![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
98 Cards in this Set
- Front
- Back
|
What is the triad for normal pressure hydrocephalus?
|
wacky, wobbly, wet
dementia, magnetic gait, urinary incontinence |
|
|
What is the etiology of normal pressure hydrocephalus?
|
impaired CSF absorption for secondary cases (half of cases secondary to previous SAH or meningitis)
chronic periventricular ischemia leading to increased ventricular compliance vs. arachnoid fibrosis in idiopathic cases |
|
|
What is modified Evan's ratio?
|
Evan's ratio is used to determine ventriculomegaly on CT. The numerator is the maximal diameter of the frontal horn of the lateral ventricle, the denominator is the maximal width of the skull at this level
|
|
|
What are some clinical symptoms associated with normal pressure hydrocephalus
|
Besides wacky-wobbly-wet;
long tract signs leading to hyperreflexia, positive babinski response, spasticity or gegenhalten; urinary urgency rather than incontinence; memory loss is specfically subcortical: impaired attention, fluency, executive function |
|
|
What is the rate of shunt complication after placement for NPH?
|
38% complication rate
22% re-surgerized 6% permenant neuro sequelae or death |
|
|
What is the Fisher test in relation to NPH?
|
document gait and memory prior to a large volume 30 to 50 ml CSF tap and then document improvement afterwards. 90-100% positive predictive value if any of those measures improve for improvement with shunt placement
|
|
|
What are some good prognostic factors for improvement with shunt placement for NPH?
|
1) short duration of disease
2) gait as prominent manifestation and early in disease process 3) etiology of secondary NPH tends to improve more than idiopathic NPH |
|
|
What is semantic memory and where is it stored?
|
Memory for facts such as vocabulary and concepts
Stored in lateral temporal cortex (non-mesial) neocortex |
|
|
What is episodic memory?
|
Memory associated with specific events and contexts (usually impaired first in alzheimer's). Stored in medial temporal lobe or hippocampus.
|
|
|
What is declarative memory and where is it stored?
|
Memory for facts, stored in mesial temporal cortex
|
|
|
Distinguish immediate memory, recent memory and remote memory by location of involvement
|
Immediate memory- processed in the prefrontal cortex "working memory"
Recent memory: enterorhinal cortex and mesial temporal structures and hippocampus (impaired most in AD) Remote memory: not involved with hippocampus |
|
|
What is the conversion rate of amnestic MCI to alzheimer's?
|
10-15% per year
|
|
|
What parameters are tested by the clock-drawing test (3)
|
1. semantic memory
2. executive function 3. visuospatial |
|
|
What are the clinical manifestations of posterior cortical atrophy?
|
Generally, present to an eye dr. initially, c/o difficulty with visual. They often present with 1) simultanagnosia 2)optic ataxia 3) ocular apraxia, later visual agnosia, ideomotor/contstructional/dressing apraxia, prosopagnosia (less likely visual hallucinations and visual field deficits)
Recent memory impaired but no prominent complain |
|
|
What is the pathology of posterior cortical atrophy?
|
similar to Alzheimer's with a primarily posterior cortex manifestation, some can be similar to lewy body
|
|
|
Why does posterior cortical atrophy affect the visual system, what does it affect?
|
dorsolateral- "Where" stream of visual processing
|
|
|
What are some AD subtypes (not classic presentation) but found to have AD pathology post-mortem?
|
1. posterior cortical atrophy
2. primary progressive aphasia (usually FTD subtype) 3. biparietal syndrome (prominent visuospatial and apraxia abnormalities) |
|
|
What are the NINCDS-ADRDA criteria for Alzheimer's Disease (5)
|
1. memory impairment confirmed by neuropsych testing
2. age b/t 40 and 90 3. no impaired consciousness 4. progressive cognitive impairment 5. not thought secondary to any other neurologic disease |
|
|
What are the DSM IV criteria for dementia?
|
1. memory impairment
2. impairment in more than 1 cognitive domain: aphasia, agnosia, apraxia, executive function 3. impaired social or work functioning 4. not secondary to delirium, reversible or any other metabolic etiology 5. gradual onset and progressive decline |
|
|
What are 3 genetic mutations that can lead to autosomal dominant Alzheimer's disease?
|
1. amyloid precursor protein
2. presenilin-1 3. presenilin-2 |
|
|
What is the most clearcut genetic risk factor for AD?
