![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
139 Cards in this Set
- Front
- Back
|
common drugs that raise blood glucose levels
|
MOST LIKELY CULPRITS:
corticosteroids protease inhibitors atypical antipsychotics MODEST INCREASE: niacin (but useful in many DM pt's) thiazide diuretics (at normal doses, only slight increase) beta agonists phenytoin cyclosporine tacrolimus |
|
|
which atypical antipsychotic is the worst offender when it comes to raising BG?
|
Zyprexa (olanzapine)
also may increase blood pressure & lipids |
|
|
What constitutes pre-diabetes?
|
FPG:
100 - 125 mg/dL or OGTT (oral glucose tolerance test, 75 g) 140 - 199 mg/dL or HbA1C 5.7 - 6.4 % |
|
|
Criteria for the diagnosis of diabetes
|
Signs and sx of diabetes AND a random BG of 200 mg/dL or higher
or FPG 126 mg/dL or higher or 2-hr OGTT 200 mg/dL or higher or HbA1C 6.5% or higher |
|
|
Other than diabetes itself, what can precipitate DKA?
|
acute illness, such as infection, pancreatitis, myocardial infarction, stroke
|
|
|
DKA symptoms
|
hyperglycemia
polyuria polyphagia polydipsia blurred vision metabolic acidosis (fruity breath, dyspnea) dehydration (dry mouth, excessive thirst, poor skin turgor, fatigue) |
|
|
DKA lab abnormalities
|
BG 300 mg/dL or greater
ketones present in urine and blood blood pH 7.2 or less bicarb < 15 mEq/L WBC 15 - 40 cells/mm2 |
|
|
DKA treatment
|
IV fluids and insulin
replacement of electrolytes close monitoring (typically use NS, followed by 1/2 NS, and correcting potassium level > 3.5 mEq/L) potassium, if high initially, should be expected to drop as insulin is administered; it may be necessary to replace potassium as the insulin drives it into cells |
|
|
eAG
|
estimated average glucose (3-month average)
based on HbA1C may be easier for patients to understand goal eAG for diabetics is < 154 mg/dL |
|
|
goal pre-prandial BG for diabetics?
post-prandial? |
pre-prandial goal:
70 - 130 mg/dL post-prandial (1-2 hrs after eating): < 180 mg/dL |
|
|
LDL goal in DM
TG goal in DM HDL goal in DM BP goal in DM |
< 100 mg/dL in pt's without overt CVD
in pt's with overt CVD, treating LDL to < 70 mg/dL is an option TG should be < 150 mg/dL HDL should be > 40 in men, > 50 in women BP should be < 130/80 |
|
|
preferred initial therapy for HTN in diabetics?
preferred add-on therapy for HTN in diabetics? |
initial:
ACE or ARB (helps reduce development of nephropathy) If pt is still not at goal with ACE or ARB, a thiazide diuretic should be added (if CrCl > 30), or a loop diuretic (if CrCl < 30) |
|
|
what routine exams and services should pt's with diabetes receive?
|
annual urine test for albumin (any protein in urine indicates renal disease and requires strict BG and BP control)
feet should be examined daily by pt , and at every visit by physician, and annually by a podiatrist initial dilated retinal exam, followed by annual eye exams (may have eye exams every 2-3 years if past exams are normal) all DM pt's should get the fall influenza vaccine all DM pt's should get the pneumococcal vaccine (repeat vaccine if pt is 65 or older, and/or if it was longer than 5 years since 1st immunization) consider aspirin therapy for PRIMARY prevention in diabetics with increased CV risk (10-year risk > 10%); this includes men over 50 and women over 60 with at least one additional risk factor (HTN, family hx, smoking, dyslipidemia, albuminuria); dose should be 75 - 162 mg/day (if pt has ASA allergy, give clopidogrel 75 mg per day) |
|
|
when should diabetic patients get aspirin therapy?
|
consider aspirin therapy for PRIMARY prevention in
diabetics with increased CV risk (10-year risk > 10%) this includes men over 50 and women over 60 with at least one additional risk factor (HTN, family hx, smoking, dyslipidemia, albuminuria) dose should be 75 - 162 mg/day (if pt has ASA allergy, give clopidogrel 75 mg per day) |
|
|
Type 2 Diabetes treatment algorithm (basic, see book for more detail)
|
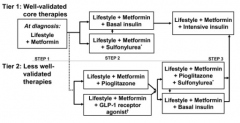
usually wait 3 months and move to next step if A1C is 7 or greater
if A1C is 10 or greater at any point, add insulin if FBG is > 250 mg/dL, or if pt has ketouria or sx of hyperglycemia, consider using insulin |
|
|
Glucophage
- generic - class - MOA |
metformin (Glucophage, Glumetza, Fortamet)
Class: biguanide MOA: - decreases hepatic glucose output (primary MOA) - decreases intestinal absorption of glucose - improves insulin sensitivity |
|
|
Glucophage dosing forms
|
metformin (Glucophage, Glucophage XR, Fortamet, Glumetza)
IR (tablets in mg): 500, 850, 1000 ER (tablets in mg): 500, 750, 1000 Riomet is a liquid formulation of metformin |
|
|
Riomet
|
metformin (Riomet)
liquid 500 mg/5 mL |
|
|
Metaglip
|
metformin
+ glipizide |
|
|
Glucovance
|
metformin
+ glyburide |
|
|
Actoplus Met
|
metformin
+ pioglitazone |
|
|
Avandamet
|
metformin
+ rosiglitazone |
|
|
Janumet
|
metformin
+ sitagliptin |
|
|
Kombiglyze XR
|
metformin
+ saxagliptin |
|
|
PrandiMet
|
metformin
+ repaglinide |
|
|
Glumetza dosing
|
metformin (Glumetza, Glucophage, Fortamet, Riomet)
start IR 500 - 850 mg daily, or 500 mg BID start ER 500 - 1000 mg with dinner titrate to 2 g daily, although higher doses are sometimes used the ER formulations may appear in the stool take with meals |
|
|
how much is metformin treatment expected to lower A1C?
