![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
244 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
general organization of the digestive tract
|
consists of the alimentary canal from the mouth to the anus
includes organs/glands that empty there secreation in the canal |
|
|
|
accessory organs and glands
|
salivary glands- saliva (1st line defense)
stomach- gastric juice (2nd line of defense) HCL liver and biliary tract- bile (prevent jaundice digest fat) pancreas- electrolyte and enzymes intestine- electrolyte |
|
|
|
design of the digestive tract
|
take in food and convert it into simple soluble substances that can be easily absorbed
|
|
|
|
function of the digestive tract
|
peristaltic, segmentation mass movement and other movements
synthesis & release of secreation and also hormones digestion and absorption excretion |
|
|
|
lining of the GIT
|
upper 1/3-2/3 oesophagus and the external ani sphincter- STRIATED
most lined by smooth muscles |
|
|
|
histological organization of the GIT |
serous- absent in the esophagus and distal rectum Muscles Submucosa Mucosa
|
|
|
|
splanchnic circulation
|
combined vascular bed of the liver, stomach and intestine
superior mesenteric coelic artery (80%) |
|
|
|
myenteric plexus(Auerbach plexus) from the enteric nervous system
|
between middle circulars and outer longitudinal
peristalsis and other mother activity |
|
|
|
motor neurons
|
innervate smooth muscles to elicit movement
|
|
|
|
sensory neurons
|
respond to stretch, toxicity and chemical
|
|
|
|
endocrine secreation
|
hormones release in respond to specific stimulus
cck, Motilin, secretin, gip, gastrin |
|
|
|
neurocrine secreation
|
peptide are release at nerve endings
VIP, GRP and enkephalins |
|
|
|
paracrine secreation
|
substances that acts as local mediators
histamine and somatostatin |
|
|
|
submucosal plexus
|
between submucosa and muscularis propria
exocrine and endocrine functions |
|
|
|
control centers of the muscles of mastication
|
brain stem
cerebral cortex hypothalamus amygdala |
|
|
|
chewing reflex
|
initiated by the presence of food in the mouth
reflex inhibition of the muscles of mastication causing the jaw to drop stretching of the jaw muscles contraction of the muscles of mastication causing a raise in the lower jaw closure of the teeth food compress against the lining of the mouth |
|
|
|
mastication |
food is mechanical broken up prior to being swallowed |
|
|
|
function of mastication
|
aids in the digestive process
allows digestive enzymes to act on larger areas of food helps to prevent damage to the gut wall increases the ease of emptying and movement of food through the gut |
|
|
|
deglutition (swallowing)
|
reflex action which allows the delivery of air, liquid and solid from the mouth to the stomach
|
|
|
|
voluntary stage of swallowing buccal |
occurs in the mouth food is squeez and rolled by the tongue tongue presses the bolus upwards and backward against the hard palate towards thw soft palate into the oropharynx |
|
|
|
involuntary stage of swallowing(pharyngeal stage) closure of the nasopharynx |
contraction of the tensor and levator Palatin elevation of the soft palat breathing stop for 3-10s superior contrictor muscle contracts to form the RIDGE OF PASSAVANT (tight seal, initiate the pharyngeal peristaltic wave and propels the bolus through the pharynx) palatopharyngeal folds forms a sacral slit allowing food to pass with ease allows properly masticated food to enter the esophagus
|
|
|
|
involuntary stage of swallowing(pharyngeal stage) closure of the larynx |
hyoid bone raised upwards and forward move the larynx forward brings it under the base of the tongue achieve by contraction of the geniohyoid and mylohyoid muscles epiglottis swings backwards Breathing stop for like a second |
|
|
|
involuntary stage of swallowing(esophageal stage)
|
closed at the upper end by the UOS (cricopharyngeal sphincter)
opening of UOS is achieved by elevation of the hyoid bone, relaxation of the cricopharyngeal sphincter and peristaltic wave stretching of the myenteric plexus initiate primary peristaltic wave retained food causes distension of the myenteric plexus give rise to secondary peristaltic wave |
|
|
|
when is swallowing complete
|
when LOS opens and material empties into the stomach
|
|
|
|
diseases of the sphincter
|
achalasia
incompetent LOS (heartburn) |
|
|
|
damage to the nerve supply
|
V IX and X by poliomyelitis
encephalitis |
|
|
|
defective muscle function
|
myasthenia gravis
muscle dystrophy |
|
|
|
other defects
|
glottis remains open e.g. anaesthesia
nasopharynx not close |
|
|
|
saliva |
1st secreation to begin the breakdown of food hypotonic ph7-8 contain water, electrolyte and high concentration of K+ Neural regulations |
|
|
|
function of saliva
|
moistens food and aids speech
facilitate chewing and swallowing maintain oral hygiene due to its bacterial properties reduce Ca2+ loss from teeth and secrets F- dilutes and neutralize acids, buffers sudden changes in pH provide evaporative cooling begin starch and fat digestion contains hormones |
8
|
|
|
functional unit of salivary gland
