![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
298 Cards in this Set
- Front
- Back
|
primary skin lesions
|
- macules, patches - papules, plaques - nodules, tumors - pustules - vesicles, bullas - wheals - cysts |
|
|
macule/patch
|
- area of altered pigment - flat, level w/ the skin - normal skin texture and architecture - ...basically a freckle - macules are small (<1cm), patches are bigger (>1cm) |
|
|
papule
|
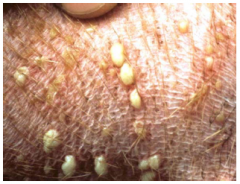
- solid elevated mass - most papule lesions are centered on hair follicles --> folliculitis - <1cm in diameter |
|
|
common ddx for papules
|
- Staphylococcal disorders - parasitic disorders - dermatophytosis |
|
|
nodule
|
- solid elevated mass - >1cm in diameter |
|
|
common ddx for nodules
|
- Staphylococcal disorders - fungal disorders - neoplastic conditions - sterile disorders |
|
|
plaque
|
- flat-topped, solid, elevated masses w/ gradually sloping walls
|
|
|
wheal
|
- flat-topped boggy mass - pits w/ pressure (filled w/ edematous fluid) |
|
|
pustule
|
- fluid-filled lesion filled w/ pus - pus = degenerate PMNs, other WBCs |
|
|
common ddx for pustules
|
- Staphylococcal disorders - sterile disorders |
|
|
vesicles/bullas
|
- fluid-filled lesions, that aren't filled w/ pus - ...basically blisters - vesicles are small <1cm - bulla are bigger >1cm |
|
|
common ddx for vesicles
|
- sterile disorders - vascular disorders - neoplastic conditions |
|
|
cysts
|
- can be congenital or acquired - multiple different kinds - diagnosed by examination of the cyst wall |
|
|
alopecia
|
- complete hair loss
|
|
|
hypotrichosis
|
- less than normal #s of hairs
|
|
|
hypertrichosis
|
- increased #s of hairs
|
|
|
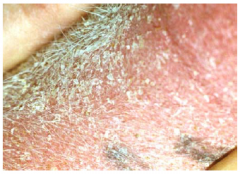
scale
|
- accumulation of exfoliated epithelial cells
|
|
|
crust
|
- dried liquid +/- cells on the skin's surface
|
|
|
comedo
|
- dilated hair follicle filled w/ keratin - blackheads are open - milia are closed |
|
|
hair cast
|
- hair follicle filled w/ keratogenous plug extending above the skin's surface - indicative of a disorder of follicular keratinazation |
|
|
ddx assoc. w/ hair casting
|
- seborrhea - follicular parakeratotic hyperkeratosis - Vit A excess/deficiency - sebaceous adenitis - demodicosis - dermatophytosis - follicular dysplasia |
|
|
secondary skin lesions
|
- epidermal collarettes - excoriations - erosions, ulcers - fissures - scars - lichenification - callus |
|
|
epidermal collarette
|
- "footprint" of a pustule or vesicle - not a good lesion to sample |
|
|
excoriations
|
- self-induced lesions - caused by the animal: scratching, chewing, licking, rubbing, rolling |
|
|
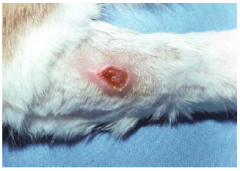
ulcers/erosions
|
- loss of epidermal +/- dermal tissue - erosions: above the BMZ - ulcers: below the BMZ - fissures are linear ulcers |
|
|
lichenification
|
- sign of chronicity - lesions are often hyperpigmented |
|
|
callus
|
- hypertrophied fibrotic material - found over bony prominences - form to protect the underlying tissues |
|
|
configuration of lesions
|
- annular - arciform - polycyclic - linear - serpiginous - central healing |
|
|
surface sampling
|
- fecal float - combing - acetate tape - Q-tip swabbing - direct impression - skin scraping |
|
|
skin scrapings
|
- useful for identifying external parasites - false negatives are common - multiple techniques used/available |
|
|
trichogram
|
- select typical areas - sample 10-15 hairs - mount in mineral oil normal trichogram should have: - mix of anagen and telogen hairs, and primary and secondary hairs - normal hair shaft anatomy - appropriate pigmentation - little to no follicular debris |
|
|
hair growth cycle
|
- hair growth is triphasic - anagen, catagen, telogen - ratio of hairs in each phase changes with breed, season, state of health |
|
|
cytology
|
- useful in inflammatory and neoplastic conditions - prereq. for c/s testing - various collection techniques: touch prep, swab, FNA |
|
|
fine needle aspiration
|
- used to collect samples from solid or deep lesions - suction or trocar methods |
|
|
cytospin cytology
|
- used to sample fluid filled lesions - microhematocrit tubes and centrifuge used - avoid bloody or viscid fluids |
|
|
diascopy
|
- used to differentiate between vascular dilatation and vascular leakage - red skin caused by vascular dilatation blanches w/ pressure - red skin caused by vascular leakage does not blanch w/ pressure |
|
|
dermatophyte test medium
|
- modified Sabouraud's agar w/ pH indicator to detect the dermatophyte - protein metabolism produces alkaline metabolites --> pH change cause red color change - color change and colony growth occur simultaneously - need to check plates every day, be sure to see color change when it first appears; other pathogens will produce color change after longer periods of growth |
|
|
bacterial c/s testing
|
- cytology should always precede culture - indicated when: organism can't be ID, rational tx are ineffective, tx options vary greatly in expense - culture intact lesions - use a reliable lab |
|
|
skin biopsy
|
- underutilized dx - inflammatory lesions should be examined by a veterinary dermatopathologist - incisional or excisional biopsy techniques - biopsy punches are contraindicated in deep or fragile lesions |
|
|
pathologic process of papules/pustules/crusts
|
- invasion of the follicle wall (mural folliculitis) - progression into the follicle lumen (luminal folliculitis) --> makes pus --> pustule - rupture of pustule --> crust OR rupture of hair follicle wall --> furunculosis |
|
|
neutrophilic pustular disorders
|
- bacterial infections - fungal infections - Leishmaniasis - viral infections - Pemphigus foliaceous & erythematosus - drug reactions - subcorneal pustular dermatosis - Sweet syndrome - superficial suppurative necrolytic dermatitis - linear IgA pustular dermatitis - some other autoimmune disorders |
|
|
eosinophilic pustular disorders
|
- pemphigus foliaceus & erythematosus - pemphigus vegetans - drug reactions - sterile eosinophilic pustulosis - sterile eosinophilic folliculidites - sterile eosinophilic pinnal folliculitis - allergic contact dermatitis - idiopathic linear papulopustular acantholytic dermatosis |
|
|
commonest causes of folliculitis in dogs, cats, pigs
|
- Staph infections - demodicosis - dermatophytosis (order varies by species) |
|
|
commonest causes of folliculitis in horses, ruminants
|
- dermatophytosis - dermatophilosis - Staph infections |
|
|
impetigo
|
- "puppy pyoderma" - NONfollicular bacterial (Staph spp.) pustular disease - doesn't bother dog - self-limiting |
|
|
Staphylococcal folliculitis & furunculosis
|
