![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
Only 10% of blood flow to the kidney ends up in the?
what is the reason for that? p02 in that area is? |
-medulla
-vasa recta are sparse -low pO2, vulnerable to hypoxic damage |
|
|
morphology of the glomerular capillaries?
relation to the peritubular capillaries? increased filtration (inc. movement of particles OUT of capillary) in the glomerular capillary means what for the peritubular capillaries? |
-glomerular capillaries are more porous than peripheral capillaries (more filtration)
-glomerular capillaries are in series with the peritubular capillaries -increased filtration in the glomerular capillary means increased colloid osmotic pressure at the end of the glomerular capillary and, therefore, in the peritubular capillaries |
|
|
GFR defined as?
|
sum of Starling forces Pf (net filtration pressure) multiplied by Kf (glomerular filtration coefficient):
Kf x (PGC-PBS-colloid oncotic glomerular capillary P) |
|
|
is colloid osmotic pressure constant along the length of the glomerular capillaries? is the hydrostatic P constant?
|
-NO! hydrostatic P is constant and albumin is unfiltered the colloid osmotic pressure rises along the length of the capillary
|
|
|
what happens to Pf as you progress down the length of the capillary?
end point of Pf at the end of glomerulus? this point is called? |
-Pf decreases as colloid osmotic pressure increases until Pf decreases to a point where filtration stops because there is no gradient (filtration equilibrium)
|
|
|
Since hydrostatic P drops across the efferent arteriole, starling forces now favor?
|
-Starling forces favor re-uptake of water and solute by the peritubular capillaries
|
|
|
as blood flows along the glomerular capillary from afferent to efferent what happens to the colloid osmotic P? why?
how is oncotic P related to plasma protein (albumin) and filtrate? |
-colloid osmotic pressure increases as plasma protein concentration inc (as ultrafiltrate leaves the capillary)
-oncotic P directly related to plasma protein, indirectly related to filtrate |
|
|
with increased renal plasma flow, what happens to the contact time between the blood and tubules? what happens to the oncotic P? GFR? Pf?
when renal plasma flow declines? |
-when RPF inc., less filtrate leaves the blood, oncotic P decreases (plasma protein is diluted), GFR inc. and Pf inc (because of decreased oncotic P)
-when RPF decreases, more filtrate is taken out of the blood-->oncotic pressure increases, GFR dec and Pf dec |
|
|
what is the primarily regulator of Pgc?
-effect of increased afferent arteriolar resistance on Pgc and GFR? -effect of increased efferent arteriolar resistance on Pgc and GFR? |
-afferent and efferent arteriole resistance
-inc. afferent arteriolar resistance dec. Pgc and GFR -inc. efferent arteriolar resistance inc. Pgc and inc. GFR |
|
|
effect of contracting mesangial cells on GFR and Kf?
effect of relaxing mesangial cells on GFR and Kf? |
-contracting mesangial cells-->dec. Kf, dec. GFR
-relaxing mesangial cells-->inc. GFR and inc. Kf |
|
|
autoregulation=?
how is autoregulation achieved? |
-ability of the kidney to regulate itself and maintain a constant RBF and GFR over wide range of BP
-autoregulation achieved by tubuloglomerular feedback |
|
|
How does the tubuloglomerular feedback work with increased systemic BP?
effect on RBF and GFR? |
-inc. BP inc. RBF and GFR. This increases delivery of NaCl to the macula densa in the DT. This increases the production of vasoactive substances and increases afferent arteriolar constriction to protect the glomerulus from HTN and keep RBF and GFR constant
|
|
|
Neural factors controlling tubuloglomerular feedback? effect on GFR and RBF?
|
-NE innervates afferent and efferent arteriole vasoconstriction-->dec. RBF and GFR
|
|
|
Hormonal factors controlling tubuloglomerular feedback?