|
usually 1 - 2 %
|
|
|
Fortamet
- adverse effects - caution & when would you hold metformin? |
diarrhea, or loose stools, occurs in up to 20% (often goes away)
abdominal discomfort WEIGHT NEUTRAL NO HYPOGLYCEMIA BBW: lactic acidosis (rare, but can be fatal; more common in pt's with renal impairment and cardiac disease, counsel for sx) Caution in HF: if HF is acute or worsening, it is best to hold the metformin; the pt may experience hypoperfusion, which can lead to hypoxia and acute renal failure metformin should be stopped in any case of hypoxia, such as decompensated HF, respiratory failure, or sepsis hold metformin 48 hours prior to use of IV contrast dye, and wait 24 hours after the procedure (or test renal fxn before resuming); contrast dye increases risk of lactic acidosis |
|
|
Fortamet
|
metformin
|
|
|
T or F:
metformin may cause hypoglycemia |
False
|
|
|
T or F:
Metformin won't cause weight gain. |
True
(metformin is considered weight neutral) |
|
|
Glumetza renal dosing
|
metformin (Glumetza)
contraindicated with SCr 1.5 or greater (males), or 1.4 or greater (females) contraindicated with CrCl < 60 |
|
|
Glucophage drug interactions
|
metformin (Glucophage)
alcohol can increase risk for lactic acidosis, especially with renal impairment and advanced heart disease iodinated contrast dye increases the risk of lactic acidosis - hold x 48 hrs before and recheck renal fxn before resuming (or wait 24 hours) metformin decreases folate and B12 absorption: this can lead to neuropathic damage, consider vitamin supplement |
|
|
Glucophage counseling
|
metformin (Glucophage)
sx of lactic acidosis (weakness, increasing sleepiness, slow heart rate, cold feeling, muscle pain, SOB, stomach pain, feeling light-headed, fainting) take with meals (twice daily with morning and evening meal for IR, once daily with evening meal for ER) do not chew/crush/swallow ER tablet diarrhea and abdominal discomfort may occur, often goes away; stomach upset may be worse if taken on an empty stomach if using Glumetza, you may see a shell of medicine in the stool; this is not a problem |
|
|
sulfonylureas MOA
|
sulfonylureas work by stimulating insulin secretion from the pancreatic beta cells (do not use with meglitinides due to similar MOAs)
|
|
|
sulfonylurea drug interactions
|
primary interaction is with insulin b/c hypoglycemia
use caution with drugs that can cause hypoglycemia: alcohol, azole antifungals, penicillamine, pentamidine, quinidine, quinolones, pramlintide and SMZ-TMP |
|
|
Diabinese
|
chlorpropamide
sulfonylurea (an older one, no longer routinely used; ADA guidelines state not to use chlorpropamide due to long duration and risk of hypoglycemia) |
|
|
The ADA cautions against using which two sulfonylureas (include brand & generic names), and why?
|
glyburide (Diabeta, Micronase)
chlorpropamide (Diabinese) Both can cause long-lasting hypoglycemia. Glyburide has a partially active metabolite that is renally cleared; it accumulates with renal dysfunction and is not recommended in patients with a CrCl < 50 mL/min. micronized glyburide (Glynase PresTab) has better absorption than glyburide (3 mg micronized = 5 mg glyburide) |
|
|
Which sulfonylurea should be taken on an empty stomach?
|
glipizide (immediate release) and glimepiride
take on an empty stomach, 30 minutes before eating NOTE: glyburide can also be taken this way, but it is sometimes advised to take glyburide during or immediately after a meal, because it carries a higher risk of hypoglycemia than other SU's (particularly important if an elderly patient is put on glyburide!) |
|
|
adverse effects of sulfonylureas
|
hypoglycemia
weight gain decreased efficacy after long-term use (pancreatic cell burnout) NOTE: sulfonylureas do NOT typically cause much GI upset, unlike metformin |
|
|
sulfonylurea counseling
- if dosed once daily? - if dosed twice daily? |
do not crush/chew/break ER tablets
if dosed once daily, take 30 min before breakfast if dosed twice daily, take 30 min before breakfast and dinner (except glyburide, take with meal to decrease hypoglycemia risk, esp in elderly who are cautioned with glyburide use anyway) may cause low blood-sugar (sx are shakiness, irritability, hunger, headache, confusion, drowsiness, weakness, dizziness, sweating, fast heartbeat); always keep a source of sugar on hand |
|
|
Glucotrol dosing
|
glipizide (Glucotrol, Glucotrol XL)
sulfonylurea IR: 2.5 - 10 mg BID XL: 2.5 - 10 mg daily, maximum 20 mg daily take on an EMPTY stomach, usually 1/2 hour before meal! |
|
|
Amaryl dosing
|
glimepiride (Amaryl)
sulfonylurea 2 - 4 mg, maximum 8 mg daily avoid in the elderly because it is longer-lasting (glipizide is the preferred agent in elderly) |
|
|
which sulfonylurea is preferred in the elderly?
