![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
82 Cards in this Set
- Front
- Back
|
What is the treatment of a traumatic pseudoaneurysm
|
coil or gelfoam
|
|
|
Can a traumatic AVF be coiled sometimes
|
yes, this may be coiled sometimes
|
|
|
What is the general cutoff where long segment stenosis will not do well with percutaneous therapy
|
> 10 cm, do not do well with percutaneous intervention
|
|
|
What is the treatment for long segment stenosis
|
if greater than 10cm then surgery
|
|
|
What is the treatment for stenosis less than 10 and greater than 3 cm
|
For obstructions < 10 cm but > 3 cm, not involving SFA origin or distal popliteal, can thrombolyse and then balloon
|
|
|
What is done is the stenosis is less than 3cm
|
For < 3 cm, can balloon angioplasty alone
|
|
|
What is the ddx of no flow to the renal artery
|
embolus (usually from heart), thrombus superimposed on stenosis, dissection, traumatic injury or avulsion, iatrogenic
|
|
|
How long can the kidney tolerate total ischemia before it becomes non-viable
|
Kidney can tolerate total ischemia for 90 min before it becomes nonviable
|
|
|
When is embolectomy performed on a renal emboli
|
There is increased morbidity with embolectomy of the kidney therefore conservative management is preferred unless there is bilateral emboli or emboli of a solitary kidney
|
|
|
What is the conservative treatment for emboli of the kidney
|
percutaneous catheter-directed thrombolysis (< 3 h), anticoagulation,
|
|
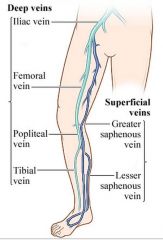
Superficial lower extremity veins
|
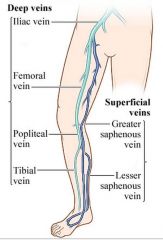
Deep lower extremity veins
|
|

superficial
|

deep
|
|
|
What is the location of the greater saphaneous vein
|

The greater saphenous vein continues along the medial aspect of the thigh and drains into the common femoral vein (CFV) at the saphenofemoral junction (SFJ).
|
|
|
What is the MCC of AVF in the lower extremities
|
usually traumatic
|
|
|
If there is a traumatic AVF can it be coiled
|
yes, can occasionally be coiled if there is a long fistula
|
|
|
When do you drain a pancreatic pseudocyst
|
drain if symptomatic
infected greater than 4-5cm |
|
|
What is the technique for drainage of a pancreatic pseudocyst
|
Most can be drained via transabdominal or retroperitoneal approach but
can also drain transgastric and transhepatic |
|
|
What are the complications of pancreatic pseudocyst
|
bleeding, infection, pneumothorax, empyema
|
|
|
Last slide was complication of treatment
|
yes
|
|
|
Is it possible to get a pancreatic fistula with a pseudocyst
|
yes, if there is continued drainage despite
|
|
|
What is the treatment of a pancreatic pseudocyst fistula
|
Can give octreotide 100 ug SC TID
|
|
|
What is the technique for drainage of a pancreatic pseudocyst
|
Seldinger technique with US or CT guidance
18G Chiba needle into collection, 0.038 wire Check wire placement with US or CT Progressively dilate tract 10 Fr catheter inserted over guidewire, form pigtail Drain as much fluid as possible by aspiration Attach 3-way stopcock and irrigate with saline until fluid is clear Attach to drainage bag or suction |
|
|
Do you leave the catheter in for drainage of a pseudocyst
|
yes, and leave suction on
|
|
|
Do you irrigate with the pseudocyst with saline
|
yes
|
|
|
When do you remove the pseudocyst catheter
|
Catheter removal
Improvement in clinical symptoms (afebrile) Decreasing or normal WBC count Drainage from catheter < 10 mL or stopped |
|
|
If there is persistance of drainage from a pseudocyst after 4 wks what should be suspected
|
Persistence despite drainage for > 4 w = persistent pancreatic fistula
|
|
|
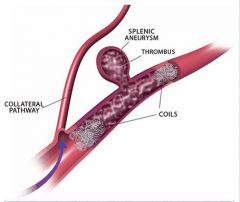
What is the ddx of a splenic artery aneurysm
3 |
pancreatitis
infection atherosclerosis |
|
|
When is a splenic artery aneurysm at higher risk of rupture
|
Frequency of rupture is increased with liver transplantation, portal hypertension, and pregnancy
|
|
|
What is the mortality of rupture of a splenic artery aneurysm
|
Rupture carries mortality risk between 20% and 36%
|
|
|
What is the treatment of a splenic artery aneurysm
|
Embolization is the primary approach to treatment. Embolization and/or stent-graft placement may be used also to exclude splenic artery aneurysms from the normal vessel lumen and thereby prevent aneurysm rupture.
|
|
|
How is embolism of a splenic artery aneursym accomplished
|
Packing of the aneurysmal sac with embolic agents (most commonly with coils, but also with detachable balloons and inert particles) and exclusion of the aneurysmal neck with the “sandwich” method are the recommended techniques for treating splenic artery aneurysms
|
|
|
What is the sandwhich technique of embolizing a splenic artery aneurysm
|
coil the aneurysm first and then proximal and distal with in the splenic artery
|
|