|
salivon
acini of salivon produce the 1' secreation of saliva ducts modify by striated cell the secreation to a 2' secreation contractions of the myoepithelial cells expel saliva from the acini into ducts |
|
|
|
primary secreation from acini |

rich in: enzymes(amylase) mucins(glycoprotein that lubricate food) isotonic Cl- is actively secreted Na is actively extruded into the lumen Cl- diffusers in the lumen along with HCO3 Na-H exchanger drive secretion of HCO3 |
|
|
|
secondary secreation from ducts |

hypotonic ducts are impermeable to water Cl- in exchange for HCO- Na+ is reabsorbe(removed from the solution by ATPase) K+ is secreted in exchange with H Na-H Drive the exchanger of for Cl-HCO3 in the basalateral area |
|
|
|
transporters modify the 1' acinar secreation
|
apical Na+-H+ excganger
apical Cl-HCO- exchanger Cl- exits the basolateral membrane via CL- channel basolateral Na-H exchanger drives the Cl-HCO exchange in the apical membrane |
|
|
|
siliva at low rate |
Na+Cl- decrease K+ increase significantly saliva become hypotonic and rich in K+ and HCO- |
|
|
|
siliva at high secreation |
Na+ Cl- increase less time for secreation of K+ HCO- remain high saliva reach isotonic rich in Na+Cl |
|
|
|
function of saliva
|
protection
digestion lubrication |
3
|
|
|
regulation of salivary secreation |
sympathetic and parasympathtic both neural mediated parasympathetic increase acinar cells to realise kallikrein which causes lyso bradykine to be produce which cause vasodilation that increase blood flow to the gland VIP cause vasodilation |
|
|
|
hormones that modify the composition in saliva |
ADH and ALDOSTERONE |
|
|
|
function of the stomach
|
store large quantities of food
mixes food with gastric secreation to form semi solid mixture of chyme allows for slow and timely emptying of chyme in the small intestine for proper absorption and digestion secretes HCL pepsinogen mucous IF begin protein digestion HCL helps destroy invading organisms IF allows for the absorption of Fe and VitB12 |
7
|
|
|
Gastrectomy |
partial or full surgical removal of the stomach results in Cyanocobalmin (VitB12) Parental IF deficiency Fe deficiency anaemia Dumping syndrome |
|
|
|
Dumping syndrome
|
hypoglycemia- pancreas release a lot of insulin so will be rapid uptake of glucose
hypovolemia- because the material being dumped in the intestine would be more hypersonic its going to pull water from the EFF into the intestine to make it isotonic hence there is going to be a reduction in blood volume hypotension-because of the reduction in blood volume activated the sympathetic nervous system causing tachycardia |
|
|
|
proximal motor unit of the stomach |
body fundus cardia accommodate ingested food reserve for incoming food main regulator of intragastric pressure excitatory and inhibition(VIP NO)
|
|
|
|
distal motor unit of the stomach
|
antrum pylori antral pump
function as a integrated unit peristaltic pump for outgoing chyme contain pacemaker cells that set the pace caval excitatory |
|
|
|
gastric filling |
occurs in the proximal motor unit Triggered by swallowing triggered by peristalsis occurring throughout the pharynx and esophagus intragastric pressure remains constant Receptive relaxation
|
|
|
|
laplace's law |
P=2T-tensions R-radius constant stretch of smooth muscle cause a decrease in tension Vago-vagal inhibitory reflex |
|
|
|
gastric emptying |
as food is collected in the stomach rhythmic peristaltic wave arise in the DMU contraction waves mix and squirt the chyme into the duodenum at a controlled rate peristaltic contractions begins in the mid stomach contractions arise from BER (basic electrical rhythm)or gastric slow waves pacemaker cells present in the fundus and body |
|
|
|
constrictor waves
|
ringed contraction of the circular muscle layer arises in the mid stomach
move towards the gastroduodenal junction cause evacuation of some content into the duodenum most of the contents are passed over and then forced back into the body of the stomach |
|
|
|
retropulsion |
food lying in the core is forced back in the stomach allows for grinding and mixing of food contractions of the pylori persist longer than that of the duodenum serves to prevent regurgitation |
|
|
|
factors affecting gastric emptying
|
antral pump
pylori resistance |
|
|
|
factors affecting antral pump
|
duodenal chyme
hormones inhibition- GIP secretin glycogen CCK activated- gastric motilin |
|
|
|
secreatory neurons
|
regulates endocrine and exocrine secreation
|
|
|
|
Gastric juice |
Isotonic solution rich in H+ pH 1-2 2L/day
|
|
|
|
Gastric gland |
Tubular gland found in the body of the stomach Contain surface epithelial cells Mucous neck cells- protective Chief cells- pepsinogen HCL split it to Pepsin 1 (pH2) pepsin 2 (pH3) Parietal- HCL and IF |
|
|
|
APUD amine precursor uptake and decarboxylation |
Found in the base of the gastric gland Produce GI Hormones |
|
|
|
Pyloric gland |
Present in the antrum Secrete mucus mainly G-cells secrete gastrin D-cell secrete somatostatin S-cell secrete secretin |
|
|
|
Gastric acid |
pH 0.87 Rich in H+ |
|
|
|
