![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
136 Cards in this Set
- Front
- Back
|
Explain the difference between concentric versus eccentric hypertrophy of the heart.
|
Concentric is due to an increased afterload. Eccentric is due to volume-overload (preload problem).
|
|
|
Holosystolic high pitched blowing murmur, loudest at the apex during systole. What heart murmur is this?
|
Mitral regurgitation.
|
|
|
Diamond shaped systolic ejection murmur following an ejection click. What heart murmur is this?
Where does it radiate? |
Aortic stenosis. Radiates to carotids.
|
|
|
When does S3 and S4 heart sounds occur?
|
S3 occurs in early diastole. S4 (decreased compliance) occurs in late diastole (atrial systole).
|
|
|
Will there be left ventricular hypertrophy in mitral stenosis?
|
No. No volume overload.
|
|
|
What does mitral stenosis murmur sound like?
|
Opening snap in early diastole followed by a rumbling murmur.
|
|
|
What does an aortic regurgitation murmur sound like?
|
High pitched blowing diastolic murmur. S3 and S4 would be present because LV overload. Increased intensity on expiration.
|
|
|
What valve leaflet is hit by the dripping of blood from aortic regurgitation? Whats the murmur that is heard?
|
Anterior leaflet of the mitral valve. Austin-Flint murmur.
|
|
|
What is the most common cause of tricuspid stenosis? How do you differ tricuspid stenosis from mitral stenosis?
|
Infective endocarditis. Tricuspid stenosis is louder with inspiration.
|
|
|
What is the average weight of the heart? What is the average wall thickness of the left ventricle? Right ventricle?
|
Average weight = 250-300g in females, 300-350g in males
Thickness: RV = 0.3-0.5, LV = 1.3-1.5 |
|
|
What does azotemia indicate?
|
If perfusion deficit of the kidney becomes sufficiently severe, impaired excretion of nitrogenous products may cause azotemia. LHF can cause this.
|
|
|
What is anasarca?
|
Generalized massive edema.
|
|
|
What type of heart failure causes pulmonary edema?
|
Left sided heart failure.
|
|
|
What can be seen histiologically in the lungs of a person with chronic left heart failure?
|
Heart failure cells: alveolar macrophages engulfing RBC's and breaking them down into hemosiderin.
|
|
|
What is the main symptom of left heart failure?
|
Dyspnea.
|
|
|
Hydrostatic pressures increase where in right heart failure? Consequences?
|
Backward failure: venous system. Neck vein distension, hepatomegaly (nutmeg liver), pitting edema. Possibly ascites.
|
|
|
Paroxysmal nocturnal dyspnea. Right or left heart failure?
|
Left heart failure. aka Pillow orthopnea, sleeping upright decreases VR and decreases pulmonary congestion.
|
|
|
What type of heart failure does endotoxic shock cause?
|
High-output failure by mass vasodilation. Increase stroke volume (hyperthyroidism), decrease blood viscosity (severe anemia), and arteriovenous fistulas (Paget's disease) can also cause high-output heart failure.
|
|
|
How does estrogen protect against coronary artery disease?
|
Increases HDL.
|
|
|
How does cholestyramine protect against coronary artery disease?
|
Decreases LDL by decreasing bile acid reuptake. Body must make new bile from cholesterol.
|
|
|
What are the four types of ischemic heart disease?
|
Angina pectoris, sudden cardiac death syndrome, myocardial infarction, chronic ischemic heart disease?
|
|
|
What is sudden cardiac death syndrome? Cause of death?
|
Patient dead within one hour of onset of symptoms. Autopsy reveals no thrombus, but severe coronary artery disease (atherosclerosis). Cause of death is VT.
|
|
|
What is chronic ischemic heart disease?
|
Progressive onset of CHF due to small infarcts. Ejection fraction falls too low.
|
|
|
How do you determine if a patient with stable angina is a candidate for an angiogram?
|
If they have ST depression of > 1.5 on exertion.
|
|
|
What is the common cause/onset of Prinzmetal's variant angina? Male or female more common?
|
Prinzmetal angina is secondary to coronary artery spasm. W > M.