- pre-existing condition needed for infection (i.e. immune deficiency, metabolic disorder, skin disease) - common species: S. pseudintermedius, S. aureus, S. schleiferi - Staph does not normally inhabit/infect face |
|
|
regionalized furuncular disorders
|
- nasal - chin and muzzle - post-grooming - mucocutaneous - acute moist folliculitis & furunculosis - acral lick furunculosis - pedal |
|
|
nasal furunculosis
|
- can occur secondary to nasal trauma (i.e. pruritic disorders, rodent hole burrowing) - a slowly progressive disorder --> take about a week or so for bacterial disease to progress - painful or pruritic - heals w/ scarring |
|
|
chin & muzzle furunculosis
|
- "canine acne" - common in "bristly" coated breeds - initiated by trauma to the chin region (i.e. frisbee, tug-of-war, eating/drinking behaviors) - initially sterile ingrown hairs causing the lesion - heals with scarring |
|
|
post grooming folliculitis & furunculosis
|
- common in short-coated breeds - occurs 12-24 hours after bathing - caused by contaminated shampoos, bathing utensils, or tap water - usu. painful w/ systemic signs of illness - more often Pseudomonas spp. (not Staph.) |
|
|
mucocutaneous staphylococcal pyoderma
|
- chronic, recurrent - common in German Shepherds - infections start at a mucocutaneous junction (i.e. lips, nares, eye lids) |
|
|
acute moist folliculitis & furunculosis
|
- mimics acute, moist dermatitis ("hot spot) - sudden onset of self-trauma to otherwise normal skin - painful - distinguish from hot spot by: palpation (follicular/furuncular lesions are thicker than surrounding skin), presence of satellite lesions (hot spots do not have satellite lesions) |
|
|
acral lick folliculitis & furunculosis
|
- occurs after behavioral issues, skin trauma, or deep seated skin disease - hairs become deeply imbedded - heals w/ scarring |
|
|
pedal furunculosis
|
- triggered by: foot conformation, pruritic pedal disorders, environmental factors - progressive disorder - heals w/ scarring |
|
|
feline Staphylococcal infections
|
- not common - mimics noninfectious miliary dermatitis - secondary to: pruritic skin disorders, chronic corticosteroid use |
|
|
equine Staphylococcal infections
|
- not common - can occur following: skin damage, overzealous treatments by owners |
|
|
manifestations of Dermatophilosis
|
- streptothricosis - rain scald - rain rot - lumpy wool - strawberry foot rot - mycotic dermatitis - aphis |
|
|
otitis
|
- inflammation can be sterile or w/ infection - otitis externa --> affecting the tissues from the pinna to the tympanic membrane - otitis media --> affecting the tissues comprising or contained w/in the middle ear cavity |
|
|
cerumen
|
- yellow, waxy substance made up of the secretions from ceruminous and sebaceous glands, and desquamated keratinocytes - aka ear wax |
|
|
glandular hyperplasia
|
- an increase in the number of glandular cells - typically incited by inflammation |
|
|
stenosis
|
- abnormal narrowing of a structure
|
|
|
fibrosis
|
- excessive fibrous connective tissue formation in a reparative or reactive process
|
|
|
dystrophic mineralization
|
- calcium deposition within cells resulting in phosphate accumulation and microcrystal formation - occurs in response to tissue damage |
|
|
primary causes of otitis externa
|
- primary causes are agents that induce otitis in a NORMAL ear ex: - hypersensitivity disorders - parasites - foreign bodies - keratinization disorders - immune-mediated diseases |
|
|
hypersensitivity induced otitis externa
|
- most common cause of OE in dogs - can include: atopic dermatitis, food hypersensitivities, contact hypersensitivities, adverse cutaneous drug reactions |
|
|
parasite induced otitis externa
|
- mites: Otodectes cynotis, Demodex sp., Sarcoptes sp., Notoedres cati, "chiggers" - ticks: spinose ear tick - flies: stable fly, deer fly |
|
|
keratinization disorder induced otitis externa
|
- can be caused by: chronic ceruminous otitis externa, idiopathic seborrhea, hypothyroidism
|
|
|
secondary causes of otitis externa
|
- secondary causes are agents that induce otitis in an ABNORMAL ear ex: - bacteria: Staph. pseudintermedius, Pseudomonas, Proteus, E. coli, Klebsiella - yeast: Malassezia pachydermatis, Candida sp. - topical acquired irritant reactions |
|
|
factors predisposing to otitis externa
|
- ear conformation - increased relative humidity is most important factor; hairy ear canals - excessive moisture - increased humidity, swimming, contaminated water - obstructive ear disease - nasopharyngeal polyps, ceruminous cystomatosis, ceruminous gland neoplasms - primary otitis media |
|
|
factors perpetuating otitis externa
|
- progressive pathologic changes - glandular hyperplasia, stenosis, fibrosis, etc. - tympanic membrane alterations - otitis media |
|
|
normal ear cytology (cat, dog)
|
- yeast: median of 0.2 yeast per HPF - bacteria: 0-0.3 cocci per HPF; no rods - corneocytes w/ small #s of nucleated keratinocytes |
|
|
bacterial infection
|
- evidence of organisms w/in inflammatory cells on cytology
|
|
|
bacterial overgrowth
|
- evidence of organisms on cytology, but not within inflammatory cells
|
|
|
indications for c/s when tx OE
|
- severe OE w/ rods seen cytologically - poor response to appropriate therapy - presence of otitis media - cytology should always be performed first! |
|
|
indications for otoscopy/myringotomy when tx OE
|
- poor response to therapy - otitis media --> myringotomy, culture, flush - mass/FB --> potential removal or biopsy |
|
|
indications for advanced imaging when tx OE
|
- further assessment of potential otitis media - pre-sx planning |
|
|
tx of OE
|
- correct/manage underlying causes/factors - cleaning - topical therapy - systemic therapy - surgery - follow-up |
|
|
indications for systemic tx of OE
|
- presence of parasites - severe or refractory cases of OE - marked proliferative changes - owner can't administer topical tx - topical adverse rxns are present or suspected |
|
|
sx tx interventions for OE
|
- lateral ear canal ablation - total ear canal ablation +/- bulla osteotomy |
|
|
techniques for draining an aural hematoma
|
- teat cannula - suction drain - multiple perforations w/ skin punch, laser - multiple aspirations - plastic rivets - incision w/ through-and-through sutures |
|
|
aural hematoma
|
- accumulation of blood, intracondrally, within the pinna - secondary to head-shaking/trauma - often assoc. with otitis externa |
|
|
surgical technique for aural hematoma
|
- pt is anesthetized - ear canal examined (must tx underlying OE), pinna clipped and prepped - incision made over the hematoma - fibrinous material removed from hematoma to improve cosmetic result - full thickness sutures are placed parallel to long axis of the incision to minimize ligation of the auricular blood supply - sutures are placed through a non-adherent pad (or buttons!) - left on for 3 wks - wrap can be applied over ear/head to reduce head shaking |
