![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
1.What's the difference between a macule, papule and vesicle?
2.What do they have in common? |
1.Macule= flat, papule= elevated and solid, vesicle= circumscribed collection of fluid
2. All are under 5mm |
|
|
|
1. What's the difference between a patch, plaque and bulla?
2. How are they the same? |
1. patch= flat lesion abnormal in color only, plaque= elevated flat topped lesion, bulla= circumscribed collection of fluid
2. All greater than 5mm |
|
|
|
1. What's the difference between a nodule and a papule?
|
Nodule= below the epidermis, papule- solid elevated lesion in the epidermis
|
|
|
|
1.What's the difference between a excoriation and lichenification?
2.What's the difference between an erosion and an ulcer ? |
1.excoriation: an erosion of epidermis 2ndary to scratching lichenification= thickening of epidermis 2ndary to rubbing
2. erosion= focal loss of epidermis that doesn't enter dermis (no scarring) ulcer= focal loss of epidermis and dermis (scarring) |
|
|
A patient presents to ER with this lesion having suddenly appeared. You tell the patient that the lesion is a result of infiltration of 1. what layer of skin and that it will be resolved in 2. a) 1 week b) 1 day c) 1 month
|
This is a wheal. It is a result of inflamation of the dermis and will resolve in less than 24 hours.
|
|
|
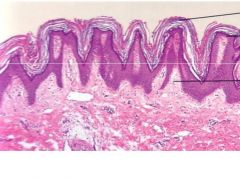
Name a disease state in which this abnormality is seen.
|
Psoriasis is a good example. This abnormality is parakeratosis and is a result of rapid turnover of the epidermis without normal maturation (that's why there are nuclei in the stratum corneum)
|
It is abnormal of nucleated cells to be present in the stratum corneum.
|
|
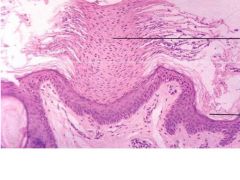
1.What is the abnormality in this section?
2.Contrast it with the appearance of a normal section. |
Hypergranulosis
Granular layer should only be 1-2 cell layers thick. |
|
|
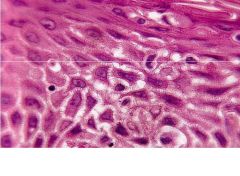
What form of epidermal hyperplasia is this? What cells have proliferated?
|
Acanthosis as a result of proliferation of the cells in the spinous layer.
N.B. acantha is Greek for thorn. |
|
|
What is this condition called? It caused by proliferation of what cell layer?
|
papillomatosis, and it is a subtype of acanthosis (proliferation of spinous layer)
|
|
|
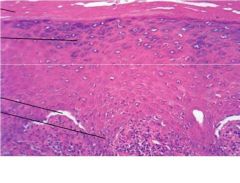
What caused this condition?
|
Edema between the spinous cells. Note the widening of the intercellular spaces
|
|
|
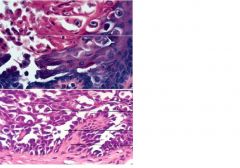
The section from your patient whom you strongly suspect has IgG antibodies to his cell-cell connection proteins got mixed up on the way to the lab. the tech has it down to these two slides.
1. Which one is it and what condition does your patient have? 2. If you could use this punch biopsy what test would you run to confirm the presence of the antibodies and why? |
1. The bottom one because it shows evidence of acantholysis. Pts. with anti-self antibodies develop pemphigus vulgaris because of loss of cell-cell cohesion in the epidermis.
2. You would run DIF on the skin biopsy because DIF tests for presence of anitgen on pts. skin, IIF would test for presence in serum. |
|
|
|
what type of eczematous dermatitishas a different presentation in children and adults and what are they?
|
atopic.
infants: face and head; acute older children/adults: scaling and lichenification of flexural areas; chronic |
|
|
|
1.What type of eczematous dermatitis is similar to a burn and requires no prior sensitization?
2. What types of skin are protected from this type of dermatitis? |
1.irritant contact dermatitis
(more exposure/ worse symptoms) 2. dry and thick (more corneum, more better, so palms of hands) |
|
|
|
What's the difference between acute spongiotic dermatitis and chronic eczematous dermatitis?
|
acute: no acanthosis, epidermal spongiosis with papillary dermal edema, intraepidermal vesicle formation, the inflammatory infiltrate has lymphocytes with some eosinophils.
chronic: HYKERKERATOSIS, ACANTHOSIS, spongiosis w/o visicles, thickening of dermal collagen |
|
|
|
What type of eczema can be treated with antihistamines and tacrolimus?
|
atopic (NB all can be treated with topical steroids)
|
|
|
|
1.What type of hypersensitivity reaxn is it if your patient has a itchy wheals that have been reappearing for three weeks after starting penicillin?
