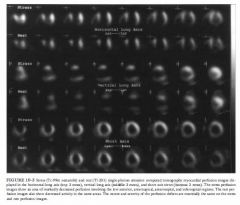
DIFFERENTIAL DIAGNOSIS
• Myocardial infarction without stress-induced ischemia: Tlus is the best diagnosis based on the presence of a fixed perfusion defect with essentially no change in the extent and severity of the perfusion abnormalities between rest and stress studies. • Myocardial ischemia without infarction: This diagnosis is made when a perfusion defect induced by stress is not present on the rest study. This is not the situation in the case illustrated. • Myocardial infarction and stress-induced ischemia: This diagnosis is made when a stress-induced perfusion abnormality incompletely or only partially normalizes on the rest images. • Nonischemic cardiomyopathy: Large perfusion defects either or both at rest and during stress are typically absent ill nOluschemic cardiomyopathy. The large defects that are present in this study make tlus diagnosis unlikely. Furthermore, left ventricular dilatation is a prominent feature of this entity but is not seen in tlle present study. DIAGNOSIS: Myocardial infarction without stress-induced ischemia. KEY FACTS CLINICAL • Several risk factors are known to predispose to coronary artery disease, including age, fanlliy history, hypertension, smoking, and diabetes. • Patients with coronary artery disease may present with symptoms such as either or both angilla and shortness of breath. However, silent ischemia is a well-recognized entity, particularly in diabetic patients. Such patients can have arterial occlusion and infarction in the absence of symptoms. • Myocardial illfarction with coexistent low left-ventricular ejection fraction is associated with a poor prognosis. RADIOLOGIC • Myocardial perfusion studies are performed to determine the severity and extent of myocardial ischemia and infarction and assess prognosis. 525 • TI-201 and Tc-99m sestamibi are myocardial perfusion radiotracers that distribute in proportion to blood flow. There is a good correlation between myocardial perfusion defect size and actual infarct size. • Tc-99m pyrophosphate and In- l l l antimyosill are myocardial illfarct ilnaging radiotracers. These radiotracers are infarct-avid, localizing in illfarcted myocardium. However, these radiotracers are used infrequently because tl1e illformation provided using studies with these agents can be obtained from other tests. • On perfusion ilnaging, myocardial infarction is typically seen as one or more persistent defects on both rest and exercise studies. However, areas of persistent defects at 4 hours on the redistribution TI-20 1 study can decrease or resolve ( indicating myocardial viability) after reinjection or on 24-hour redistribution images. • Large perfusion defects are associated with poor left ventricular function and poor prognosis. • The term hibernating myocardium refers to regions of wall motion abnormality or ventricular dysfunction that ilnprove on perfusion images at 24-hour redistribution or reinjection TI-201 studies. Foci of hibernating myocardium are thought to result from chrome reduction in coronary artery blood flow and represent areas of impaired function with reversible myocardial damage. • The gold standard study for myocardial viability is positron emission tomography ( PET) imagmg with F- 1 8 fluorodeoxyglucose (FDG) and N - 1 3 anlI110ma. Approxilnately 25% of areas with fIXed perfusion defects on TI-20 1 studies are found to be viable on FDG studies. SUGGESTED READING Bonow RO, Dilsizian V. Thallilun-201 for assessment of myocardial viability. Semin Nucl Med 1 99 1 ;2 1 :230-24l . Palmer EL, Scorr JA, Strauss HW. Practical Nuclear Medicine. Philadelphia: Saunders, 1992;7 1-1 20. Verani MS. TI-201 myocardial perfusion imaging. Curr Opin Radiol 199 1 ;3 : 797-809. |
|
|
A 49-year-old woman who underwent complete thyroidectomy for papillary carcinoma
of the thyroid. A metastasis to a left superior jugular node was found at surgery but not resected. An 1- 1 3 1 whole body scan was performed to evaluate for residual thyroid tissue and metastases after the patient developed hypothyroidism. |
DIFFERENTIAL DIAGNOSIS
• Solely residual thyroid tissue: The presence of residual thyroid tissue alone could produce the larger, midline focus of radiotracer accumulation but would not account for the smaller focus to the right of midline. Furthermore, it is known that residual metastatic disease was left at the time of surgery. Therefore, this diagnosis is incorrect. • Functioning thyroid metastatic disease alone: This diagnosis is incorrect because it would not account for the large midline focus, which is at the expected site of the thyroid gland. In addition, it is quite unusual to have no residual thyroid tissue remaining after attempted total thyroidectomy. • Residual thyroid tissue and functioning metastasis: This diagnosis would account for both foci of radiotracer accumulation and is the most likely consideration. • Swallowed radioiodine: Radioiodine that is swallowed can often be seen in the esophagus. This artifarct is prevented by having the patient ingest small amounts of food and fluids. However, the radiotracer activity would be expected to be seen only in the midline. This diagnosis is incorrect because it would not account for the small focus of radio tracer accumulation to the right of midline. • Residual thyroid tissue in the neck with metastatic spread to the abdomen and pelvis: The radio tracer activity in the abdomen and pelvis in the case illustrated is that which is normally seen on 1 - 1 3 1 total body scans, due to excretion into the stomach, colon, and bladder. This radiotracer activity does not represent metastasis. DIAGNOSIS: Residual functioning thyroid tissue and functioning metastasis. KEY FACTS CLINICAL • Thyroid cancers are rarely of a single cell type and are designated by the predominant histologic type. • Three types of carcinoma-well-differentiated papillary carcinoma, follicular carcinoma, and mixed papillaryfollicular carcinoma-comprise about 75% of all primary thyroid malignancies. • Anaplastic and poorly differentiated thyroid carcinomas comprise 20% of all thyroid malignancies and occur primarily in elderly patients. • Medullary thyroid carcinoma constitutes approximately 5% of all primary thyroid cancers and can be associated with other endocrine lesions such as pheochromocytoma as part of a multiple endocrine neoplasia syndrome. 527 • In well-differentiated thyroid cancers, the overall prognosis is good, with a 5 -year survival rate of >95% in properly treated patients. • Well-differentiated papillary carcinoma tends to metastasize to local lymph nodes in the neck, whereas follicular carcinoma tends to spread hematogenously, producing metastases in lungs and bone. • When evaluating patients with well-differentiated thyroid cancer using 1 - 1 3 1 sodium iodide, it is important to stop thyroid replacement therapy and allow thyroidstimulating hormone (TSH) levels to elevate before administration of radiotracer for a total body scan. The resultant high TSH levels stimulate any remaining thyroid tissue or functioning metastases and increase detection of these sites on imaging studies. • Elevation of endogenous TSH takes approximately 4 to 6 weeks to occur after a total thyroidectomy or after cessation of exogenous thyroxin. RADIOLOGIC • Normal radiotracer accumulation of I- 1 3 1 occurs within the salivary glands, stomach, bladder, and bowel . • To optimize the tumor-to-background ratio, imaging should be performed 48 or 72 hours after administration of I - 1 3 l . • The usual dose of I- 1 3 1 administered for whole body imaging for the detection of metastatic differentiated thyroid cancer is 5 to 1 0 mei. • TI-2 0 1 can be used to image functioning metastases from well-differentiated thyroid carcinoma. An advantage of TI-20 1 over 1 - 1 3 1 is that the patients do not need to be in a hypothyroid state for the TI-2 0 1 to detect metastatic foci. • Medullary and anaplastic thyroid cancers rarely, if ever, concentrate I - 1 3 l . • Significant residual thyroid tissue can produce a star pattern that is caused by septal penetration of the collimator by the high energy photons. The star pattern is less likely to result from accumulation in thyroid cancer because the accumulation in functioning thyroid cancer is usually less than in normal thyroid gland. |
|

A 50-year-old man with a history of coronary artery disease and atypical chest pain
6 months after angioplasty of the right coronary artery. Repeat coronary angiography (not shown) revealed stenosis of the left anterior descending coronary artery. |
DIFFERENTIAL DIAGNOSIS
• Myocardial infarction without stress-induced ischemia: The inferior wall motion abnormality at rest is consistent with previous infarction. Myocardial infarction without exercise-induced ischemia would be seen on a perfusion study as a fixed perfusion defect with no significant change between rest and stress studies. However, the changes in perfusion and function from rest to exercise, development of new wall motion abnormalities, and decrease in ejection fraction with exercise indicate that ischemia is also present. • Myocardial ischemia without infarction: Myocardial ischemia alone would produce a stress-induced perfusion defect (typically in the apical, inferior, and anterior walls of the left ventricle) against the background of a relatively normal resting study. Alternatively, ischemia could be seen as exercise-induced wall motion abnormalities on the first-pass study in the anterior and apical regions. However, the resting study in this patient is not normal; the presence of a fixed perfusion defect and resting wall motion abnormality in the inferior wall indicate previous infarction. • Myocardial infarction and stress-induced ischemia: This diagnosis is made when a resting perfusion defect is present that accentuates ( i . e . , increases in either or both severity and extent) during exercise. Typically, the wall motion study shows a wall motion abnormality at rest that worsens during exercise. All these findings are present in this case, making this consideration the best diagnosis. • Noruschemic cardiomyopathy: In the case illustrated, multiple perfusion defects and a new focal wall motion abnormality are induced by exercise. These findings would not be expected in nonischemic cardiomyopathy. • Valvular heart disease: This entity is not commonly associated with perfusion defects and focal wall motion abnormalities. Therefore, valvular heart disease alone (without ischemic heart disease) is an unlikely diagnosis. + DIAGNOSIS: Myocardial infarction and stressinduced ischemia. + KEY FACTS CLINICAL • Atherosclerotic coronary artery disease is the most common cause of cardiovascular disability and death in the United States. • Elevated total serum cholesterol and low-density lipoproteins are involved in the development of atherosclerosis and are markers of high-risk patients. Other risk factors are age, genetic predisposition, hypertension, smoking, and diabetes. • High-density lipoproteins play an equally important protective role against the development of atherosclerotic coronary artery disease. 