Formation of HCL |
Formed at the membran of the canaliculi and shunted out through opening at the apex of the gland Needs a lot of mitochondria |
|
|
|
H+ are from |
Cytochrome oxidase system- pumps H+ in the canilicula Dissociation of water Dissociation of carbonic acid- contain carbonic anhydrase to split it it create bicarbonate ions to at buffer the acid |
|
|
|
Mucus cells |
Secreation of bicarbonate ions to neutralize the acid buffer the acid Prostoglandins inhibite cAMP hence inhibiting Cl which inhibit HCL secretion Sticky viscous Neck cell |
|
|
|
Gastric mucosal barrier |
When it is breach peptic ulcer formation Protect the stomach and prevent ulcer formation |
|
|
|
Mechanism of acid secreation |
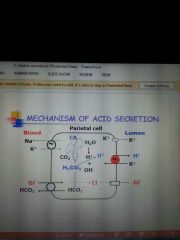
Na+K- ATPase pump in the basolateral area if the cell pump out Na+ and replace it with K-
Base of the cell exchange Cl- for bicarbonate ions
Cl- ions move in the cell creat and electropotential which create a negative potential in the lumen and then its shift out of the cell called Cl shift cause K to enter the canaliculi Bicarbonate is pumped out the cell by facilitated transport and exchange for Cl-
When K is in the lumen H+/K+ ATPase pump at the apex exchange k for H
|
|
|
|
Regulation of acid secreation |
Neurohumoral regulation Occurs in 3 phases Cephalic phase- shortest in respond to meal Gastric phase- longest Intestinal phase |
|
|
|
Cephalic phase of gastric secreation |
Neural mediated Conditioned reflexes and neurogenic signals from cerebral cortex and appetite centers in the hypothalamus Direct vagal stimulus |
|
|
|
Gastric phase in gastric secreation |
Neurohumorally Distention of the stomach and products of protein digestion Gastrin+ vagovagal excitoray reflex |
|
|
|
Intestinal phase of gastric secreation |
Humorally Increase in acid secreation due to protein products stimulation of G cells Mainly inhibition Due to enterogastric |
|
|
|
Neurohumoral control mechanism of gastric secreation |
Acid is stimulated by- histamine via H2 sensitized the cell to gastric and Ach ACH via M3 Gastric via G receptor Gastrin stimulates histamine release from enterochromaffin like cells Prostaglandins inhibite acid secreation |
|
|
|
Regulation of acid two hormones |
Somatostatin close to G cells inhibited acid Direct paracrine inhibition on gastrin G cell Release is stimulated at antral pH less than 3 secretin released from S cells due to acid chyme entering the duodenum inhibition of acid secreation Cause large secreation of bicarbonate in the duodenum to neutralize the acid CCK and ACH cause the release increase intracellular Ca+ Works on the duct cells to release HCO Activate cAMP pH less than 4 |
|
|
|
Exocrine pancreatic secreation |
2L per day Na+ HCO- is secreated Isotonic pH 8 Protein- globulin and albumin Digestive enzymes- antitrypsin |
|
|
|
Acute pancreatitis |
Autolysis of the pancreas Activated phospolipase A2 damage the cell |
|
|
|
Zollinger Ellison syndrome |
Gastrinoma of the delta cells in the pancreas |
|
|
|
Cystic fibrosis |
Cl- channel damage |
|
|
|
Secreation through ducts |
Duct- intra lobular duct- inter lobular ducts |
|
|
|
Mechanism of bicarbonate secreation |

The solution is secreted between the central acinar cells and the gut cells Basolatrral NaH exchanger Na in and H out NaK pump pumps Na out and K in Bicarbonate is exchange at the apical cell in exchange for Cl- Cl- depends on the opening of the Cl- channels opening is activated by cAMP in response to secretin stimulation Water moves with Na hence creating an isotopic solution |
|
|
|
What happens in larger ducts of the exocrine pancreas |
Bicarbonate is reabsorbe |
|
|
|
Acinar cells |
Produce Na and Cl ions Secrets enzyme |
|
|
|
Duct cells |
Bicarbonate ions |
|
|
|
At low rate for exocrine secreation |
NaCl high because the duct cells cant produce a lot of bicarbonate ions
|
|
|
|
At high flow rates for exocrine secreation |
Na HCO |
|
|
|
Active forms of enzymes |
Alpha amylase antitrypsin Pancreatic lipase |
|
|
|
CCK in pancreas |
Secreted by I cells in the mucosa of the duodenum and jejunum fatty acids and protein stimulates the I cells causes release of acinar cells Act on acinar cells Inhibit stomach contraction At the same time it causes emptying of the bladder it slow emptying of the stomach to give adequate time for digestion of the fats |
|
|
|
Activation of enzymes |
Tripsinogen turns in trypsin by enterokinase- CCK can cause the cells to release it Trypsin then activate the other enzymes |
|
|
|
Bile salts in the pancreas |
Prolipase to lipase |
|
|
|
Regulation of the pancreas secreation |
Main regulator is the intestinal phase the largestest phase Cephalic and gastric similar to gastric phase |
|
|
|
Things from the vagal afferent |
CCK- relaxation of the sphincter of oddi gastric |
|
|
|
Intestinal phase of the pancreas |
initiated by protein fats and H entering the duodenum Secretin-H+ pH4.5 CCK- fats and proteins GIP glucagon- mainly carbohydrates |
|
|
|
Cephalic and gastric of pancreas |
ACh has a greater effect Gastrin |
|
|
|
Mechanism of enzyme regulation |