|
|
|
What does ST depression indicate?
|
Subendocardial ischemia.
|
|
|
What does the ST segment look like in Prinzmetal angina?
|
ST elevation.Vasospams effects the full thickness of endocardium causing transmural (full thickness) ischemia.
|
|
|
A patient who use to get pain on exertion now gets chest pain at rest. What do they have?
|
Unstable angina.
|
|
|
What is the most common manifestation of coronary artery disease?
|
Angina pectoris
|
|
|
What vessels can be used in coronary artery bypass graft?
|
Internal mammary artery graft (10 years) or saphenous veins (10 years). Saphenous veins undergo arterialization of the vessels, fibrosis, and occlusion common after 10 years.
|
|
|
What are the treatments for coronary artery diseases?
|
Angina pectoris stable and Prinzmetal: nitroglycerin, Ca-channel blockers.
Angina pectoris unstable: percutaneous transluminal coronary agnioplasty (PTCA), stenting, coronary bypass graft MI: same as unstable angina plus thrombolysis |
|
|
What is the difference between a myocardial infarction and angina pectoris?
|
Angina is myocardial ischemia without cellular necrosis (no infarction).
|
|
|
What is reperfusion injury?
|
Restored blood flow reintroduces oxygen and superoxide free radicals that damages cells.
|
|
|
What are the most common coronary artery occlusions in MI?
|
LAD > RCA > circumflex
|
|
|
What does the left anterior descending artery supply?
|
The anterior portion of the heart and the anterior 2/3rds of the IV septum.
|
|
|
What does the right coronary artery supply?
|
The posterior side of the heart. The posterior 1/3rd of the IV septum. The entire right ventricle. Also supplies posterior-medial papillary muscle of the mitral valve. AV node.
|
|
|
Obstruction of which can cause bradycardia: RCA or LAD?
|
RCA. It supplies the AV node.
|
|
|
How many hours/days after an MI is the heart the softest and at risk of rupture?
What type of necrosis do you see? After how many hours/days? |
Between 3-7 days.
Coagulation necrosis (low oxygen) after ~12-24 hrs. |
|
|
At point does tachycardia compromise filling of the coronary arteries?
|
180 bpm
|
|
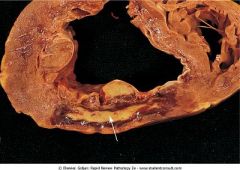
What is this showing?
|
Day 7 of acute MI in the posterior wall of LV. Yellow area is surrounded by dark, red granulation tissue.
|
|
|
What is the appearance of an MI 1-3 days after event? 4-7?
|
1-3: myocyte nuclei disappear, neutrophils lyse dead myocardial cells.
4-7: red granulation tissue, macrophages removing necrotic debris. |
|
|
Patient presents with severe retrosternal pain radiating down the left arm. The patient presents with sweating, anxiety, and hypotension. His symptoms are not relieved by nitroglycerin. What does he have?
|
MI
|
|
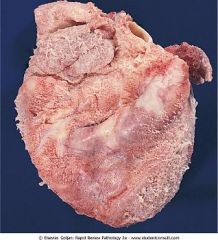
What does this show?
|
Fibrinous pericarditis
|
|

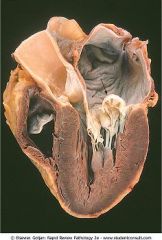
What does this show? Look at thin wall on the inferior portion of the ventricle.
|
Left ventricle aneurysm. Thin wall of scar tissue. Rupture is uncommon.
|
|
|
What is a mural thrombosis? How do you treat?
|
Thrombosis on the wall of the ventricle (most often LAD). Mixed characteristics of venous (stasis) clot and platelet-like clot. Asprin (platelet-like) and heparin/warfarin (venous-like).
|
|
|
MI complications:
|
Arrhythmia
Congestive heart failure Rupture (anterior wall, posterior papillary muscle, IV septum) Aneurysm (mural thrombus) Fibrinous pericarditis (early, late autoimmune) |
|
|
What is the most common arrhythmia caused by MI? Most common cause of death?
|
Ventricular premature beat. V-fib.