529 • Atherosclerosis is a chronic process that occurs over decades. However, most acute ischemic syndromes such as infarction and unstable angina are precipitated by plaque ulceration, intimal hemorrhage, and thrombosis. • Advanced stages of coronary artery disease can remain clinically silent, particularly in diabetic patients. Silent ischemic episodes have the same prognostic importance as episodes associated with chest pain. • The most sensitive procedure for determining coronary artery stenosis location and extent is coronary angiography, but myocardial ischemia can be detected noninvasively by either or both myocardial perfusion and left ventricular function studies. • Indications for radionuclide stress testing include evaluation of chest pain, determination of severity and extent of disease, and prognostic assessment. • Patients with multiple perfusion defects ( more than three segments) and low left ventricular ejection fraction ( LVEF) during exercise ( <40%) have a poor prognosis. • Left ventricular exercise ejection fraction provides about 80% of the prognostic information obtained from radionuclide angiography. • Patients with low ejection fraction during exercise are more likely to benefit from revascularization. RADIOLOGIC • Tc-99m-labeled myocardial perfusion radio tracers such as Tc-99m sestamibi allow assessment of myocardial perfusion and left ventricular function with a single injection of radiopharmaceutical. Ventricular function studies can be performed with either a first-pass study or gated images of the perfused myocardium. • I f both the perfusion and functional studies are normal, significant coronary artery disease is extremely unlikely. • If both tests are abnormal, the likelihood of significant coronary artery disease is very high, even if the disease prevalence is low. • Myocardial perfusion and left ventricular function studies provide different, independent types of diagnostic information . • Another method for performing ventricular function studies is to label the blood pool with Tc-99m albumin or Tc-99m red blood cells and to gate the acquisition to the electrocardiogram. This technique is referred to as a gated blood pool study or MUGA study. |
|
|
A 77-year-old Englishman with progressive swelling and deformity of legs and
right upper arm. He has also noted increasing frequency of headaches and increasing hat size over several years. Laboratory studies include an elevated alkaline phosphatase level and normal acid phosphatase and prostate-specific antigen values. |
DIFFERENTIAL DIAGNOSIS
• Paget's disease of bone: The pattern seen on the radionuclide bone scan is that of regions of markedly increased bone tracer accumulation with an expanded appearance to the entire bone. These features are typical of Paget's disease, the most likely diagnosis. • Metastases: Metastases can simulate lesions of Paget's bone disease. The advanced degree of tracer accumulation and expanded bone appearance seen in this case are atypical even for advanced prostate, breast, or lung carcinoma. Tlus diagnosis is an wllikely consideration. • Fractures: The expanded bone and diffuse tracer accumulation make fractures unlikely considerations. • Osteomyelitis: Regions of intense tracer accumulation can be seen in osteomyelitis, but the clinical setting, the diffuse nature of the abnormalities, and the expansile changes seen on the radiograph make tlus diagnosis highly unlikely. • Fibrous dysplasia: Polyostotic fibrous dysplasia can produce increased tracer accumulation in multiple bones, as is seen in this case. However, me history of progressive bony expansion late in life and the radiographic findings make this diagnosis unlikely. DIAGNOSIS: Paget's disease of bone. KEY FACTS CLINICAL • Paget's disease is most commonly encowltered in Eastern and Western Europe (with me exception of Scandinavia) , with a prevalence of 3 . 5% to 4.5% and witll a 3 to 2 male-to-female predominance. • The etiology of Paget's disease is not known definitively. Slow virus inoculation early in life is one hypothesis that has been strongly considered . • Progression o f Paget's disease can b e classified into iliree stages: ( 1 ) bone resorption, ( 2 ) mixed bone resorption and deformation, and ( 3 ) decline in resorption accompanied by a decrease in irregularity and fibrosis. • The prevalence of fractures in Paget's disease is reported to be 8% to 1 8%, based on retrospective series. • Sarcomatous degeneration of pagetoid bone can occur and can be solitary or multicentric. • Elevated cardiac output is seen in some patients wim Paget's disease due to me increased vascularity of acute pagetoid bone. RADIOLOGIC • On radiographs, vertebrae appear enlarged and deformed; me scapulae and pelvic bones appear expanded and thickened; the skull enlarges wim basilar flattening and cortical thickening; and me long bones bow and develop cortical thickening. • The degree of radiotracer accumulation in pagetoid bone is variable. • The radionuclide study is reported to be more sensitiven than radiographs: 5% to 20% of patients have abnormal bone scans and normal radiographs, comparedn to 1% with abnormal radiographs and normaln radionuclide bone scan. • Bone scan findings do not correlate well Witll the severity of bone pain in Paget's disease. • Reduced accumulation of In- I l l-labeled leukocytes and of Tc-99m sulfur colloid has been reported to occur in Paget's disease. • Photopeluc regions can be seen in pagetoid bone in instances of sarcomatous degeneration, most likely due to proliferation of nonosteoblastic tissue . • A photopenic area in a bone scan that occurs in a radiographically evident region of Paget's disease can represent either early disease or sarcomatous degeneration. • Ga-67 may be useful for sarcoma detection. In one small study, slightly more than half of Paget's disease patients with sarcomas and a focal photopenic area on bone scan were found to have increased Ga-67 accumulation at me site of the sarcoma. Another small series found the Ga-67 scan to be less sensitive. |
|
|
The bone scans of three patients are presented. Patient A is a 67-year-old man with
an elevated prostate-specific antigen value of 86 ng/ml and biopsy-proven prostate cancer. Patient B is a 69-year-old man with a history of prostate carcinoma and a borderline normal prostate specific antigen value of 6 ng/ml. Patient C is a 7 1 - year-old woman with a history o f stage IV breast carcinoma. A different diagnosis is possible in each of the cases. |
Metastases: Bone metastases can appear on bone scans as any or all of the following: multiple foci of increased radiotracer accumulation (Figure 1 0-7A), increased or decreased radiotracer accumulation (Figure 1 0-7C), and normal bone radiotracer accumulation. The pattern and
location of the abnormalities in Figures 1 0-7A and 1 0-7C make bone metastases the most likely consideration. • Pathologic fractures: Pathologic fractures can be solitary or multiple and usually occur in metastatic bone lesions that are subject to stress or trauma. Bone metastases in weight-bearing regions are particularly susceptible to fracture. • Multiple benign fractures: The pattern, location, and clinical history are important in distinguishing benign fractures from metastatic disease. Some patterns of fractures (e.g., the string-of-pearls appearance in Figure 1 0-7B ) are typical of benign fractures. This is the diagnosis in patient B . • Degenerative joint dlisease/arthritides: These processes occur at joints and can be difficult to distinguish from metastases. Concomitant benign arthropathic disease can occur in patients with metastatic disease, but the pattern of nonarticular bone abnormalities in all three patients shown above makes benign arthropathic disease alone unlikely. DIAGNOSIS: Patients A and C: multiple bone metastases; patient B: benign rib fractures. KEY FACTS CLINICAL • The likelihood of bone metastases depends on the primary tumor (e.g., most primary bone tumors rarely metastasize) and stage of disease. • The lifetime risk of developing breast cancer in American women is reported to be approximately 1 1 %, and over one-half of breast cancers occur in women after the age of 65 years. In autopsy series of women with metastatic breast carcinoma, the frequency of bone metastases has been reported to be between 44% and 7 1 % . • The digital rectal examination and serum prostate-specific antigen ( PSA) test are currently the recommended screening procedures for prostate carcinoma. Approximately one-third of men over the age of 5 0 years harbor foci o f prostatic carcinoma without clinical evidence of disease. • Approximately 80% of patients with detectable prostate carcinoma and distant metastases are found to have bone metastases. RADIOLOGIC • The majority of metastatic bone tumors appear as focal regions of increased radiotracer accumulation on radionuclide bone scan. However, photopenic foci can be seen in malignancies such as breast, lung, renal, and anaplastic carcinomas; neuroblastoma; and multiple myeloma. 533 • Soft-tissue neoplasms can invade bone and produce increased radiotracer uptake or a photopenic focus, which usually has a rim of increased radiotracer accumulation. • Benign bone conditions that can appear photopenic include bone infarction, bone resection, very early osteomyelitis, radiation-induced bone changes, and histiocytosis X. • Skeletal involvement from multiple myeloma, plasmacytoma, neuroblastoma, and eosinophilic granuloma can produce normal, increased, or decreased radiotracer accumulation. • Particular care must be taken in evaluating the radio nuclide bone imaging study of a patient with bone metastases during the first 4 to 6 months after starting chemotherapy, because a disparity between the clinical/radiologic status and findings on radionuclide bone scan can be seen. These patients can improve clinically and have a decrease in number and size of bone lesions on radiographs but no change or apparent worsening of lesions (the so-called flare phenomenon) on the radionuclide bone imaging study. This pattern change presumably reflects healing of lesions and is most commonly reported in bone metastases from a primary breast or prostate tumor. Following further healing of bone lesions after this initial period, the radionuclide bone study reflects the clinical and radiologic status more accurately. • Patients with a PSA value of dO ng/ml during their initial evaluation for prostate carcinoma have a very low likelihood of having a positive radionuclide bone imaging study for metastases. • The likelihood of a solitary bone scan lesion being a metastasis is reported to range from 1 0% (in adults) to 60% (in children) . • In the presence o f a known primary malignancy, approximately 1 0% to 20% of solitary rib lesions on bone scans are metastases. On the other hand, focal rib lesions having a string-of-pearls pattern are highly likely to be benign rib fractures. • Correlation with radiographs or other imaging studies is often useful to confirm the presence of bone metastases in patients with bone scan abnormalities. In the presence of an abnormal radionuclide bone scan, a normal radiograph actually makes a bone metastasis a likely consideration by excluding other possible causes. |
|
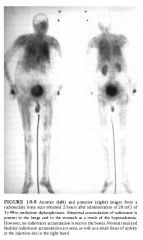
A 75-year-old man being treated for hypercalcemia.
