![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Even though muscle action is understood as concentric contraction, ie. shortening resulting in change in joint angle, to produce everyday movements, muscle action also includes what 2 events?
|
1. isometric contraction (to stablize joints)
2. eccentric contraction , ie. controlled lengthening (ie., contraction while muscle length increases) |
|
|
|
How is sitting accomplished?
|
The iliopsoas is the prime flexor of the hip.
The gluteus maximus is the prime extensor of the hip. Sitting requires flexion at the hip… Which muscle controls sitting? Sitting is accomplished by eccentric contraction of the gluteus maximus; the iliopsoas is not involved. |
|
|
|
Describe the monosynaptic reflex arch and give an example?
|
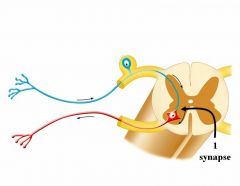
It is the fundamental functional circuit of the nervous system. The knee jerk is a monosynaptic reflex where the afferent synapses directly on the efferent neuron. In a monosynaptic reflex, a muscle either contracts or doesn’t for a given stimulus….So, it is an all or none response, no variation.
|
|
|
|
Describe a disynaptic reflex arch?
|
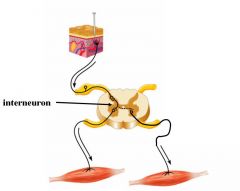
It is the addition of an interneuron between afferent and efferent neurons allowing motor responses to be more complex. For a given set of sensory inputs, the repertoire of motor responses is greatly increased by adding neurons between the input/output elements of a reflex arch.
|
|
|
|
What are the 4 major components of the motor system?
|

SEE DIAGRAM
If you sever the spinal cord of a cat there is a problem Connection between the cortex and spinal cord The cerebellum has no direction with the spinal cord Motor neuron in the spinal cord, the final one is in the alpha motor neuron of the ventral horn, with EFF, ; the gamma is related to muscle spindles |
Company Must = Celebrate PBS
|
|
|
Damage of the spinal cord & lesion of motor pathways below the origin of the brachial plexus (C5-T1) and above S4 results in what?
|
Paraplegia: Paralysis of the lower half of the body with involvement of both legs.
|
|
|
|
Damage of the spinal cord at the origin of the brachial plexus results in what?
|
Quadreplegia: Paralysis of both arms and both legs.
|
|
|
|
Damage of the spinal cord at the origin of the phrenic nerve or above results in what?
|
Asphyxiation and death (without medical intervention)because you sever descending control of the phrenic nerve and you get paralysis of the diaphragm.
|
|
|
|
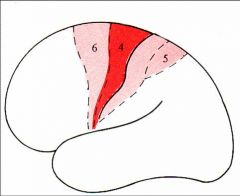
Compare:
1. Precentral gyrus 2. Postcentral gyrus |
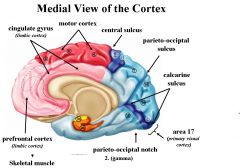
1. The precentral gyrus is the primary motor cortex controlling voluntary movement of skeletal muscle and it has 2 divisions:
A = premotor cortex = areas 6 B = precentral motor cortex (primary motor cortex) = area 4. It occupies most of the precentral gyrus. 2. Postcentral gyrus is the primary somatosensory cortex receiving inputs conveyed by general sensory systems and it consists of the postcentral sensory cortex = areas 3, 1, and 2 Both the motor and somatosensory systems are topographically organized. Their cortical maps form a motor and a somatosencory homunculus. |
|
|
|
Describe the premotor region (area 6) and name its 2 subdivisions?
|
The premotor region (area 6) is found immediately rostral to the primary motor cortex. It is composted of 2 subregions:
1. Premotor cortex 2. Supplementary motor cortex |
|
|
|
1.Even though a cortex typically has 6 layers, what is unique about Areas 4 and 6?
2. Where are the cell bodies of the corticospinal tracts? |
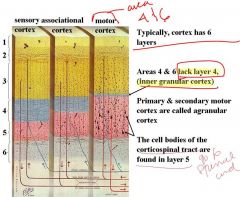
1. Areas 4 & 6 lack layer 4, (inner granular cortex)
2. The cell bodies of the corticospinal tract are found in layer 5 |
|
|
|
Describe the origin of the axons in the corticospinal tract?
|
Approximately ½ of the axons in the corticospinal tract originate in the primary motor cortex (Brodmann’s area 4).