|
apo E4 allele
|
|
|
Where does digit span or simple rehearsal of items localize?
|
inferior prefrontal cortex Bradley p. 861
|
|
|
Where does more complex attention task, manipulating such as digits backwards localize?
|
dorsolateral prefrontal cortex
|
|
|
Where does episodic memory localize?
|
neocortex especially the hippocampus
|
|
|
Give some examples of episodic memory
|
memories of a personal experience, delayed recall, do not or cannot reverse the items, orientation to date, location, current events
|
|
|
What is Ribot's law?
|
retrograde amnesia of medial temporal pathology follows a temporal gradient where recent memory is more impaired than distant
|
|
|
What is semantic memory?
|
Our knowledge of facts about the world, also affected by Alzheimer's disease; ex. would be categorical fluency
|
|
|
What is the Heidenhain variant of CJD?
|
visual variant, affects visual processes in Alzheimer's first
|
|
|
What is tau and what is its role in alzheimer's disease?
|
The center of the neurofibrilllary tangles is a cytoskeletal protein called tau which has 6 isoforms (different isoforms may lead to different disease) misfolding leads to accumulation and disease
|
|
|
What is the role of APOE4 in Alzheimer's Disease?
|
2 to 4 fold risk factor for heterozygotes, even more for homozygotes up to 8 fold leading to sporadic and familial disease, most well defined risk factor for AD, not used in clinical practice only increases the PPV of AD clinical diagnosis from 90 to 94% when using pathology as gold standard
|
|
|
Role of Vitamin E in AD?
|
Vitamin E 1000 IU BID has been shown to decrease rate of conversion from mod. to severe dementia as well as decrease time to nursing home placement
|
|
|
What is the mech of action memantine in AD?
|
NMDA receptor antagonist, because glutamate excitotoxicity thought to play a role, FDA approved for mod. to severe AD 5-15
|
|
|
What are the main SE of achE inh and when do they occur, how to avoid?
|
occur during escalation, go slowly, take after meals
|
|
|
What did the WHIMS womens helath initiative memory study show about estrogens and AD?
|
no effect, may even lead to increased dementia
|
|
|
What does the consortium to Establish a Registry for Alzheimer's disease criteria measure?
|
NFT and NP in relation to age
|
|
|
What are Hirano bodies?
|
They are eosinophilic inclusions found in the pyramidal cells of the hippocampus
|
|
|
How often does major depressive disorder by DSM-IV criteria co-exist with Alzheimer's?
|
15-20%
|
|
|
How many AD patients c/o at least one depressive symptom?
|
2/3
|
|
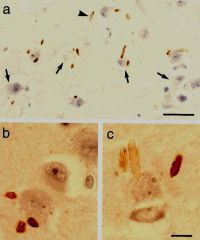
What are hirano bodies
|
Eosinophilic cytoplasmic inclusions found in the PYRAMIDAL CELLS of the hippocampus assoc. with Alzheimer's disease
|
|
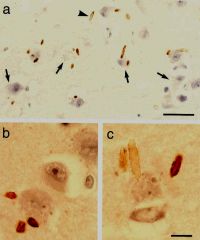
What are hirano bodies?
|
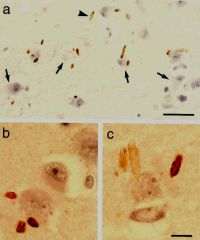
Eosinophilic cytoplasmic inclusions found in PYRAMIDAL CELLS of hippocampus, assoc. with alzheimer's disease
|
|
|
What is Ganser syndrome?
|
forensic personality, approximate answers, the answer is wrong but in its nature reveals that the pt. understands the question. For example what seaon is it? Spring rather than summer; hallucinations, clouding of consciousness, memory or personal identity loss
|
|
|
What is Geschwind's syndrome
|
circumstantiality, excessive verbal output, hypergraphia (harvard), altered sexuality, intensifed mental life (deepening of many emotions resulting in religious or philosphical preoccuation; a strong moralistic sense)
|
|
|
What features are characteristics of Kluver Bucy syndrome?
|
hyperdocility, placidity, hypersexuality, hyperorality, hypermetamorphosia (attends to visual stimuli)
|
|
|
When should an LP be performed for sx of dementia? (3)
|
short duration <6 months
atypical features rapid progression |
|
|
Describe the progression of language disturbance in Alzheimer's?
|
1. word-finding
2. impaired comprehension intact repetition 3. impaired comprehension & repetition expressive speech problems |
|
|
what chromosome has the gene for presenilin 1?