|
DIFFERENTIAL DIAGNOSIS
• Administration of incorrect radiopharmaceutical: This diagnosis is unlikely because no radiopharmaceutical has the pattern of distribution seen in this patient. • Presence of excess aluminum ion: Contamination of Tc-99m methylene diphosphonate (MDP) with aluminum ion from the eluate or the presence of high plasma aluminum levels in patients taking aluminum hydroxide antacids can alter the biodistribution of radiopharmaceutical. However, these conditions cause increased uptake in the liver and kidney and not the lung accumulation seen in the case illustrated. • Effect of therapy for hypercalcemia: The patient shown above was receiving intravenously administered etidronate for treatment of hypercalcemia. Etidronate (hydroxyethylidene diphosphonic acid [ EHDP] ) inhibits the formation, growth, and dissolution of hydroxyapatite crystals. This agent can cause the lack of radiopharmaceutical accumulation within bones, as shown above. • Premature imaging: Images obtained immediately after administration of Tc-99m MDP will typically show blood pool activity, prominent soft-tissue activity, and some bone accumulation. However, accumulation in the lungs would not be expected, making this diagnosis unlikely. • Iron overload: This diagnosis might be considered because in iron overload conditions such as occur in hemochromatosis or following multiple blood transfusions, the accumulation of Tc-99m MDP into bone is diminished and renal excretion is increased. However, pulmonary deposition of the radiotracer would not be expected. DIAGNOSIS: Hypercalcemia with etidronate therapy. KEY FACTS CLINICAL • Hypercalcemia can occur secondary to a number of entities, including hyperparathyroidism, metastatic skeletal disease, hyperthyroidism, and sarcoidosis. • Biphosphonates such as etidronate and pamidronate are used to treat the hypercalcemia of malignancy because of their effect on bone turnover. The biphosphonates interact with the hydroxyapatite crystal, inhibiting bone resorption, and may impair osteoclast function. These agents are also used to treat Paget's disease and heterotopic ossification and may have a role in treating osteoporosis. • Radionuclide bone scans in patients with hypercalcemia and elevated calcium phosphorus products frequently show abnormal localization of the radiopharmaceutical in the lungs, stomach, and kidneys, reflecting the acid-base changes that occur in these tissues. Furthermore, these are the sites of metastatic calcification that can occur in these patients. • The effect of biphosphonates on Tc-99m MDP bone scans is variable. The biphosphonate used and the method of administration ( oral or intravenous) may make a difference in the effect on the bone scan. Some studies report difficulty in interpretation of radionuclide bone scans of patients undergoing biphosphonate therapy, whereas other studies have shown no effect on the sensitivity of the bone scan. RADIOLOGIC • A Tc-99m MDP bone scan that shows poor bone uptake and prominent soft-tissue accumulation usually results from a radiopharmaceutical preparation problem, with excess Tc-99m pertechnetate in the preparation. The excess pertechnetate is manifested by radiotracer accumulation in the thyroid and stomach . • The clue t o the diagnosis i n the patient shown above is accumulation of the Tc-99m MDP in the lungs, which occurs with hypercalcemia. In a patient with accumulation of Tc-99m MDP in the lungs, associated bone scan findings should be considered as possibly related to hypercalcemia or its treatment. • Radionuclide bone scans usually provide diagnostic information in patients receiving biphosphonates, but as noted above, this agent can affect the scan. The effect of this therapy needs to be taken into account when interpreting the images. |
|
A 6-week-old girl with jaundice, total bilirubin of 19.8 mg/d!, and a conjugated
bilirubin of 7.8 mg/dl. |
DIFFERENTIAL DIAGNOSIS
• Idiopathic neonatal hepatitis: Jaundice and bile stasis are features of idiopathic neonatal hepatitis, but the biliary system is patent (unlike the case illustrated) . Hepatic uptake and blood pool clearance o f radiotracer can be delayed in neonatal hepatitis, and the degree of delay reflects the severity of hepatocyte damage. • Choledochal cyst: The absence of visualization of the proximal ducts or an actual cyst makes this diagnosis unlikely. • Biliary atresia: This is the best diagnosis because good hepatocyte extraction of radiopharmaceutical is seen in the absence of visible intrahepatic bile ducts or gastrointestinal ( G I ) activity, even on 24-hour images. • Bile plug syndrome: This rare condition results in conjugated hyperbilirubinemia due to obstruction of the common bile duct by inspissated bile/secretions. Sepsis, hemolytic disorders, dehydration, total parenteral nutrition, and cystic fibrosis are predisposing conditions. Careful ultrasound examination to exclude echogenic, nonshadowing bile plugs within the dilated biliary tree is necessary to distinguish this condition from biliary atresia. • Arteriohepatic dysplasia (Alagille syndrome): This syndrome is characterized by typical dysmorphic facies, pulmonary artery stenosis, and hepatic ductular hypoplasia. Distinction from true biliary atresia can be difficult if the other components of the syndrome are not recognized . DIAGNOSIS: Biliary atresia. KEY FACTS CLINICAL • Hyperbilirubinemia is a common problem in neonates and infants. Unconjugated hyperbilirubinemia, in which < 1 5% of the total bilirubin is conjugated (or "direct," which is the nomenclature used on laboratory reports) is most often due to physiologic jaundice of the newborn, breast milk jaundice, or erythroblastosis fetaLis. In conjugated hyperbilirubinemia, where at least 30% of the bilirubin is conjugated, a search for causes of obstructive jawldice is necessary. The most common causes of obstructive jaundice are included in the differential diagnosis Listed above . 537 • Biliary atresia is the most common cause of extrahepatic cholestasis in infants. The incidence ranges from 1 in 8 ,000 to 1 in 1 0 ,000 live births. • Distinction between idiopathic neonatal hepatitis, a nonsurgical disease, and biliary atresia, a surgical disease, is important within the first 3 months of life. The Kasai procedure (or portoenterostomy) is performed using a Roux -en -Y loop of intestine to bypass the hypoplastic or absent biliary duct segments. The surgical success rate varies according to patient age at the time of surgery. The procedure is 90% effective in patients <2 months of age, but only 1 7% effective in patients >3 months of age. RADIOLOGIC • DIS IDA ( diisopropyliminodiacetic acid, disofenin) and mebrofenin ( trimethyl-bromo-IDA) have the highest extraction rate by hepatocytes and shortest transit time of the IDA derivatives. Between 5% and 1 5% of the disofenin is excreted via the kidneys in normal subjects. Dynamic image acquisition immediately after radiopharmaceutical injection is helpful to determine hepatocyte extraction and hepatocyte function. Static images performed over the next 1 to 2 hours with delayed images taken up to 24 hours are generally required. • Pretreatment with oral phenobarbital (5 mg/kg/day for 5 days) is recommended to improve bile flow. With phenobarbital pretreatment, biliary scintigraphy is approximately 95% accurate in determining biliary patency in infants <3 months of age. • Progressive hepatocyte damage and hepatic cirrhosis occur in the setting of untreated biliary atresia and in persistent neonatal hepatitis. The two diseases can be indistinguishable in patients >3 months of age. |
|

A 68-year-old man with a history of Crohn's disease of the terminal ileum and colon
presents with a 3-day history of nausea and right upper quadrant pain radiating posteriorly to the back. The pain is worsened by eating. |
DIFFERENTIAL DIAGNOSIS
• Acute pancreatitis: This process presents with abdominal pain and can be seen in patients with Crohn's disease. An elevated serum amylase is usually present. Hepatobiliary imaging studies are normal unless pancreatitis is due to underlying hepatobiliary disease. This diagnosis is therefore unlikely. • Acalculous cholecystitis: Acute inflammation of the gallbladder can occur in the absence of cholelithiasis, most often as a complication of severe underlying illnesses (e.g., burns, trauma, sepsis, and following major surgery) associated with bile stasis. The benign clinical features and sonographic finding of gallstones make this diagnosis unlikely. • Common bile duct obstruction: Approximately 1 0% to 1 5% of patients with cholelithiasis will pass a gallstone into the common bile duct (CBD), from which it can ( 1 ) pass into the duodenum, ( 2 ) remain without producing symptoms, or ( 3 ) obstruct the CBD. The presence of radiotracer in the CBD and the duodenum by 10 minutes essentially excludes CBD obstruction. • Chronic cholecystitis: Patients with chronic cholecystitis frequently have gallstones and gallbladder wall thickening, and can have repeated bouts of biliary colic without cystic duct obstruction. The most frequent abnormal finding on scintigraphy is delayed visualization of the gallbladder beyond 1 hour, but imaging is normal frequently. Scintigraphy is generally an ineffective study in the evaluation of chronic cholecystitis, except to exclude a superimposed acute cystic duct obstruction. The majority of patients with only chronic cholecystitis would be expected to have visualization of the gallbladder by 1 80 minutes, making this diagnosis unlikely in the case illustrated. • Acute cholecystitis: This entity typically has the presentation of right upper quadrant pain and tenderness with fever and leukocytosis. It often begins as an attack of biliary colic that progressively worsens and is associated with anorexia, nausea, and, commonly, emesis. With cystic duct obstruction, bile does not flow into or out of the gallbladder (as in the case presented above ) . The imaging findings in this case make this the most likely diagnosis. • DIAGNOSIS: Cholelithiasis with acute cholecystitis. • KEY FACTS CLINICAL • Patients with Crohn's disease are at increased risk for development of cholelithiasis (due to altered bile salt absorption) and acute cholecystitis. • Acute cholecystitis is most commonly caused by acute occlusion of the cystic duct by a gallstone. • Seventy-five percent of patients with acute cholecystitis respond to medical therapy, of whom 25% have recur- rent acute cholecystitis within 1 year. Another 25% of patients treated conservatively develop a major complication, such as empyema, hydrops, gangrene, emphysematous cholecystitis, perforation of the gallbladder, or gallstone ileus. Therefore, early surgical therapy is the preferred treatment. • As expected, patients with suspected empyema, emphysematous cholecystitis, or perforated gallbladder require more urgent surgical intervention than those with uncomplicated acute cholecystitis. It is important to search for evidence of these complications at the time of imaging. • Perforation of the gallbladder has an estimated 30% mortality rate. These patients can have sudden transient relief of right upper quadrant pain as the distended gallbladder decompresses but then develop generalized signs of peritonitis. RADIOLOGIC • The diagnosis of acute cholecystitis can be confidently excluded on the basis of a normal hepatobiliary imaging study (negative predictive value of 98%). • False-positive hepatobiliary scans can be seen in the following settings: alcoholism, total parenteral nutrition or prolonged fasting, within 2 hours of eating, and in severe intercurrent illnesses. • Radiotracer in the duodenum or pericholecystic hepatic uptake of radio tracer (the "rim sign") can be mistaken for gallbladder uptake, resulting in a falsenegative interpretation . The finding of pericholecystic hepatic uptake of radio tracer is important to recognize. It is present in 57% of patients with gangrenous cholecystitis and 3 1 % of patients with perforated gallbladder. • Potential mechanisms by which pericholecystic hepatic uptake occurs include hyperemia with increased delivery and extraction of radiotracer along the gallbladder fossa, focal hepatic cellular injury with impaired excretion of radio tracer, and mechanical obstruction with focally delayed clearance of radio tracer. • If the gallbladder is not seen by 30 to 45 minutes but there is radio tracer in the small bowel, the study can be shortened from 4 to 2 hours by giving intravenous morphine sulfate ( 0.04 mg/kg; maximum 4 mg). Morphine sulfate contracts the sphincter of Oddi and redirects bile flow into the gallbladder if the cystic duct is patent. The study can be stopped when the gallbladder is filled or at 2 hours (whichever occurs first) . |
