![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
abdomen topography: medicalviculat plan
subcostal plan intertubercular plan |

|
|
|
|
median plan and transumbilical plane
|

|
|
|
|
the abdominal wall layers
|
skin/ superficial fascia fatty layer ( camper's fascia)/ superficial fascia membranous layer(scrapas fascia)/external oblique muscle / internal oblique muscle/ transversal abdominal muscle / transversalis fascia/ extra peritoneal fascia/ parental peritoneum
|
|
|
|
abdominal wall muscle
|
rectus muscle( azole jeloee)
external oblique internal oblique transverse oblique |
|
|
|
abdominal muscle function
|
in respiration system with contraction and relaxation ( inhalation) helps breathings
|
|
|
|
greater omentum
|
very large sheet fat for reserve energy
|
|
|
|
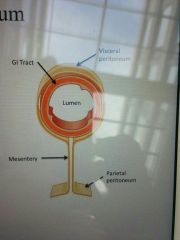
mesentry
|
The mesentery is a fold of membranous tissue that arises from the posterior wall of the peritoneal cavity and attaches to the intestinal tract.
it connects intestine to body |
|
|
|
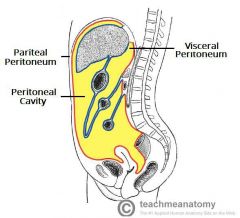
perientonum peritonium
|
serious otlr visceral peritenum is continue by parental peritenium
|
|
|
|
peritenium
|
|
|
|
|
mucus membrane fun
|
protective,secretory,absorptive,
|
|
|
|
5 step in gastrointestinal tract
|
ingestion, fragment, digestion, absorption, elimination
|
|
|
|
hepatic vein
|
vein that carries blood out of liver
|
|
|
|
dodenum function
|
first part of small intestim
bile from liver break fats and pancreases juice digestvall part of foods |
|
|
|
portal vein
|
carries blood from entire digestive tract to liver
|
|
|
|
bacteria in large intestine
|
makevvitamine
|
|
|
|
protein
how digest converte to: |
denaturation by gastric juice
enzimatic hydrolysis to into polypeptide( trypsin, Chymotrypsin,elastas, carboxypeotidase) -->membrane bound peptide hydrolases produce amino acids -->carrier enzymes actively transport individual amino acids |
|
|
|
carbohydrate
which part digest it |
enzymatic hydrolysis( salivary and pancreatoc Amylase)
membrane bound di and oligosacharidase ,glucouse,fructouse, galactos -->sorbed by facilitated diffusion |
|
|
|
lipids
|
trigliciride convert to course emulsion in stomache
converted into a fine emulsion by combination with bile acids in the duodenum pancreatic lipases break triglyceride down to monoglyceride and to two free fatty acids absprbe and then re-synthesised |
|
|
|
oesophagus layers from inside
|
epithelium( with gland) : startified squmpus non kratinised
2 lamina propria 3 muscular is mucousa: circular and longidinal layers adventia connective tissue |
|
|
|
stomach histological layers
|
1 epithelium( with gland) : simple columnar
2 lamina propria 3muskularis: fibrae obliqae, circular and longidinal layers subserosa peritoneum viscerale |
|
|
|
colon histological layers
|
1 epithelium( with gland)
2 lamina propria 3 muskularis: circular and taenia layers subserosa/ adventita peritoneum viscerale |
|
|
|
small intestine histological layers
|
mukosa:1 epithelium( with gland)
2 lamina propria 3 muskularis: circular and longitude layers subserosa peritoneum viscerale |
|
|
|
nervous control of GI tract
|
1 myentric plexuse ( BTW longitude and circular muscle)
2 submuscosal plexus( BTW circular and muscosal |
|
|
|
blood supply in abdominal
|
celiac( shekami)--> stomach, liver, pancrease ( foregut part)
superior mesentric artrey connected to small intestine and cecenum, ascending, part of transversal inferior mesentric artrey: to large intestine |
|
|
|
lesser omentum
|
connect liver to stomach
|
|
|
|
stomach divided to
|
1- fundus
2- body( corpus) 3- pylorus : end part of stomach |
|
|
|
cardia stomach
|
entrance of esphogaus
|
|
|
|
greater curvature
|
inferior part of stomach (gaster)
|
|
|
|
lesser curvature
|
place of connection of lesser momentum to stomach
|
|
|
|
ragae
|
curve shape of epithelium of stomache
|
|
|
|
pylorus sphincter
|
direct food to small intestine
|
|
|
|
muscle layer of stomach
|
longitude
oblique muscle layer circular muscle layer |
|
|
|
gastric secretory cells
|
mucousae neck cells
parental cell chief (peptic) cells enteroendocrone cells |