|
|
|
What is the consequence of an anterior wall rupture due to an MI? Where does the occlusion commonly occur?
|
Causes cardiac tamponade (fluid in pericardial cavity). This rupture is associated with thrombosis of the LAD coronary artery.
|
|
|
What is the consequence of an IV septal rupture as a result of an MI?
|
This rupture is associated with LAD coronary artery thrombosis. It produces a L to R shunt causing RHF.
|
|
|
What is the most common cause of death after a ventricular aneurysm?
|
A ventricular aneurysm as a result of an MI is clinically recognized within 4-8 weeks. CHF due to lack of contractile tissue is the cause of death.
|
|
|
What is Dressler's syndrome?
|
Autoimmune phenomenon resulting in fibrinous pericarditis several weeks post-MI.
|
|
|
Three weeks out of MI patient notices his chest bulging. What does he have? Whats the most common complication?
|
Ventricular aneurysm. Heart failure (<<EF)! (Not rupture).
|
|
|
CK-MB appears within ___to___ hours; peaks at ___ hours; disappears within ___to___ days.
|
4 to 8
24 hours 1.5 to 3 |
|
|
cTnI and cTnT appear within __to__ hours; peak at ___ hours; disappear within __to__ days.
|
3 to 6
24 7 to 10 |
|
|
How do you diagnose reinfarction?
|
CK-MB, because it shows up again 3 days later.
|
|
|
What is the LDH (1-2) flip?
|
Normally, LDH2 is higher than LDH1. In acute MI, LDH1 in cardiac muscle is released causing the "flip."
Appears within 10 hours; peaks at 2 to 3 days; disappears within 7 days |
|
What murmur would you here with this pathology?
|
Click (midsystolic) followed by late systolic murmur (not snap, murmur). Most common valvular lesion.
|
|
|
Whats the pathophysiology of mitral valve prolapse?
|
Redundancy of valve tissue:
Myxomatous degeneration of the mitral valve leaflets due to excess production of dermatan sulfate |
|
|
What valvular diseases most commonly causes hemolytic anemia with schistocytes?
|
Aortic stenosis
|
|
|
You hear an early diastolic murmur and notice a bunding pulses (water hammer pulse), head nodding, and a pulsating uvula. What is the diagnosis?
|
Aortic regurgitation.
|
|

What is shown?
|
Acute rheumatic fever. Uniform, verrucoid-appearing sterile vegetations appear along the line of closure of the mitral valve.
|
|
|
What is the pathogenesis of Rheumatic fever?
|
Pathology: Immune-mediated disease that follows group A streptococcal infection. Antibodies develop against group A streptococcal M proteins. Antibodies cross-react with similar proteins in human tissue. Type II hypersensitivity reaction
|
|
|
What causes Rheumatic fever?
|
Group A streptococcal pharyngitis.
|
|
|
How is acute rheumatic fever diagnosed?
|
Increased antistreptolysin (ASO) titers, positive throat culture, leukocytosis, increased PR interval, increased C-reactive protein.
|
|
|
What valvular disease are commonest in rheumatic fever?
|
Mitral regurgitation > aortic regurgitation. In chronic infection: mitral stenosis.
|
|
|
What are Aschoff bodies?
|
They are present in myocarditis caused by rheumatic fever. They are a central area of fibrinoid necrosis surrounded by reactive histiocytes.
|
|
|
What is Sydenham's chorea?
|
Reversible rapid, involuntary movements affecting all muscles. It results from childhood infection with Group A beta-hemolytic Streptococci (rheumatic fever).
|
|
|
Mitral senosis is most often caused by chronic rheumatic fever. Give four clinical findings in mitral stenosis.
|
Dyspnea (pulmonary capillary congestion).
Atrial fibrillation (atrial dilation/hypertrophy). Pulmonary venous hypertension (leads to RVH). Dysphagia for solids (compression of the esophagus). |
|
|
Give the most common causes of mitral regurgitation.
|
Mitral valve prolapse, LHF, infective endocarditis, and dysfunction of the papillary muscle.
|
|
|
What causes aortic stenosis?
|
Dystrophic calcification of a normal or bicuspid aortic valve. Chronic rheumatic fever.
|
|
|
What causes aortic regurgitation?
|
Isolated aortic valve root dilation.