|
|
A 59-year-old man with melena 48 hours prior to developing brisk, bright red rectal
bleeding. Upper and lower G I endoscopy failed to show a bleeding source. A Tc-99m sodium pertechnetate-Iabeled red blood cell imaging study was obtained, followed by selective abdominal arteriography. |
aneurysm can have focally increased radiotracer on
blood pool imaging. This is an unlikely diagnosis because it is generally seen early and does not change in shape or location during the study. • Free Tc-99m pertechnetate in the bowel: Free Tc- 99m sodium pertechnetate can be present on reinjection of tagged red blood cells. Pertechnetate is normally secreted by gastric mucosa. The stomach will be visualized, and during the latter part of the study, some of the normally secreted pertechnetate can occasionally enter small bowel. However, the intensity of radiotracer activity within bowel is usually faint and moves only minimally, making this an unlikely diagnosis in this case. • Inflammatory bowel disease: Inflammatory bowel disease can produce a positive gastrointestinal (GI) bleeding scan by two mechanisms: ( 1 ) active bleeding, and (2) blood pool accumulation of radio tracer at sites of inflammation, even in the absence of active bleeding (in which case the sites remain static during the study). The latter possibility is unlikely in the case shown because the abnormal radiotracer accumulation in the case presented above is seen to progress through the small bowel. • Active bleeding originating in the colon: Unless retrograde movement of radiotracer from the cecum into the terminal ileum occurs, radio tracer activity in the small bowel is generally not seen after hemorrhage from a colonic bleeding source. The findings in the patient shown are therefore unlikely to be due to an active bleeding site originating in the colon. • Active small bowel bleeding: Active small bowel hemorrhage can usually be distinguished from that arising in large bowel and further localized to the proximal, mid-, or distal small bowel. The findings of this case make the diagnosis of a mid-small bowel (jejunal) bleeding site the most likely diagnosis. + DIAGNOSIS: Acute mid-jejunal gastrointestinal hemorrhage. + KEY FACTS CLINICAL • The presence of melena usually denotes bleeding from the esophagus, stomach, or duodenum, but lesions in the jejenum, ileum, and the ascending colon can cause melena, depending on the transit time of blood within the GI tract. • Hematochezia generally signifies a bleeding site from a source distal to the ligament of Treitz, but rapid hemorrhage from the esophagus, stomach, or duodenum 541 with rapid peristalsis can also produce bright red rectal bleeding. • Initial attempts to localize a GI bleeding site should include nasogastric tube insertion, esophagogastroduodenoscopy, sigmoidoscopy, and colonoscopy (which is impaired when the lumen of the colon is obscured by large amounts of brisk bleeding) . • Peptic ulceration, erosive gastritis, variceal bleeding, and Mallory-Weiss syndrome account for 90% of all cases of upper GI hemorrhage in which a definite cause is found . RADIOLOGIC • The primary purpose of the scintigraphic GI bleeding study is to localize an active bleeding site to serve as a guide before selective abdominal angiography. • In general, the rate of bleeding required for scintigraphic detection of GI bleeding is less than that required for detection by angiography. Therefore, if the scintigraphic GI bleeding study is negative, angiography is not indicated. • Evaluation for GI bleeding by scintigraphy can be performed using sulfur colloid. The major disadvantage of this teclmique is rapid removal of the sulfur colloid by the liver, spleen, and bone marrow. Active bleeding must occur within minutes of radiotracer injection if the bleeding site is to be shown. • Because GI bleeding is often intermittent, the labeled red blood cell technique is the preferred method for scintigraphic evaluation. Imaging is performed for a minimum of 2 hours, allowing a reasonable time for bleeding to occur. • GI bleeding study findings are evaluated best by reviewing the images in a dynamic cine display (obtained at a rate of 1 frame per minute), which increases conspicuity of radiotracer movement compared to sequential static images by making subtle . fmdings more apparent. Dynamic display should be a routine part of the imaging protocol. |
|

A 43-year-old woman presents with a history of multiple hepatic masses.
|
DIFFERENTIAL DIAGNOSIS
• Neuroendocrine tumor metastatic to the liver: This is the Likely cliagnosis because of the increased accumulation of In- l l l octreotide in the focal masses in the liver. • Metastatic colon cancer: This cliagnosis is unlikely because In- l l l octreotide does not accumulate in metastatic colon cancer. • Pheochromocytoma: This is an unlikely consideration because neither the meta-iodobenzylguanicline (MIBG) scan nor the In- I l l octreotide scan showed abnormal accumulation in the region of the adrenal glands. • Neuroendocrine tumor metastatic to the left chest: This cliagnosis is unlikely because the accumulation in the left chest on the MIBG scan is a normal finding related to carcliac innervation. • Multicentric hepatoma: This cliagnosis is unlikely because hepatoma does not accumulate In - I l l octreotide. + DIAGNOSIS: Liver metastases from neuroendocrine tumor. + .KEY FACTS CLINICAL • Neuroendocrine tumors are derived from the amine precursor uptake and decarboxylation (APUD) system and contain secretory granules. • Somatostatin, a peptide hormone consisting of 14 amino acids, has a short plasma half-life (2 to 4 minutes) . • Octreotide, a peptide that has eight amino acids, i s an analog of somatostatin that is used therapeutically to block secretions from neuroendocrine tumors that contain somatostatin receptors. • Somatostatin receptors have been demonstrated in a wide variety of tumors, including pituitary tumors, 543 gastrinomas, insuLinomas, glucagonomas, paragangliomas, medullary thyroid carcinomas, pheochromocytomas, carcinoid tumors, small cell lung cancer, neuroblastomas, meningiomas, breast cancers, lymphomas, granulomatous cliseases, and the thyroid glands of patients with Graves' clisease. RADIOLOGIC • Inclium- l l l octreotide localizes in most neuroendocrine tumors because they have somatostatin receptors. • Indium- I l l octreotide imaging can be used to select patients who are likely to respond to octreotide treatment. • MIBG labeled with either 1- 1 3 1 or 1 - 1 2 3 localizes in most neuroendocrine tumors because of the presence of a neuronal pump mechanism for norepinephrine. • MIBG and In- l l l octreotide demonstrate different metabolic functions, and the images in a patient may be abnormal with one racliotracer but not with the other. • lodine- 1 3 1 MIBG has been used therapeutically in patients who have neuroendocrine tumors that accumulate racliotracer on cliagnostic imaging. • At present, there is no therapeutic analog of In- l l l octreotide. + SUGGESTED READING Hanson MW, Feldman JM, Leight GS, Coleman RE. Iodine 1 3 1 - labeled meta-iodobenzylguanidine scintigraphy and biochemical analyses of pheochromocytomas. Arch Intern Med 1 99 1 ; 1 5 1 : 1 397- 1 402. Kvols LK. Somatostatin-receptor imaging of human malignancies: A new era in the localization, staging, and treatment of tumors. Gastroenterology 1993;105: 1909-19 1 1 . Tenenbaum F, Lumbroso J , Schlumberger M, et al. Comparison of radiolabeled octreotide and meta-iodobenzylguanidine (MIBG) scintigraphy in malignant pheochromocytoma. J Nucl Med 1 995;36: 1-6 . |
|
A 28-year-old woman with a nontender, ftrm, palpable thyroid nodule.
|
• Carcinoma: Carcinoma constitutes 1 0% to 20% of
solitary nonfimctioning nodules. The nodules are usually very firm or hard on palpation. This is the most likely diagnosis. • Functioning adenoma: These lesions are usually firm but not hard in texture. This is an unlikely diagnosis because a ftmctioning adenoma would be expected to accumulate Tc-99m sodium pertechnetate. • Colloid cyst: This entity is usually soft on palpation and therefore unlikely to be the etiology in this case. FIGURE l O - 1 3B An image with markers on the superior and inferior margins of the palpable nodule. The focal region of decreased accumulation between the markers corresponds to the palpable nodule. These lesions are usually well defined by sonography, but biopsy is definitive . • Chronic thyroiditis (Hashimoto's disease): This is an unlikely diagnosis because chronic thyroiditis is usually multinodular on palpation and has a more inhomogeneous appearance on radionuclide imaging than the finding in the patient illustrated. • Hemorrhage: Hemorrhage into an adenoma or cyst can present as a solitary nodule but is usually tender, making it an unlikely diagnosis in this patient. CASE #13 • Nuclear Medicine DIAGNOSIS: Thyroid carcinoma. KEY FACTS CLINICAL • Papillary carcinomas are the most common thyroid neoplasm in North America, are four times more frequent in women, and have peak incidence between ages 20 and 40 years. They metastasize primarily via the lymphatic system. Patients with papillary carcinomas have about a 90% l a -year survival rate. • Follicular carcinomas comprise about 1 5% of thyroid carcinomas and usually occur after 40 years of age. They metastasize via hematogenous spread. Patients with follicular carcinomas have a l a -year survival rate of about 70%. • Hfuthle cell carcinomas are considered variants of follicular cell carcinoma, are relatively rare, and have a variable prognosis. • Medullary carcinomas comprise 5% to 1 0% of thyroid carcinomas. About one-fifth of these patients inherit this disease as part of one of the following three syndromes: multiple endocrine neoplasia ( MEN) groups 1 and 2 and a non-MEN syndrome. The familial nonMEN group has the best prognosis, followed by the familial MEN 2A, and then the nonfamilial ( sporadic) form. Familial MEN 2B syndrome has the worst prognosis. Overall l a -year survival for all patients with medullary carcinoma of the thyroid is about 60%. • Anaplastic carcinomas comprise about 1 0% of thyroid carcinomas, usually occur late in life (after the sixth decade) , and have a 5 -year survival for all patients with medullary carcinoma of the thyroid rate of <5%. • The risk of metastasis increases with age at time of diagnosis, particularly for follicular thyroid carcinoma. In addition, recurrence and mortality rates are significantly higher after 45 years of age. • External beam radiation therapy to the neck region before late adolescence increases the risk of developing either or both benign and malignant thyroid nodules. • Based on autopsy series, incidental small foci of occult malignant thyroid cells are found in about 1 0% of patients with no prior clinical evidence of thyroid malignancy. • Between 1 0% and 20% of solitary nonfunctioning nodules seen on radioiodine thyroid imaging studies in adults are malignant. • Only 5% of thyroid nodules are hyperfunctioning and cause suppression of normal thyroid tissue. These nodules may result in toxic nodular goiter. A very small percentage (2% to 4%) of hyperfunctioning thyroid nodules have been reported to have regions of malignant neoplasia. Clinicians who treat toxic nodular goiter with radioiodine usually presume the hyperfunctioning nodule to be of benign histology. • With the advent of fine-needle aspiration biopsy, largeneedle aspiration biopsy, and large-needle cutting ( "core " ) biopsy as definitive means of evaluating thyroid nodules, radionuclide imaging studies for this purpose are performed infrequently. Nonetheless, these studies can be useful in defming an autonomous functioning or hyperfunctioning thyroid nodule, which usually precludes the need for biopsy. • A solitary thyroid nodule in a prepubescent child has a higher likelihood of being malignant than that in an adult. • Initial reports suggested that the presence of a diffuse toxic goiter offered protection from developing a thyroid malignancy. However, it has subsequently been shown that the likelihood of a solitary nonfunctioning thyroid nodule being malignant does not differ in patients with diffuse toxic goiter and patients who are euthyroid. |
|
|
A 26-year-old woman has partial complex seizures that are refractory to anticonvulsants.