|
|
lateral ear canal resection
|
- sx tx option for non-responsive OE - horizontal ear canal must be patent - provides improved drainage of ear canal, reduces humidity in canal - 50% effective - most still require med tx to control ear disease |
|
|
lateral ear canal resection - sx technique
|
- pinna, ear canal and skin over canal are shaved/prepped - skin incisions made cranial and caudal to tragus; length of incision is 1.5x length of vertical canal - skin flap dissected from SQ - dissection to level of parotid salivary gland - parallel incisions in lateral wall of canal create hinge at junction of vertical/horizontal canals and expose entrance to horizontal canal - skin sutured to canal walls - post-op analgesia, head wrap 3-5 days, abx for 14 days, sutures removed 10-14 days |
|
|
vestibular signs indicating inner ear involvement
|
- head tilt - circling - nystagmus (quick phase away from lesion) |
|
|
feline inflammatory polyps
|
- common in cats age 1-3 y.o. - often hx of URTI - polyps originate in middle ear - poss. immune-mediated rxn to upper resp. virus - CS depend on which way the polyps extend: chronic OE, upper resp. signs, Horner's syndrome, vestibular signs |
|
|
extraction of feline polyps
|
- lateral polyps can be extracted through ear canal - 13-40% recurrence - nasopharyngeal polyps extracted through mouth - 10-41% recurrence - steroids may reduce/prevent recurrence |
|
|
indications for TECA
|
- non-responsive OE w/ severe epithelial hyperplasia - neoplasia in the ear canal - revision of failed lateral ear canal resection |
|
|
`TECA sx technique
|
- T-shaped incision made over ear canal - incision made that encircles the external ear canal - excise ear canal w/ carfeul dissection near facial n. - skin is closed - post-op analgesia, head wrap for 3-5 days, E-collar, 3 wks of abx |
|
|
complications of TECA
|
- 10% facial nerve paralysis - <5% facial fistula - <1% vestibular signs - 100% hearing loss in affected ears |
|
|
when and why to take a skin biopsy
|
- if skin lesions are acute and severe - if the tx for a disorder is assoc. w/ sig. side effects or potentially life-threatening - if you suspect a neoplastic process - if skin lesions appear unusual - if new lesions develop while on therapy - if lesions fail to respond to tx |
|
|
where to take a skin biopsy
|
- biopsy primary lesions - biopsy multiple sites and a range of lesions |
|
|
preparing to take a biopsy
|
- may need abx 2-3 wks before biopsy - eliminate secondary infections that may mask pathology - stop PO/topical steroids 2-3 wks before and injectable steroids 6 wks before biopsy |
|
|
biopsy techniques
|
- trim hair, but not too close - never scrub the surface! - use local anesthetic - use 6-8mm biopsy punch for haired skin - use 4mm biopsy punch for footpad, nasal planum, near eyes/eyelids - use elliptical/wedge biopsies for fragile and deep lesions |
|
|
taking a biopsy of an area of depigmentation
|
- take a margin - an area where it is actively depigmenting |
|
|
taking a biopsy of an area of alopecia
|
- take a biopsy of 1) an area of alopecia, 2) an area of hypotrichosis, and 3) a normally haired area for comparison
|
|
|
taking a biopsy of an ulcer/erosion
|
- take a wedge biopsy from the junction of the ulcerative and non-ulcerative skin
|
|
|
DON'Ts of skin biopsy
|
- don't prep/scrub - don't clip the hair too close - don't crush/squeeze the samples - don't use resterilized punch biopsy instruments - don't use cautery on small samples - don't ship samples over the weekend during the winter --> freezing - don't use punch biopsies on fragile or deep lesions - take a wedge or elliptical sample |
|
|
hyperkeratosis
|
- epidermal change - increased thickness of the stratum corneum - orthokeratotic - no nuclei - parakeratotic - have retained nuclei |
|
|
epidermal hyperplasia
|
- epidermal change - aka acanthosis - increased thickness of the non-cornified epidermis due to an increased # of epidermal cells - can be: regular, irregular, psoriasiform, papillated, pseudocarcinomatous |
|
|
apoptosis
|
- intentional cell suicide - non-inflammatory - activated by growth factors, cytokines, hormones, immune system, viruses, sublethal cell damage - can be seen in small #s in any hyperplastic epidermis |
|
|
intercellular edema
|
- epidermal change - "spongiosis" - widening of intercellular spaces, formation of spongiotic vesicles - common in acute or subacute inflammatory dermatosis |
|
|
intracellular edema
|
- epidermal change - increased size, cytoplasmic pallor, displacement of nucleus - common feature of acute or subacute inflammatory dermatosis |
|
|
ballooning degeneration
|
- epidermal change - "koilocytosis" - type of degeneration seen in epidermal cells - swollen, stippled cytoplasm w/o vacuolization - enlarged or condensed, sometimes multiple, nuclei - specific feature of viral infections |
|
|
hydropic degeneration of basal cells
|
- epidermal change - intracellular edema in the stratum basale - uncommon finding |
|
|
acantholysis
|
- epidermal change - loss of cohesion between epidermal cells --> clefts, vesicles, bullae |
|
|
exocytosis
|
- epidermal change - migration of inflammatory cells or erythrocytes through the intercellular spaces of the epidermis - common feature of any inflammatory dermatosis |
|
|
microvesicles, vesicles, bullae
|
- epidermal change - fluid-filled, relatively acellular spaces - can be caused by intercellular edema, ballooning degeneration, acantholysis, hydropic degeneration, subepidermal edema or autoantibodies |
|
|
microabscesses and pustules
|
- epidermal change - cavities w/ inflammatory cells - pustules are grossly bigger than miscroabscesses |
|
|
crusts
|
- epidermal change - consolidated dessicated surface mass composed of keratin, serum, cellular debris and microorganisms - can be serous, serocellular, cellular, hemorrhagic, palisading - crusts indicate a prior exudative process |
|
|
changes seen in collagen
|
- hyalinizaton - lysis and loss of structural details - dystrophic mineralization - atrophy - dysplasia - "flame figures" |
|
|
pigmentary incontinence
|
- dermal change - melanin granules free w/in the subepidermal and perifollicular dermis and w/in macrophages - can be seen in any process that damages the stratum basale and the BMZ |
|
|
edema |
- dermal change - dilated lymphatics, widened spaces btwn blood vessels and perivascular collagen, or widened spaces between areas of collagen - common in any inflammatory dermatosis |