Infective endocarditis. HTN. Rheumatic fever. Aortic dissection. Coarctation |
|
|
Name the microbial pathogens responsible for infective endocarditis.
|
Streptococcus viridians – most common cause of IE.
Staphylococcus aureus – most common cause of IE in IV drug abuse. Staphylococcus epidermidis – most common cause of IE due to prosthetic device. Streptococcus bovis – most common cause of IE in ulcerative colitis or colorectal cancer. |
|
|
Patient presents with fever, splenomegaly, splinter hemorrhages, and a pansystolic murmur which is heard louder on expiration. What does this patient have?
|
Infective endocarditis causing mitral valve regurgitation.
|
|
|
What produces sterile vegetations on the mitral valve surface?
|
SLE associated Libman-Sacks endocarditis.
|
|
|
Patient presents with fever, chest pain, CHF. Labs show increased CK-MB, troponins. What virus could cause these symptoms? What protozoa?
|
Coxsackievirus. Trypanosoma cruzi. A lymphocytic infiltrate is highly predictive of coxsackievirus.
|
|
|
What are the clinical features of pericardial effusion?
|
Muffled heart sounds, hypotension associated with pulsus paradoxus, Kussmaul's sign (jugular vein distention).
Water bottle configuration on CXR. |
|
|
Patient presents with hypotension and the heart on ausculation has a distinctive knock. What does this patient have?
|
Constrictive pericarditis. TB is the most common cause worldwide. the pericardial knock is due to the ventricles hitting the thickened parietal pericardium.
|
|
|
Define cardiomyopathy. What three types are there?
|
Group of diseases that primarily involve the myocardium and produce myocardial dysfunction.
Dilated, hypertrophic, restictive. |
|
|
Name the causes of cardiomyopathy.
|
Idiopathic > genetic causes > drugs (doxorubicin, cocaine), postpartum > thiamine deficiency (EtOH).
|
|
|
Patient presents with an EF < 40%, CXR shows a global enlargement of the heart, and echo shows poor contractility. What type of cardiomyopathy is this?
|
Dilated.
|
|
|
What is the most common cause of sudden death in young individuals?
|
Hypertrophic cardiomyopathy. Familial form in young individuals: mutation in heavy chain of beta-myosin and in the troponins.
|
|
|
What is the pathophysiology of hypertrophic cardiomyopathy?
|
Hypertrophy IV septum + anterior MV leaflet drawn against septum = decreased CO.
Conduction system in the IV septum is damaged = sudden death. |
|
|
How is the ejection murmur created by hypertrophic cardiomyopathy affected by preload?
|
Increased preload decreases the murmur (reclining, negative inotropic drugs).
|
|
|
What is Pompe's disease? Why type of cardiomyopathy can it cause?
|
Autosomal recessive glycogen storage disease. Lysosomal storage disease with a deficiency in alpha-glycosidase. The muscular weakness can lead to restrictive cardiomyopathy.
|
|
|
Name the infiltrative causes of restrictive cardiomyopathy.
|
Pompe's glycogenosis, amyloidosis, hemochromatosis. Sarcoidosis.
|
|
|
Loeffler endocarditis?
|
Cardiac damage caused by the damaging effects of eosinophil granule proteins (ex. major basic protein) is known as Loeffler endocarditis
|
|
|
The afferent pain fibers from the heart run centrally in the thoracic cardiac branches of the sympathetic trunk and enter spinal cord segments at the same dermatome level as __to__.
|
T1 - T5
|
|
|
The innervation of the pericardium is supplied by the phrenic nerve. Pain sensation is referred to __to__ dermatomes.
|
C3 -C5
|
|
|
The epicardium is also known as what layer of the heart?
|
The visceral layer of serous pericardium.
|
|
|
What percent of cases is the cause of myocardial ischemia due to atherosclerotic coronary arterial obstruction?
|
90%. This IHD is often termed coronary artery disease.