The seizures are preceded by an aura of a feeling of fear, followed by staring and oral automatic movements. An interictal F- 1 8 FDG positron emission tomography (PET) brain scan is performed for seizure focus localization before temporal lobectomy. |
DIFFERENTIAL DIAGNOSIS
• Low-grade tumor: A low-grade tumor with associated edema can have diminished F- 1 8 FDG uptake . The loss of hippocampal volume, rather than a mass lesion, on the MR image makes this diagnosis unlikely. • Radiation necrosis: Tissue necrosis following radiation therapy can have diminished F- 1 8 FDG uptake, but the absence of a brain tumor or prior radiation therapy excludes this diagnosis. • Ictal seizure focus: After F- 1 8 FDG injection at the time of a seizure, increased radiotracer uptake would be expected rather than the decreased uptake seen in the case presented, making this diagnosis incorrect. • Interictal seizure focus: When F- 1 8 FDG is injected at a point when the patient is between seizures (i.e., interictally), the uptake of radiotracer in the dormant seizure focus is diminished. This choice, therefore, is the most likely diagnosis. • Infarction: Infarcted brain tissue can have diminished F- 1 8 FDG uptake. The clinical history and the fact that the abnormality is confined to the hippocampus on the MR image make this diagnosis unlikely. DIAGNOSIS: Interictal seizure focus. KEY FACTS CLINICAL • Complex partial seizures (psychomotor or temporal lobe seizures) are frequently preceded by an aura manifested by hallucinations, illusions, affective changes, or aberrations of cognition, and often are accompanied by complex movements. These auras are characteristic of a seizure focus in certain regions of the temporal lobe or limbic system. • Most complex partial seizures are due to epileptiform activity in the temporal lobes (especially the hippocampus or amygdala), but they can also originate from mesial parasagittal or orbital frontal regions. • The surface electroencephalogram ( EEG) can be normal in patients with complex partial seizures. Depth electrode placement may be required to define the seizure focus by EEG criteria more accurately. • Complex partial seizures can progress to generalized major motor ( grand mal) seizures, manifested by loss of consciousness and tonic/clonic movements. RADIOLOGIC • F- I 8 FDG is a positron-emitting radiopharmaceutical with a half-life of 1 1 0 minutes that functions as an analog of glucose . It accumulates in viable cells in proportion to the individual cellular consumption of glucose. • F- 1 8 FDG imaging of the central nervous system is optimally performed at approximately 30 minutes following the injection of radiotracer. During the 30- minute delay, the patient should be wlstimulated-i.e., kept in a quiet, dimly lit environment with only background noise. • In the evaluation of patients for a seizure focus, an EEG should be acquired during the 30-minute uptake phase of F- I 8 FDG to document the presence or absence of seizure activity that may not be apparent clinically during this interval. • Metabolic imaging with F- 1 8 FDG of patients with seizures can show functional abnormalities even when MRI studies and histologic specimens obtained from the temporal lobe fail to show an abnormality. • F- 1 8 FDG imaging is more useful for localization of a seizure focus in patients with suspected temporal lobe seizures than in those with a suspected extratemporal lobe origin of seizure activity. • Single-photon emission computed tomography (SPECT) brain perfusion imaging performed in the ictal and interictal states has an accuracy similar to F- 1 8 FDG PET in localizing the seizure focus. • High-resolution MRI of the hippocampus also has an accuracy similar to F- 1 8 FDG PET in localization of the seizure site. |
|
A S4-year-old man referred for evaluation of dyspnea on exertion. Exercise (Figure
l O - l SA) and redistribution ( Figure l O - l SB ) TI-201 images are obtained. |
DIFFERENTIAL DIAGNOSIS
• Myocardial ischemia: The lack of normalization of the perfusion defects makes this diagnosis unlikely. • Myocardial infarction: The perfusion abnormalities at exercise without normalization on redistribution makes this diagnosis the most likely. • Nonischemic cardiomyopathy: The presence of large perfusion defects makes this diagnosis unlikely. • Valvular heart disease: The presence of large perfusion defects makes this diagnosis unlikely. • Normal study with attenuation of inferolateral myocardium: The extent of the perfusion abnormality, the dilated ventricle, and accumulation of radio tracer in the lungs on the images obtained after exercise make this diagnosis unlikely. DIAGNOSIS: Myocardial infarction. KEY FACTS CLINICAL • Approximately 5 million adults in the United States have symptomatic coronary artery disease. One and one-half million people have an acute myocardial infarction each year. Coronary artery disease accounts for 25% of deaths from all causes. • Myocardial ischemia occurs when coronary artery blood flow is inadequate to meet the metabolic requirements of the myocardium. Myocardial infarction occurs when the myocardial blood flow to a segment of the myocardium is <0 . 1 ml/min/g of tissue (normal flow is 0.5 to 1 .0 mi/rnin/g of tissue). • The normal end diastolic volume of the left ventricle is approximately 1 50 mi . When the ejection fraction decreases from a normal value of >50% to <50% (such 549 as can occur with myocardial infarction), the ventricle dilates to maintain an adequate stroke volume and cardiac output. • With exercise, transient ischemia that causes ventricular failure can result in an increase in ventricular cavity size and an increased left ventricular end diastolic pressure. The transient increase in left ventricular end diastolic pressure results in a transient pulmonary edema, and thereby increased pulmonary radiotracer accumulation . RADIOLOGIC • The TI-201 images in the case presented above show a large fixed defect in myocardial perfusion, abnormal TI-2 0 1 accumulation in the lungs on the postexercise images, and prominent right ventricular TI-201 accumulation on both sets of images. These findings are typical of myocardial infarction with exercise-induced left ventricular failure causing transient TI-2 0 1 lung accumulation. Lung accumulation on a TI- 2 0 1 study is definitely abnormal if the lungs are clearly outlined on the images. Regions of interest can be obtained in the left lung adjacent to the anterior wall and in the myocardium. A ratio of lung counts to myocardial counts >0.5 is indicative of abnormal lung accumulation and left ventricular dysfunction. • The prominent right ventricular accumulation in the case shown above is diagnostic of right ventricular hypertrophy. + SUGGESTED READING Bonow RO, Dilsizian V. Thallium-201 for assessment of myocardial viability. Semin ucl Med 199 1 ; 2 1 :230-24 l . Palmer EL, Scott JA, Strauss HW. Practical Nuclear Medicine. Philadelphia: Saunders, 1 992;7 1-120. Verani MS. TI-2 0 1 myocardial perfusion imaging. Curr Opin Radiol 199 1 ;3:797-809. |
|
|
A 59-year-old man with diabetes, hypertension, and hyperlipidemia presents with
dyspnea on exertion and peripheral edema. The patient has no history of prior myocardial infarction. Cardiac catheterization (not shown) reveals normal coronary arteries but diminished left ventrivular ejection fraction ( LVEF). He is referred for a multiple gated acquisition (MUGA) study. |
Left ventricular aneurysm: The ventricular abnormalities
in the case illustrated are diffuse, rather than focal, as would be expected with an aneurysm. • Restrictive cardiomyopathy: Typical findings of restrictive cardiomyopathy are mild cardiac enlargement and a left ventricle that has preserved systolic function but is resistant to diastolic filling. In the case illustrated, however, a dilated left ventricle with poor systolic function is seen, making this an incorrect diagnosis. • Myocardial infarction: A focal abnormality, typically involving the left ventricle, would be expected with infarction, rather than the diffuse dysfunction involving both ventricles in the case illustrated . • Dilated (congestive) cardiomyopathy: Dilated cardiomyopathy produces varying degrees of cardiac enlargement ( as seen in Figures 1 0- 1 6A and 1 0- 1 6B ) , left ventricular dilatation, increased l e ft ventricular volume, global patterns of abnormal contractility, and a diminished LVEF ( as seen in Figures 1 0- 1 6C and 1 0- 1 6D ) . This diagnosis the most likely one for the case illustrated. • Hypertrophic cardiomyopathy: Hypertrophic cardiomyopathy can produce mild to moderate cardiac enlargement, but it is usually associated with vigorous left ventricular contractility and septal thickness that is increased out of proportion to the thickness of the left ventricular free wall. The absence of these findings in the case shown above makes this diagnosis unlikely. DIAGNOSIS: Dilated (congestive) cardiomyopathy. KEY FACTS CLINICAL • Dilated cardiomyopathy is most commonly seen in middle-aged men but can occur at any age. • Infectious, metabolic, and toxic causes are the most common etiologies of dilated cardiomyopathy. Known specific causes include alcohol, Adriamycin, cyclophosphamide, neuromuscular disease (muscular dystrophies), and pregnancy. However, a definite etiology cannot be discerned in many cases. • Histologic examination of the myocardium in dilated cardiomyopathy reveals extensive regions of perivascular and interstitial fibrosis accompanied by mild necrosis and cellular infiltration. • Patients with dilated cardiomyopathy present with symptoms of Ieft- or right-sided congestive heart failure--e.g., fatigue, peripheral edema, dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea, and palpations. Vague chest discomfort can occur, but typical angina pectoris is uncommon and, when present, implies the presence of concomitant coronary artery disease. • Most patients with dilated cardiomyopathy have progressive clinical deterioration. The disease is often fatal within 2 years of symptom onset, especially for older ( > 5 5 years old) patients. Progressive congestive heart failure and ventricular arrhythmias are the most common causes of death. RADIOLOGIC • The gated blood pool study is widely accepted as an accurate imaging technique for evaluation of left ventricular function and is often used for assessment of congestive heart failure, effects of cardiotoxic drugs, left ventricular function following cardiac surgery, and effects of exercise on left ventricular function in patients with suspected coronary artery disease. • A gated blood pool study can be performed using either Tc-99m sodium pertechnetate-Iabeled autologous red blood cells (the preferred technique) or Tc- 99m-labeled human serum albumin. • The best septal view is one that allows separation of the ventricles, facilitating determination of both the LVEF and the right ventricular ejection fraction ( RVEF). This view is typically a 45-degree left anterior oblique projection ( Figures 1 0- 1 6C and 1 0- 1 6D above) . • Correct determination o f background activity ( usually 30% to 60% of left ventricular end diastolic counts) is critical in calculating an accurate LVEF. Overestimation of background activity falsely elevates the LVEF, while underestimation of background activity falsely decreases the L VEF. • Calculation of the RVEF on a gated blood pool study is less accurate than LVEF calculation. This fact is primarily due to the contribution of activity from the right atrium into the right ventricular region of interest and the uncertainty of the location of the pulmonic valve . Because of the larger volume of the right ventricle, the accepted normal RVEF is generally 5% to 1 0% less than the normal LVEF. |
