![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
% of salt reabsoprtion, MOA, and diuretic acting at that site for . . .
1. PCT 2. LOH 3. DCT 4. collecting duct |
1. 67%; Na/H antiporter, Na/H/2Cl symporter; carbonic anhydrase inhibitors, osmostic agents
2. 25%; Na/K/2Cl symporter; loop agents 3. 5%; NaCl symporter, Na channels; thazides 4. 3%; Na channels; KSDs, ARAs |
|
|
How do drugs that aren't filtered by the glomerulus get into the PCT?
|
organic anion transporters and organic cation transporters actively secrete drug into tubule
|
|
|
Examples of Osmotic Drugs
|
mannitol (IV), urea (IV), glycerin (PO), isosorbide (PO)
|
|
|
2 MOA's of Osmotic Drugs
|
1. limits water resorption in the PCT> increased serum osmolality > water pulled out of cells, increasing ECF volume
(only effects H2O, not electrolytes) 2. expansion of ECF > decreased renin release and blood visocisity > increased renal blood flow |
|
|
Adverse Effects of Osmotic Drugs
1. In general 2. Urea 3. Glycerin |
1. worsen volume status in pts with heart failure, ESLD, etc, cause hyponatremia initially followed by dehydration and hypernatremia, bloating/diarrhea (ex: eating too many sugar free candies)
2. extravasation/thrombosis, inducing encephalopathy in cirrhotic pts, contraindicated w/ active cranial bleeding (mannitol too) 3. hyperglycemia |
|
|
Therapeutic Uses of Osmotic Drugs
|
-reducing cerebral edema (mannitol/urea)
-prophylaxis against acute renal failure (not superior to NS/hydration) -second line (After loop drugs) therapy for oliguric renal failure -acute glaucoma attacks, perioperatively for ocular surgery |
|
|
Examples of Carbonic Anhydrase Inhibitors
|
"-amide": acetazolamide (most common), brinzolamide, dorzolamide, dichlorphenamide, methazolamide
|
|
|
Effect of Carbonic Anhydrase Inhibitors on Urinary electrolytes and pH changes
|
-NaCl: +
-NaHCO3: +++ -K: + -body pH: decreased |
|
|
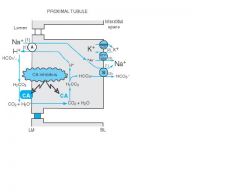
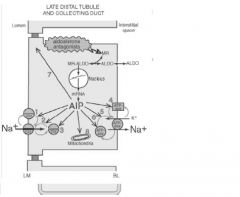
Carbonic Anhydrase MOA
1. N/K ATPase 2. N/H exchanger 3. Carbonic anhydrase (type IV) 4. Carbonic anhydrase (type II) 5. Na/HCO3 co-transporter **what happens when carbonic anhydrase inhibitor is present? |
1. provedes chemical gradient to allow Na+ resorption from lumen into interstitum
2. resorbes Na+ and secrete H+ into lumen which interacts with bicarb to form H2CO3 (carbonic acid) 3. normally carbonic anhydrase (type IV) breaks down H2CO3 into CO2 and H2O which diffuse back into cell 4. CO2 with the help of carbonic anhydrase (type II) combines with water reforming H2CO3 which freely dissociates into H+ and bicarb 5. pumps bicarb and Na+ into interstitium (aids in reabsorption of water from tubule) **filtered bicarb isn't broken down and taken back into cell > inc urine pH, dec body pH; inhibits ultimate water resorption |
|
|
Osmotic Drugs Pk
-dosing -how does it get into tubule? |
-give large doses
-passively filtered through glomerulus |
|
|
Carbonic Anhydrase Inhibitor MOA
|
|
|
|
Physiologic Effects of Carbonic Anydrase Inhibitors
1. urine and body pH 2. Na delivery to TAL 3. K and PO4 4. tachyphylaxis 5. TGF |
1. bicarbonate uria (ph 8), non-AG hyperchloremic metabolic acidosis