-Angiotensin II -PTH -Vasopressin -Endothelin 1 -Adenosine -NO -Prostaglandins |
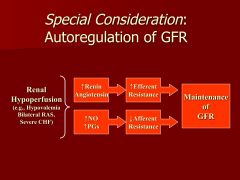
-Angiotensin II: inc. efferent resistance>>afferent-->inc. Pgc
-PTH: dec. GFR by dec. Kf -Vasopressin: contracts mesangial cells and dec. Kf -Endothelin 1: potent vasoconstrictor of afferent and efferent arterioles-->dec. RBF and GFR -Adenosine: dec. GFR because of inc. preglomerular vascular resistance and dec. efferent arteriolar resistance -NO: NO inc. RBF and GFR by dec. afferent and efferent resistance (counteract angiotensin II and NE) -Prostaglandins: vasodilatory, lower afferent arterial resistance and inc. RBF; synthesis stimulated by angiotensin II! |
|
|
Renal Failure from reduction in renal perfusion; if prerenal, referred to as?
Hypovolemia causes prerenal failure by reduced aterial filling (intravascular volume can be nl or increased)? -cardiac failure? renal response? -liver cirrhosis? -sepsis? early? late? |
-Prerenal azotemia
-cardiac failure: dec. in cardiac fxn-->low CO-->low renal perfusion-->retention of salt and water -liver cirrhosis: profound reduction in peripheral vascular resistance (vasodilation of the splanchnic vessels)-->renal response to hypovolemia -sepsis: profound drop in PVR and arterial filling, BP maintained early on by elevated CO; later on myocardial fxn depressed-->hypotension |
|
|
response to pre-renal azotemia?
-sympathetic activity? -tubular sodium reabsorption? -renin release? |
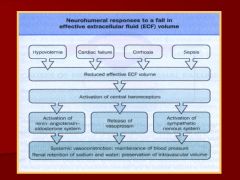
-inc. symp activity-->arterial vasoconstriction, inc. renin release
-angiotensin II and aldosterone inc. tubular sodium reabsorption |
|
|
Renal Vascular Obstruction
effect of renal artery embolism/thrombosis and renal vein thrombosis on RBF and GFR? result? |
-renal artery embolism/thrombosis and renal vein thrombosis can result in abrupt cessation of RBF and GFR
|
|
|
Renal artery stenosis effect on RBF and GFR? initially?
renin release? Ang II? systemic result? RBF and GFR constant until? |
-initially, renal artery stenosis dec. RBF and GFR but autoregulation corrects
-Renin release is increased in response to low RBF, elevated Ang II-->efferent arteriole resistance inc. GFR -systemic result=HTN -RBF and GFR are constant until renal artery lumen reduced more than 75%; autoregulation surpassed, GFR falls |
|
|
Altered Renal Vascular Resistance
-ACE-i effect? -NSAID effect? |
-ACE-i: with decreased blood flow, GFR is dependent on vasoconstriction of the efferent arteriole by Angiotensin II-->ACE-i cause reduced hydrostatic P and reduced GFR
-NSAID: NSAIDs inhibit Prostaglandins, PGE2 help preserve RBF and GFR by vasodilating afferent arterioles; with NSAIDS, there is unopposed vasoconstriction-->reduce Pgc and GFR |
|
|
gold standard for diagnosing prerenal azotemia=?
PE? Urine signs? |
-if restoring arterial filling returns GFR to normal!
-hypovolemic/hypervolemic signs (CHF, hepatic cirrhosis) -urine: ADH released-->urine specific gravity and urine osmolality high, increased reabsorption of urea (BUN high), low urinary sodium |
|
|
how can you distinguish true high urinary sodium from water reabsorption?
equation? below 1%=? 2%-3%? |
FENa!
UNa/PNa / UCr/PCr x 100 FENa reflects ONLY tubular sodium reabsorption -below 1%=prerenal disease -excess Na lost; ATN or renal disease |
|
|
correct CHF or liver cirrhosis with?
|
diuresis
|