Most of the other axons originate from area 6: mainly from the supplementary motor cortex and a smaller portion from the (lateral) premotor cortex. Parietal cortex (area 5) and somatosenry areas (3, 2 & 1) contributes a small number of axons to the corticospinal tract. |
|
|
|
Electrical stimulation of motor cortex (area 4) leads to what 3 things?
|
It evokes movements of:
1. An individual (or a few) muscle 2. The lowest threshold 3. Short latency |
LISt
|
|
|
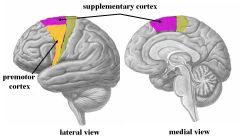
Compare the function of:
1. Primary motor cortex (area 4) 2. Supplementary motor cortex (area 6) |
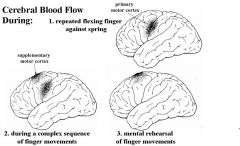
1. The primary motor cortex (area 4) is central in the production of precision, skilled movements by initiating and control the movement's 1. direction, 2. speed, and 3. force.
2. Supplementary motor cortex is important in programming motor sequences and in coordinating bilateral movements and postural responses. Area 6 plans a strategy for movement requiring sequences of muscles contractions or a planned strategy (such as brushing teeth). Supplementary motor cortex controls: a. proximal muscles through the corticospinal tract. b. distal muscles (such as in the hand) through area 4 Therefore, Stimulation of area 6 also evokes movements but at higher threshold than area 4. In contrast to single muscles, stimulation of supplementary cortex produces complex movements involving several joints* (eg., opening and closing the hands), often bilaterally. ASIDE: Premotor (lateral) cortex controls proximal movements that project the arm to targets |
|
|
|
Describe lesions of the internal capsule (capsular)? What is not affected by these lesions and what is affected?
|
Capsular lesions are a common cause of lesions to the corticospinal tract. Capsular lesions are common due to obstruction or hemorrhage of the:
a. deep branches of the middle cerebral b. anterior choroidal artery Usually the face is not affected by a lesion of the posterior limb of the Internal Capsule. The symptoms of capsular lesions are seldom restricted to the “pyramidal syndrome” because other projections pass through the IC including: -thalamic radiations - corticothalamic fibers -corticopontine fibers -corticostriate fibers -corticoreticular Therefore you get a syndrome since so many other structures are affected. |
|
|
|
What will happen if there is a lesion of the cerebral peduncle?
|
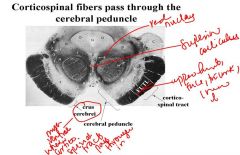
The crus cerebrei of the cerebral peduncle has axons from other tracts so lesions of cerebral peduncle will give you upper motor neuron symptoms.
|
|
|
|
What happens to corticospinal fibers in the pons?
|
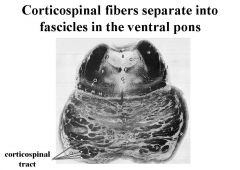
Corticospinal fibers separate into fascicles in the ventral pons
|
|
|
|
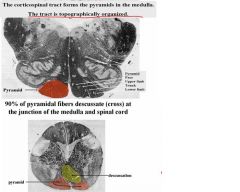
Discuss the corticospinal tract and what it does in the medulla?
|
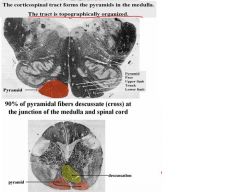
After it forms the pyramids in the medulla, the pyramids will then decussate or cross at the junction of the medulla and spinal cord.
|
|
|
|
What happens if there are lesions of the corticospinal tract prior to the discussation of the pyramids?
|
It produces contralateral signs, including:
1. monoplegia (paralysis of a single limb) 2. hemiplegia (paraylsis of ½ of the body) |
|
|
|
Discuss the formation of the lateral corticospinal tract, and the anterior (ventral) corticospinal tract?
|

SEE DIAGRAM
|
|
|
|
What do they innervate:
1.lateral corticospinal tract 2. anterior (ventral) corticospinal tract |
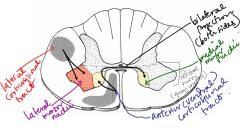
1. The lateral corticospinal tract (white matter) innervates lateral motor nuclei of the ventral horn (gray matter) and the tract is contralateral.