CCk and ACh potential effects of secretin They increase intracellular Ca+ via phospholipase C Secretin binding increases ardently cyclase activity to increase cAMP cAMP and Ca2+ leads to activation of kinases involved in regulating the synthesis of enzymes |
|
|
|
Blood flow in the liver |
Portal vein- central vein- hepatic vein- IVC |
|
|
|
Function of the liver |
1)Storage: fat glycogen vitamins 2)Secreation of bile 3)Metabolism of glucose/glycogen 3)Synthesis of plasma protein, transport protein, clotting protein, hormones 5)detoxification 6)immunity |
|
|
|
Excretory substances of bile |
Bile pigment Cholesterol Bilirubin Lecithin Alkali phosphate |
|
|
|
Secretory substances of bile |
Bile salt |
|
|
|
Bile |
500ml/day Isotonic pH 8 Ducts secret watery HCO rich fluid |
|
|
|
Jaundice |
Accumulation of free or conjugated bilirubin in the blood, skin, secular and mucus membran. Mucus membran turn yellow Detectable when total plasma bilirubin> 2mg/dL Excess production of bilirubin such as sickle cell anemia Decrease uptake of bilirubin in the hepatocytes |
|
|
|
Liver |
Largest gland Lobules contain hepatocytes and kuffer cells. |
|
|
|
Bile salt |
0.2-.0.5 day Formed from the metabolism of cholesterol |
|
|
|
Primary bile acid |
Cholic acid and chenodeoxycholic acid |
|
|
|
Secondary bile acid |
Due to bacteria action on primary bile acid in the colon Deoxycholic acid and lithocholic acid |
|
|
|
Primary to secondary bile acid |
Cholic acid - deoxycholic acid Chenocholic acid- lithocholic acid |
|
|
|
Water soluble bile salt |
Na K salt of bile acid and glycine or taurin |
|
|
|
Transport mechanism of bile Bile acid independent secreation |
Actively transport of Na HCO by hepatocytes duct cell Dependent on secretin( act on the duct cell to release HCO) BILE become alkaline |
|
|
|
Bile concentration and storage |
Sphincter of oddi remains closed between meals Bile collects in the gall bladder where it is concentrated and acidified (water moves out and take HCO with it hence acidified) When food In the mouth relaxation of the sphincter |
|
|
|
Function of CCK in bile salt |
CHOLAGOGUE Contractions of gall bladder to release bile in the duodenum When fats and proteins enters the duodenum causing the release of CCK Found in the jejunum
|
|
|
|
Function of secretin in bile salt |
CHOLERECTIC watery flow Increase secreation of alkaline solutions of bile |
|
|
|
Osmotic gradient of the bile salts |
Na moves out and H2O follow a as well as the other ions |
|
|
|
Transport mechanism of bile Bile acid-dependent secreation |
Active process Hepatocyte Actively secreat bile acid Dependent on entero hepatic circulation of bile salt (go thy o the intestine then to the hepatocytes) Water moves out due to osmotic gradient with the blood plasma Small amount of bile salt is secreted Active reabsorbtion takes place at the terminal ilium |
|
|
|
Entero hepatic circulation of bile salt |
Bile salt emulsify fats to aid in digestion and absorption 90% actively reabsorbe from the terminal ilium Return to the liver via portal vein ReMoved from the blood by hepatocytes and re secreation in the bile |
|
|
|
Bile salt needed |
4-8g per meal 12-30per day Bile salt circulate 1-2x during meals and 6-8x daily in response to all meal |
|
|
|
Remaining 5% of unabsorbed bile salts |
Enter the colon and converted to deoxycholic acid and lithocholic acid |
|
|
|
Deoxycholic acid |
Soluble and reabsorbe |
|
|
|
Function of bile in haem |
End product of haemoglobin metabolism of 120 day it break down and oxidase and from bilirubin and something else |
|
|
|
Bilirubin |
Water insoluble bond to albumin and called free bilirubin in the blood Liver converts/conjugated this pigment into more water soluble form bilirubin glucuronide by the enzyme glucuronoyl transferase Excreted as urobilinogens(unconjugated) in the urine(blood) and faeces(intestine) give it some colour Active process using ATP In the intestine bacteria act on it to form a water soluble form unconjugated |
|
|
|
Three types of movements in the intestine |
Segmentation- mixing waves Peristalsis- propulsive wave Tonic contractions- prolonged contractions |
|
|
|
The purpose of movements in the intestine |
Mix ingested foodstuffs with digestive enzymes and secreation Circulate contents to facilitate contact with intestinal mucusa Net aboral propulsion of intestinal content |
|
|
|
Where does BER not occur |
Esophagus Proximal stomach |
|
|
|
What initiates slow waves |
Interstitial cells of Cajal believe to be electrical pacemaker for smooth muscles cells Present in the circular muscle layer Coordinate contractions do not initiates them Need an intact myenteric plexus |
|
|
|
Depolarization and repolarization that increase muscle tension |
Depolarization- influx of Ca Repolarization- efflux of K ACh increases the intensity of the spike potential and tension of smooth muscles |
|
|
|
Peristalsis |
Initiated by stretching of the gut wall Needs an intact myenteric plexus Local streach receptors release 5-HT 5-HT activates sensory neurons that in turns activate the myenteric plexus |
|
|
|
Cholinergic neurons that activate neurons |