|
glipizide (Glucotrol) is preferred
AVOID glyburide and chlorpropamide in the elderly, because they have more hypoglycemia AVOID glimepiride in elderly, because it is longer-lasting & elderly pt's tend to do better with shorter-acting SU's (less hypoglycemia) |
|
|
which sulfonylurea should be avoided in pt's with low creatinine clearance (and how low)?
|
avoid glyburide (Diabeta, Micronase) in patients with CrCl < 50
glyburide has a partially active metabolite that is renally cleared |
|
|
which sulfonylurea has a disulfiram-like reaction?
|
chlorpropamide (Diabinese)
|
|
|
Metaglip
|
glipizide
+ metformin |
|
|
Duetact
|
glimepiride
+ pioglitazone |
|
|
Avandaryl
|
glimepiride
+ rosiglitazone |
|
|
Diabeta dosing
|
glyburide (Diabeta, Micronase)
1.25 - 5 mg/day |
|
|
Glucovance
|
glyburide
+ metformin |
|
|
which sulfonylurea may be preferred in patients with CAD?
|
glimepiride
induces nitrous oxide formation in human coronary endothelial cells (HCAEC's), also shown to inhibit formation of atheromatous plaques in mice NOTE: glimepiride should generally be avoided in elderly patients because it is longer acting; glipizide is the preferred agent in the elderly |
|
|
meglitinide MOA
|
meglitinides work by stimulating insulin secretion from the pancreatic beta cells (do NOT use with sulfonylureas because of similar mechanism!)
|
|
|
which two classes of diabetes drugs work by stimulating insulin secretion from pancreatic beta cells, and how are these two classes different?
|
sulfonylureas and meglitinides
they have different binding sites of more clinical relevance, SU's last longer in the body and thus have more prolonged effects and do not need to be taken as often, but also carry a higher risk of hypoglycemia meglitinides (rapaglinide and netaglinide) are much shorter-acting with peak effects in one hour, so they may have to be taken up to three times a day 15 - 30 minutes before meals, but they carry a lower risk of hypoglycemia |
|
|
Prandin dosing
|
repaglinide (Prandin)
meglitinide if A1C is < 8%: 0.5 mg TID if A1C is 8% or more: 1 - 2 mg TID |
|
|
Starlix dosing
|
nateglinide (Starlix)
meglitinide if near goal A1C: 60 mg TID otherwise: 120 mg TID take 15 - 30 minutes before meals |
|
|
how much is a meglitinide expected to lower A1C?
|
meglitinides lower A1C 0.5 - 1.5 %
used to lower post-prandial glucose nateglinide is slightly less effective than repaglnide |
|
|
what are the benefits of meglitinides over sulfonylureas?
what are the benefits of sulfonylureas over meglitinides? |
meglitinide benefits (repaglinide, nateglinide):
- weight neutral (unlike SU's, which can cause weight gain) - less hypoglycemia sulfonylurea benefits: - more convenient dosing (meglitinides dosed up to TID) - lower A1C more (1-2% lowering, vs meglitinides which are 0.5-1.5%) |
|
|
adverse effects of meglitinides
|
hypoglycemia
weight neutral! |
|
|
meglitinide drug interactions
|
primary interaction is with insulin, because both can cause hypoglycemia
gemfibrozil increases Prandin (rapeglinide) concentrations and can decrease GB: recommend fenofibrate instead use caution with drugs that can cause hypoglycemia: alcohol, azole antifungals, penicillamine, pentamide quinidine, quinolones, pramlintide & SMX-TMP |
|
|
meglitinide counseling
|
Prandin (repaglinide)
Starlix (nateglinide) take 15 - 30 minutes before meals if you forget to take a dose until after eating, skip that dose and take only your next regularly scheduled dose, before a meal if you plan to skip a meal, skip the dose for that meal (some pt's will be told to increase dose if they eat significantly more food at a meal) may cause low blood sugar (sx are shakiness, irritability, hunger, headach, confusion, drowsiness, weaness, dizziness, sweating, fast heartbeat); always keep glucose tabs on you |
|
|
thiazolidinediones MOA
|
thiazolidinediones
peroxisome proliferator-activated receptor gamma agonists causing peripheral insulin sensitivity (increased insulin entry into muscle cells; insulin sensitizer) TZD's are pioglitazone (Actos) and rosiglitazone (Avandia) |
|
|
Actoplus
|
pioglitazone
+ metformin |
|
|
Duetact
|
glimepiride
+ pioglitazone |
|
|
Avanadamet
|
rosiglitazone
+ metformin |
|
|
Actos dosing
|
pioglitazone (Actos)
TZD 15 - 45 mg daily |
|
|
Avandia dosing
|
2 - 8 mg daily
NOTE: not in any guidelines. Restricted due to CVD risk. Patients must be enrolled in the Avandia-rosiglitazone REMS program. |
|
|
TZD adverse effects
|
TZD's ("Glitazones"):