|
|
|
During which weeks of embryogenesis do congenital heart defects occur?
|
Gestational weeks 3-8 when major cardiovascular structures develop.
|
|
|
What is the primary site for gas exchange in the fetus?
|
Chorionic villus.
|
|
|
What fetal vessel has the highest amount of oxygen? Lowest?
|
Highest: umbilical vein
Lowest: umbilical arteries (2) |
|
|
Why do newborns have polycythemia?
|
HbF has a higher affinity for oxygen. To supply sufficient oxygen to tissue the baby increases the number RBC.
|
|
|
What vasodilator keeps the ductus arteriosus open?
|
Prostaglandin E2 made by the placenta.
|
|
|
What shunts lead to a step up in oxygen content? What shunt leads to a step down?
|
Step up = left-to-right (75 to 80)
Step down = right-to-left (95 to 80) |
|
|
What are the clinical findings in left-to-right shunts?
|
Pulmonary hypertension which will cause right ventricular hypertrophy. Reversal of the shunt occurs when pressure in RV overrides LV pressure, which leads to cyanosis (Eisenmenger syndrome).
|
|
|
Name the left-to-right cardiovascular defect shunts.
|
ASD, VSD, AVSD, patent ductus arteriosus.
|
|
|
Name the types of atrial septal defects.
|
Secundum ASD (90%), primum ASD and sinus venosus (5% each). Patent foramen ovale is present in up to 1/3rd of individuals and may/may not be considered an ASD.
|
|
|
Atrial septal defects are associated with ______ and ______.
|
Fetal alcohol syndrome and Down syndrome. Down syndrome is actually an AVSD.
|
|
|
Which left-to-right cardiovascular shunt commonly spontaneously closes?
|
VSD. Types: membranous and infundibular VSDs.
|
|
|
Ventricular septal defects are associated with _____,_____, and _____.
|
Cri du chat syndrome, trisomy 13, and trisomy 18.
|
|
|
A continuous machine-like murmur is heard during systole and diastole. Additionally the patient has a pink upper body and a cyanotic lower body. Diagnosis?
|
Patent ductus arteriosus which as reversed to a right-to-left shunt.
|
|
|
Patent ductus arteriosus is associated with _____.
PDA can be closed with _____. |
Congential rubella.
Indomethacin. Inhibits PGE2. |
|
|
What are the clinical features of right-to-left shunt
|
Cyanosis. With chronic cyanosis patients can develop hypertrophic osteoarthropathy (clubbing), polycythemia, and infective endocarditis
|
|
|
Name the right-to-left cardiovascular shunts.
|
Tetralogy of Fallot, complete transposition of the great vessels, truncus arteriosus, tricuspid atresia, total anomalous pulmonary venous connection.
|
|
|
What are the four features of tetralogy of Fallot? Which feature determines the severity?
|
VSD, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy. The degree of pulmonary stenosis determines the severity of the disease.
|
|
|
Name two cardioprotective shunts that would aid the survival of someone with tetraology of Fallot.
|
PDA and ASD.
|
|
|
What is the congenital defect in total anomalous pulmonary venous return?
|
Pulmonary vein empties oxygenated blood into the right atrium.
|
|
|
Name the obstructive congenital anomalies.
|
Coarctation of the aorta, pulmonary stenosis/atresia, and aortic stenosis/atresia.
|
|
|
Hows does adult and infantile aortic coarctation differ?
|
Infantile is preductal while adult is distal to the ligamentum arteriosum.
|
|
|
Patient presents with a systolic murmur, decreased blood pressure in the lower extremities (>10 mmHg less than upper), leg claudication and hypertension. What is your diagnosis?
|
Adult coarctation.
|
|
|
Infantile coarctation is associated with _____.
|
Turner's syndrome.
|
|
|
What is paradoxical embolization?
|
In right to left shunts, emboli from peripheral veins can bypass the normal filtration action of the lungs and enter the systemic circulation.
|
|
|
A 9 year old girl is diagnosed with acute rheumatic fever. Instead of recovering she dies. What is the cause of death?
|
The most common cause of death that occurs during acute rheumatic fever is cardiac failure secondary to myocarditis.