Retrograde- ACh and SubP cause smooth muscle contractions Anterograde- VIP & NO or ATP to cause relaxation ahead of stimulus |
|
|
|
Segmentation contractions |
Weaker then peristalsis Formed when a portion of the SI becomes distended with chyme Localized ring like contractions of the circular muscle layer Allows for chopping and mixing of chyme with intestinal secreation |
|
|
|
Mass action contractions |
Evacuation of faeces Start defecation reflex coordinated by BER Controlled by a sequence of events Contrictive ring Distal to the contrictive ring lose thier haustration Initiated by gastrocolic and duodenocolic reflexes |
|
|
|
Haustration |
Large mixing wave Storage Absorption of H2O Contractions of the teniae coli |
|
|
|
Intrinsic defecation reflex |
A weak reflex Occurs following mass movement of the sigmoid colon Serve to empty materials in the rectum Initiates peristalsis to move contents towards the anus Relaxation of internal anal sphincter Rectosphincteric reflex 2min- ilioceacal valve 6min-sigmoid colon |
|
|
|
Extrinsic defecation reflex |
Impulses pass up the sigmoid colon due to rectal streaching Efferent impulses pass via the pelvic nerve to intensify the peristaltic wave and relax tge internal ani sphincter Rectal pressure 18mmHg At 55mmHg both sphincter relax Assisted by a series of voluntary and involuntary acts: Deep inspiration Closure of glottis Lowering of diaphragm Contraction of abdominal muscles |
|
|
|
Defecation reflex |
1st urge Rectal pressure at 18mmHg Movement of faeces towards the anus initiates contraction of the external anal sphincter Rectal accommodation Inhibition of the reflex may lead to constipation At 55mmHg both sphincter relax leading to evacuation |
|
|
|
Migration myoelectric complexes |
Occur in the fasted animals Abolished upon feeding MMC begin in the stomach and sweep undigested material through S.I. into colon regulated by motilin Each cycle of electrical and motor activity starts with: quiescent period Irregular activity Regular activity Prevent bacteria overgrowth |
|
|
|
Vomiting |
Centre is near the nucleus tractus solitarius at the level of the dorsal motor nucleus |
|
|
|
Causative factors of vomiting |
Excessive destension or irritation of the stomach and S.I. psychological stimulation Rapidly changing motion Drugs- stimulate cells in the chemoreceptor trigger zone (located in walls of tge 4th ventricle)
|
|
|
|
Vomiting mechanism |
Starts with salivation and nausea Deep inspiration to lower the intrathoracic pressure Lifting of the soft palate to close the nasopharynx Raising hyoid bone and larynx to close the glottis and stretch open the UOS Relaxation of LOS and esophagus Contraction of abdominal muscles and downward movement of the diaphragm increase the intra abdominal pressure Material in the stomach is therefore squeezed and shot out through the mouth Failure of the UOS to open results in retching |
|
|
|
Chief dietary forms of fats |
Triglycerides(main neutral fats) Phospholipide Cholesterol Cholesterol esters |
|
|
|
Chief forms of fats in plasma |
Triglycerides Phospholipids Cholesterol Non-esterified fatty acids |
|
|
|
What are lipids bound to in plasma |
Protien |
|
|
|
Plasma lipoproteins |
High density lipoproteins Low density lipoprotein Very low density lipoprotein Chylomicrons transport fats |
|
|
|
Fat digestion |
Begins in the mouth Due to action of ligual lipase secreted by Edner's glands on the dorsal surface of tongue Gastric lipase secreted by pharygeal cells ( may play a role in pancreatic insufficiency) Stomach accounts for 30% fat digestion Most fat digestion occurs in the duodenum due to pancreatic lipase and bile salt
|
|
|
|
Hydrolysis of triglycerides |
Pancreatic lipase acts on 1 and 3 bonds faster than 2 bond Hence you get 2- monoglyceride or beta-monoglyceride and free fatty acids Can get isomerisation of the 2 bond to get glycerol and free fatty acids |
|
|
|
Role of colipase |
Action of pancreatic lipase requires colipase It is activated in the intestinal lumen Requires trypsin Colipase helps to anchor lipase to the fat droplets It binds to th COOH domain of the pancreatic lipase This causes a lid (amphipathic helix) covering the active site to be bent backwards Exposes the active site on lipase |
|
|
|
Bile salt activated lipase |
Represents 4% of the total protein in pancreatic juice Pancreatic lipase is more active in adults It catalyzes the hydrolysis of Cholesterol esters Esters of fat soluble vitamins Phospholipids Cholesterol esters hydrolase also hydrolyzes the dietary cholesterol esters in the intestinal lumen |
|
|
|
Emulsification of fats |
Fats must first be emulsified before lipase can act Increases the oil/water interface Oil droplets are broken up into small sizes Achieve mainly via: bile salt Lecithin |
|
|
|
Function of bile salt |
Amphipathic i.e. hydrophobic and hydrophilic At low concentrations, bile salts form molecular solutions At critical concentration, bile salts aggregate to form micelles activation of I cells to activate the CCK 50% of ingested fats can be absorbed in the absence of bile salt |
