![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back

What kind of desquamation is this?
|
Erythema multiforme
|
|
|
Erythema multiforme
|
Acute self-limited eruption characterized by a distinctive eruption (target lesion)
|
|
|
EM minor
|
Localized eruption of the skin with mild or no mucosal involvement
|
|
|
EM major
|
more sever mucosal and skin disease- potentially life threatening
|
|
|
What causes erythema multiforme?
|
Infections (HSV, mycobacterium, EBV), drugs (PCN, sulfa, anticonvulsants, salcylates, antituberculoids)
|
|
|
Pathophysiology of erythema multiforme
|
immune rxn with epidermal and dermal junction-- epidermal necrosis and blister formation.
|
|

What kind of desquamation is this?
|
Steven Johnson Syndrome
|
|

What kind of desquamation is this?
|
Toxic epidermal necrolysis
|
|

What kind of desquamation is this?
|
Staphylococcal scalded skin syndrome
|
|
|
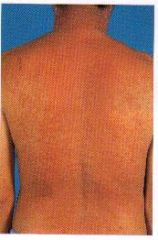
What kind of desquamation is this?
|
Exanthematous drug reaction
|
|

What kind of desquamation is this?
|
Exanthematous drug reaction
|
|
What kind of desquamation is this?
|
Drug hypersensitivity syndrome
|
|
|
Signs and symptoms of Erythema multiforme minor
|
Prodromal symptoms mild/absent. Abrupt onset of rash usually occurs within 3 days, starts on extremities symmetrically with centripetal spreading
|
|
|
Signs and symptoms of erythema multiforme major
|
Most have non specific prodromes; usually 1-4 days before eruption
|
|
|
Skin lesion appearance of erythema multiforme
|
dull red macule or urticarial plaque over 24-48 hours. Small central papule, vesicle, or bulla develops followed by a raised, pale, edematous ring. Periphery eventually becomes cyanotic or violaceous.
|
|
|
Distribution of erythema multiforme
|
extensor surfaces of extremities with central spreading: palms, neck, and face are frequently involved- some mucosal involvement.
|
|
|
Dx of erythema multiforme
|
CBC, electrolytes, BUN, elevated ESR and LFTs, HSV Ag and cultures from blood, sputum, erosive areas
|
|
|
Tx of Erythema multiforme
|
Symptomatic- PO antihistamines, analgesics, local skin care, and soothing mouth washes; topical steroids
Low dose acyclovir for herpes related cases |
|
|
Complications of erythema multiforme
|
secondary bacterial infx, dehydration, blindness, urinary retention, vaginal/urethral stenosis
|
|
|
Prognosis of erythema multiforme minor
|
lesions subside within 2-3 weeks without scarring; recurrence common and mostly preceded by apparent or subclinical HSV infx
|
|
|
Prognosis of erythema multiforme major
|
clearing may take 3-6 weeks; heal with hyperpigmentation/ hypopigmentation. Scarring usually absent
|
|
|
Steven Johnson Syndrome
|
Immune complex-mediated hypersensitivity complex that is a severe expression of erythema multiforme. Sononymous with TEN
|
|
|
Etiology of SJS
|
idopathic in 25-50% cases, infx (HSV, AIDS, mycobacterium), drugs (PCN, sulfa, anticonvulsants), malignancy mediated
|
|
|
Pathophysiology of SJS
|
immune complex mediated hypersensitivity disorder with no etiology in most cases.
|
|
|
Signs and symptoms of SJS
|
Nonspecific URTI, Clusters of mucocutaneous nonpruritic lesions develop abruptly-- MC = trunk. Dysphagia, dysuria, urinary retention, cough with thick sputum, orthostasis, altered consciousness
|
|
|
Dx of SJS
|
biopsy, CBC, UA, BUN, electrolytes, culture.
|
|
|
Tx of SJS
|
Supportive and symptomatic; ***TREAT AS BURN PATIENT without silver sufladiazine.
|
|
|
Toxic Epidermal Necrolysis (TEN)
|
Over 30% of BSA desquamated. Life threatening mucocutaneous skin disorder characterized by widespread erythema, necrosis, and bullous detatchment of the epidermis and mucous membranes, resulting in exfoliation sepsis and death
|
|
|
Etiology of TEN
|
medications (*sulfa)
|
|
|
Pathophysiology of TEN
|
Unknown. Immunologic mechanisms suspected. Epidermal apoptosis also suspected.
|
|
|
Signs and symptoms of TEN
|
Prodrome followed by poorly defined erythematous macular rash with purpuritic centers.--> forms into flaccid blisters and *sheet like epidermal detachment**TRUNK. Positive Nikolsky sign. In mucous membranes first
|
|
|
Dx of TEN
|
Per SJS
|
|
|
Tx of TEN
|
Discontinuation of offending drug and admission to burn unit. ***NO SILVER SULFADIAZINE. Antibx cream only.