|

A 27-year-old woman being treated for gestational trophoblastic disease with a 36-
hour history of severe, intermittent, left pleuritic chest pain. |
DIFFERENTIAL DIAGNOSIS
• Pulmonary artery obstruction by extrinsic mass: A focal area of ventilation-perfusion CV/Q) mismatch can result from compression by a hilar or mediastinal mass. The presence of multiple bilateral mismatched V/Q abnormalities makes this diagnosis unlikely. Furthermore, no extrinsic mass is seen compressing the pulmonary arteries on the CT scan. • Radiation therapy port: The presence of multiple perfusion defects that correspond to vascular segments makes this diagnosis incorrect . • Vasculitis: The multiple segmental V/Q mismatches and the presence of emboli on the CT scan make this diagnosis unlikely. • Pulmonary embolism (PE): The multiple segmental perfusion defects in areas that are normal on the ventilation study and the chest radiograph make this diagnosis the most likely. The diagnosis is confirmed by the presence of thromboemboli that are seen on the contrast- enhanced CT scan . • Multiple peripheral pulmonary arterial stenoses: The presence of emboli on the CT scan makes this an incorrect diagnosis . + DIAGNOSIS: Pulmonary embolism. + KEY FACTS CLINICAL • Risk factors for PE include advanced age, immobilization, history of previous PE, concurrent malignancy (usually adenocarcinoma), and hereditary causes of a hypercoagulable state-e.g . , factor S deficiency. • The presence of abnormal blood gas findings, the typical history of pleuritic chest pain, shortness of breath, and characteristic electrocardiogram changes can be helpful in raising a strong suspicion of the diagnosis . However, because some of these features are often not present, imaging studies, in particular V/Q scans and pulmonary angiography, are important in helping to establish the diagnosis firmly. RADIOLOGIC • The chest radiograph is frequently normal in patients with PE. Atelectasis, a small pleural effusion, and elevated hemidiaphragm are nonspecific radiographic findings that are seen in many patients with PE. 553 • The high probability pattern-i.e., two or more perfusion abnormalities without matching ventilatory abnormalities-is most often caused by PE. Some entities- e.g . , vasculitis-can produce a pattern ofV/Q mismatch simulating the high probability pattern, but these entities often result in a more heterogeneous pattern than seen in the case illustrated above. • The low-probability pattern includes : ( 1 ) defects surrounded by normal lung (stripe sign), ( 2 ) corresponding defects and large pleural effusion, ( 3 ) nonsegmental perfusion defects, (4) corresponding defects and opacity in the upper or middle lung zones, ( 5 ) a perfusion defect with a substantially larger radiographic abnormality, ( 6 ) matched ventilation and perfusion abnormalities with a normal radiograph, and ( 7 ) more than three small perfusion defects . • The intermediate probability pattern includes ( 1 ) one moderate to two large perfusion defects without corresponding ventilation of radiographic abnormalities, (2) corresponding ventilation, perfusion, and parenchymal abnormalities in the lower lung zones, and ( 3 ) corresponding defects and small pleural effusion. • The very low probability category consists of three or fewer small defects. The normal category consists of no perfusion abnormalities. • The gold standard examination for the diagnosis of PE is pulmonary angiography. However, MRI and helical CT can identifY patients who have proximal thromboemboli and also serve to exclude pulmonary artery compression as a cause ofV/Q mismatch. + SUGGESTED READING Gottschalk A, Sostman RD, Coleman RE, et a1. Ventilationperfusion scintigraphy in the PIOPED study. Part II. Evaluation of the scintigraphic criteria and interpretations. J Nucl Med 1993;34: 1 1 1 9- 1 1 26 . Grist TM, Sostman R D , MacFaIl JR, e t a l . Pulmonary angiography using MRI: Initial clinical experience. Radiology 1993 ; 1 89 : 528-530. Worsley DF, Alavi A. Comprehensive analysis of the results of the PIOPED study. J Nucl Med 1 995;36:2380-2387. |
|
A 67-year-old man with pain and swelling in both knees 3 years after left upper
lobe resection and radiation therapy for adenocarcinoma of the lung. |
Primary hypertrophic osteoarthropathy (pachydermoperiostosis):
This is a rare, familial, autosomal dominant disorder that occurs predominantly in men. However, the periostitis appears shaggy, irregular, and commonly involves epiphyses, unlike the findings in this case, making this an unlikely diagnosis. • Vascular insufficiency: The distribution of periostitis in vascular insufficiency is similar to that seen in the case under discussion, but the appearance is typically more thick and undulating. • Thyroid acropachy: The typical periostitis of thyroid acropachy appears solid and spiculated, not smooth (as in the case illustrated), and primarily involves the diaphyses of metacarpals and phalanges ( and not the long bones, as in Figure 1 0 - l SA ) . • Fluorosis: Solid, undulating periosteal tllickening (periostitis deformans) in the appendicular skeleton, somewhat similar to that in the present case, can occur in fluorosis. However, osteosclerosis of the axial skeleton, the most striking feature in fluorosis, is absent in the case illustrated. • Secondary hypertrophic osteoarthropathy (HOA): HOA is the best diagnosis because of the metaphyseal and diaphyseal involvement, soft-tissue swelling, joint pain, and history of lung cancer. + DIAGNOSIS: Hypertrophic osteoarthropathy (secondary to a previously undiagnosed recurrence of lung adenocarcinoma). + KEY FACTS CLINICAL • HOA can be secondary to a wide variety of conditions, including pulmonary ( bronchogenic carcinoma, lymphoma, abscess, bronchiectasis, cystic fibrosis, metastasis, emphysema), pleural ( mesothelioma, fibroma), cardiovascular ( cyanotic congenital heart disease, infected vascular grafts) , and gastrointestinal ( inflammatory disorders, portal or biliary cirrhosis, biliary atresia, polyposis, neoplasms) etiologies. • The pathogenesis is unknown, but neurogenic mechanisms, increased blood flow, and chemical mediators have been implicated. • Articular findings occur in about 40% of patients Witll HOA. Joint pain and swelling can be the presenting complaint. Joint effusions are common. 555 • Digital clubbing is a frequent, but nonspecific, finding. • Treatment of tlle underlying lesion (e.g., thoracotomy, chemotherapy, or radiotherapy for lung carcinoma) is often followed by rapid clinical improvement of symptoms related to HOA. • There is anecdotal evidence that regrowth of a previously treated neoplasm causing HOA is associated with worsening HOA. In the case illustrated, appearance of HOA was the first indication of a recurrence of lung carcinoma. RADIOLOGIC • Bone scintigraphy is a highly sensitive method for detecting HOA. The scintigraphic findings appear before radiographic abnormalities, correspond to clinical signs and symptoms, and regress with therapy. • The "tram track" or "parallel stripe" sign is due to diffuse cortical radio tracer uptake in tlle metaphyses and diaphyses of tubular bones that results from periosteal new bone formation. • HOA findings are typically bilateral and symmetric and primarily involve the appendicular skeleton. Less common sites include the clavicles, scapulae, pelvis, digits, and facial bones. • Increased periarticular radiotracer uptake in HOA often indicates associated synovitis. • Plain film appearance of periostitis in HOA is variable. Findings include ( 1 ) simple periosteal elevation; ( 2 ) smooth laminated ( "onion-skin" ) periostitis; ( 3 ) irregular, wavy, or solid periostitis; and (4) cortical thickening. • The periostitis of HOA begins in the diaphyses, then later involves the metaphyses and sometimes tendinous insertions. • Digital clubbing can manifest as soft-tissue swelling, with or without focal tuftal resorption or hypertrophy. • The soft-tissue swelling, periarticular osteoporosis, and joint effusions of HOA can mimic rheumatoid arthritis. However, the joint space narrowing and erosions seen in rheumatoid arthritis are not present in HOA. |
|

A 3 1 -year-old man with left side neck swelling found to have enlarged lymph nodes
on physical examination. |
DIFFERENTIAL DIAGNOSIS
• Sarcoidosis: This diagnosis is unlikely because of the absence of salivary and lacrimal gland radiotracer accumulation. • Hodgkin's lymphoma: This diagnosis is the best consideration because the abnormal radiotracer accumulation is limited to the thorax, particularly the hilum and supraclavicular regions. • Non-Hodgkin's lymphoma: This diagnosis is unlikely because the abnormal radiotracer accumulation is limited to the chest and supraclavicular region . • Opportunistic infection: This diagnosis is unlikely because abnormal radio tracer activity diffused throughout the lung parenchyma (as is typically seen in infection with Pneumocystis carinii pneumonia) would be expected. • Abdominal abscess: An abdominal process, such as an abscess, is unlikely because, as noted above, the radiotracer activity in the right abdomen has changed ( decreased) in the 96-hour study, indicating that it is due to normal colonic activity. +DIAGNOSIS: Hodgkin's lymphoma. + KBY FACTS CLINICAL • Hodgkin's lymphoma has a bimodal age distribution, with one peak around age 20 years and a second peak at age >50 years. • The most common mode of presentation is a painless mass in the neck. Constitutional symptoms include fever, weight loss, night sweats, and generalized pruritus. • Pain in an involved lymph node following alcohol ingestion is an uncommon symptom that is nonetheless rather characteristic. • An important clinical feature is the tendency of Hodgkin's lymphoma to arise within one lymph node area and spread to contiguous lymph nodes. However, late in the course of the disease, vascular invasion can lead to hematogenous dissemination. 557 • Hodgkin's disease should be distinguished pathologically from other malignant lymphomas. • Patients with stages I -A and II-A disease have 1 0-year survival rates >80%. • Patients with disseminated disease ( I II-B, IV) have a 5 -year survival rate of 50% to 60%. • Patients who relapse after chemotherapy may be cured with autologous bone marrow transplantation. |
|

A 56-year-old woman with a history of left hand laceration and tendon repair to
the left fourth and ftfth digits. Several months later she developed pain and a burning sensation in her left hand and fmgers. |
DIFFERENTIAL DIAGNOSIS