|
|
|
Bile salts micelles |
Spherical globular 25A in diameter Hydrophilic (head) Faces outwards into the watery medium Hydrophobic (tail) Is oriented inward and grouped to form a non polar core |
|
|
|
Mixed bile salt micelles |
2 monoglycerides and fatty acids are incorporated into the non polar core 40A in diameter Contain 20-50 molecules |
|
|
|
Transport mechanism of fats |
Micelles decrease the interracial tension between fat and unstirred water layer |
|
|
|
Fat absorption |
Greatest in the duodenum and jejunum Fate is dependent on size FAT< 10-12 carbon atoms pass directly into portal system Transported as free unesterified fatty acids FFA> 12 carbon atoms are re-esterified to triglycerides in mucosal cells Cholesterol is esterified Re-esterified fats enters the blood in chylomicrons |
|
|
|
Esterification on fat (major) Monoacylglycerol pathway |
Direct acylation of monoglycerides to diglycerides then triglycerides in SER |
|
|
|
Esterification on fat Phosphatidic pathway |
Phosphatidic acid, derived from glycerophosphate, is converted to diglyceride then to triglycerides and glycerophopolipid in the RER |
|
|
|
Function of chylomicrons |
Re-esterified fats are enclosed by a layer of beta-lipoprotein (protein shell), cholesterol and phospholipids
Extruded from the basolateral aspect, enter the lymphatic and emptied into the great veins of the neck
This is important because triglycerides will block vessels Bile salts and chylomicrons allow absorption of 95% ingested fats |
|
|
|
Rate limiting step in fat digestion |
Assembly and exocytosis of chylomicrons Lack of beta-lipoprotein will results in mucosal cells becoming engorged with fatty products |
|
|
|
What is absorption |
Process by which molecules are transported into the epithelial cells of the GI tract, then the blood and lymph drainage that region of the GI tract |
|
|
|
Luminal digestion |
Due to enzymes secreted by salivary glands, stomach and pancreas |
|
|
|
Membran digestion |
Significant digestion due to hydrolysis by enzymes of the intestinal brush border |
|
|
|
Chief dietary forms of carbohydrates |
Polysaccharides (starches, glycogen, cellulose) Disaccharides (sucrose and lactose) Monosaccharides (glucose and galactose) |
|
|
|
What starch consists of |
Linked by alpha 1-4 glycosidic bonds which branched points formed by alpha 1-6 glycosidic linkage |
|
|
|
Ptyalin |
Catalyses the hydrolysis of Alpha 1-4 amylase Can not hydrolyzes 1-6 amylase linkage Inactive in stomach because pH falls bellow 4 |
|
|
|
What happen in the stomach before ptyalin is inactivated |
30-40% starches hydrolyzes to maltose, 2% to isomaltose |
|
|
|
Pancreatic amylase in the small intestine and brush border cells |
Splits starch into maltose and small glucose polymers Bush border cells split disaccharides and trisaccharides into monosaccharides |
|
|
|
End product of carbohydrate digestion |
Hexose Glucose-active transport Galactose- active transport Fructose- facilitate transport |
|
|
|
Pentose |
Simple diffusion |
|
|
|
Absorption of glucose and galactose |
Highest in the duodenum and upper jejunum Absorb across the bush border epithelial cells by Na+dependent secondary active transport mechanism Depends on the amount od liminal Na+ Glucose and galactose share same cotransporter SGLT1 Glucose and galactose are transported into intestitium via facilitated diffusion by means of a transporter: GLUT2 max. Rate of glucose absorption is 120g/h Competitive binding for SGLT1 SGLT1 has a greater affinity for galactose Galactose is most rapidly transported Active transport is inhibited when luminal Na+ falls<90mM |
|
|
|
Fructose absorption |
It is absorbed in the enterocytes by facilitated diffusion via GLUT5 and tgen transported in the intestitium by GLUT2 |
|
|
|
Defective transport of carbohydrates |
Congenital defect in the Na+/glucose cotransporter (SGLT1) results in glucose and galactose malabsorption. Cause severe diarrhea Can be fatal if both sugars are not removed from the diet |
|
|
|
Digestion of protein |
Begins in the stomach due to action of pepsin Pepsins I and II split the polypeptide by hydrolyzing bonds between an aromatic a.a and second a.a Pepsin digest the protein collagen |
|
|
|
Pepsin I found in? |
Acid secreation regions (pH 2) |
|
|
|
Pepsin II found in the |
Pyloric region (pH3) |
|
|
|
Termination of pepsin |
When gastric contents enter duodenum/jejunum (pH 6.5) Small intestine have a much higher capacity to digest protein |
|
|
|
Intestinal digestion of proteins |
pancreatic enzymes brush border aminopeptidases
|
|
|
|
Endopeptidases |
Trypsin Chymotrypsin Elastase act at the interior peptide bonds |
|
|
|
Exopeptidases |
Carboxypeptidase Aminopeptidase Dipeptidase Hydrolyzed the a.a at the carboxyl and amino ends of the polypeptide |
|
|
|
Protein absorption |
> 7 different transport system exit for a.a. Most require Na+ dependent secondary active transport Di and tri peptide require H+ instead of Na+ > 5 transport systems transport a.a. out of the enterocytes from the ba solateral membrane into the portal blood Involves secondary active co-transport Absorption is rapid in duodenum Transport systems have a greater affinity for the L-isomers Glycine prefer amino groups Cysteine prefer basic groups |