2. The ventral corticospinal tract (white matter) innervates medial motor nuclei of the ventral horn (gray matter)* *Note: some axons of the ventral tract cross at the segmental level; therefore, the projection is bilateral. |
|
|
|
Describe the role of these based on the somatotopic organization of the ventral horn:
1.Lateral motor nuclei 2.Medial motor nuclei |
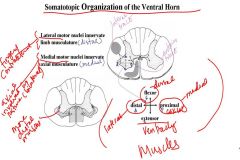
1. Lateral motor nuclei innervate limb musculature
2.Medial motor nuclei innervate axial musculature |
LL
MAximum money |
|
|
Name 4 areas that corticospinal axons synapse on?
|
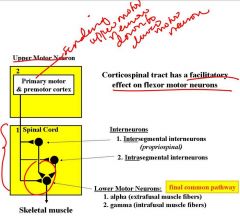
1. alpha motor neurons
2. gamma motor neurons(to muscle spindles) 3. intrasegmental interneurons (that project within the segment) 4. intersegmental interneurons (that ascend & descend to other segmental levels) |
|
|
|
Compare signs of upper motor neuron disease to lower motor neuron disease?
Whaat is unique about diagnosing upper motor neuron disease? |
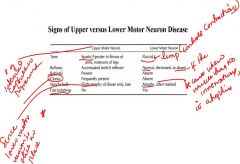
SEE CHART FOR COMPARISON
Very shortly after injury to the brain or spinal cord, upper motor signs may be lacking, and, therefore, may even be falsely interpreted as lower motor neuron signs. Initially, the CNS shuts down where the injury occurs so you get flaccid at first, which is a lower motor neuron symptom. This transient state is known as ‘cerebral’ or ‘spinal shock’ (not to be confused with “shock” due to hypotension. Therefore, only 3 to 4 days after the spinal cord recovers is when you get expression of upper motor neuron signs so give days or a week for diagnosis of upper motor neuron disease. NOTES: Slow degeneration of lower motor neuron is fasciculations For upper motor neuron, there is weakness on the affected side and no flexion of upper limb. |
|
|
|
Describe the corticobulbar pathway?
|
The corticobulbar pathway terminates directly or through the reticular formation (in the brainstem) in cranial nerve nuclei (CN V, VII, IX, X, IX & XII. (Innervation relayed to motor nuclei) It projects bilaterally (with a contralateral predominance) to motor nuclei of CN V, VII**, & XII
|
|
|
|
Compare the bilateral and contralateral projections of the corticobulbar pathway and the effect of lesions on these projections?
|
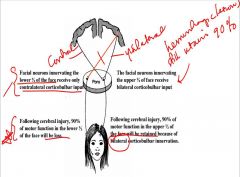
1. Corticobulbar projections to facial nucleus supplying the upper ½ of the face are bilateral. Following cerebral injury, 90% of motor function in the lower ½ of the face will be loss.
So, paresis (not paralysis) or pseudobulbar palsy results if lesioned because of the bilateral input 2. In contrast, the projections to the lower ½ of the face are contralateral. Following cerebral injury, 90% of motor function in the upper ½ of the face will be retained because of bilateral corticobulbar innervation. |
|
|
|
What are the 8 major descending pathways of the spinal cord?
|
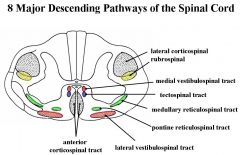
SEE PICTURE
|
TuRn LAMP Light Medium
|
|
|
What are the 2 fiber columns that the descending motor systems are organized into?
|
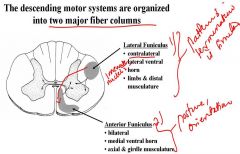
1. Lateral Funiculus
-contralateral -lateral ventral horn -limbs & distal musculature 2. Anterior Funiculus -bilateral -medial ventral horn -axial & girdle musculature |
|
|
|
Describe the RUBOSPINAL TRACT
(indirect corticospinal tract)? |
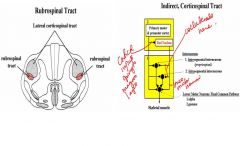
It arises in the contralateral red nucleus of the midbrain and plays a role in the control of flexor tone. It is located ventral to the lateral corticospinal tract. The rubrospinal tract crosses in the ventral tegmental descussation and overlaps with the lateral corticospinal tract in the lateral funiculus
Also, rubospinal firing activity is related to the dynamics of force and to limb velocity. |
|
|
|
Describe the red nucleus?
|
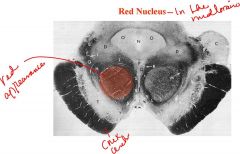
The Red Nucleus is located in the midbrain and it is composed of two parts:
1. magnocellular (caudal, oldest, and largest) 2. parvocellular (rostral, newest) It receives inputs from: 1. cortex (magnocellular) 2. cerebellum (parvocellular) The magnocellular part sends outputs that parallel the contralateral lateral corticospinal tract (axons to spinal cord for the rubrospinal tract) |
|