|
|
mucinosis
|
- dermal change - large amounts of amorphous, stringy, granular, basophilic material that separates, thins, or replaces dermal collagen fibrils and surrounds blood vessels and adnexae |
|
|
perivascular dermatitis
|
- superficial is more common - hypersensitivity, ectoparasites, dermatophytosis, dermatophilosis, nutritional deficiencies, seborrheic disorders, contact dermatitis - deep is less common - systemic disorders, severe local reactions |
|
|
interstitial dermatitis
|
- infiltration of cells btwn collagen bundles of the dermis - infiltrate is poorly circumscribed, mild to moderate, does not obscure anatomy of the skin |
|
|
vasculitis
|
- immune and non-immune mechanisms - most thought to be immune-complex or type-III hypersensitivity |
|
|
nodular dermatitis
|
- discrete clusters of cells
|
|
|
diffuse dermatitis
|
- denotes a cellular infiltrate so dense that discrete cellular aggregates are no longer easily visualized and the anatomy of the skin is obscured
|
|
|
interface dermatitis
|
- dermoepidermal junction is obscured by hydropic degeneration, lichenoid cellular infiltrate, or both
|
|
|
intraepidermal vesicular and pustular dermatitis
|
- most useful to classify intraepidermal vesicles and pustules to their anatomic level of occurrence w/in the epidermis
|
|
|
perifolliculitis
|
- accumulation of inflammatory cells around a hair follicle
|
|
|
folliculitis
|
- mural folliculitis: wall of the follicle is targeted - luminal folliculitis: accumulation of inflammatory cells w/in the lumen |
|
|
furunculosis
|
- follicular rupture - most commonly occurs as a result of luminal folliculitis - usu. assoc. w/ pyogranulomatous inflammatoin, eosinophils --> FB rxn to free keratin and hair shafts |
|
|
atrophic dermatosis
|
- characterized by varying degress of epithelial and connective tissue atrophy - may show following histopath changes: hyperkeratosis, atrophy, follicular keratosis, follicular atrophy, telogenization, flame follicles, epithelial melanosis, sebaceous gland atrophy |
|
|
panniculitis
|
- inflammation of the subcutis
|
|
|
cause of dermatophytosis
|
- Microsporum spp. and Trichophyton spp. infect animals most frequently - M. canis most common in cats, dogs |
|
|
pathogenesis of dermatophytosis
|
- more common in hot, humid climates - more common in very young, old, or immunocompromised - transmitted through contact w/ infected animals, environment, or fomites - arthrospore is infective portion - surives up to 18 mos. in environment - spore invades anagen hair follicle, adheres to keratin and germinates - clinical lesions appear in 7-14 days |
|
|
dermatophytosis in dogs
|
- less than 5% of derm cases - usu. in dogs less than 1 y.o. - infection usu. localized to face, pinnae, paw, tail - variably pruritic |
|
|
sylvatic ringworm
|
- acquire from wildlife - more common in adults - M. persicolor, T. mentagrophytes |
|
|
other lesions assoc. with canine dermatophytosis
|
- onchomycosis - rare, more common w/ sylvatic spp. - fungal kerion on face or distal limbs |
|
|
feline dermatophytosis
|
- #1 dermatitis in cats - annular areas of alopecia, +/- scales - lesions on head, pinnae, paws - most common in young cats <1 y.o. - variably pruritic |
|
|
other lesions assoc. with feline dermatophytosis
|
- onchomycosis - rare - widespread, severe alopecia w/ little inflammation - pruritic military dermatitis - chin folliculitis - seborrheic-like eruption - resembling pemphigus foliaceous |
|
|
equine dermatophytosis
|
- #2 dermatitis in horses, ~9% of skin disease - Trichophyton equinum most common - usu. in animals <2 y.o. - usu. minimally pruritic - lesions on face, beck, dorsolateral thorax and girth - lesions usu. multifocal, rarely generalized |
|
|
bovine dermatophytosis
|
- Trichophyton verrucosum most common - usu. in animals <1 y.o. - more common in fall, winter in confined animals - crusted papules --> thick gray crusts on face, head, pinnae, neck, rump, tail, perineum |
|
|
caprine dermatophytosis
|
- Trichophyton verrucosum most common - usu. in animals <1 y.o. - lesions on face, head, pinnae, neck and legs |
|
|
porcine dermatophytosis
|
- Microsporum nanum most common - brown to orange annular crusts on face, pinnae, trunk - alopecia and pruritus are rare |
|
|
dx of dermatophytosis
|
- hx - PE: folliculitis - Wood's lamp... lots of false + and - - scrapes and trichograms - fungal culture - most reliable - biopsy |
|
|
dermatophyte fungal culture
|
- Dermatophyte test medium - Sabouraud's dextrose agar + antimicrobial agents to deter growth of other organisms - phenol red in agar turns red as fungus grows and produces alkaline metabolites |
|
|
goals of dermatophyte treatment
|
- maximize the pt's ability to respond to tx - good nutrition, tx underlying conditions, avoid immunosuppression - reduce contagion - hasten resolution of the infection - in-contact animals - environment |
|
|
Malassezia dermatitis
|
- M. pachydermatis part of normal flora in dogs, cats - found in haired skin, ear canals and mucosal areas - underlying causes: atopic dermatitis, food allergy, endocrinopathy, keratinization disorders, metabolic disease, corticosteroids - causes hypersensitivity in dogs - pruritic, alopecia, excoriations, erythema, seborrhea, lichenification, hyperpigmentation, hyperkeratotic |
|
|
dx of Malassezia
|
- hx - PE - smears/impression/tape - culture (normal flora) - biopsy - response to tx |
|
|
tx of Malassezia
|
- address predisposing causes - topicals for localized dz - systemic antifungals for severe, generalized, chronic or deep infections |
|
|
nodules
|
- circumscribed, solid lesions greater than 1cm in diameter - may be elevated above skin's surface or completely SQ - nodules can also be described as tumors... |
|
|
tumors
|
- defined as a swelling of part of the body - abnormal benign or malignant new growth of tissue |
|
|
plaques
|
- circumscribed, solid, elevated and flat-topped
|
|
|
causes of nodules, tumors, plaques
|
- inflammation - neoplasia - cysts - hamartomas - benign focal malformations, resemble neoplasms |
|
|
sterile granuloma syndrome
|
- common in cats, dogs, horses - cause usu. unclear - on cytology: granulomatous, pyogranulomatous, eosinophilic - culture to exclude infection |
|
|
feline eosinophilic granuloma complex
|
- reaction pattern, not a dx - causes can include: allergies to environment, food, fleas, mosquitoes; idiopathic - common cutaneous, mucocutaneous, oral mucosal lesion of cats - papular, nodular, raised oval to linear plaques - firm, erythematous to orange-yellow - chin and caudal thighs are common sites |
|
|
feline eosinophilic plaques
|