|
|
|
Defects in protein absorption |
Hartnup disease: congenital defect in the mechanism that transports neutral amino acid Cystinuria: congenital defect in the transport of basic amino acids |
|
|
|
How water and minerals enters the blood |
Through the intestines Provide the solutes and solvent water for body fluids |
|
|
|
Sources of water |
9L/day Food and drink- 2L/day GI secreation- 7L/day Saliva- 1.5L/day Gastric juice- 2L/day Pancreatic and biliart secreation- 2L/day Intestinal secreation- 1.5L/day Absorption- 8.8L/day
|
|
|
|
Absorption of water |
Max. Absorption capacity of the intestines- 20L/day Small amounts of water move across the gastric mucosa Water moves passively across the intestinal mucosa Direction of movement depends on the osmotic gradient |
|
|
|
Absorption of water in the small intestine |
98% of water= 8.5 L Very little absorption in the duodenum Duodenum converts hypertonic chyme to isotonic chyme Jejunum is more active than the ilium in absorption of water |
|
|
|
Absorption in the colon |
6L/day Absorbs 90% of water present in it 1300mL/day its absorptive capacity 200ml excreted in the faeces |
|
|
|
Mechanism of water absorption |
Water moves into and out of the intestine until the osmotic pressure of the intestinal content to plasma |
|
|
|
Mechanism of water absorption in the jejunum and ilium |
Osmotically active particles produce by digestion are removed by absorption Water moves passively out of the gut and into the blood along the osmotic gradient generated |
|
|
|
Mechanism of water absorption in the colon |
Na+ moved out of the lumen and pumped from the cell Water move passively with it, along the osmotic gradient created |
|
|
|
How ions move between cells |
Transcellular- across cell Paracellular- between cells |
|
|
|
Regulation of Na passive movement |
Tight junctions or obular occludens |
|
|
|
Rate of Absorption of electrolytes is affected by |
Electrochemical gradient Sterling's forces |
|
|
|
Na+ Cl- absorption in the small intestine mechanism |
Counter transport with H+ (H-Na exchanger at the apical aspect of the cell) Co-transport with organic solutes Co-transport with Cl- Passive diffusion Glucose and amino acids in the intestinal lumen is facilitated Na+ absorption Absorption by secondary active transport is linked to Na/K electrogenic exchanger |
|
|
|
Na+Cl- absorption in the colon |
All areas absorb Na+ with Cl Co-transport of Na with organic solutes is lacking Co-transport with Cl exits Na-H counter transport coupled with Cl/HCO Channels regulated by mineralocorticoids e.g. aldosterone Aldosterone increase number of Na channel which increase Na absorption |
|
|
|
Restricted diffusion |
Primary mechanism for colonic absorption of Na+ |
|
|
|
Mechanism of K transport |
S.I. Primary mechanism is by diffusion through paracellular pathway Colon K channels are present in the luminal and basolateral membranes Allows for K secreation Chronic diarrhea can result in severe hypokalemia
|
|
|
|
Cl- secreation |
Cl- normally enters the enterocytes from the interstitial fluid via Na-K-2Cl co-transporters Cl is then secreted into the intestinal lumen via channels regulated by cAMP &/ or Ca |
|
|
|
Cholera vibrio |
Increases cAMP; results in increase secreation of Cl- which reduced absorption of NaCl then diarrhea |
|
|
|
Absorption of vitamins |
Most occurs in upper s.i. by passive diffusion Absorption of water soluble vitamins is rapid Vitamins B12 absorption is dependent on IF complex is absorbed across the mucosa of the terminal ilium by pinocytosis |
|
|
|
Absorption of Fe |
Store in the ferrous form Fe2+ Stomach acid helps to dissolve the ferric form so it can change to the ferrous form for absorption Transferring binds to the ferric form and it is transported in the blood |
|
|
|
Absorption of Fe increases due to |
Decreased body stores Increase erythropoiesis |
|
|
|
Fe deficiency |
Apoferritin decreases More Fe is passed into the blood |
|
|
|
Fe overload |
Transferrin decreases Ferritin stores increase which increase shedding |
|
|
|
Abnormal Fe absorption |
Normal rate of absorption can be maintained if ingested load is increased 15-810c normal requirements If excretion is low, ferritin molecules aggregate to form deposited called hemosiderins Prolonged overload causes accumulation in tissues: hemosiderosis- cirrhosis of liver, hepatic carcinoma, pancreatic damage with diabetes |
|
|
|
Calcium absorption |
30-80% of ingested Ca2+ is absorbed by active transport mainly in the S.I. Active transport is facilitated by VitD & parathyroid hormones Parathyroid hormone activate VitD VitD induces synthesis to 2 forms of CaBP in the mucosal cells and Ca-H ATPases Absorption is adjusted to the body's needs and facilitated by protein |
|
|
|
Faeces output of ion |
K+ most then Na then Cl |
|
|
|
Absorption of electrolytes the most |
Na+ is absorbed the most then Cl- then K+ |
|
|
|
Spike potential |