|
chromosome 14
|
|
|
what chromosome has the gene for presenilin 2?
|
chromosome 1
|
|
|
what neuropathologic changes correlate best with the severity of dementia due to AD?
|
neurofibrillary tangles correlate best with the severity of dementia
|
|
|
What are the clinical features of progressive supranuclear palsy?
|
supranuclear gaze palsy
axial musculature dystonia dysarthria pseudobulbar palsy |
|
|
What are the clinical characteristics of dementia with Lewy Bodies? (5)
|
1. fluctuating confusion and dementia
2. vivid visual hallucinations 3. extrapyramidal features 4. neuroleptic sensitivity 5. rem sleep disorder |
|
|
What are clinical features of corticobasal degeneration?
|
alien limb phenomenon
tremor rigidity grasp reflex apraxia myoclonus usually they get dementia with time |
|
|
What are some difference between subcortical dementia and cortical dementia?
|
In subcortical dementia, short-term spontaneous recall may enhance with encoding and recognition cuing. Procedural memory better preserved in cortical dementias. May not follow Ribot's law like in cortical dementias. Recognition memory preserved in subcortical dementia
|
|
|
What is Ribot's law?
|
in cortical amneisa, there is a temporally graded retrograde amnesia, recent memories are lost first
|
|
|
Where is working memory stored and how many bits of information can it usually hold?
|
dorsolateral prefrontal cortex (neurology secrets), 7-10 bits of information, the phonological loop; inferior prefrontal cortex (Bradley)
|
|
|
What is doppelganger syndrome?
|
the patient sees himself as his own double
|
|
|
What is Fregoli's syndrome?
|
Patients believes that familiar person has taken on the appearance of another person to persecute them
|
|
|
Intermetamorphosis
|
patients belive that they have switched identities with another individual or believe that other people or objects have changed physically and psychologically into someone else
|
|
|
what is aphemia?
|
poor speech output with sparing of comprehension and writing; localized in the motor strip
|
|
|
Where does expressive aprosody localize?
|
the R hemisphere in the equivalent region to the broca's area (frontal operculum)
|
|
|
Where is receptive aprosody?
|
r hemisphere equivalent to wernicke's
|
|
|
What is ideational apraxia, where does it localize?
|
inability to perform a sequence of learned acts such as making coffee, diffuse brain injury or with frontal lobe lesions impaired attn and exec fxn
|
|
|
What is ideomotor apraxia and where does it localize?
|
inability to perform learned familiar movements to command, dominant inferior parietal area and or arcuate fasciculus, contains praxicons,
|
|
|
What is sympathetic apraxia and where does it localize?
|
A patient may have a L MCA stroke, and R hemiparesis, but difficulty using the L hand ideomotor apraxia because the praxicons in the L inferior parietal lobe does not send the information to the R premotor cortex
|
|
|
What is limb-kinetic apraxia and where does it localize?
|
loss of dexterity of fine distal limb movements, contralateral supplementary motor cortex
|
|
|
what is topographagnosia and where is the lesion?
|
inability to navigate complex spatial layouts like a building or even home, or describe with a map how to get there, localizes in the parahippocampal place area
|
|
|
Where is the lesion for prosopagnosia?
|
inability to recognize familiar faces, usually bilateral inferior occipito-temporal lesions affecting fusiform gyri which contains an area called the fusiform face area
|
|
|
What is achromatopsia and where does it localize?
|
acquired lack of color vision, localizes to occipital cortex below calcarine sulcus
|
|
|
What is verbal dysdecorum and where does it localize?
|
disinhibited, poorly monitored verbal output that is socially unacceptable and seen most freq. following right frontal convexity
|
|
|
What is primary progressive aphasia?
|
a progressive disorder of expressive language, effortful speech production, phonologic and grammatical errors and word retrieval difficulty, clinically similar to people with Broca's aphasia, onset not as abrupt, 20% assoc with tauopathies, 60% lack histology, 20% due to AD
|
|
|
What is semantic dementia?
|
similar to wernicke's aphasia, a progressive disorder of severe naming and word comprehension impairment
|
|
|
Where does aphemia localize?
|
lower motor strip
|
|
|
Where does transcortical motor aphasia localize?
|
supplementary motor area
|
|
|
What percentage of MS patients develop cognitive dysfunction at some point?