2. increased delivery of Na and water to TAL 3. excretion of K and PO4 4. tachyphylaxis b/c eventually less bicarb is available (needed for drug to work) 5. enhanced TGF, owing to increased Na deliver to JG (dec GFR and renal blood flow) |
|
|
Adverse Reactions of Carbonic Anhydrase Inhibitors
|
1. contain Sulfur: rash, BM suppression, interstitial nephritis
2. rare hepatotoxicity 3. drowsiness/paresthesias at high doses 4. bicarbonaturia/metabolic acidosis: NH4>NH3 may lead to encephalopathy, Ca3(PO4) precipitation (stomes), may worsen acidosis 5. PG category C |
|
|
Drug Interactions of Carbonic Anhydrase Inhibitors
|
1. weak organic bases (dextroamphetamine, quinidine) more likely non-ionized
2. weak organic acids (phenobarbital, ibuprofen) more likely ionized 3. additive hypokalemia (loops, amp B, steroids) |
|
|
Therapeutic Uses of Carbonic Anydrase Inhibitors
|
1. weak diuretics by themself (chronic use limited by tachyphylaxis and acidosis)
2. decreased intraocular pressure for glaucoma 3. anti-seizure 4. prophylaxis for altitude sickness 5. treatment of metabolic alkalosis (when giving Na isn't an option) |
|
|
Loop Agents effect on Urinary Electrolytes and pH changes
|
-NaCl: ++++
-NaHCO3: 0 -K: + -body pH: decreases |
|
|
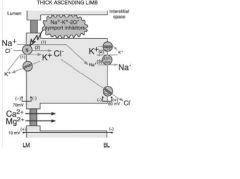
Loop MOA
|
1. inhibit Na/K/Cl symporter on luminal side (normally pumps 1Na, 1K, 2Cl- into cell)
2. minimizes Na/K/Ca/Mg/NH4 resorption 3. lack of cation resoprtion decreases interstitial osmolality decreasing the drive to resorb more water from the collecting duct 4. disrupt transepithelial potential differences (more neg cell), favoring loss of Mg and Ca |
|
|
Physiologic Effects of Loops
1. Na, Ca, Mg 2. uric acid 3. TGF 4. renin production 5. effect on blood vessels |
1. increase Na/Ca/Mg excretion
2. cause uricosuria acutely, but hyperuricemia w/ chronic use 3. TGF is negligible 4. Na flux across macula densa leads to increased renin production; exacerbated by volume depletion 5. cause vasodilation (esp frosemide) |
|
|
Examples of Loop Diuretics
|
furosemide, bumetanide, ethacrynic acid (only one w/o S), torsemide
|
|
|
Adverse Rxns of Loops
|
1. Na/volume depletion (hypotension, renal insuffiency)
2. hypokalemia (arrhythmia), hypocalcemia (tetany), hypomagnesemia (arr), metabolic alkalosis 3. ototoxicity 4. rash, photosensitvity, BM suppression 5. PG category C (except ethacrynic acid which is category B) |
|
|
Drug Interactions of Loops
|
1. AGs: ototoxicity
2. salicylates/warfarin: albumin displacement 3. anti-DM agents: hyperglycemia 4. NSAIDS: block natriuretic/diuretic effects (in Na resorption in PCT) 5. probenecid: compete for OASP (Shift dose curve to right) 6. thiazides: duresis, dehydration (sometimes combo used in pts more resistant to diuretics) |
|
|
Therapeutic Uses of Loops
|
1. CHF
2. HTN (second line- thiazides first choice b/c take less often) 3. nephrotic syndrome 4. ascites (w/ spironalactone) 5. hypercalcemia, hyponatremia (SIADH) 6. diuresis w/ significant renal disease (inc dose so you can get enough into tubule) 7. forced diuresis to minimize toxicity (uncommon) |
|
|
Thiazide Effect on Urinary Electrolytes and Body pH
|
-NaCl: ++
-NaHCO3: + -K: + -body pH: increases |
|
|
Examples of Thiazide Diuretics
|
all end in "-azide" except chlorthalidone, indapamide, metolazone