|
|
|
Complications of TEN
|
Septicemia, hypoxemia, pulmonary edema, pneumonia, GI hemorrhage, hypovolemia, renal failure
|
|
|
Prognosis of TEN
|
Poor. High mortality rate. Lesions will scar
|
|
|
Staphylococcal Scalded Skin Syndrome (Ritter's disease)
|
Toxin mediated epidermolytic disease characterized by erythema and widespread detachment of the superficial layers of the dermis, most common in newborns.
|
|
|
Localized form of SSSS
|
bullous impetigo (least severe- mouth only)
|
|
|
Generalized form of SSSS
|
extensive epidermolysis and desquamation (body)
|
|
|
Abortive form of SSSS
|
Scarliatiniform variant. Initial rash with NO desquamation.
|
|
|
Etiology of SSSS
|
staph aureus- endotoxins cause disease
|
|
|
Signs and symptoms of SSSS
|
Fever, irritability. Local effects of bullous impetigo. Tender skin- scarlatiniform lesions with sandpaper appearance. Positive Nikolsky's sign. SPARES MUCOUSA! **CONTAGEOUS!
|
|
|
Dx of SSSS
|
gram stain, biopsy (intra-epidermal cleavage with splitting occurring in the stratum granulosum)
|
|
|
Tx of SSSS
|
hospitalization for IV fluids and electrolyte replacement. Use naf, ox, clox (DOC), diclox. Can use silver sulfadiazine.
|
|
|
Prognosis of SSSS
|
Good for children- adult mortality is high.
|
|
|
Toxic Shock Syndrome
|
Acute toxin-mediated illness caused by enterotoxin producing S. aureus characterized by rapid onset of fever, hypotension, generalized skin and mucosal erythema, organ hypoperfusion/MOSF, and desquamation.
|
|
|
Dx of TSS
|
Fever, sunburn rash, hypotension, organ system failure, dequamation (1-2 wks from onset) **MUST HAVE 3
|
|
|
Tx of TSS
|
Admit to ICU, REMOVE OFFENDING AGENT. Supportive treatment. IV antibx (naf, ox, clox, diclox or other PCN reistant)
|
|
|
Prognosis of TSS
|
Mortality rate 5-15%. recurrences reported at 30-40%. STSS- mortality 25-75%
|
|
|
Exanthematous drug reactions
|
MOST COMMON TYPE OF CUTANEOUS DRUG RXN! Adverse hypersentivity rxn to drug characterized by a cutaneous eruption that mimics a measles like viral exanthema (type IV rxn)
|
|
|
Routes for producing an exanthemous drug eruption
|
1. excessive therapeutic effect
2. pharm. side effect 3. immune hypersensitivity |
|
|
Signs and symptoms of an exanthemous drug eruption
|
Pruritic but not painful. Bright red macules and/or papules that may become confluent; resolve in hues of tan and purple. Rash is generally SYMMETRIC- trunk and extremities
|
|
|
Appearance of a drug eruption
|
acne-form, bullous, eczematous, erythema multiforme, fixed drug eruption, hair loss, photosensitivity, pigmentation change, urticaria, vasculitis, possible mucosal involvement
|
|
|
Most common appearance of toxic erythema
|
Morbilliform rash or urticaria, trunk > extremities, accompanied by fever and peeling of the skin. Clears 1-2 wks after stopping drug.
|
|
|
Dx of exanthematous drug reactions
|
Clinical- sometimes by biopsy (perivasular lymphocytes and eosinophils elevated)
|
|
|
Tx of exanthematous drug reactions
|
DIFINITIVE STEP IS TO IDENTIFY THE OFFENDING DRUG AND DISCONTINUE USE. Also, antihistamine and topical steroids.
|
|
|
Drug hypersensitivity syndromes
|
Idiosyncratic drug reactions that begins acutely in the first 2 months after initiation of a drug
|
|
|
Most common drugs which cause hypersensitivity
|
antieptileptic, sulfonamides
|
|
|
Pathophysiology behind drug hypersensitivity reactions
|
Genetically determined inability to detoxify the toxic metabolic products of drugs; increased susceptibility of leukocytes to toxic metabolites.
|
|
|
Signs and symptoms of drug hypersensitivity reactions
|
Onset- 2-6 wks post admin, Rash is on FACE then trunk and extremities- SYMMETRIC. Constitutional symptoms.
|
|
|
Dx of drug hypersensitivity reactions
|
Elevated levels of: eosinophils, WBCs. Mononucleosis-like lymphocytes. Biopsy- mimics cutaneous lymphoma, eosinophils, dermal edema
|
|
|
Diagnostic critera of hypersensitivity rxn
|
1. Cutaneous drug eruption
2. Hematological abnormalities 3. Systemic involvement (heart, liver, kidneys, lungs, lymph) |
|
|
Tx of drug hypersensitivity rxn
|
Identify and discontinue use of offending drug. Symptomatic treatment, antihistamines, topical and systemic steroids PRN.
|