2. What is the pathogenesis of this condition? |
Type I hypersensitivity (urticaria), this is acute onset.
2. This is a vascular reaxn caused by mast cell degranulation. |
|
|
|
1. What are the LM pathological signs of urticaria?
2. What is the treatment for urticaria? |
normal epidermis, dermal edema, perivascular inflammatory cell infiltrate, ** also eosinophil hanging out in tissue is typical
2. avoid irritant, antihistamines |
|
|
|
1. describe the key features of a target lesion
2. If your patient presented with target lesions on hands and feet what syndrome would you be thinking of? 3. Of the three diseases in the Em like illness group, which are associated more with infections, and which are associated more with drugs? |
1.Central dusky purpura/vesicle
elevated edematous pale ring peripheral ring of macular erythema 2. Erythema Multiforme 3. EM-infection related SJS/TEN drug related |
|
|
|
Your patient had a HSV infection a month ago. They show up with target lesions after feeling tired for a week. They probably have ______?
2. If a patient with target lesions had been taking sulfa antibiotics for a sinus infection and NSAIDS for headache/fever like symptom, what other derm syndromes would be in your differential? |
1.EM, EM also associated with mycoplasma
2. SJS and TEN (antiepileptics and allopurinol can trigger also) |
|
|
|
Name 4 ways to differentiate Em from SJS/TEn
|
1. trigger (infectious)/drug
2. prodrome (febrile/ mild-absent) 3. aytpical or confluent lesions/ typicl target lesion 4. prominent mucosal involvement/ no mucosal involvment |
|
|
|
1.Where would you look for blister formation on histologic sections for EM or SJS/TEN?
2.In these diseases what is the cause of the blister formation? 3. T/F You would expect to see necrotic keratinocyted in SJS extending from the basal layer of the epidermis upward |
1.At the dermal/epidermal junction.
2. damage to basal cells-> vacuolization ->(blister) + inflammatory infiltrate at junction 3. True. |
|
|
|
1. T/F: EM is self limited and is treated by avoiding the trigger or treating the viral/infectious cause.
2. T/F: The role of oral steroids early in treatment of SJS/TEN is standard of care. |
1. True
2. False, controversial. IVIG is established for TEN. It is standard of care to treat as burn patient. |
|
|
|
What is the Koebner phenomenon? Name a skin condition that it's associated with.
|
appearance of lesion at the site of trauma (aka isomorphic response)
psoriasis |
|
|

1.This patient is a 14 yo male with hx of acute sore throat. After treatment with antibiotics, he had abrupt onset of these itchy papules. What's the diagnosis?
2. What test could confirm the diagnosis? |
1.Guttate psoriasis (2-5 mm red papules, also demonstrates Koebnner/ isomorphic response
2. ASO titer (antistreptolysin). Why? b/c Streptococcal inf. (pharyngitis)is typical cause. N.B. usually seen in younger individuals. |
|
|
|
What is the most common arthritic presentation of psoriasis?
|
aymmentric oligoarthritis hand joints, most commonly DIP and PIP
|
|
|
|
What is the pathologic name for nuetrophils in the stratum corneum and what skin condition is it associated with?
|
Munro's microabscesses
psoriasis |
|
|
|
What is the manifestation of epidermal thinning of the dermal papillary tips and dilated vessels in the dermal papillae?
|
Aupitz' sign.
Pinpoint bleeding when scale is forcibly removed from psoriasis plaque. |
|
|
|
1.How do you treat guttate psoriasis?
2. How do you treat conventional psoriasis? |
1.Antibiotics
2. Topical therapy: vit d, retinoids; light: PUVA, UVB; |
|
|
|
What psoriasis therapy can cause "iaotrogenic HIV" and what is its mechanism of action?
|
1. Alefacept
It targets Th cells for destruction. (it binds Cd2 on memory T Cells) |
|
|
|
What psoriasis drug inhibits t cell adhesion to endothelium and what are its side effects?
|
Efalizumab
Thrombocytopenia, rebond phenomenon in 5% |
|
|
|
1.How do is the demographics of Lichen Planus different for men and women?
2. What is the etiology of L.P.? 3. What disease is L.P. associated with? |
1.incidence in men stays the same, it increases in women until age 60.
2. Unkown, but involves helper T cells acting at basal layer. 3. Hep C. (increased incidence in Japan bc Hep C is more common in Japan) |
|
|
|
T/F The course of Lichen Planus generally follows regular, predictable stages.
T/F If you have LP with mucouse membrane involvement you are less likely to have recurrences. |
False
2/3 have it less than 1 year, 50% of people recurrences, course is unpredictable. 2. False, you are more likely to have Chronic LP with mucouse membrane involvement. |
|
|
|
1. What is the most common form of Lichen Planus?
2. What form of LP is associated with increased risk of squamous cell cancer? |
1. reticulate N.B. - these demonstrate Wickham's striae.