|
|
|

interlobar arteries
|
interlobary arteries
|
|
|
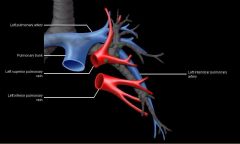
If there are chronic PEs what is the typical measurement of main PA pressure
|
35-60mmhg (nl is 9-18)
|
|

Classification for leg ischemia
|
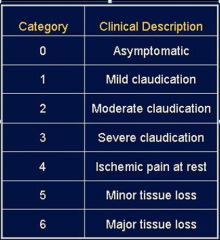
Classification for leg ischemia
|
|
|
What is a normal ABI
|
greater than 0.9 is normal
|
|
|
What is the treatment for an ABI less than 0.9 and asymptomatic
|
smoking cessation, exercise, HbA1c < 7, statin, antihypertensive (thiazide, ACEI), antiplatelet (ASA, Plavix)
|
|
|
What is the treatment for an ABI of 0.5-0.8 with symptoms
|
Claudication (ABI 0.5-0.8) medical tx + Pletal (cilostazol) + walking regimen
1-3% require amputation over 5 y period |
|
|
What is the treatment of rest pain, non-healing ulcer, gangrene and ABI less than 0.4
|
revascularization (endovascular, surgical bypass) > 70% limb salvage
|
|
|
What is the prognosis of severe stenosis of lower extremity vessels
|
Without tx, 20% dead, 35% amputated, 45% alive w/o amputation in 1 y
|
|
|
When is PTA for leg ischemia indicated
|
Flow limiting, short, single or multiple stenoses
|
|
|
What are the contraindications of PTA for leg ischemia
|
diffuse disease, long occlusions, severe arterial calcification
|
|
|
Is it possible to PTA infrapopiteal arteries
|
yes, PTA of infrapopliteal arteries made feasible by low profile balloon catheters delivered through 4 or 5 Fr sheath and thin steerable guidewires
|
|
|
What is the approach of PTA of a ischemic vessel of the leg
|
Antegrade puncture of ipsilateral CFA
|
|
|
Is anticoagulation used in conjunction with tibial artery PTA
|
yes, Anticoagulation important for reducing risk of thrombus in tibial vessels
Aspirin prior to angioplasty Heparin during the procedure Vasodilators (NTG) extremely helpful in preventing arterial spasm |
|
|
What are the potenital complications of PTA of the tibial arteries
|
Complications: thrombosis, distal embolization, intimal dissection
|
|
|
What is the treatment of bilateral common iliac artery stenosis
|
simultaneous “kissing” angioplasty + stent placement
|
|
|
Do common iliac stenosis do well with percutaneous therapy
|
yes, 1 y and 3 y patencies of 90% and 85% for stents and 80% and 70% for PTA alone
|
|
|
What is the MC congenital cause of pulmonary AVMs
|
Osler-Weber-Rendu (hereditary hemorrhagic telangiectasia)
|
|
|
What are the findings of osler weber rendu
|
Autosomal dominant w/incomplete penetrance
Telangiectasias of nasal mucosa ( epistaxis), mouth, GI tract, brain, lung Multiorgan AVMs |
|
|
Do most pulmonary AVMs of osler weber rendu have a single feeding artery
|
90% have a single feeding artery and draining vein (simple), other 10% complex w/multiple feeders
|
|
|
What is a feared complication of pulmonary AVMs
2 |
R to L shunt w/possible stroke, brain abscess
|
|
|
What are 3 clinical signs of pulmonary AVMs
|
Dyspnea, fatigue, hemoptysis (rare)
|
|
|
What are the plain film findings of a patient with AVMs
|
Nodule or multiple nodules with tubular structures leading to them (vessels)
|
|
|
What are the angiographic findings in a patient with AVMs
|
One or more dilated arteries feeding an aneurysmal dilated sac, rapid venous outflow
|
|
|
What are the indications of treating a pulmonary AVM
|
Indications: arterial feeder ≥ 3 mm, symptomatic
|
|
|
Is embolization successful in treatment of pulmonary AVMs
|
yes, Embolization successful long term in > 90%
|
|
|
What is the procedure for treateing pulmonary AVMs
|
Coils placed proximal to nidus, should be 1-2 mm larger than artery being embolized
|
|
|
What screening of the brain should occur in pt with known or suspected osler weber rendu
|
Brain AVM: MR, once in childhood, once as an adult (brain AVMs thought to be congenital)
|
|
|
What screening of the lungs should occur in pt with known or suspected osler weber rendu
|
Pulmonary AVM
In childhood, O2 saturation every 1-2 y Contrast (bubble) echocardiogram in adults If positive, chest CT |
|
|
What screening of the liver should occur in pt with known or suspected osler weber rendu
|
Doppler US
|
|
|
If a pt has osler weber rendu and has AVM in the liver when are they treated (what is the treatment)
|
Only treated if signs of liver or heart failure, severe portal HTN liver transplantation
|
|
|
Can the AVMs of osler weber rendu within the liver be treated with embolization
|
no, embolization (severe complications: parenchymal, biliary necrosis sepsis)
|
|
|
What are the 2 major causes of dissections of the vessels of the lower extremities
|
Dissections in lower extremities most often from either extension of aortic dissection or iatrogenic/catheter-related
|
|
|
What is the pathophysiology of a dissection
|
Dissection = separation b/w intima and media or within the media
|
|
|
What are 2 potential major complications of dissections
|
ischemia and rupture
|
|
|
What is the treatment of a dissection
|
stent
|
|
|
|
|