- severely pruritic - well-circumscribed, raised, erythematous, eroded, oozing, often ulcerated - oval to linear - abdomen and medial thighs most common |
|
|
feline indolent ulcer
|
- common oral mucosal lesions - usu. near upper lip near philtrum - may be early reaction to flea allergic dermatitis |
|
|
equine eosinophilic granuloma
|
- common in spring, summer - round, elevated, well-circumscribed - non-painful, non-pruritic - caused by: hypersensitivity, trauma, body-clipping, injection sites |
|
|
Habronema
|
- common cause of eosinohilic granulomas in horses - pruritic - possibly a hypersensitivity rxn |
|
|
panniculitis
|
- most cases are sterile and idiopathic - other causes: infectious, drug reactions, vaccine and other injections, FB, pancreatitis, neoplasia, nutritional deficiencies, trauma, burns - most common in dogs; cats, horses - commonly occurs on the trunk |
|
|
cutaneous cysts
|
- non-neoplastic, simple sac-like structure with an epithelial lining - usu. solitary lesions - common in head, neck, trunk, proximal limbs - can be: follicular, epithrichial, dermoid, sebaceous |
|
|
follicular cysts
|
- well-circumscribed, round, smooth, firm to fluctuant lesions - dermal to SQ - can arise from different portions of the hair follicle (i.e. infundibular, isthmal, matrical...) |
|
|
epithrichial gland cysts
|
- common in dogs; uncommon in cats - caused by duct obstructions - well-circumscribed, smooth, tense to fluctuant lesions - may be alopecic w/ a blue hue - common on head, neck and limbs |
|
|
dermoid cysts
|
- developmental abnormality, congenital, hereditary - lesions can be solitary or multiple - lesions often along dorsal midline |
|
|
sebaceous gland cysts
|
- rare - occur in sebaceous ducts - solitary, firm, <1 cm |
|
|
trichoblastoma (basal cell tumors)
|
- common in adult/old cats - usually benign - freq. melanotic - may be alopecic, ulcerated |
|
|
sebaceous gland tumors
|
- nodular hyperplasia - adenomas, epitheliomas, carcinomas - common in adult/old dogs - smooth, shiny pink to orange papules --> cauliflower-like - +/- hyperpigmented, ulcerated |
|
|
epitrichial sweat gland tumors
|
- adult dogs, cats - can be benign or malignant - solitary lesions on head, neck, trunk, limbs - commonly blue, cystic - may be solid, ulcerated |
|
|
lipoma
|
- very common in adult/old dogs - common on trunk, abdomen, proximal limbs - well-circumscribed, soft to firm, SQ |
|
|
mast cell tumors
|
- common in dogs - dermal or SQ - variable appearance and biologic behavior |
|
|
histiocytoma
|
- common in dogs under 2 y.o. - tumors of Langerhans cells - usu. solitary lesions on head, pinnae, limbs - appear suddenly, often ulcerated - spontaneous remission in several months |
|
|
melanocytic neoplasms
|
- 70% are benign - usu. solitary masses on head, trunk - lesions on digits, scrotum, lips more commonly malignant |
|
|
equine melanoma
|
- common in old gray horses on perineum, tail, pinna, periocular, distal limbs - 2/3 metastasize eventually, freq. w/o clinical signs |
|
|
equine sarcoids
|
- most common equine skin neoplasm - occur commonly on inguinal area, head, axilla, abdomen, thorax, neck, distal limbs - locally aggressive, but not metastatic - genetic, viral, trauma - can be occult, verrucous, nodular, fibroblastic, malevolent |
|
|
pruritus
|
- unpleasant sensation that provokes the desire to scratch - physiologic or pathologic - pruritic and painful stimuli carried on same nerve fibers |
|
|
methods of itching in animals we treat
|
- scratching - licking - chewing - rubbing - rolling |
|
|
triggers for "pruritus"
|
- behavioral disorders - orthopedic disease - neurologic disease - skin disease - lesional or "normal" skin |
|
|
behavioral skin dz
|
- rare - always assoc. w/ other behavioral signs |
|
|
neurogenic/orthopedic skin disease
|
- uncommon to rare - localized - variable speed of onset and intensity of pruritus |
|
|
common lesionless pruritic disorders in dogs
|
- flea bite hypersensitivity - atopic dermatitis - food hypersensitivity - Cheyletiella infestation - Demodex injae infection |
|
|
common lesionless pruritic disorders in cats
|
- flea bite hypersensitivity - Cheyletiella infestation - atopic dermatitis - food hypersensitivity - Demodex gatoi infestation |
|
|
common lesionless pruritic disorders in horses
|
- Culicoides hypersensitivity - Chorioptic mange - atopic dermatitis |
|
|
common lesionless pruritic disorders in farm animals
|
- Chorioptic mange - P. tenuis |
|
|
flea dermatitis
|
- CS due to irritation or allergy - pruritic papular eruptions on: dogs - rump, inguinal, posterior thighs; cats - neck, rump |
|
|
atopic dermatitis
|
- genetically predisposed inflammatory and pruritic skin disease w/ CS assoc. w/ IgE antibodies most commonly to environmental allergens
|
|
|
atopic-like dermatitis
|
- genetically predisposed inflammatory skin disease w/ CS identical to atopic dermatitis in which IgE antibodies to environmental allergens are not demonstrable - ...atopic dermatitis that you can't attribute to environmental allergens |
|
|
canine atopic dermatitis
|
- early onset (6-36 mos.) - breed disposition, family hx - seasonal --> increased severity and duration - CS: recurrent OE, pruritus of face, ears, feat, axilla, inguinal area; Staph pyoderma, Malassezia dermatitis, pyotraumatic dermatitis, acral lick dermatitis, anal sacculitis, hyperhidrosis |
|
|
feline atopic dermatitis
|
- onset between 1-3 y.o. - can have lesional or non-lesional pruritus - protracted seasonality - CS: pruritic otic dz, pruritus of face, head and neck; miliary dermatitis, traumatic alopecia, eosinophilic granuloma complex |
|
|
equine atopic dermatits
|
- early age onset (1.5-6 y.o.) - seasonal or non-seasonal at onset - presents variably - nonlesional pruritus, urticaria, symmetrical eosinophilic folliculitis |
|
|
dx, tx of atopic dermatitis
|
dx: - hx, PE - eliminative testing - allergy testing?? tx: - resolve secondary disorders - removal allergens - medical management w/: glucocorticoids, antihistamines, NSAIDs, cyclosporine, Janus kinase inhibitor (Apoquel) - (should resolve w/ steroids) - allergen-specific immunotherapy |
|
|
food hypersensitivity
|
- allergens usu. water-soluble glycoproteins - variable clinical presentation - skin, non-skin, combination - sources of exposure: daily ration, treats, supplements, meds, scavenged foods, "digested" allergens, water |
|
|
CS of canine food allergy
|
- CS: urticaria, atopy-like pruritus, OE, acute moist dermatitis, lumbosacral pruritus, scabies-like pruritus
|
|
|
CS of feline atopy or food hypersensitivity
|
- CS: pruritic OE, pruritus or face, head and neck; miliary dermatitis, traumatic alopecia, eosinophilic granuloma complex
|
|