BBW: may cause or exacerbate heart failure in some patients Adverse Effects: peripheral edema weight gain macular edema CHF fracture risk pioglitazone has increased risk of bladder cancer when used beyond 1 year Hepatic: d/c when liver enzymes >3x normal, or sx of hepatitis - monitor liver enzymes periodically CV Risk: use caution in CHF, can cause fluid retention, peripheral edema, HF decompensation - contraindicated in NYHA 3 or 4. Rosiglitazone can increase the risk of MI (BBW). Pioglitazone is better for lipids: rosiglitazone can increase LDL. CI: NYHA Class 3 & 4 heart failure; do not use pioglitazone in patients with active bladder cancer |
|
|
glitazone counseling
|
"glitazones" are pioglitazone (Actos) & rosiglitazone (Avandia)
thiazolidinediones may take several weeks for the drug to lower blood sugar, monitor your levels carefully take once daily, with or without food contact your doctor right away if you are passing dark-colored urine, have pale stools, feel more tired than usual or if your skin and/or whites of your eyes become yellow (signs of liver damage) this drug can cause water retention and may cause your ankles to swell; if you develop trouble breathing, contact your doctor right away |
|
|
alpha-glucosidase inhibitors MOA
|
alpha-glucosidase inhibitors are acarbose (Precose) and miglitol (Glyset)
these agents inhibit alpha-glucosidase in the intestines and alpha-amylase in the pancreas, resulting in decreased absorption of glucose they also inhibit the metabolism of sucrose to glucose and fructose |
|
|
how much do TZD's lower A1C?
|
TZD's = thiazolidinediones (a.k.a. "glitazones")
lower A1C 0.5 - 1.4 % |
|
|
how much do alpha-glucosidase inhibitors lower A1C
|
alpha-glucosidase inhibitors are Precose (acarbose) and Glyset (miglitol)
lower A1C 0.5 - 0.8 % used to lower post-prandial A1C |
|
|
Precose dosing
|
acarbose (Precose)
alpha-glucosidase inhibitor started at 25 mg with the first bite of each main meal; increased by 25 mg every 1-2 months, maximum of 200 mg/day, divided according to meals |
|
|
Glyset dosing
|
miglitol (Glyset)
alpha-glucosidase inhibitor started at 25 mg with the first bite of each main meal; increased by 25 mg every 1-2 months, maximum of 200 mg/day, divided according to meals |
|
|
alpha-glucosidase inhibitors side effects (good and bad)
contraindications? |
alpha-glucosidase inhibitors are Precose (acarbose) and Glyset (miglitol)
GI effects [flatulence, diarrhea, abdominal pain (all in >20% patients)], so titrate slowly! weight neutral! Good: increased HDL, lowered TG's and total cholesterol! CI: IBS colonic ulcerations intestinal obstruction (do not use in any significant GI disease!) acarbose can rarely increase liver enzymes, check LFT's every 3 months during the 1st year also monitor SCr periodically |
|
|
alpha-glucosidase inhibitor counseling
|
alpha-glucosidase inhibitors are Precose (acarbose) and Glyset (miglitol)
take with a full glass of water with your first bite of food; needs to be in your stomach with your food if you plan to skip a meal, you do not need to take the meal-time dose will cause flatulence and diarrhea, but this usually goes away with time; the dose may be increased as you get over these side effects These agents by themselves do not cause low blood-sugar, however, you can still get hypoglycemia from other meds. Keep in mind that if you get hypoglycemia after taking acarbose or miglitol, you CANNOT treat it with sucrose (because these drugs prevent the metabolism of sucrose)!! If you take other meds that carry a risk of hypoglycemia, you MUST carry tablets or gel with glucose. Sucrose is the sugar in fruit juice, table sugar and most candy, and will not be helpful in hypoglycemia in patients taking acarbose or miglitol. This med does not cause weight gain, and may improve your cholesterol. |
|
|
DPP-4 inhibitors MOA
|
DPP-4 inhibitors are Januvia (sitagliptin), Onglyza (saxagliptin), and Tradjenta (linagliptin)
DPP-4 inhibitors preven the enzyme DPP-4 from breaking down incretin hormones, glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP). These hormones help to regulate blood glucose levels by increasing insulin release from the pancreatic beta cells and decreasing glucagon secretion from pancreatic alpha cells. A reduction in glucagon results in decreased hepatic glucose production. These are incretin enhancers. Overall: - increased insulin release from pancreatic beta cells - decreased hepatic glucose production (because of decreased glucagon secretion from pancreatic alpha cells) |
|
|
how much do DPP-4 inhibitors lower A1C?
