![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
Aortic dissection |
• deterioriation of medial collagen and elastin • a tear in the intimal layer allows blood to enter theintima-media space • blood propagates down this new space creating a true and a flase lumen • begins proximal aorta just above the valve typeA • begins at the site beyond the origin of the left subclavian artery typeB |
|
|
Factors predisposing to dissection of the aorta |
- hypertention - Marfan and Ehler-Danlos - coarctation and bicuspid aortic valve - pregnancy - trauma - perforation theough an intimal atheromatous plaquesigns |
|
|
Signs and symptoms of aortic dissection |
•Sever chest pain with sudden onset progressing to the abdominal and hip areas •Partial or complete occlusion of the areas arising from the aortic arch •Peripheral pulses and BP may be diminished or unequal •Aortic diastolic murmur may develop if the dissection is typeA resulting in AR, HF and cardiac tamponade |
|
|
Imaging findings in aortic dissection |
• X-ray: wide superior mediastinum, pleural or pericardial effusion • CT & MRI too time consuming • immediate angio: needed by surgeons preoperatively • TEE: diagnostic study of choice • ECG: LVH from long-standing HTA |
|
|
TEE in aortic dissection |
• hallmark: dissection flap and entry site • dilated aorta • aortic insufficiency • pericardial and/or pleural effusion |
|
|
Complications of aortic dissection |
-rupture -tamponade -AR -coronary artery involvement -other brach vessel involvement |
|
|
Mechanism of AR development in aortic dissection |
1. Dilation of aortic root 2. Pressure from dissecting hematoma may depress one leaflet 3. Torn annular support of the leaflet 4. Intimal flap prolapse |
|
|
Pulseloss in aortic dissection |
- due to direct compression - blockade due to flap of intima |
|
|
Differential diagnosis of aortic dissection |
- myocardial infarction - pulmonary embolism - renal-visceral ischemia |
|
|
Treatment of aortic dissection |
1. Lower BP to 100mmHg - iv Nitroprusside 0.5 mL/min - iv Trimetaphan 1-2 mg/mL - iv Metoprolol or Propranolol 0.15 mg/kg given 5 min and repeated to keep pulse 60/min 2. Surgery |
|
|
Surgical guide in aortic dissection |
- if pain is not relieved - if significant occlusion of a major brach of the aorta develops - if progressive aortic enlargement or rupture occurs - all typeA cases |
|
|
Surgical approach in aortic dissection |
TypeA: may involve aortic valve and arch replacement with re-attachement of the coronaries and brachiocephalic vessels. >20% mortality TpyeB: surgical removal of the origin, closing the false lumen, graft insertion. Higher mortality than typeA No surgery: permanent medical therapy (betablockers/antiHTA) |
|
|
Prognosis of aortic dissection |
- without treatment 90% in 3months - surgical mortality is higher in typeB bcz of comorbid illness - survival without treatment usually due to re-canalization |
|
|
Aortic aneurysm |
Pathological dilatation of the normal aortic lumen involving one or several segments. -fusiform(common) -saccular -pseudoaneurysm: well defined collection of blood and connective tissue outside the vessel wall |
|
|
Thoracic aortic aneurysm |
•40% asymptomatic •pain •symptoms due to mass effect - superior vena cava syndrome, tracheal deviation • surgery if >5cm (mean expansion rate=0.43 cm/year) •op risk 5% |
|
|
Atherosclerotic occlusive disease |
- of the aorta and its braches - common couse of disability - smoking is high risk factor - serum cholesterol should be determined - Predictor for morbidity in patient with cardiac disease and undergoing general surgery - manifests in men >50y |
|
|
Clinical findings in atherosclerotic occlusive disease |
- ankle pressure > arm - no change in BP during excersize - in limbs there is a reduced distal pressure - at rest the mesured BP at the ankle is less than normal |
|
|
Occlusive disease of the aorta and iliac arteries |
-begins proximal to the bifurcation of the common iliac arteries or distal to the bifurcation of the aorta - abrupt worsening of limb ischemia symptoms associated with plaque rupture |
|
|
Clinical findings in atherosclerotic iliac artery disease |
-intermittent claudication -impotence -rest pain -femoral pulses are absent or very weak, distal pulses are often impalpable -bruit may be heard over the aorta or iliac femoral arteries -sBP higher in brachial artery than in the ankle -atrophic changes of skin and muscles -PAOD (peripheral arterial occlusive disease) like ischemic gangrenes |
|
|
Fontaine staging of occlusive atherosclerotic diease |
I.: asymptomatic IIa: mild claudication IIb: moderate to severe claudication III.: ischemic rest pain IV.: ulceration or gangrene |
|
|
Rutherford grade system in atherosclerotic occlusive disease |
0/0: asymptomatic I/1: mild clau. I/2: moderate clau. I/3: severe clau. II/4: ischemic rest pain III/5: minor tissue loss III/6: major tissue loss |
|
|
Treatment of occlusive arterial disease |