|
CS of equine food hypersensitivity
|
- CS: atopic-like pruritus, non-pruritic urticaria, pruritic urticaria
|
|
|
Cheyletiellosis
|
- ectoparasite w/ caudo-dorsal distribution - 3 wk life cycle - eggs cement to hair shaft - CS: none --> seborrhea +/- pruritus --> scabies-like pruritus |
|
|
canine demodicosis
|
- D. injae - initial lesions present in sebaceous regions - face, chin, feet, dorsal midline - non-pustular, facial and pedal pruritus |
|
|
feline demodicosis
|
- D. gatoi - ectoparasite - contagious - CS variable - lesions start ventrally and move dorsal |
|
|
causes of tailhead rubbing in horses
|
- Culicoides hypersensitivity - pediculosis (lice) - stall vice - psoroptic mange - oxyuriasis (pin worms) - allergy |
|
|
control of Culicoides
|
- environmental changes - mosquito traps - body suit - on-horse insecticides - selective stabling - paddock fans |
|
|
Chorioptic mange
|
- common in winter - 21 day life cycle - can survive off host for 70 days - tx: clean environment, tx everyone, topicals best (permethrin sprays, selenium sulfide shampoo, fipronil spray, lime sulfur dips) |
|
|
disorders of keratinization
|
- altered epidermal turnover - altered epidermal hydration - altered epidermal differentiation - altered lipid formation or deposition - any combination thereof |
|
|
antiseborrheic therapy
|
- ID and resolve triggering event - topical and systemic agents can treat seborrhea - tx secondary bacterial or yeast dermatitis |
|
|
antiseborrheic bathing
|
- results of bathing influenced by: frequency, thoroughness and the shampoo used - a prebathing bath may be beneficial - contact time w/ the shampoo is important: 10-15 minutes |
|
|
primary disorders of keratinization in dogs
|
- ichthyosis - follicular parakeratosis - epidermal dysplasia - primary seborrhea - primary sebaceous hyperplasia - sebaceous adenitis - ectodermal dysplasia |
|
|
primary disorders of keratinization in cats
|
- ichthyosis - primary seborrhea |
|
|
ichthyosis
|
- rare - onset at, near birth - flaky skin, large plates of scales, worse in "seborreic trouble spots" - interdigital, axilla, skin folds... |
|
|
follicular parakeratosis
|
- rare - only affects females - are often stunted and have other non-cutaneous defects |
|
|
epidermal dysplasia
|
- only in Westies - keratinization defect w/ susceptibility to Malassezia hypersensitivity - onset between 6-12 mos. - variably greasy and pruritic |
|
|
control of Malassezia
|
- topical agents (i.e. chlorhexidene, miconazole, ketoconazole, zymox, enilconazole) - systemic agents (i.e. -conazoles, terbinafine) - therapeutic of maintenance protocols |
|
|
canine generalized primary seborrhea
|
- early onset in life - involves al keratinized surfaces - worsens with age - very susceptible to secondary bacterial or yeast infections - no systemic complaints |
|
|
ectodermal dysplasia
|
- congenital abnormality of pilosebaceous unit - results in follicular hypoplasia, abnormal sebaceous and/or epitrichial sweat glands - worsens with age- tx: moisturizers, topical kerolytics, systemic agents |
|
|
canine generalized secondary seborrhea
|
- common - can onset at any point in life - may involve all keratinized surfaces - very susceptible to secondary bacterial or Malassezia infections - can have variable systemic signs |
|
|
feline generalized secondary seborrhea
|
- low incidence - can onset at any point in life - may not involve all the keratinized surfaces - very susceptible to secondary bacterial or Malassezie infections - can have variable systemic signs |
|
|
exfoliative dermatoses
|
- many different causes - indicative of serious disease - epidermis comes off in large sheets |
|
|
localized acquired disorders of keratinization in dogs
|
- callus - nasodigital hyperkeratosis - ear margin dermatosis - tail gland hyperplasia |
|
|
localized acquired disorders of keratinization in cats
|
- feline acne - tail gland hyperplasia |
|
|
callus
|
- hyperkeratotic plaques over pressure points - environmental trigger - not a medical problem |
|
|
senile nasodigital hyperkeratosis
|
- common - middle to old dogs - uncommonly symptomatic - does not typically require tx - can try hydration (Vaseline) or keratolytic products |
|
|
feline acne
|
- common - single, multiple or persistent episodes - usually doesn't bother cat at all - chronic cases should be checked for Malassezia, Demodex - tx: manual evacuation, topical keratolytics, systemic glucorticoids, abx or retinoids |
|
|
hypotrichosis
|
- condition of abnormal hair loss
|
|
|
hypertrichosis
|
- abnormal amount of hair growth
|
|
|
alopecia
|
- partial or complete absence of hair from areas of the body where it normally grows
|
|
|
mechanisms of hair loss
|
- trauma - hair follicle inflammation - hair follicle irregularity |
|
|
endocrine hair loss
|
- variable systemic signs - coat changes due to: altered hair follicle growth rate, altered hair follicle cycle, hair follicle receptor interactions |
|
|
canine hypothyroidism
|
- most common endocrine disease - T4 needed to institute anagen phase of hair cycle - hairs already in anagen show decreased growth rate - hair loss first occurs in frictional areas - CS: lethargy, dullness, weight gain, heat seeking, skin changes, CV signs, neuropathy, myopathy, repro system irregularities |
|
|
feline thyroid disease
|
- hypothyroidism: rare - hyperthyroidism: uncommonly see skin signs |
|
|
canine hyperadrenocorticism
|
- predictably progresses from systemic signs --> altered hair coat --> hair loss - excess steroids result in: decreased sebum secretion, decreased epidermal turnover, slowed hair growth, delayed hair regrowth, altered coat color, comedones - CS: pu/pd, polyphagia, hepatomegaly, pot-bellied, skin changes, anesterus/testicular atrophy, virilization, hypertension, excessive bruising, poor wound healing, secondary infection, increased panting, neuro signs |
|
|
feline hyperadrenocorticism
|
- rare - skin changes variable and atrophic |
|
|
gonadal sex hormone disorders
|
- systemic signs usually absent - results in patterned alopecia - variable coat color alteration - androgen and estrogen receptors on hair follicles vary w/ # and affinity w/ gender and body site |
|
|
male pattern alopecia
|
- rump - caudal thighs - collar - shoulders |
|
|
female pattern alopecia
|
- flank - caudal thighs - ventrum - back of head |
|
|
gonadal disorders of intact female
|
- hyperestrogenism - hyperprogesteronism - cutaneous pseudocyesis - primary anestrous - estrogen responsive alopecia |
|
|
hyperestrogenism
|
- caused by ovarian tumors, cysts - signs of constant estrus, acromegaly, DM - patterned alopecia - comedones |
|
|
cutaneous pseudocyesis
|