|
DPP-4 inhibitors are Januvia (sitagliptin), Onglyza (saxagliptin), and Tradjenta (linagliptin)
lower A1C: 0.5 - 0.8 % primarily lower post-prandial BG |
|
|
Januvia dosing
|
sitagliptin (Januvia)
DPP-4 inhibitor 100 mg daily (can start at 50 mg) 25 mg with CrCl < 30 (including dialysis) take once daily in the morning, with or without food |
|
|
Onglyza dosing
|
saxagliptin (Onglyza)
DPP-4 inhibitor 5 mg daily 2.5 mg daily if CrCl < 50 (or with strong CYP3A4 inhibitors) take in the morning, with or without food (Note that Kombiglyze XR is given daily with the evening meal) Kombiglyze XR = saxagliptin + metformin |
|
|
Tradjenta dosing
|
linagliptin (Tradjenta)
DPP-4 inhibitor 5 mg daily no renal dose adjustment take once daily in the morning, with or without food |
|
|
DPP-4 inhibitors and renal function
|
no renal dose adjustment with Tradjenta (linagliptin)
1/4 dose (25 mg instead of 100 mg) with Januvia (sitagliptin) if CrCl < 30 half-dose (2.5 mg instead of 5 mg) with Onglyza (saxagliptin) if CrCl < 50 |
|
|
which DPP-4 inhibitor requires a dose adjustment in patients taking strong CYP 3A4 inhibitors?
|
Onglyza (saxagliptin)
2.5 mg daily (instead of the normal 5 mg daily) |
|
|
adverse effects of DPP-4 inhibitors
|
DPP-4 inhibitors are Januvia (sitagliptin), Onglyza (saxagliptin) and Tradjenta (linagliptin)
nasopharyngitis, upper respiratory tract infections, peripheral edema, rash and hypoglycemia rarely, may cause acute pancreatitis weight neutral monitor renal function |
|
|
DPP-4 inhibitor drug interactions
|
Onglyza (saxagliptin) - use the lower 2.5 mg dose with strong CYP 3A4 inhibitors including ketoconazole, atazanavir, clarithromycin, indinavir, itraconazole, nefazodone, nelfinavir, ritonavir, saquinavir and telithromycin
Tradjenta (linagliptin) - 3A4 and PGP substrate. Linagliptin levels are decreased by strong inducers (carbamazepine, efavirenz, phenytoin, rifampin, St. John's wort) |
|
|
DPP-4 inhibitor counseling
|
take once daily in the morning, with or without food
nasopharyngitis, upper respiratory tract infections, hypoglycemia if you have trouble breathing, or any kind of rash, see the doctor at once counsel patients to be seen right away if they develop sx of pancreatitis including severe stomach pain that does not go away, with or without vomiting; pain can radiate from abdomen through to the back |
|
|
GLP-1 agonists MOA
|
glucagon-like peptide-1 agonists (GLP-1 Agonists):
Byetta (exenatide) and Victoza (liraglutide) These agents are analogs of glucagon-like peptide-1 (GLP-1) which increase insulin secretion, decrease glucagon secretion, slow gastric emptying, improve satiety, and may result in weight loss. These are incretin mimetics. |
|
|
how much will Byetta decrease A1C?
|
glucagon-like peptide-1 agonists (GLP-1 Agonists):
Byetta (exenatide) decrease A1C 0.5 - 1 % primarily decrease post-prandial A1C |
|
|
Byetta dosing
|
exenatide (Byetta)
GLP-1 agonist a synthetic version of exenedin, a substance found in Gila monster saliva 5 mcg and 10 mcg pens START: 5 mcg SQ BID for 1 month AFTER 1 MONTH: 10 mcg SQ BID should be given within 60 minutes (usually 30 minutes) before the morning and evening meal abdomen is the preferred injection site, but can use thigh or upper arm count to 5 before withdrawing the syringe can be stored at room temp up to 30 days |
|
|
Victoza dosing
|
liraglutide (Victoza)
GLP-1 agonist Available pre-filled pens: 0.6 mg 1.2 mg 1.8 mg START: 0.6 mg SQ daily x 1 week WEEK 2: 1.2 mg SQ daily x 1 week (can increase to 1.8 mg SQ daily, if needed) given without regard to meals can be stored at room temp up to 30 days |
|
|
how much will Victoza decrease A1C?
|
liraglutide (Victoza)
GLP-1 agonist lowers A1C 0.5 - 1.1 % |
|
|
Byetta side effects
|
exenatide (Byetta)
GLP-1 agonist nausea (primary side effect), vomiting, diarrhea hypoglycemia, weight loss (usually ~ 5lbs) anti-exenatide antibodies can cause pancreatitis Pancreatitis (fatal and non-fatal) is more likely in pt's with risk factors: do not use in pt's with a history of pancreatitis, gallstones, alcoholism, or high triglycerides may cause thyroid neplasms renal: use caution with moderate impairment, AVOID in severe impairment (CrCl < 30) |
|
|
Victoza side effects
|
liraglutide (Victoza)
GLP-1 agonist BBW: thyroid C-cell carcinomas seen in rats and mice - unknown if this could happen in humans. CI in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Side Effects: more weight loss and less hypoglycemia than exenatide N/V/D anti-liraglutide antibodies pancreatitis |
|
|
which GLP-1 agonist generally causes more weight loss?
