![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
26 Cards in this Set
- Front
- Back
|
Describe the pertinent epidemiologic features of bacterial pharyngitis
|
occurs most often in kids 5-10 y/o
highest incidence in late winter & early spring |
|
|
Describe the clinical manifestations of bacterial pharyngitis
|
- Abrupt onset of sore throat with pain on swallowing
- Nausea, vomiting (especially in children), and fever (above 102.5F) - Red, edematous, posterior pharynx, soft palate, and/or tonsils - Small pinpoint, focal or confluent areas of yellow to gray exudate are often present on tonsils - Tender, enlarged (>1 cm) anterior cervical lymph nodes |
|
|
Recall the laboratory diagnosis of bacterial pharyngitis
|
collection of specimen from throat, tonsils & area of inflammation
a. culture = plate specimen on SBA, apply bacitracin, incubates in 18-24hr, should reveal hemolytic colonies inhibited by bacitracin (5% resistant) b. Rapid latex agglutination or Enzyme immunosorbent assays (rapid strep tests) = high sensitivity & specificity |
|
|
List the important virulence factors for Streptococcus pyogenes
|
M-protein
Group A carbohydrate T antigen capsule (hyaluronic acid) peptidoglycan layer streptolysin (O & S) streptodornase NADase streptokinase hyaluronidase erythrogenic toxin (scarlet fever) chemotaxins SpyCEP (inactivates IL-8) |
|
|
Describe the appropriate therapy for Streptococcus pyogenes pharyngitis
|
Pen G IM or
Pen V oral 10 days or azithromycin or cephalexin for 10 days |
|
|
List the important virulence factors for Corynebacterium diphtheriae
|
Exotoxin (due to lysogenic B-phage w/tox+ gene)
B fragment of toxin binds to receptors, endocytosed, toxin cleaved by protease enzyme, fragment enters cytoplasm of cell, blocks protein synthesis. |
|
|
Describe the appropriate therapy for Corynebacterium diphtheriae pharyngitis
|
DTaP vaccination
passive immunization Penicillin |
|
|
A 26-year-old man presented to the emergency department with a two-day history of a sore throat. He was unable to eat solids because of pain and swelling but was tolerating liquids. He was afebrile but had taken 800 mg of ibuprofen one hour before arrival. On physical examination, a white exudate was seen on the tonsils
1. what is the Dx? 2. what was the causative organism? 3. what is an appropriate treatment? 4. why is treatment important? |
1. sore throat, pain on swallowing, fever & white exudate on swollen tonsils point to strep pharyngitis
2. group A streptococci 3. pen G IM shot 4. in order to prevent rheumatic fever |
|
|
address the common misconceptions about streptococcal pharyngitis
|
- need strep test to confirm H&P findings
- culture is still of use, but Direct Ag testing is used more often - antimicrobial treatment does not relieve symptoms - patient needs to complete entire antibiotic regimen even if symptoms improve, to prevent rheumatic fever |
|
|
describe scarlet fever
|
caused by group A strep lysogenized w/bacteriophage that causes production of erythrogenic toxin resulting in clinical presentation of:
- bright red tongue - diffuse erythmatous rash - desquamation of skin 1 week after onset pharyngitis symptoms too |
|
|
what are clinical sequelae of not treating streptococcal pharyngitis adequately
|
acute rheumatic fever
acute glomerulonephritis pediatric autoimmune neuropsychiatric disorder associated w/group A streptococci (PANDAS) - due to strep antigens mimicking self-antigens |
|
|
describe the general characteristics of strep pyogenes (Group A strep)
|
gram (+) cocci in chains
facultative anaerobe ferments glucose -> lactose catalase (-) hemolysis on SBA sensitive to bacitracin |
|
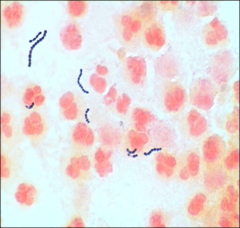
how does streptococcus pyogenes (group A strep) appear on gram stain?
|
see image
|
|
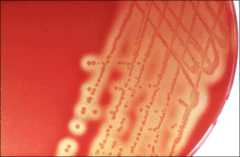
how does streptococcus pyogenes (group A strep) appear on sheep blood agar?
|
see image
|
|
|
describe the pathogenesis of strep A infection
|
pt obtains bacteria from direct contact with oral secretions and/or inhalation of droplet nuclei.
Next it attaches to mucosal epithelial cell (fibrils or M protein and lipoteichoic acid), resists phagocytosis (capsule and M protein), invades tissue (enzymes). Then causes damage via an intense inflamatory response, hemolysins and other enzymes |
|
|
define sensitivity
define specificity |
% of positives that are true positives
% of negatives that are true negatives |
|
|
how do you calculate sensitivity?
|
true pos / (true pos + false neg)
|
|
|
how do you calculate specificity?
|
true neg / (false pos + true neg)
|
|
|
define the positive predictive value
|
% true positives that are test positives
|
|
|
define the negative predictive value
|
% true negatives that are test negatives
|
|
|
describe the epidemiology of diphtheria
|
rare due to vaccination
primarily affects infants & children in the fall - transmission via saliva or inhalation of droplet nuclei - historiaccly an epidemic disease w/high mortality |
|
|
Describe the clinical manifestation of Diphtheria infection
|
sore throat, fever, pallor, listlessness, tachycardia, weakness, really bad garlic-like breath
- severe cases -> peripheral vascular collapse & death (due to toxin) |
|
|
describe the characteristics of corynebacterium diphtheriae
|
club-shapped
resemble Chinese letters stain w/methylene blue (beaded appearance) strong garlic odor |
|
|
briefly describe the pathogenesis of diphtheriae
|
Toxin is absorbed into mucous membranes → destroys epithelium and incites a strong inflammatory response.
Necrotic epithelium is imbedded with fibrin and blood cells → grayish "pseudomembrane" over tonsils. Bacteria continues to multiply → toxin absorbed into bloodstream & damages heart, liver, kidneys, adrenals, and peripheral nerves |
|
|
what other bacteria (aside from strep pyogenes & diphtheriae) can cause pharyngitis?
|
Non A beta hemolytic Streptococcus (B, C and G)
Mycoplasma pneumoniae Chlamydia pneumoniae Neisseria gonorrhoea Haemophilus influenzae type b |
|
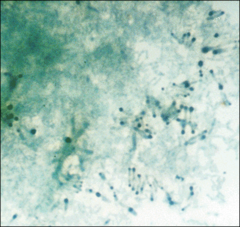
how does corynebacterium diphtheriae appear on methylene blue stain?
|
see image
|