2. Ulcerative |
|
|
|
What is the pathologic name for nuetrophils in the stratum corneum and what skin condition is it associated with?
|
Munro's microabscesses
psoriasis |
|
|
|
What is the manifestation of epidermal thinning of the dermal papillary tips and dilated vessels in the dermal papillae?
|
Aupitz' sign.
Pinpoint bleeding when scale is forcibly removed from psoriasis plaque. |
|
|
|
1.How do you treat guttate psoriasis?
2. How do you treat conventional psoriasis? |
1.Antibiotics
2. Topical therapy: vit d, retinoids; light: PUVA, UVB; |
|
|
|
What psoriasis therapy can cause "iaotrogenic HIV" and what is its mechanism of action?
|
1. Alefacept
It targets Th cells for destruction. (it binds Cd2 on memory T Cells) |
|
|
|
What psoriasis drug inhibits t cell adhesion to endothelium and what are its side effects?
|
Efalizumab
Thrombocytopenia, rebond phenomenon in 5% |
|
|
|
What are 5 histologic feature of lichen planus?
|
1.hyperkeratosis
2.saw tooth epidermal hyperplasia 3.lymphocytes at dermal-epidermal junction 4.vacuolation at basal level 5. civatte bodies |
|
|
|
What type of immunoflourcence is more specific?
|
Direct, it uses the pts tissues.
|
|
|
|
What are two ways to test for Pemphigus Vulgaris in a physical exam?
|
Nikolsky- apply slight pressure at edge of blister and see if epidermis sloughs off
asboe-hansen- gentle pressure on intact blister pushes fluid away into adjacent skin |
|
|
|
1.What are the two antigens culpable for Pemphigus Vulgaris and what are the immunoglobins that mediate the immune response?
2.What is the result of the immune response against these antigens? |
1.Desmoglein-1 and Desmoglein-3; IgG mediated
2. Loss of intercellular adhesion: flaccid blishter |
|
|
|
1.What is the presenting sign of Pemphigus Vulgaris most of the time?
2. If fatal, what do pemphigus vulgaris pts die of? |
1.oral lesions
2. sepsis 5-10% of the time |
|
|
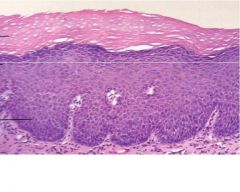
1.What findings do you note on these slides?
2. What blistering disease is it associated with? 3. What test could you run to confirm your diagnosis and what positive finding would you expect to see? |

1. intrapepidermal blister, suprabasal acantholysis, "row of tombstones"
2. pemphigus vulgaris 3. punch bipsy with DIF, "chickenwire" intercellular staining |
|
|
|
1.What are example of 1st line Pemphigus treatments?
2. What treatment is reserved for refractory cases? |
1.predinsone, azothioprine, mycophenolate mofetil, methotrexate, cyclosporine and IVIG
2. Retuximab (shuts done antibodies 2. |
|
|

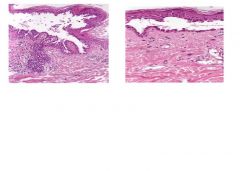
What is the etiology of this skin disease?
|
IgG antibodies to basement membrane antigens, the hemidesmosomal proteins. Causes subepidermal blistering and large tense bullae that rupture and heal spontaneously.
|
|
|
|
1.T/F: Bullous pemphigoid pts. usually present with oral mucosal involvement.
2. T/F There are no clear age associations with BP. |
1. False, the mucosa is rarely involved in BP.
2. False, 65-75 and young children are the age groups. |
|
|
|
What conclusions can you draw from high levels of circulating IgG antibasement membrane Abs in a bullous pemphigoid pt.?
|
not very many as they do not parallel disease activity.
|
|
|
|
What features are evident from path sections of B.P.?
|
1. subepidermal blistering, lack af acantholysis, perivascular inflammation with eosinophils**, nuetrophils and lymphocytes.
|
|
|
|
What features are evident on DIF taken from the edge of a skin lesion of a pt. with antibodies to his basement membrane proteins?
|
No staining in epidermis. Its a linear staining along the basement membrane.
|
|
|
|
what pathological findings are responsible for the staining of basement membrane in bullous pemphigoid?
|
IgG and C3
|
|
|
|
Which condition is more responsive to low doses of steroids, pemphigoid or vulgaris?
|
pemphigoid
|
|
|
|
What are the immunoflourescence findings of Dermatitis herpeteformis?
|
IIF negative (igA antibodies)
DIF postive for IgA in the tips of dermal papillae |
|
|
|
What is the mainstay treatment for the skin disorder that is present in people with gluten senstive enteropathies?
|
Dapsone (g6pd level must be monitored)
sulfapyradie = secondary |
|