- hair loss starts ~ 6 wks post-estrus - usu. w/ behavioral and/or mammary changes - resolves spontaneously |
|
|
gonadal disorders of intact male
|
- testicular neoplasia - "normal" testes - hyperandrogenemia - primary testicular atrophy |
|
|
testicular neoplasia
|
- most tumors are benign - estrogens produced by Sertoli cell tumors and seminomas - testosterone produced by interstitial cell tumors |
|
|
Otodectes cyanotis
|
- nonburrowing psoroptid mite - 3 wk life-cycle; 2 month lifespan - host non-specific - can be found in ears and on the body - feeds on cell debris and tissue fluid - tx: parasiticidal otic preps, ivermectins, avermectins, isoxazolines |
|
|
Cheyletiellosis
|
- non-host specific - 3 wk life cycle - can survive off the host for 10 days - surface parasite, eggs cemented to hair shaft - CS: dorsally-oriented seborrhea, pruritus - dx: fecal float, acetate tape impression, flea comb, skin scrape?? - tx: lime sulfur, fipronil, avermectins |
|
|
canine scabies
|
- Sarcoptes scabiei var. canis - 17-21 day lifecycle - off-host survival influenced by temperature and humidity - burrowing, lives w/in epidermis - incubation period of about >30 days - prefers ears, elbows, feet, ventrum and hocks - intensely pruritic - dx: skin scrape - tx: lime sulfur, amitraz, fipronil, avermectins, isoxazolines |
|
|
feline sacbies
|
- Notoedres cati or Sarcoptes scabiei - rare - mites are easy to demonstrate- tx: lime sulfur, amitra, fipronil, avermectins |
|
|
demodicosis
|
- 3 species: D. canis, D. cornei, D. injae - part of normal fauna - transferred to neonate while nursing, otherwise not contagious between adults - resides in the hair follicle - feeds on sebum and cellular debris - 28-35 day life cycle - dx: skin scraping, trichogram, pustular cytology - tx: symptomatic tx, miticidal agents (Mitiban, avermectins, isoxazolines) |
|
|
localized canine demodicosis
|
- uncertain pathogenesis - disease of young dogs - can cause hair loss or ceruminous OE - tx: mild topical agents, ear cleaners, topical parasiticides |
|
|
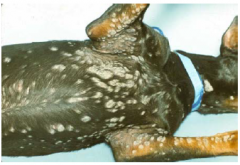
generalized canine demodicosis
|
- serious - disease of the mite-specific immuno-incompetent --> genetic predisposition - clinical presentations: multifocal lesions, facial dermatitis, pododermatitis, seborrhea, widespread dermatitis, pyoderma |
|
|
juvenile-onset demodicosis
|
- onset between 3-18 mos. - genetically predisposed - self-curing usu. |
|
|
adult-onset demodicosis
|
- onset over 4 yrs - triggered by systemic dz: endocrine disorders, neoplasia, others?? |
|
|
D. injae
|
- non-pustular - lesions in "sebaceous" regions (face, chin, feet, dorsal midline) - pruritic - mites are deep in follicle - tx: Mitaban, avermectins, isoxazoline |
|
|
feline demodicosis
|
- uncommon - D. cati, D. gatoi, maybe others - tx: lime sulfur, amitraz, ivermectin, Advantage Multi |
|
|
D. cati demodicosis
|
- assoc. w/ immunosuppression - follicular or otic - dx: skin scrape - tx: difficult |
|
|
D. gatoi demodicosis
|
- surface parasite - contagious - starts on the ventrum - dx: fecal float, tape |
|
|
disorders caused by insects
|
- pediculosis - flea dermatitis - fly dermatitis - myiasis - hymenoptera |
|
|
tick control
|
- environmental management - manual removal - topicals (fipronil, avermectins, etc.) - collars (Seresto, Scalibor, PReventic) - systemics (ivermectin, selamectin, isoxazolines) |
|
|
pediculosis
|
- species specific - 14-21 day life cycles - 1-2 day off host survival - eggs are operculated, cemented to hair shaft - tx: topicals (Advantage, Frontline) |
|
|
fleas
|
- numerous spp. and ssp. - feed on blood, bite is irritating/allergenic - vector disease - survivability and rate of development dependent on temp. and humidity - life cycle 21-28 days - tx: treat environment, flea combing, topical insecticides/IGRs, orals |
|
|
flea dermatitis
|
- CS due to irritation or allergy - pruritic papular eruptions - dogs: rump, inguinal region, posterior thighs - cats: neck, rump |
|
|
pyrethrins/permethrins
|
- insect repellent - can be neurotoxic at high doses - use w/ caution in cats (some are ok, some are not) |
|
|
amitraz
|
- acaricide, insecticide and insect repellent - neurotoxic at high doses |
|
|
imidocloprid
|
- insecticide
|
|
|
fipronil
|
- insecticide
|
|
|
avermectins
|
- macrocyclic mactone derivatives - anthelminthic, insecticide |
|
|
milbemycins
|
- group of macrolides similar to avermectins - anthelminthic, insecticide |
|
|
spinosad - spinetoram
|
- insecticidal
|
|
|
metaflumizone
|
- insecticide
|
|
|
dinotefuran
|
- insecticide
|
|
|
isoxazolines
|
- afoxolaner, furlaner, sarolaner - insecticide, acaricide |
|
|
factors impacting selection of a parasiticide
|
- site of parasitism - life cycle of parasite - off host survival - feed behavior of parasite - owner issues (i.e. chemical sensitivities) - animals issues (i.e. thick hair coats, no hair, swimming, etc.) |
|
|
Seresto collars
|
- anti-flea and tick- rx dispensed over skin in sebum - effective in 24-48 hrs; replace every 8 mos. - cats and dogs - EPA |
|
|
Scalibor collars
|
- anti-flea and tick - rx travels over dog through sebum - 2-3 wks to reach efficacy; replace every 6 mos. - dogs only - EPA |
|
|
Preventic collars
|
- anti-tick - rx travels over dog through sebum - dogs only - EPA |
|
|
Lime Sulfur
|
- antiparasitic, antibacterial, antifungal, antipruritic, keratolytic - used as a dip - always dilute to a 2% solution when using |
|
|
spot-application preventatives
|
- easy - product applied over back - nature of skin/coat can impact efficacy - can be distributed on the surface or transdermally, w/ relocation to skin - concentration on skin depends on: time from application, body site, nature of skin |
|
|
Advantage
|
- insecticide w/ IGR - fleas, lice - products for dogs and cats - 30 day efficacy, can be applied once a week - EPA - K9 Advantix has arachnicidal properties - Advantage Multi is FDA reg. |
|
|
Frontline
|
- insecticide/IGR, arachnicide - cats and dogs - monthly topical - EPA |
|
|
Revolution
|
- insecticide, arachnicide, anthelminthic - dog and cat - monthly topical - FDA |
|
|
Capstar
|
- insecticide (adulticide only) - oral - rapidly kills exisiting fleas, but does not prevent reinfestation - dogs and cats - FDA |
|
|
Comfortis
|
- insecticide - dogs and cats - monthly PO - FDA |
|
|
Nexgard
|
- insecticide, acaricide - extra-label use for Demodex, scabies... - monthly PO - dogs only - FDA |
|
|
Bravecto
|
- insecticide, acaricide - extra-label use for Demodex, scabies... - every 3 mos. - PO for dogs; topicals for cats, dogs - FDA |
|
|
macrocyclic lactones
|
- avermectins, milbemycins - active when ingested by parasites - FDA |
|