|

|
|
|
What is a consideration when analyzing a horseshoe kidney
|
Usually supplied by 3 or more arteries arising from the aorta, iliac arteries, or both
|
|
|
What are the blood supplies to an adrenal tumors
|
Usually 3 blood supplies to adrenal
Superior adrenal artery from inferior phrenic artery Middle adrenal artery from suprarenal aorta Inferior adrenal artery from proximal renal artery |
|
|
What is the ddx of malignant tumors of the adrenal gland
|
adrenal cortical tumor
pheo mets |
|
|
What is a consideration when treating a patient a pheochromocytoma
|
For pheochromocytoma, pretreat for 3 d prior to angio w/phenoxybenzamine and use phentolamine as needed during procedure to avoid a hypertensive crisis
|
|
|
What percent of pheochromocytoma are in the adrenal medulla
|
90%
|
|
|
What syndromes is pheochromocytoma associated with
|
men 2a and 2b
|
|
|
What is an important consideration when obtaining angiographic images of a pheochromocytooma
|
The angio is usually delayed until hypertension is controlled by a combination of α-blockers and β-blockers (usually phenoxybenzamine and propanalol
. β-Blockers should not be used until adequate α-blockade has been achieved |
|
|
Alpha 1
|
vasoconstricts
|
|
|
Beta 1
|
increase heart rate
|
|
|
Beta 2
|
dilates
|
|
|
Alpha vasonstricts blood vessels and beta 2 will dilate so you stop alpha first because you dont want unopposed alpha if beta 2 is blocked first
|
yes
|
|
|
Do aortocaval fistulas commonly occur
|
no, rare (4% of ruptured AAA) other causes are trauma, and iatrogenic.
|

