![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
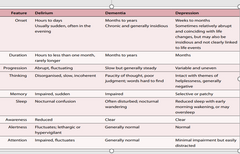
triad of diseases with overlapping symptoms |
dementia delirium depression |
|
|
delirium dementia depression |
|
|
|
dementia |
complex and progressive syndrome: a collection of signs and symptoms caused by a number of diseases dementia starts with cognitive and behavioural changes and progress to affect the person more globally |
|
|
demntia stage one vs two vs three |
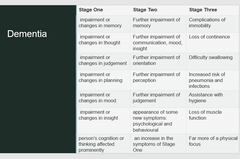
stage 1 impairment in changes in memory stage 2 further impairment of memory stage 3 complication of ommobility |
|
|
pathology of dementia |
alzheimers disease lwey body disease frontotemporal dementia vascular dementia |
|
|
alzheimers |
60-70 percent cases of dementia in older people likely to be Alzheimer's disease progressive loss of ability to form new memories loss of higher order human capabilities difficulty with orientation time and place language difficulties; expression and sometimes comprehension personality changes |
|
|
alzheimers cerebral cortex |
Alzheimer's disease tends to rob people of higher brain functions and many of these are locked in the cerebral cortex. Specific parts of the cerebral cortex become damaged, shrinks and atrophy Specifically the Frontal, Temporal and Parietal lobes |
|
|
Alzheimer's specific pathophysiology |
beta amyloid plaques happens outside nerve cells beta amyloid proteins form filaments which self combine to form the actual plaque like structures cant diagnose someone with Alzheimer's just from this one thing, will also need neurofibrillary tangle |
|
|
neurofibrillary tangle |
Occur inside the nerve cell Tau Proteins undergo abnormal changes and form tangles The neurofibrillary tangles cause the nerve cell to die because as they are insoluble they are left in the brain after the nerve cell has gone then they are called tombstone tangles |
|
|
hippocampus and alzheimer's |
within the temporal lobes Tangles form in the hippocampus first Hippocampus has a role in processing sensory info for memories so the tangles disrupt this process this is why they cant make new memories |
|
|
Summary Alzheimer's disease |
Amyloid plaques and neurofibrillary tangles are key pathological changes in Alzheimer's There are variations in genes that are linked to relative risk of dementia The hippocampus and memory formation are affected very early on Alzheimer's disease starts in the brain many years before symptoms are expressed. This is known as the 'preclinical' phase of the disease |
|
|
FTD - behavioral Variant |
FTD - behavioural Variant personality and behavioural changes impaired planning and judgement apathy loss of empathy disinhibition diet |
|
|
FTF - speech variant |
primary progressive aphasia (inablity to comprehend language) inability to understand speech inability to produce speech |
|
|
Frontotemporal dementia |
often thought of as an early onset of dementia |
|
|
Frontal temporal dementia pathophysiology |
Protein Tau and TDP-43 cause clumps or aggregates Where: inside the cell , axon, oligodendrocytes |
|
|
TDP-43 PROTEIN |
is aggregated in some cases of frontotemporal dementia plays a role in motor neuron disease 15% of people who have motor neuron disease may go on to develop frontotemporal dementia VIA VERSA |
|
|
Frontotemporal dementia summary |
Characterized: atrophy of frontal cortex and front parts of temporal cortex There are several disease that cause frontotemporal dementia Two forms of frontotemporal dementia - BEHAVIOURAL and SPEECH Two key proteins: Tau and TDP-43 which abnormally accumulate in neural cells Strong genetic predisposition Frontotemporal dementia and motor neuron disease are related and one may cause the other |
|
|
Lewy body disease vs Alzheimer's |
different to alzheimers because cognitive changes from degeneration in cortex FLUCTUATE. good or bad days |
|
|
Lewy body disease changes |
visual.spatial awareness sleep disorder Parkinson's type features |
|
|
Lewy body protein does what |
lewy body proteins form spherical structures within neurons Main protein present in Lewy Body is ALPHA-SYNUCLEIN Form in the substantia nigra |
|
|
Summary of Lewy Body disease |
aka know as lewy body dementia or dementia with lewy bodies characterised by: prescence of spherical bodies in the nerve cells in the cortex call 'lewy bodies' Main protein is ALPHA-SYNUCLEIN Features of disease include: sleep/wake, visual/spatial, parkinsons type features |
|
|
Vascular dementia symptoms |
step-wise pattern of degeneration problems in gait and executive functions problems in mood/behaviour small vessel disease |
|
|
Therapeutic goals |
symptom management disease modification neuroprotection |
|
|
risk factors dementia non modifiable |
older age inheritance of genes |
|
|
risk factors dementia potentially modifiable |
smoking high cholesterol obesity type 2 diabetes hypertension sedentary lifestyle |
|
|
increase quality of life by |
early diagnosis 5 years from diagnosis to death The earlier diagnosis, more time for medical trials to delay symptom onset time to talked to family about values and what to do before loss of ability to do so |
|
|
Four strategies dementia prevention |
keeping mind active keeping body active acessing apropriate suport managing health conditions and nutrition |
|
|
Medical management of dementia |
medications careful considerations protection of brain treating symptoms caused by dementia providing comfort end of life can have unwanted side effect can make dementia worse |
|
|
Medications for dementia |
Cholinesterase inhibitors symptoms control meds avoid meds that make worse eg: opiate anagesia, anti cholinergics |
|
|
non pharmacological therapy |
cognitive and physical activity interventions music reminiscence aroma massage assistive technology |
|
|
BPSD what |
behavioral psychological symptoms of dementia |
|
|
BDSP is caused by |
untreated pain |
|
|
BDSP ss |
calling out agitation restlessness |