|
60%
|
|
|
What are the Petersen diagnostic criteria for amnestic MCI (4)?
|
1. memory impairment corroborated by informant
2. obj. memory impairment for age 3. not demented 4. not impaired ADLs |
|
|
What is the mechanism of pathology in CADASIL?
|
NOTCH3 gene product on chromosome 19 acts as a transmembrane receptor specifically in vascular smooth muscle cells. In CADASIL eosinophilic proteins deposit in the media of the vascular wall leading to angiopathy
|
|
|
What is the usual age of onset and clinical symptoms in CADASIL?
|
40s, migraine-type headaches, seizures, depression and stroke like symptoms
|
|
|
What is the characteristic imaging feature in CADASIL?
|
anterior temporal lobe hyperintensities as well as lacunar infarctions, white matter disease
|
|
|
How do you diagnose cerebral amyloid angiopathy?
|
definite is via full post-mortem examination, probable with pathology is possible, probable clinical diagnosis would show multiple hemorrages restricted to lobar, cortical or cortico-subcortical regions, age > 55 years
|
|
|
What are the characteristics of Sneddon's syndorome?
|
multiple cerebral infarcts, livedo reticularis, hypertension, mitral valve pathology and seizures
|
|
|
What symptoms are characteristic of HIV deentia?
|
overt neuro symptoms: generalized hyperreflexia, abnormal extraocular movements, increased tone, clonus, tremors, ataxia, psychomotor slowing
|
|
|
What are the characteristics of Herpes infection related dementia?
|
Occurs in some patients after the acute viral infection, memory/language impairment, limbic features secondary to location of medial temporal encephalitis
|
|
|
What is the causative organism for Whipple's disease?
|
gram- negative actinomycete Tropheryma whippelii, rare, men 30-50; skin hyperpigmentaiton
|
|
|
Where is the prion protein gene located associated with familial (10-15% of all) CJD?
|
Chromsome 20
|
|
|
What are the clinical symptoms associated with CJD?
|
starte myoclonus, ataxia, progressive dementia
|
|
|
Where does alcoholic dementia tend to affect the CNS?
|
in the mamillary bodies and dorsomedial thalamic nuclei
|
|
|
What clinical correlates are asosciated with the cognitive deficits and severity of disease in MS?
|
corpus collosal atrophy, number and size of WML
|
|
|
How to make the diagnosis of metachromatic leukodystrophy?
|
arylsulfatase-A in leukocytes and skin
|
|
|
What are the clinical manifestations of Wilson's disease?
|
20s to 30s
neuropsych sx, cognitive abnl wing beating tremor, ataxia, facial dystonia (sardonic smile), abnormality in copper metabolism with autosmal recessive inheritance, low ceruloplasmia, elevated copper excretion |
|
|
What is the genetics behind Wilsons?
|
autosomal recessive
Chr. 13 ATP7B gene |
|
|
What are the clinical characteristics of HallevordenSpatz or neurodegneration with brian iron accumulation?
|
demntia, parkinsonism, speech abnormality. All have the eye of the tiger sign central hyperintensity surrounded by hypointensity in GP on MRI
|
|
|
What are the genetics of Hallervorden-Spatz disease?
|
mmutation in gene encoding pantothenate kinase 2 on chromsome 20p13
|
|
|
What is the syndrome of idopathic basal ganglia calcifiation called?
|
Fahr's disease
|
|
|
What are the clinical characteristics of Fahr's diseae?
|
dementia and parkinsonism with extensive calcifcation of the basal ganglia and subcortical structures
|
|

What is the characteristic MR imaging in CADASIL
|

temporal lobe hyperintensity
|
|
|
What is the sensitivity and specificity of anterior temporal pole hyperintensity in CADASIL?
|
90% sensitive 100% specific
Yamamato, Yumi. Neuropathologic correlates of temporal pole hyperintensities in CADASIL |
|

What is the characteristic slit lamp finding in patients with Wilson's disease?
|
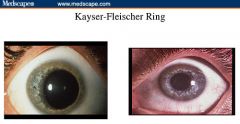
Kayser Fleischer Rings
Copper deposition in Descemet membrane |
|
|
What is Capgras syndrome?
|
It is the feeling that a familhy member is replaced by an unfamiliar impostor.
|
|
|
What is the etiology of Capgras syndrome?
|
Etiology of Capgras syndrome is thought to be a disconnection of the inferior frontal lobe (face recognition) and amygdala
|