|
|
|
small intestine parts
|
dudenuom
jejenum ilium |
|
|
|
duodenum func
|
neutralize stomach acid
enzymatic digestion are received from liver and pancreas |
|
|
|
bile duct location
|
in duodenum
there two hole in duodenum: minor duodenal papilla and major duodenal papilla |
|
|
|
small intestine jejenum function
|
further enzymatic digestion, nutrient absorption
|
|
|
|
plicae circulares
|
surface of small intestine contain curving epithelium
it contain microvilly |
|
|
|
ilium fun and location
|
further enzymatic digestion, nutrient absorption,
local: lower right( and left quadrant) |
|
|
|
crypt، villi
|
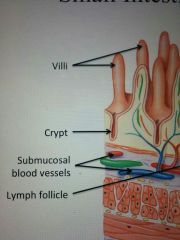
|
|
|
|
intestinal crypts contain enteroendocrone cells responsible for?
|
production of several intestinal hormones, including cholecystokinin and secretion, and enzymes with antibacterial activity
|
|
|
|
lamina proper contains
|
lymphatic cells
network of capillaries terminal lymphatic: lacteal--> transport material can't enter to capillaries( large lipid) |
|
|
|
how dudenum keep epithelium
|
it has abundant number of glands( submacousal glands), make large quantities of mucus --> protection from acid
|
|
|
|
ileum and jeunum epithelial histology
|
plicae and villi remain prominent over proximal half of jejenum( reduce absorption)
aggregated lymphoid nodules or Peters patches in ileum.( not allowed the bacteria from large intestine enter |
|
|
|
colon function
location |
water resorption and electrocyted, micro floraaided digestion and nutrient absorption
absorption of important vitamin produced by bacteria sorting fecal loc: surrounding the small intestine sigmoid is intra- peritoneal( jelly peritetion) |
|
|
|
colon parts
|
ceceum
ascending trasverse sigmoid rectum anal canal |
|
|
|
omentral appenics?
haustra? |
serous of colon contains numourous teardrop shape
haustra: series of pouches that allow a long at I on in colon |
|
|
|
taeniae coil
|
separate longitudinal ribbon of smooth muscle on outer surface of the colon
|
|
|
|
epithelium of colon
|
simple columnar epithelium with many foveolae |
|
|
|
colon histolgy
|
thinner wall
lack of villi globlet cells are abundant large intestine has distinctive crypts, deeper gland large lymphoid nodes no longitudinal layer,it reduced to taenia coli |
|
|
|
rectum location
|
retro peritoneal
internal and external sphincters |
|
|
|
anus canal epithelium
end anus |
stratified sqoumus nonkratinised ( same as mouth)
similar to skin keratinised |
|
|
|
rectum epithelium
|
single layer columnar epithelium
|
|
|
|
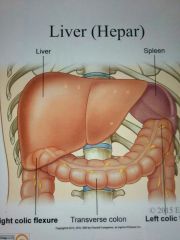
liver( hepar) location
|
it start from right colic flexure( khamshodegie roode bozorg) to left colic flexure, next to spleen
intra peritoneal organ |
|
|
|
liver lobes
|
right lobe
quadrate lobe left lobe |
|
|
|
falciform ligament
|
anterior surface , a ventral mesentery , the falciform ligament mark division between lobs
|
|
|
|
four loubs of livet
|
left
right quardratic caudate lobe |
|
|
|
gastry secretory cells tepys: mucousae neck cell fun
|
mocouse neck shape cells are columnar in shape, for lubrication
|
|
|
|
gastry secretory cells tepy chief cell or peptic cell
|
secret pepsinogen convert by acid to pepsin( protein digestion)
newborn baby stomach produce rennin and gastric lipase( milk digestion) |
|
|
|
gastry secretory cells tepys: mucousae parental cell fun
|
intrinsic factor --> fascilitate absorption of vitamin B12and hydrochloric acid HCL---> kills microorganism, breal dpwn cell wall of food
activate secretion of chief cells |
|
|
|
gastry secretory cells tepys: enteroendpcrine cell fun
|
g cells: most abundant in gastric pits of pyloric region( secret gastric)
|
|
|
|
gastin hormones fun
|
active parental and chief cells and smooth muscle activity
|
|
|
|
blood supply to stomach
|
three branches of celiac trunk
1- left gastric artrey: lesser curvature and cardiac 2- the splenic artrey: supply the fundus and greater curvature 3- coomon hepatic:lesser and greatur of pylorus |
|
|
|
plicae circularis
|
number of villi projecting into the lumenof the small intestine.
|
|
|
|
affarent blood vessels and other structure reach the liver by traveling by connective tissue known as
|
porta hepatis
|
|
|
|
two blood vessels deliver blood to liver
|
hepatic artrey proper
hepatic portal veib |
|
|
|
liver function
|
1-metabolic regulation
2-hematological regulation: remove old rbc , synthesize plasma proteon 3-synthesize and secretion of bile |
|
|
|
hepatocyte
|
liver cell
|
|
|
|
kupffer
|
type of phagocyte and macrophage cells
|
|
|
|
liver fun
|
fat metabolism-> oxidizing triglycerides, synthesis of cholesterol and phospholipid
carbohydrate metabolism-> conversion of carbohydrates into fatty acids and triglycirids, regulation of blood glucose by glycogenolysis, glyconeogenisis protein metabolism-> synthesis of plasma proteins( albumin, coagulations),synthesis of non essential amino acids,detoxification or metabolic waste ( ammonia) storage-> glycogen, vitamins A,D,K,B12, iron, copper intermediary metabolism-> detoxification of drugs and toxins( alcohol,industrial chemicals, pharmaceuticals) secretion--> bile, hormones( igf, thrombopoietin,angiotensin) |
|
|
|
bile canaliculi
|
network canals between hepatocytes in liver
|
|
|
|
cystic duct
|
duct connective gall bladder to common duct
|
|
|
|
cystic artrey
|
blood vessel of gall bladder
|
|
|
|
panxretic acini
|
secretory unit in pancreas( exocrine)
|
|
|
|
epithelium of collecting ducts
|
larger collecting ducts lined by stratified cuboidal epithelium
smaller collecting ducts lined by simple cuboidal epithelium mucouse |
|
|
|
pancreatic ducts secret buffers
|
HCO3( sudium bicarbonate) and water
|
|
|
|
pancreatic islet
|
endocrine cells in oancreae
|
|
|
|
pp cells secret
|
pancreatic polypeptide control nutrient absorption
|
|
|
|
sigma cells secret
|
somatostatine, slows food absorption
|
|
|
|
betta cells secretion
|
insulin
decrease blood glucose |
|
|
|
alpha cells absorption
|
glucagen
increase blood suger |
|