|
Victoza (liraglutide) causes more weight loss than Byetta (exenatide) typically.
|
|
|
Byetta counseling
|
exenatide (Byetta)
GLP-1 agonist take twice daily in the morning and evening, 30 to 60 minutes before food slows gastric emptying, so administer any other meds 1 hour before injection! if you develop nausea (common), be sure to consume adequate fluids; take fluid replacement if diarrhea or vomiting, and call doc; nausea generally decreases over time so dose can be increased (usually after 1 month, from 5 to 10 mcg BID) administer in thigh, abdomen (preferred) or upper arm; count to 5 before withdrawing syringe! possibility of hypoglycemia or allergic reaction never inject after a meal because of hypoglycemia risk do not store pen with needle attached; can cause Byetta to leak from pen and air bubbles may form in cartridge store at room temp for 30 days, discard after 30 days even if not empty pancreatitis is a rare side effect; report stomach pain with or without vomiting to doctor; limit alcohol consumption |
|
|
Victoza counseling
|
liraglutide (Victoza)
GLP-1 agonist use once daily, without regard to meals (SQ) slows gastric emptying, so administer any other meds 1 hour before injection! if you develop nausea (common), be sure to consume adequate fluids; take fluid replacement if diarrhea or vomiting, and call doc; nausea generally decreases over time so dose can be increased (usually after 1 week, from 0.6 mg - 1.2 mg, some pt's may go to 1.8 mg) administer in thigh, abdomen (preferred) or upper arm possibility of hypoglycemia or allergic reaction never inject after a meal because of hypoglycemia risk do not store pen with needle attached; can cause Victoza to leak from pen and air bubbles may form in cartridge store at room temp for 30 days, discard after 30 days even if not empty pancreatitis is a rare side effect; report stomach pain with or without vomiting to doctor; limit alcohol consumption |
|
|
Symlin MOA
|
pramlintide (Symlin, alone in its class) is a synthetic Amylin Analog (amylin is a human hormone, produced by pancreatic beta cells to assist in post-prandial glucose control)
amylin (and thus pramlintide) slows gastric emptying, preventing an increase in serum glucagon following a meal also increases satiety an "amylomimetic" agent |
|
|
Symlin dosing
|
pramlintide (Symlin)
amylin analog Symlin Pen 120 (Type 2 DM) Symlin Pen 60 (Type 1 DM) can use in both Types 1 and 2; decrease short acting, and fixed-mix (e.g. 70/30) insulins by 50% when starting this drug Type 1: Start at 15 mcg immediately prior to meals - can titrate up to 60 mcg if no significant nausea Type 2: Start at 60 mcg prior to meals - can increase to 120 mcg if no significant nausea administered SQ in abdomen or thigh PRIOR to each meal (greater than 250 calories) |
|
|
Symlin adverse effects
|
pramlintide (Symlin)
amylin analog BBW: co-administration with insulin may induce severe hypoglycemia (usually within 3 hours following dose) Side effects: hypoglycemia (reduce meal time insulins 50% when starting) nausea (30%) anorexia (15%) weight loss CI: gastroparesis hypoglycemia unawareness store pen at room temp up to 30 days |
|
|
Symlin counseling
|
pramlintide (Symlin)
amylin analog inject SQ in abdomen or thigh at least 2 inches away from insulin injection site if you miss or forget a dose, wait until the next meal; do not inject after meals use only for meals > 250 calories pens are good at room temp for 30 days hypoglycemia risk! Your physician should have instructed you to decrease the dose of insulin you take with or before meals by 50% nausea is the most common side effect, mild nausea is more likely during the first few weeks and usually does not last long; important to start at a low dose and increase only as directed |
|
|
Welchol MOA
|
colesevelam (Welchol)
bile acid binding resin resins work by binding bile, blocking reabsorption bile is produced from cholesterol and cholesterol levels decrease the mechanism by which colesevelam improves glycemic control is not known |
|
|
Welchol dosing
|
colesevelam (Welchol)
bile acid binding resin available as 625 mg tabs also 3.75 gram adn 1.875 gram packets for oral solution 6 tabs daily OR 3 tabs BID (with a a meal AND liquid) OR one 3.75 gram packet daily OR 1.875 gram packet BID (dissolved in 1/2 to 1 cup of water) approved for lipids (decreases LDL ~ 20%) AND type 2 DM (decreases A1C ~0.5%, lowers post-prandial glucose) |
|
|
how much does Welchol lower A1C?