|
|
|
What is Sydenham chorea?
|
A central nervous system manifestation of acute rheumatic fever. It is characterized by involuntary, purposeless muscular movements, and bizarre grimaces, as well as emotional lability.
|
|
|
In what disease is the bundle of Kent present? What does the characteristic ECG look like?
|
Wolf-Parkinson White syndrome. ECG has prolonged QRS with a delta wave.
|
|
|
Describe the ECG tracing of atrial fibrillation. How do you treat?
|
Irregularly irregular and no discrete P waves. Coumadin to prevent clot formation.
|
|
|
Describe the ECG tracing of atrial flutter. How do you treat?
|
Sawtooth appearance. Class IA, IC or III antiarrhythmics.
|
|
|
Describe the ECG's of AV heart blocks.
|
First degree: prolonged PR (>.2)
Second degree: Mobitz I: progressively longer PR intervals till P wave is dropped. Mobits II: consistent PR's from beat to beat until one drops. Third degree: independent atria and ventricular beats. |
|
|
How would a LBBB appear on an ECG tracing?
|
Wide QRS which are mostly negative in V1-2. M morphology in V5-6.
|
|
|
How would a RBBB appear on an ECG tracing?
|
QRS is mostly positive with M morphology in V1-2. Large S wave in V5-6.
|
|
|
Tosades de pointes can be caused by:
a. prolonged PR b. absent T c. prolonged QT d. tachycardia |
c. Prolonged QT interval can predispose to torsades de pointes. It shows up on ECG as a sinusoidal waveform around the isoelectrical point.
|
|
|
Does hyperkalemia or hypokalemia increase the risk of ventricular fibrillation?
|
Hyperkalemia. Nerst equation includes -(K in/K out). Increasing K out makes the membrane potential less negative and closer to the threshold potential, therefore it is easier to elicit an AP.
|
|
|
What are the pacemaker rates at the SA, AV, and His-Purkinje system?
|
SA = 60-80, AV = 40-60, Purkinje = 20-40
|
|
|
What antiarrhythmic drug class is used to treat acute ventricular arrhythmias?
|
Class IB - lidocaine. Lidocaine is best used in post-MI conditions, because it acts on damaged tissue, not normal myocytes.
|
|
|
What is the best antiarrhythmic drug to use for paroxysmal supraventricular tachycardia?
|
Adenosine.
|
|
|
Hyperthyroidism can cause _____ in the heart.
|
Arrhythmia. Most often tachycardia.
|
|
|
What are the three types of atria fibrillation?
|
Paroxysmal - recurrent episodes that are self-limiting within 7 days
Persistent - recurrent episodes that are not self-limiting Permanent - last than more than a year |
|
|
What is the atrial rate (of impulses) in atrial fibrillation? In this condition what is the rate in the ventricles?
|
400-600 bpm, but most are blocked in the AV node and the ventricles are normally 80-180 bpm.
|
|
|
What antiarrhythmias would you use in atrial fibrillation to control the rate in the ventricles?
|
Beta blockers which suppress abnormal pacemakers by decreasing the slope of phase 4. Ca channels also work at the AV nodal cells (verapamil).
|
|
|
How many premature ventricular contractions qualifies as ventricular tachycardia?
|
3 or more.
|
|
|
What is sick sinus syndrome? What are some causes?
|
Both fast and slow arrhythmia due to a malfunctional SA node.
Can be caused by sarcoidosis, amyloidosis, Chagas, cardiomyopathies |
|
|
In what situation is the antiarrhythmic Mg (2+) used?
|
Torsades de pointes and digoxin toxicity.
|
|
|
What antiarrythmic drug class can cause bradycardia?
|
Beta blockers.
|
|
|
What is the Jones criteria used for?
|
Diagnoses of Rheumatic Fever. Major criteria: erythema marginatum, migratory polyarthritis, subcutaneous nodules, chorea, carditis. Minor: fever, arthralgia, leukocytosis, increased ESR, ECG heart block, ASO, etc. Diagnosis: 2 major and + culture or 1 major, 2 minor, + culture.
|