|
macules (<1cm) and patches (>1cm)
|
|

|
papules
|
|

|
nodule
|
|
|
plaques
|
|

|
wheals
|
|
|
pustules
|
|

|
vesicle/bulla
|
|
|
scales
|
|

|
comedo
|
|

|
epidermal collarette
|
|
|
ulcer
|
|

|
lichenification
|
|

|
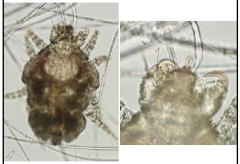
Otodectes (ear mites)
|
|

|
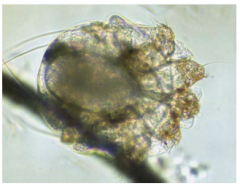
Demodex canis
|
|
|
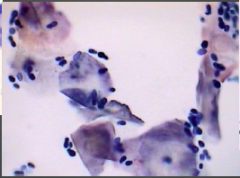
Malassezia
|
|
|
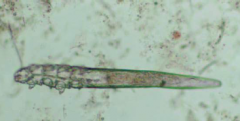
Demodex injae
|
|
|
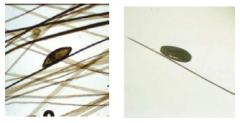
Cheyletiella
|
|
|
left: lice right: Cheyletiella |
|

|
Sarcoptes scabiei
|
|
|
Notoedres cati
|
|

|
Demodex cati
|
|

|
Demodex gatoi
|
|

|
sucking louse
|
|

|
chewing louse
|
|

|
Ctenocephalides felis felis (fleas)
|
|
|
nitenpyram
|
- insecticidal (adult fleas only)
|