|
colesevelam (Welchol)
bile acid binding resin lowers A1C ~0.5% |
|
|
side effects of Welchol
|
colesevelam (Welchol)
bile acid binding resin constipation, abdominal pain, dyspepsia, nausea can increase TG's ~5% decreases absorption of other drugs, the following should be taken 4 hours before Welchol: phenytoin, levothyroxine, glyburide, cyclosporine, oral contraceptives (E + P) Note that Welchol has fewer GI side effects than other agents in this class that are used for lipid lowering (Welchol is the only one that's approved for DM) |
|
|
Welchol drug interactions
|
colesevelam (Welchol)
bile acid binding resin decreases absorption of other drugs, the following should be taken 4 hours before Welchol: phenytoin, levothyroxine, glyburide, cyclosporine, oral contraceptives (E + P) with warfarin, monitor INR frequently during initiation take bile acid resins 4-6 hours before Niaspan |
|
|
Welchol counseling points
|
colesevelam (Welchol)
bile acid binding resin check for other constipating drugs or constipation, and counsel appropriately (laxative, such as senna, or the stool softener docusate, if appropriate); adequate fluid intake is required decreases absorption of other drugs, the following should be taken 4 hours before Welchol: phenytoin, levothyroxine, glyburide, cyclosporine, oral contraceptives (E + P) take tablets with a meal and liquids take powder dissolved in 1/2 to 1 cup of water may take a multivitamin at other time, due to possible risk of lowering A,D,E,K (mostly K) absorption |
|
|
Cycloset MOA
|
bromocriptine (Cycloset)
dopamine agonist bromocriptine is indicated as an adjunct to diet and exercise to improve glycemic control by working with the CNS to decrease insulin resistance |
|
|
How much is Cycloset expected to lower A1C?
|
bromocriptine (Cycloset)
dopamine agonist lowers A1C by 0.5% |
|
|
Cycloset dosing
|
bromocriptine (Cycloset)
dopamine agonist used in DM 1.6 - 4.8 mg daily take with food to decrease nausea start at 0.8 mg daily within 2 hours of waking; if you miss a dose, do not take later in the day titrate in 0.8 mg increments weekly |
|
|
Cycloset side effects
|
bromocriptine (Cycloset)
dopamine agonist nausea, dizziness due to orthostasis (requires slow dose titration) fatigue, headache, vomiting rhinitis, risk of psychiatric effects CI: patients allergic to ergot-related drugs patients with syncopal migraines nursing women |
|
|
Cycloset drug interactions
|
bromocriptine (Cycloset)
dopamine agonist used in DM bromocriptine is extensively metabolized by 3A4; inducers or inhibitors affect levels do not use with other ergot medications; may increase ergot-related side effects or reduce ergot effectiveness for migraines if co-administered within 6 hours of ergot-related drug monitor for hypoglycemia in patients using sulfonylurea - may need dose adjustment |
|
|
AACE recommends against which kinds of insulin, and why?
|
AACE treatment algorithm recommends against the use of REGULAR human insulin ("R") and NPH insulin ("N") if possible.
These insulin preparations do not have a sufficiently predictable time course that adequately mimics the normal physiological profile, and thus they carry an increased risk of hypoglycemia. Basal and rapid-acting insulins should be chosen instead. (However, R and N formulations are less expensive and are still commonly written for) |
|
|
rapid-acting insulins
- which ones are they - how are they used - duration of action |
rapid-acting insulins:
Humalog (lispro) Novolog (aspart) Apidra (glulisine) injected when the person sits down to eat, or up to 15 minutes prior to eating; designed to last for a meal, but can last up to 5 hours duration of action is shorter than regular insulin dosed for the amount of carbohydrate in a meal, or on a fixed regimen; they are clear and can be mixed with other insulins (except glargine and detemir), but are usually given by themselves with meals |
|
|
short-acting insulins
- which ones are they - how are they used - duration of action |
short-acting insulins = "regular" human insulin
- Humulin R - Novolin R usually given in a mixture with longer-acting NPH (or N) insulin in the mixture 70/30 (70% NPH) injected 30 minutes before breakfast & dinner; takes ~ 30 minutes to start working, which is why it is injected 30 minutes prior to the meal no injection of the 70/30 mix is required at lunchtime, because there may be some regular still acting mid-day, and NPH will still be in effect regular insulin lasts 4-6 hours |
|
|
intermediate-acting insulin
- which ones are they - how are they used - duration of action |
intermediate-acting insulin:
- NPH is the only one (Humulin N, Novolin N) this formulation of insulin can last up to 24 hour, but it peaks anywhere from 4-14 hours which can cause hypoglycemia symptoms; this is why AACE treatment algorithm prefers basal insulin for long-term control |
|
|
basal insulin
- which ones are they - how are they used - duration of action |
basal insulins (24-hour insulin)
- Lantus (glargine) - Levemir (detemir) dosed once or twice daily if dosed once daily, usually given at bedtime to ensure no mixing occurs with other insulins (which are usually given at meal times) Lantus has an onset of ~1 hour Levemir has an onset of ~4 hours both last ~24 hours and do not peak (so less risk of hypoglycemia, although if there is hypoglycemia it can last a long time and may require re-treatment) |
|
|
insulin side effects
|
hypoglycemia
weight gain local skin reactions (rotate injection sites) Lantus (glargine) may sting a little when injecting (minor) |