|
|
|
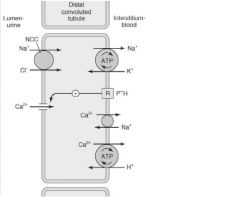
Thiazide MOA
|
1. inhibit NaCl cotransporter in DCT which prevents NaCl reabsorption
3. causes Na/Ca anti-transporter to work harder (more Ca pumped into intersititum) |
|
|
Physiological Effects of Thiazides
1. affect on collecting duct 2. TGF effect 3. effect on Ca and Mg 4. carbonic anhydrase 5. uric acid |
1. allow water resorption from CD (unlike loops) since they don't act on TAL
2. no effect of TGF, renal blood flow, or renin production 3. hypercalcemia (reduced secretion into lumen; opp of loops), hypomagnesemia |
|
|
Adverse Reactions of Thiazides
|
1. ED
2. hypovolemia, hypokalemia, hyponatremia, hypochloremia, hypomagnesemia, hyperuricemia, hypercalcemia, metabolic alkalosis 3. impaired glucose tolerance (unmask latent DM2) 4. worsened FLP (inc LDL and trigs) 5. sulfonamide allergy (rash, SJ, TEN, etc) |
|
|
Drug Interactions of Thiazides
|
1. hypokalemia (w/ concurrent agents)
2. agents that may cause SIADH and promote hyponatremia (SSRIs, vasopressin, carbamazepine, sulfonylureas) 3. Hypercalcemia (tamoxifen, calcium carbonate, calcitriol) 4. hypomagnesemia (AGs, loops, cisplatin) 5. lithium toxicity (competition for OASP) 6. volume depletion (loop + thiazide) |
|
|
Therapeutic Uses of Thiazides
|
1. edematous states (second line to loop, b/c not as potent)
2. HTN (first line) 3. Calcium nephrolithiasis (prevents Ca secretion into tubule) 4. nephrogenic diapetes insipidus (MOA unknown) 5. PG category C |
|
|
Thiazide Dosage: 25-50mg PO QD
|
-depends on what you are using drug for (anti-HTN effect at lower dose than diuretic effect)
-higher dose provides no additional benefit for HTN and may increase toxicity -start on lowest dose when combined w/ loop -ineffective w/ CrCl <30mL/min |
|
|
Examples of Potassium Sparing Drugs ( 2 classes)
|
1. potassium sparing diuretics (KSDs): tiamterene, amiloride (weak bases unlike other DUs)
2. Alodosterone receptor antagonists (ARAs): spironolactone, eplerenone |
|
|
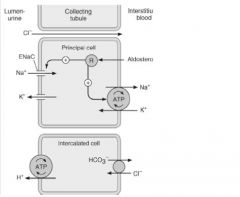
KSD MOA
|
1. block Na channels from luminal side of collecting duct
2. decreasing Na reabsorption results in less potassium excretion 3. minimizes H+ secretion by blocking membrane depolarization w/in alpha-intercalated cells (metabolic acidosis) |
|
|
ARA MOA
|
1. bind recceptors in cell cytoplasm, preventing the binding of aldosterone
2. prevents increased Na+ channel activity, upregulation of basolateral Na/K ATPase, and less permeable tight junctions induced by aldosterone 3. net result is less Na+ and water resorption |
|
|
Physiologic Effects of . . .
1. KSDs 2. ARAs |
1. eliminate lumen-negative potential, minimizing K, Mg, Ca secretion; no effect on renin/TGF
2. similar to KSDs, but natriuresis depends on endogenous levels of aldosterone (more aldosterone, more potent effect); block steroid synthesis |
|
|
Pk of KSDs and ARAs
1. triameterene and liver function 2. spironolactone 3. eplerenone oral absorption |
1. triamterene is metabolized to active metabolite by liver; bad choic for decreased liver function pts
2. spironolactone is metabolized to active metabolite (canrenone); enterohepatic circulation 3. eplerenone as oral F of 100% |
|
|
Adverse Effects of . . .