True action potential Become active when the membran potential greater than 40mV Contain calcium sodium channels (slower to open) |
|
|
|
Resting membran potential |
-56mV |
|
|
|
Factors that depolarize the membrane |
Stretching of the muscles Stimulation of ACh Stimulation by parasympathetic nerve Stimulation by GI Hormones |
|
|
|
Factors that hyperpolarize the membran |
Norepinephrine and epinephrine Stimulation of sympathetic nervous system |
|
|
|
Gastrocolic reflex |
Signals from the stomach to c as use evacuation of the colon |
|
|
|
Enterogastric reflex |
Signals from the colon and small intestine to inhibit stomach motility and stomach secreation |
|
|
|
Colonoileal reflex |
Reflexes from the colon to inhibit emptying of ileal content into the xoli n |
|
|
|
Gastrin |
Release from G cells of the antrum of the stomach Its release due to: Distension of the stomach Products of protein GRP Action is to: Stimulation of gastric acid secreation Stimulation of growth of the grastric mucosa |
|
|
|
Secretin |
Release from S cells in the mucosa of the duodenum in respond to acidic chyme entering the duodenum Helps to promote pancreatic secreation of bicarbonate because it activate cAMP |
|
|
|
GIP |
Secreted by tge mucosa of the upper small intestine in respond to fats and proteins Slow emptying in the duodenum when its full |
|
|
|
Motilin |
Secreted from the upper duodenum during fasting Increase GI motility |
|
|
|
Inhibitors of stomach emptying |
Gastrin Secretin GIP CCK |
|
|
|
Peristaltic rush |
Intense irritation of the intestinal mucosa |
|
|
|
Function of the ileocecal valve |
Prevent backflow of fecal contents from the colon into the small intestine |
|
|
|
Function of the colon |
Absorption of water and electrolyte from chyme to form solid feces Storage of fecal matter until it can be expelled |
|
|
|
Inhibition of saliva |
Sleep rough objects |
|
|
|
Two major types of protein secreation |
Serous contails ptylin Mucus contain mucin |
|
|
|
Two form of gastrin polypeptide |
Large G34 Small G17 more abundant |
|
|
|
Achlorhydria |
Lack of stomach acid secreation |
|
|
|
VitB12 absorption |
Ilium |
|
|
|
Large polypeptide |
Gatrin- 34 terminal 4 are functional CCK- terminal 8 functional 33 a.a. Secretin- all essential 27 a.a. Motilin- 22 a.a.
|
|
|
|
Inhibition of gastric secreation |
VIP CCK GIP somatostatin Secretin |
|
|
|
Pentagastrin |
Gastrin terminal 4 a.a. and alanine |
|
|
|
VITB1 absorption |
In the jejunum |
|
|
|
Kerckrings fold |
Found in the SI |
|
|
|
Mechanism of enzymes secreation |
Synthesis begins when exportable proteins in association with polysomes at the RER
Synthesis proteins are collected in RER cristernae
Enzymes pass in golgi vesicles
Then transported to condensing vacuols
Concentrated into zymogenic vacuols and release upon stimulation |
|
|
|
Lithocholic acid |
Insoluble Most excretion in the stool 1% absorption Liver synthesis amount lost in faeces |
|
|
|
Parasympathetic neurons in the digestive system |
Medulla oblongata Vagus |
|
|
|
Secondary peristaltic wave |
Retained food causes detention of the myenteric plexus |
|
|
|
Swallowing centers |
Dorsal motor nerve of the vagus Nucleus ambiguous Tracts soltarius |
|
|
|
VIP NO |
Inhibitory to the gastric system |
|
|
|
Kallikren |
Causes dilation of blood vessels |
|
|
|
Function of HCL |
Convert Ferris ion to ferrous ion Secind line of defence Splits pepsinogen to Pepsi 1and 2 |
|
|
|
Pacemaker cells |
BER initiated by interstitial cells of Cajal Set the pace for contractions Coordinate contraction Requires a functional and intact myenteric plexus Located in the funds and body Connected by gap junction 3/mins - stomach 12/min- duodenum 8/min- terminal ilium |
|
|
|
Enterogastric reflexes |
Inhibitory reflex When chyme enters the duodenum it inhibites contraction of the antral pump |
|
|
|
Regulation of pepsinogen secretion |
No intestinal phase Increased by vagal stimulation Gastric Secretin |
|
|
|
GRP |
Release from vagal nerve ending which cause the release of gastric from G cells which cause the relays of HCL from parietal cells |
|
|
|
GIP |
Cause the release of insulin |
|
|
|
Liminal digestion |
Enzymes s ecreated from the salivary glands stomach and pancreas |
|
|
|
Ptyalin does not hydrolyse |
Alpha 1,6 glycosidic bond Terminal alpha 1,4 glycosidic bond Alpha 1,4 next to branching points |
|
|
|
Dorsal vagal complex |
T ractus soltarius Dorsal motor nuclei of the vagus Nucleus ambiguous |
|
|
|
Location of gastric lipase |
Fundus |
|
|
|
Gastric juice content |
Bicarbonate HCL IF vitB12 |
|
|
|
Why H needs a pump |
It is pumped against its electrochemical gradient into a positive environment |
|
|
|
Increase in gastric secreation |
Calcium gastrin histamin Insulin epinephrine Distenstion of the stomach |
|
|
|
Function of gastrin in tutorial |
Increase mucosal growth and motility Activate pepsinogen |
|
|
|
D cells in fetal life. |
Produce gastrin |
|
|
|
D cells in fetal life. |
Produce gastrin |
|
|
|
ZED |
marked increase in serum gastrin with calcium Small increase with serum gastrin with a test meal Paradoxical increase in serum gastrin with secreation |
|