|
|
SLIDING SCALE INSULIN:
BG < 60 mg/dL |
hold insulin, contact MD
|
|
|
SLIDING SCALE INSULIN:
BG 150 - 200 |
give 2 units of insulin
|
|
|
SLIDING SCALE INSULIN:
BG 201 - 250 |
give 4 units of insulin
|
|
|
SLIDING SCALE INSULIN:
BG 251 - 300 |
give 6 units of insulin
|
|
|
SLIDING SCALE INSULIN:
BG 301 - 350 |
give 8 units of insulin
|
|
|
SLIDING SCALE INSULIN:
BG 351 - 400 |
give 10 units of insulin
|
|
|
SLIDING SCALE INSULIN:
BG 401 - 450 |
call MD
|
|
|
Sliding Scale insulin
|
in hospital setting, insulin is often dosed as 1 - 2 baseline injections, plus either regular or rapid-acting insulin, dosed according to a sliding scale
patients can use sliding scales to adjust insulin at home in some cases |
|
|
insulin administration
|
vials and pens in current use are good for 30 days at room temp (keep unopened pens/vials in fridge)
do not shake the insulin vial or pen, gently roll in palms to mix the suspension when mixing R or rapid-acting with NPH, draw up the clear (short-acting) insulin first, then draw up the NPH (cloudy) the abdomen is the preferred injection site pinch a layer of skin tissue and insert needle at 90 or 45 degree angle |
|
|
treatment for gestational diabetes
|
requires tighter BG control
in pregnancy, pre-prandial BG should be < 95 mg/dL A1C should be < 6% nutritional therapy is the standard of care when medication is needed, ADA recommends insulin therapy insulin is the ONLY approved medication for treatment of GDM long-acting basal insulins (Lantus, Levemir) are pregnancy category C and should not be used other medications are used during pregnancy (like metformin and glyburide) and you will see them in practice, but they are not considered 1st line |
|
|
hypoglycemia
|
normal FBG in people w/o diabetes is 70 - 110 mg/dL
hypoglycemia occurs when BG < 70 the lower the level, the more symptomatic the pt at BG < 20, seizures, coma and death can occur sx include dizziness, headache, anxiety, shakiness, sweating, hunger, confusion, clumsy/jerky movements, tremors, blurred vision |
|
|
beta blockers and hypoglycemia
|
BB's can mask shakiness and anxiety from hypoglycemia (but not sweating or hunger)
this is most notable with the non-cardioselective agents (such as carteolol, carvedilol, propranolol and others) cardioselective BB's (atenolol, metoprolol, nebivolol) are used more commonly |
|
|
hypoglycemia treatment
|
15 - 20 g of rapidly absorbed carbs, which could be:
- 3 or 4 glucose tabs - 1 serving of glucose gel - 4 or 5 saltine crackers - 1 tbsp of sugar or honey - 4 oz of juice or non-diet soda - 8 oz of milk BG should be re-tested 15 minutes after treatment to see if it has reached a safe level if not, treatment should be repeated once BG returns to normal, pt should eat a meal to prevent recurrence glucagon is only used if the patient is unconscious 1mg given SQ, IM or IV, or glucose can be given IV (dextrose 10% or 50%) repeat in 15 minutes if BG < 70 |
|
|
A diabetic patient comes in for a new niacin prescription. Choose the correct statements:
a. the use of niacin has likely increased the patient's HDL cholesterol b. niacin may slightly raise her BG levels c. niacin extended-release should be taken in the morning, with food d. A and B e. all of the above |
D
(note: ER niacin is administered at bedtime, after a low-fat snack) |
|
|
A diabetic patient brings her fasting BG recordings into the clinic. Before breakfast, her range is 111 - 143. Her post-prandial (after lunch) range is 190 - 236. According to the ADA, which of the following is correct?
a. her morning FBG levels are controlled b. her morning FBG levels are not controlled c. her lunch-time post-prandial levels are not controlled d. A and C e. B and C |
E
|
|
|
A diabetic patient has a BP of 136/78, and she is taking amlodipine for HTN. Choose the correct statement:
a. she should begin therapy with an ACEI or ARB b. her BP is acceptable; it should be < 140/90 c. she should try and use the DASH diet d. A and C only e. B and C only |
D
|
|
|
You start a diabetic patient on pioglitazone. Which of the following statements regarding pioglitazone is correct?
a. if the patient is also on metformin, their metformin dose should be increased prior to starting pioglitazone b. the starting dose of pioglitazone should be 4 mg once daily c. pioglitazone therapy is contraindicated in cases of nerve damage d. pioglitazone is contraindicated in obesity e. none of the above |
E
|
|
|
What is the primary MOA of metformin?
a. increases pancreatic insulin secretion b. decreases hepatic glucose output c. increases peripheral insulin sensitivity d. enhances the actions of incretins e. alpha-glucosidase inhibitor |
B
|
|
|
which of the following medications can cause hypoglycemia?
a. insulin b. repaglinide c. glimepiride d. A and C only e. all of the above |
E
|
|
|
a patient has been prescribed Actoplus Met; which of the following would be an acceptable substitution?
a. metformin/glipizide b. metformin/glyburide c. metformin/pioglitazone d. glimepiride/pioglitazone e. metformin/repaglinide |
C
|
|
|
which class of diabetes meds puts patients at increased risk for fractures?
|
thiazolidinediones ("glitazones")
- Actos (pioglitazone) - Avandia (rosiglitazone) |
|
|
which diabetes medication puts certain patients at an increased risk for bladder cancer? (and which patients?)
|
Actos (pioglitazone)
increased risk of bladder cancer in pt's who have been using it for longer than 1 year |