-surgical -angioplasic -stop smoking -conservative care -arterial graft (prothesis) -thrombendarterectomy -percutaneous transluminal angioplasty |
|
|
Conservative care in occlusive arterial disease |
-daily walking -Cilostazol 2x10 mg/day -Pentoxyphylline 400 mg 3xday -limited use of beta-blockers (except BB with peripheral vasodilator effect like Nebivolol) -Clopidogrel, antiplatelet -Statins |
|
|
Occlusion in an extremity causes |
-pain -numbness -tingling -weakness -coldness -pallor -motor, reflex and sensory alteration -pulselessness -symptoms vary according to the side |
|
|
Occlusion in an extremity causes |
-pain -numbness -tingling -weakness -coldness -pallor -motor, reflex and sensory alteration -pulselessness -symptoms vary according to the side |
|
|
Acute limb ischemia: |
-sudden decrease in perfusion that thratens limb viability and requires urgent management -prompt diagnosis/revascularization with catheter-based thrombolysis or thrombectomy or surgical reconstruction/amputation(10-15%) -15-20% die in 1 year from coexisting conditions |
|
|
Causes of acute limb ischemia |
- acute thrombosis - embolism - dissection - trauma |
|
|
6 Ps |
Paresthesia Pain Pallor Pulselessness Poikilothermia Paralysis |
|
|
6 Ps |
Paresthesia Pain Pallor Pulselessness Poikilothermia Paralysis |
|
|
Poikilothermia |
Impaired regulation of body temerature with the temperature of the limb usually cool, reflecting the ambient temperature |
|
|
Arterial embolism |
-complication of heart disease (IHD or Reumatic HD with or without MI) -AFib is often present -emboli tend to lodge at the bifurcation of major arteries -carotid system is involved in 20% also mesenteric and upper extremity |
|
|
Arterial embolism |
-complication of heart disease (IHD or Reumatic HD with or without MI) -AFib is often present -emboli tend to lodge at the bifurcation of major arteries -carotid system is involved in 20% also mesenteric and upper extremity |
|
|
Clinical findings in arterial embolism |
-pain (sudden or gradual), numbness, coldness —> symptoms -pulselessness distal to the block, coldness, pallor, hypoesthesia/anesthesia, weakness/paralysis —> signs - superficial vein collapsed - skin necrosis/ gangrene |
|
|
Treatment of arterial embolism |
-immediate embolectomy 4-6h - heparin 5000 U iv - extremity kept below the horizontal plane - angiography/ECHO |
|
|
Surgical treatment of arterial embolism |
- local anesthesia - remove embolus by Fogarty catheter - heparin for a week or more - prolonged anticoagulation with warfarin - delayed embolectomy —> acute respiratory distress syndrome or acute renal failure |
|
|
Algorithm for diagnosis and treatment of acute limb ischemia |
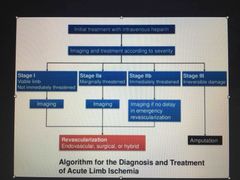
Back (Definition) |
|
|
Thrombophlebitis |
- is a partial or complete occlusion of a vein by a thrombus with secondary inflammatory reaction in the wall of the vein - trauma to the endothelium -pletelet aggregation, deposition of fibrin, leukocytes, erythrocytes forming a thrombus which may result a a free-floating clot -in 7-10 days the thrombus becomes adherent to the vein wall and secondary inflammation occurs -thrombus is invaded by fibroblasts, resulting in scarring and destruction of the valves -central recanalisation may occur later but valve wont recover -- directional flow disturbances |
|
|
Virchows triad |
-Stasis -vessel dmamge -activation of coagulation |
|
|
Risks for deep vein thrombophlebitis |
- CHF history -recent surgenry -neoplasia (adenocarcinomas of the pancreas,prostate,breast,ovary) -oral contraceptive use -varicos veins -prolonged inactivity -smoking -cardiac failure,stroke |
|
|
Rare conditions that may cause DVT |
-protein C and S deficiency -antithrombin III def. |
|
|
Symptoms of DVT |
-dull ache -tight feeling -frank pain especially while walking |
|
|
Signs of DVT |
-slight swelling -distention of the superficial venous collaterals -slight fever - tachicardia -tenderness & swelling when femoral/iliac veins are involved -cyanosis |
|
|
Lab tests of DVT |
-PPT/INR -ESR -D-dimer -ABG -protein C, S, antithrombin III |
|
|
Diagnostic techniques of DVT |
1. Ascending contrast venography (most accurate, define location/extent/degree) 2. Doppler US (rapid screening procedure) |
|
|
Differential diagnosis of DVT |
-calf muscle strain -cellulitis -obstruction of the lymphatics or the iliac vein (painless, unilateral swelling) -acute arterial occlusion (painfull, absent distal pulse, no swelling) -bilateral leg edema |
|
|
Complications of DVT |
-pulmonar thromboembolism -chronic venous insufficiency |
|
|
Prevention of DVT |
1. Non pharmacologic: -elevation of foot -leg excersise -elastic antiphlebitic stocking -walking 2. Anticoagulation -low-dose Heparin 5000 U every 8-12h (LMWH) -Aspirin 80-325 mg |
|
|
Prognosis of DVT |
- 3-6weeks returning to normal - good if underlying cause is abolished - occasionally reccurence occures - chronic venous insufficiency may result with its complications |