1. both KSDs and ARAs 2. only KSDs 3. only ARAs |
1. severe hyperkalemia and metabolic acidosis
2. megaloblastic anemia (triamterene inhibits folate pathway), rarely causes hyperglyc, interstitial nephritis, renal stones, photosensitivity, PG risk B (risk for placental dehydration) 3. decreased steroids (gynecomastia, impotence, etc- eplerenone may have fewer anti-androgen SEs), diarrhea/gastritis (spiron- caution in PUD), eplerenone not used w/ CrCl <50, spiron PG class D, Eplerenone PG class B |
|
|
KSD Effect on Urine Electrolytes and Body pH
|
1. NaCl: +
2. NaHCO3: + 3. K: 0 4. body ph: decreases (minimizes H+ secretion) |
|
|
Drug Interactions of KSDs and ARAs
|
drugs that increase risk of hyperkalemia (ACE inhibitors, K+ supplements, NSAIDs)
|
|
|
Therapeutic Uses of KSDs
|
1. minor diurect role (only 3% Na load available)
2. used in conjuction w/ potent diuretic (loops) to minimize hypokalemia 3. aerosolized amiloride: assists CF pts w/ mucociliary clearance 4. diabetes insipidus secondary to lithium toxicity (blocks lithium transport into tubule) |
|
|
Therapeutic Uses of ARAs
|
1. combo w/ potent diuretics to minimize hypokalemia
2. spironolactone for Class III/IV CHF 3. primary and secondary hyperaldosteronism (cirrhosis w/ ascites, nephrotic syndrome, etc) 4. eplerenone for CHF post-MI or HTN |
|
|
ADH/Vasopressin
1. how's is produced 2. what stimulates it's release 3. what inhibits it's release 4. what happens to urine w/ increased ADH release |
1. made by supraoptic and paraventricular nuclei, then transported to posterior pituitary
2. hyperosmolality (>280mOsm/L) and hypotension/hypovolemia (also angiotensin II/III, vincristine, cyclophosphamide, TCAs, nicotine, epinephrine, SSRIs can inc release) 3. ethanol, phenytoin, glucocorticoids, fluphenazine, haloperidol, promethazine, butorphanol 4. ADH increases osmolality of urine (more water resorption) |
|
|
Physiologic Effects of ADH
1. V1 2. V2 3. body temp 4. procoagulants 5. contractions of... |
1. constriction promotes max solute concentration capcity in medullary
2. increased water reabsorption 3. natural antipyretic factor 4. increases concentrations of factor VIII, and vWF 5. uterine and GI contractions |
|
|
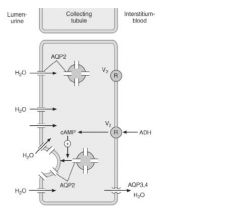
ADH action on kidney
|
1. ADH binds V2 and causes stimulation via G protein and inc cAMP production
2. aquoaporins (AQP2) form in luminal membrane allowing water to be resorbed 3. inc permeability of collecting duct to urea 4. stimulates NaCl resorption in TAL, DT, and collecting duct |
|
|
Therapeutic Uses of ADH
|
1. Central Diabetes Insipidus: give ADH preparations (pitressin, desmopressin)
2. Nephrogenic Diabetes Insipidus: remove offending drugs, consider amiloride for Li-induced DI, thiazides reduce urine volume |
|
|
Adverse Effects of ADH
|
1. nasal irritation
2. V1 mediated: cutaneous vasoconstriction and facial pallor, N, belching, cramping, urge to defecate 3. V2 mediated: water intoxication (hyponatremia) |
|
|
Tolvaptan (new drug; $312-625 per day!)
1. MOA 2. therapeutic uses 3. drug interactions 4. boxed warning 5. contraindications |
1. selective V2 antagonist in collecting duct (dec water resorption, inc serum Na)
2. treating significant hyponatremia (hypervolemic- CHF, liver disease, euvolemic- SIADH) 3. substrate for CYP3A and Pqp 4. only start in hospital to decrease risk of overly rapid correction of serum Na 5. inhability of pt to respond to thirst, hypovolemic hyponatremia (V/D), hypotension, renal failure, concomitant use w/ strong CYP3a inhibitor |
|
|
Loops MOA
|
|
|
|
Thiazide MOA
|
|
|
|
KSD MOA
|
|
|
|
ARA MOA
|
|
|
|
ADH MOA
|
|