• Reflex sympathetic dystrophy syndrome (RSDS): This diagnosis is the most likely because of the clinical history of trauma, physical findings of pain and dysesthesias, and the abnormal three-phase bone scan. • Acute arthritis: This entity can produce the threephase bone scan findings seen in the case illustrated, but the periarticular radiotracer uptake pattern is usually less uniform. • Extremity immobilization: This entity can produce the bone scan findings shown above but is not associated with the dysesthesias present in this patient. • Fracture: A recent fracture of the wrist or hand can produce increased radio tracer activity on all three phases of the bone scan, but a focal abnormality, rather than the diffuse pattern seen in the case illustrated, should be present at the site of the fracture. • Osteomyelitis: The same argument against a diagnosis of fracture applies to osteomyelitis-although all three phases of the bone scan can be abnormal, a focal lesion, rather than a diffuse pattern, should be seen. + DIAGNOSIS: Reflex sympathetic dystrophy. + KEY FACTS CLINICAL • The RSDS complex consists of upper or lower extremity swelling, hyperesthesia, burning dysesthesias, hyperhidrosis, and trophic changes to the skin and bone. It occurs in both children and in adults. • The RSDS complex refers to a spectrum of clinical abnormalities, which includes variations such as causalgia (with or without evidence of peripheral nerve injury), shoulder-hand syndrome, and Sudek's atrophy of bone. Not all of the clinical manifestations of RSDS are readily encompassed by one unifYing pathophysiologic concept. • RSDS may be classified clinically as acute, dystrophic, or atrophic. • The diagnosis of RSDS is based primarily on clinical criteria. Differential neural blockade is probably the most reliable diagnostic test. Supportive evidence can also come from findings on radiographs and radionuclide bone imaging. 559 • Clinically defined nerve damage and minor soft-tissue trauma can both result in RSDS ( minor causalgia). • Therapy is based on reducing or eliminating the clinical manifestations of sympathetic hyperactivity. Varying degrees of success have been achieved using different techniques, including surgery. RADIOLOGIC • Typical findings on the three-phase bone imaging study include ( 1 ) generalized increased radiotracer perfusion on the first phase, ( 2 ) diffusely increased radiotracer with some periarticular radiotracer accumulation on the second phase, and ( 3 ) marked periarticular radio tracer uptake in the affected extremity distally ( foot or hand ) . • The three-phase bone scan i s reported t o have a sensitivity of 60% to 96% and specificity of 92% to 97%. • Occasionally, a pattern of decreased radio tracer accumulation ' both generalized and periarticular, is seen on the three-phase study. This pattern occurs more often in children. • Three scintigraphic stages of RSDS have been described. In the first stage ( up to 20 weeks), the typical three-phase bone scan findings outlined above are seen. In the second stage (20 to 60 weeks postonset), normal first- and second-phase scans are seen, but increased radio tracer in the third phase is found. The third stage ( 60 to 1 00 weeks postonset) is marked by reduced radio tracer accumulation in the first two phases, but the third phase appears normal. • Some investigators report having encountered only the typical findings of increased radiotracer on all three phases in adults. |
|
A 69-year-old man with recurrent hypercalcemia after previous parathyroidectomy
for hyperparathyroidism. Physical examination is normal. |
DIFFERENTIAL DIAGNOSIS
• Parathyroid hyperplasia: This is an unlikely diagnosis because only a single abnormality is present. Multiple foci of tracer activity would be expected with parathyroid hyperplasia. • Thyroid cancer: The absence of a palpable mass on physical examination, elevated serum calcium level, and normal image obtained 1 0 minutes after radiopharmaceutical administration make this diagnosis unlikely. • Thyroid adenoma: The history of hypercalcemia makes this diagnosis less likely. Furthermore, the abnormality on the MR image is not located within the thyroid gland but is posterior to it. • Metastatic disease to a supraclavicular node: The lack of a history of a primary malignancy and absence of other abnormalities on the MRl study make this diagnosis wuikely, although it is not excluded. However, the history of hypercalcemia in association with the neck lesion is best explained by an alternative diagnosis-namely, parathyroid adenoma. • Parathyroid adenoma: The presence of a single, focal abnormality on the Tc-99m sestamibi image in a patient with hypercalcemia makes parathyroid adenoma the most likely diagnosis. +DIAGNOSIS: Parathyroid adenoma. + KEY FACTS CLINICAL • Hyperparathyroidism is the result of increased parathormone production. Two types of hyperparathyroidism are recognized: primary and secondary. • Primary hyperparathyroidism is due to endogenous hypersecretion of parathormone, which is caused by an adenoma ( usually a solitary lesion) in 80% of cases, hyperplasia (usually of all four glands) in 1 0% to 1 5% of cases, and parathyroid carcinoma in about 5% of cases. • Secondary hyperparathyroidism results from hypocalcemia causing stimulation of the parathyroid glands and increased parathormone production. It is usually secondary to renal failure but can be seen in malabsorption and renal tubular disorders. • Tertiary hyperparathyroidism occurs when one or more glands hypertrophy due to secondary hyperparathyroidism and then function autonomously. 561 • Symptomatic patients with hyperparathyroidism and radiologic or metabolic disturbance should be treated by surgery. • Persistent hypercalcemia after surgery for hyperparathyroidism occurs in 3% to 1 0% of cases and results from failure to remove all hyperfunctioning glands. • The combination of radionuclide imaging and new parathormone assays that can be performed very quickly ( < 1 5 minutes) and, hence, intraoperatively, permit decreased operative time and help in identifYing all hyperfunctioning tissue, allowing total resection of all hyperfunctioning glands. RADIOLOGIC • The double-phase Tc-99m sestamibi study consists of early ( 1 0 to 20 minutes after radiopharmaceutical administration) and delayed (2 to 3 hours) imaging. It is very accurate in the localization of hyperfunctioning parathyroid tissue. • The double-phase technique is based on the more rapid tracer clearance from normal thyroid than from abnormal parathyroid tissue. • Tc-99m sestarnibi is more accurate in localizing abnormal parathyroid tissue than other radionuclide techniques, sonography, CT, and MRl, which are also used for this purpose. • The detection rate of abnormal parathyroid tissue depends on gland size. Adenomas are generally larger than hyperplastic glands ( frequently > 500 mg) and thus more accurately detected. • Tc-99m sestamibi is very accurate in detecting ectopic parathyroid glands that cause hyperparathyroidism, but the abnormality must be in the field of view of the study. Parallel-hole, high-resolution collimation is used to ensure that the neck and upper chest are in the field of view. • Thyroid adenomas, tl1yroid carcinomas, and lymph nodes involved with sarcoid have been reported to cause false-positive results on Tc-99m sestamibi imaging studies for parathyroid adenoma evaluation. |
|

A 6 1 -year-old woman with coronary artery disease, congestive heart failure, severe
peripheral vascular disease, hypertension, and a creatinine level of 2.8 mg/dl. |
High-grade obstruction: This diagnosis is unlikely
because the baseline study does not show a rising baseline renogram, as would be expected with high-grade obstruction. • Acute tubular necrosis: This diagnosis is very wllikely because of lack of a history of an appropriate precipitating event (e.g., an episode of hypotension) and because acute tubular necrosis would be expected to affect both kidneys in a symmetric fashion. • Unilateral renal artery stenosis: This is not the appropriate diagnosis because the function of both kidneys ( rather than one kidney) worsened after administration of angiotension-converting enzyme inhibitor. • Bilateral renal artery stenoses: This is the best diagnosis because the function of both kidneys decreased following enalaprilat administration. The findings in the left kidney are characteristic for severe renal artery stenosis-there is a change from an ascending/ descending pattern on the baseline cortical renogram to an ascending pattern after enalaprilat administration. The pattern in the right kidney, however, is also abnormal, with a prolonged cortical phase, significant residual tubular radio tracer activity relative to peak, and a 1 3% increase from the baseline study (which exceeds 1 0% from baseline, thereby meeting criteria for renal artery stenosis) . • Chronic renal disease not causing hypertension: This diagnosis is wilikely because of the abnormal response to the angiotension converting enzyme inhibitor. +DIAGNOSIS: Bilateral renal artery stenoses (75% right kidney and 99% left kidney). + KEY FACTS CLINICAL • Renal artery stenosis is a common cause of secondary hypertension and is present in 1% to 4% of hypertensive patients. It predominantly occurs in whites. • Renovascular hypertension is produced by excessive renin release, which itself results from a decrease in renal perfusion. • Fibromuscular hyperplasia is the etiology in 30% of patients who have renovascular hypertension ( being more common in women) and is the predominant cause of renovascular hypertension in adults <40 years. In 70% of cases, renovascular hypertension results from atherosclerotic stenosis. • The following clinical features i ncrease the likelihood that hypertension is secondary to renal artery stenosis: 563 1 . Onset at age <20 and > 5 0 years of age 2. Abdominal bruit 3. Atherosclerotic disease at other sites 4. Abrupt deterioration of renal function after the administration of angiotensin-converting enzyme inhibitors • Some patients may be managed clinically if renal function does not deteriorate. • The use of angiotensin-converting enzyme inhibitors has improved the success rate of medical therapy. However, patients witll bilateral renal artery stenosis develop marked hypotension and deterioration of renal function after administration of these agents. • Surgical treatment is generally successful, but percutaneous transluminal angioplasty is now the preferred approach for fibromuscular hyperplasia and discrete atherosclerotic lesions. RADIOLOGIC • Angiography is the gold standard diagnostic procedure for determining renal artery stenosis but has a number of drawbacks: ( 1 ) it is an invasive procedure, and (2) it provides an anatomic definition of the arterial lurninal diameter but not the physiologic significance of a stenosis- i.e., that hypertension is on a renovascular basis. Renal vein renin determination is also an invasive procedure and has not proved to be accurate in the diagnosis. • Urography and conventional radionuclide scintigraphy have an unacceptably high rate of false-negative and false-positive results in the diagnosis of renovascular hypertension. Doppler ultrasonography also has variable sensitivity and specificity in diagnosis of renovascular hypertension. • Response of hypertension to renal artery angioplasty carmot be predicted from degree of arterial stenosis alone but must be combined with provocative tests such as scintigraphy following administration of angiotensin-converting enzyme. Some patients with mild stenosis but positive angiotensin-converting enzyme inhibitor scintigraphy have substantial reduction in hypertensin following angioplasty, whereas patients with severe stenoses but negative scintigraphic studies do not generally respond to revascularization. |
|
A 76-year-old man with a transient episode of chest pain on returning to bed after
voiding during the night and an episode of unexplained syncope. He is referred for exercise stress testing and myocardial perfusion imaging. |
Myocardial infarction: Myocardial infarction would
not be expected to have normal homogeneous radiotracer uptake on the resting TI-20 1 study, making this diagnosis incorrect. • Myocardial ischemia: The development of a stressinduced perfusion defect that is not present on the resting perfusion image is the typical finding in myocardial ischemia. The findings in this case are most consistent with this diagnosis. • Attenuation artifact: Most often a problem in obese women, this artifact should be seen on both the rest and stress images. It usually involves the lower anterior wall and the antero-apex region . The defect seen in the case presented is larger than that typically seen due to attenuation artifact. Furthermore, attenuation artifact would not be expected to involve the septum, as in d1e present case. • Artifact from left bundle branch block: This electrocardiographic abnormality can create a reversible perfusion defect, but it most often involves primarily the interventricular septum and is not as extensive as the defect presented in this case. • Artifact from patient motion on the stress image: Motion artifact can create apparent perfusion defects that usually, though not exclusively, occur in the apex. This diagnosis is incorrect because the defect seen in the case presented is much more extensive than that expected from patient motion. In general, review of d1e raw data in a cine mode can often identify patient motion of a degree sufficient to create apparent perfusion defects. + DIAGNOSIS: Stress-induced myocardial ischemia in the vascular territory of the left anterior descending coronary artery. + KEY FACTS CLINICAL • The symptoms, pain location and radiation patterns, and precipitating factors of angina pectoris due to myocardial ischemia can be variable. If the clinical index of suspicion is sufficiendy high-i. e . , a > 1 0% probability that the patient has significant coronary artery disease-further evaluation is indicated. 565 • The episode of unexplained syncope in this patient is worrisome because it may have been related to transient myocardial ischemia and a potentially fatal arrhythmia. • Based on this patient's presentation and perfusion images, the diagnosis is significant coronary artery disease, which was documented at cardiac catheterization. • Prevention of myocardial infarction and left ventricular damage is a primary objective for the treatment of this patient. RADIOLOGIC • The scintigraphic findings in me case presented are me typical pattern seen wim stress-induced myocardial ischemia. A perfusion defect following stress testing mat is not seen on me resting image indicates segmental myocardial ischemia. The perfusion defect is secondary to altered blood flow during coronary artery dilatation mat occurs in response to physical (e.g., exercise) or pharmacologic (e.g., dipyridamole or dobutan1ine) stress testing. • A fixed defect at rest and stress can be caused by either myocardial infarction or artifact due to attenuation of photons by surrounding soft tissue or non cardiac structures. • Myocardial perfusion imaging can be performed with TI-20 1 alone, Tc-99m sestamibi alone, or as above, wim a combination of d1e two agents. The dual isotope technique combines me advantage of TI-201 ( the preferred single-photon radiopharmaceutical for identifying viable myocardium) and me advantage ofTc- 99m sestamibi (superior image quality following stress). The dual isotope technique also decreases overall imaging time. |
|
A 1 5-year-old boy with a 2-week history of severe lower back pain (worse on the
right) that had its onset while the patient was playing tennis. Mild point tenderness is present at IA-L5, primarily on the right side. |
DIFFERENTIAL DIAGNOSIS
• Mechanical low back pain: This entity occurs secondary to mechanical strain on paraspinal and spinal ligaments, muscles, and facet joints. Clinical findings can mimic skeletal trauma. Imaging studies are typically normal. The abnormal bone scan in the case illustrated therefore excludes this diagnosis as the sole explanation of symptoms. Instead, it indicates the presence of skeletal pathology. • Herniated lumbar disk: Symptoms and signs can make distinction of this diagnosis from other causes of low back pain difficult. CT/myelography or MRI would be needed to confirm this diagnosis. However, the bone scan would be expected to be negative, unlike the study in the case illustrated. Furthermore, the location of abnormality in the posterior elements on the bone scan makes this diagnosis unlikely. • Stress fracture of the lamina: This entity has typically been reported in runners with low back pain. The plain radiographs can be entirely normal. However, an abnormal accumulation of radiotracer would be expected to be seen in the lamina, rather than in the pars interarticularis ( as shown in Figure 1 0-24D) , making lamina fracture unlikely. • Pars interarticularis stress fracture (spondylolysis): This entity is commonly seen in athletes with low back pain. Radiographs are commonly normal but bone scan, which is more sensitive, typically shows abnormal radiotracer uptake in the region of the one or both pars interarticularis. The localization of abnormal radiotracer uptake on the SPECT bone scan in the case illustrated makes this the most likely diagnosis. • Tumor or infection: The bone scan findings are nonspecific. However, tumor or infection in the case illustrated would be unlikely to cause the small, focal, bilateral abnormalities shown. DIAGNOSIS: Bilateral stress fractures of the pars interarticularis. KEY FACTS CLINICAL • Spondylolysis refers to a break in bone continuity that results from a defect in the junction between the superior and inferior processus articularis. 567 • Spondylolysis is present in approximately 7% of individuals and as many as 50% of athletes who have low back pain. • Spondylolysis is more commonly seen in gymnasts, football linemen, and weight lifters, and it is likely due to repeated hyperflexion and hyperextension of the lumbar spine. • Spondylolysis is usually treated by conservative means (e.g., bracing and restricted activity). • Spondylolysis is one of three principal causes of spondylolisthesis, a condition characterized by the forward (or occasionally, backward) displacement of a vertebra relative to the next lowest vertebra. RADIOLOGIC • Bone scintigraphy is a more sensitive indicator of acute stress injury than plain radiography; radiographic changes may not be seen acutely even when the bone scan is abnormal. • Radionuclide bone scanning can help to determine the chronicity of fractures seen on plain radiographs. Acute fractures have increased radiotracer activity, and chronic fractures have decreased radiotracer activity. • SPECT bone imaging offers an advantage over planar scintigraphic imaging by avoiding the superimposition of bony structures that is present on planar imaging. Image contrast is improved by SPECT imaging, often allowing abnormalities to be more confidently localized by SPECT than by planar imaging. |
|
|
A 37-year-old man with severe three-vessel coronary artery disease, prior
myocardial infarction, and percutaneous transluminal coronary angioplasty presents with chest pain and cardiac enzyme elevation compatible with recurrent myocardial infarction. A multigated cardiac blood pool study showed a dilated left ventricle, multiple segmental wall motion abnormalities, and an left ventricular ejection fraction (LVEF) of 14%. He is referred for a Tl-201 myocardial perfusion study for assessment of myocardial viability. |
because of the segmental changes over time in a pattern
consistent with either infarcted, nonviable myocardium or ischemic, viable myocardium. • Hypertrophic cardiomyopathy: The marked dilatation of the left ventricle with segmentally heterogeneous distribution of radiotracer makes this diagnosis unlikely. • Ischemic cardiomyopathy: The distribution of TI-20 1 is heterogeneous, with segmental areas of diminished TI-201 uptake on the immediate image that improves over time ( indicating viable myocardium) and areas of markedly diminished TI-20 1 uptake that do not change over time (indicating nonviable myocardium). These findings, in conjwlCtion with the prior cardiac catheterization findings, make this the most likely diagnosis. • Idiopathic dilated cardiomyopathy: The left ventricle in this case is dilated, which can be seen in idiopathic dilated cardiomyopathy. However, the myocardial perfusion is more heterogeneous in this study than is typically seen in idiopathic cardiomyopathy, making this diagnosis unlikely. +DIAGNOSIS: Ischemic cardiomyopathy with areas of ischemic, viable myocardium. + KEY FACTS CLINICAL • The term stunned myocardium is used to refer to transiently dysfunctional myocardium (i.e., myocardium having impaired contractility) that is reversible after restoration of coronary artery blood flow. Stunned myocardium is seen in several settings, including ( I ) after an acute episode of myocardial ischemia (e.g., an episode of angina pectoris), and (2) after acute coronary artery occlusion reversed by thrombolytic therapy. • The term hibernating myocardium is used to refer to longstanding (but potentially reversible) dysfunctional myocardium in the resting basal state. Hibernating myocardium is seen with chronic myocardial ischemia from prolonged periods of reduction in coronary artery blood flow (i.e., in the setting of chronic coronary artery disease ) . This impaired myocardial contractility is reversible after restoration of coronary artery perfusion. • An accurate, noninvasive determination of viable (i.e., stunned or hibernating) myocardium is important for identification of myocardial segments that will benefit most from revascularization procedures. 569 • In patients with unexplained congestive heart failure, severely depressed LVEF, and no history of angina pectoris or myocardial infarction, it is important to distinguish ischemic from idiopathic left ventricular dysfunction so that appropriate therapy can be started. • Myocardial viability studies in patients with known severe multivessel coronary artery disease and left ventricular dysfunction can help to decide which revascularization procedure (i.e., complete revascularization with bypass surgery or limited revascularization with coronary angioplasty) should be performed. RADIOLOGIC • Myocardium can be confidently assumed to be viable if there is normal contractility on imaging studies that are used to assess wall motion (e.g., MUGA, first-pass radionuclide angiography, contrast ventriculography, or echocardiography) . However, if there is a resting wall motion abnormality, the status of myocardial viability (i.e., whether the myocardium is stunned, hibernating, or nonviable) cannot be reliably determined based on the wall motion abnormality alone. Segmental myocardial viability can, however, be assessed reliably using TI-20 1 myocardial perfusion imaging by either a restredistribution method or a stress-reinjection method. • An alternative imaging technique for assessment of myocardial viability is positron emission tomography ( PET) using F- 1 8 FDG, viewed by some investigators as the preferred imaging technique. Viable myocardium takes up this radio tracer, while nonviable myocardium does not take it up . Limitations include availability, cost, the need to regulate plasma glucose levels to optimize F- 1 8 FDG uptake, and regional heterogeneity of F- 1 8 FDG uptake that can occur even in normal subjects. • Same-day rest/stress myocardial perfusion imaging with Tc-99m sestamibi is another technique for assessment of myocardial viability in patients with chronic coronary artery disease and left ventricular dysfunction. However, in comparison to TI-20 1 redistribution or reinjection and F- 1 8 FDG PET, it underestimates the extent of viable myocardium |

