![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
24 Cards in this Set
- Front
- Back
|
definition of pulmonary hypertension
-pulmonar artery systolic pressures greather than ____ at rest or ___ with exercise |
pulmonary arter systolic pressures of greater tahn 25mmHg at rest or 30 mmHg with exercise
|
|
|
symptoms of pulmonary hypertension
|
-asymptomatic
-lower body edema -RUQ pain or fullness -shortness of breath on exertion -weakness, fatigue -chest pain and exertional syncope -sudden death |
|
|
Direct signs of pulmonary hypertension
heart sounds |
increased or palpable P2 (the pulmonary component of S2)
-may have a systolic ejection murmur or a narrowed splitting of S2 -thus, direct signs of pulmonary hypertension are subtle, not always present and frequently underappreciated |
|
|
Name the indirect signs of pulmonary hypertension:
|
Signs of Right ventricular hypertrophy: para-sternal heave (lift); right sided S4 sound
increased atrial "a" wave" Signs of right Ventricular Fialure: -tricuspid regurg: Holosystolic murmur, "V" wave in jugular veins, pulsatile liver -volume overload: elevated jugular venous pressure right sided S3, peripheral edema |
|
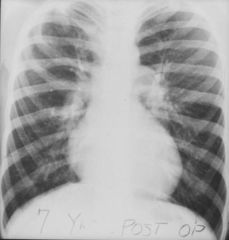
what do you see?
what would you see on an EKG? |
signs of pulmonary hypertension
-CXR: large pulmonary arteries -"pruning" of pulmonary vasculature EKG: "P" Pulmonale; right bundle block; rightward axis deviation |
|
|
Diagnosis of pulmonary hypertension
-direct vs. indirect? |
direct measurement of pressure: Swan-Ganz catheterization; advanced: Accuracy, can follow response to therapy; disadvantage: invasive, complications
-Indirect estimation of pulmonary artery pressure: Doppler echocardiography Adv: non-invasive, suggests alternative diagnosis. Disadv: accuracy, depends on TR jet, no cardiac output measurement |
|
|
-etiologies of pulmonary hypertension
|
increase in flow through pulmonary circulation
-increase in pulmonary vascular resistance -increase in pulmonary venous pressure PA=CO x PVR |
|
|
Etiology of Pulmonary Hypertension (Clinical types)
|
Hypoxic vasoconstriction (COPD, OSA, Neuromuscular disease, kyphoscoliosis, altitude)
-decreased pulmonary vasculature bed (emboli, emphysema, primary pulmonary HTN, HIV, collagen vascular disease, fibrotic lung disease, drugs) -Volume or pressure overload (congenital heart disease, left sided heart failure, mitral stenosis, pulmonary veno-occlusive disease) |
|
|
clinical classifcation of pulmonary hypertension
|
-pulmonary arterial hypertension
-pulmonary veno-occlusive disease (PVOD) -PH owing to left heart disease -PH with lung diseases/hypoxemia 4) chrnoic thromboembolic pulmonary hypertension -PH with unclear multifactorial mecahnisms |
|
|
drugs for pulmonary hypertension
|
endothelin receptor antagonists (bosentan, selective ET-A inhibitiors (oral)
-PDE-5 inhibitors: sildenafil and Tadalafil -combination therapy -atrial septostomy -transplant -nitric oxide -Phosphodiesterase type 5 inhibitor (leads to vasodilation, prevents breakdown of cAMP) -prostacyclin derivatives (prostacyclin, Iloprost, Treprostinil) |
|
|
symptoms/clinical manifestations of pulmonary thromboembolism?
|
asymptomatic
leg swelling, redness, pain, SOB (73%) (on exertion) -pleuritic chest pain (66%), cough (37%), hemoptysis (13%), syncope, sudden death (8%) |
|
|
risk factors for PE (in general)
Virchow's triad? |
1) Stasis
2) Hypercoagulability 3) endothelial damamge |
|
|
Risk factors for PE
acquired vs. congenital name the congental risk factors name the acquired factors |
Congenital: Thrombophilia (Factor V Leiden, Thrombin gene mutations, protein C and S deficiency, Antithrombin III deficiency)
Acquired: immobility of Lower Extremities, Surgery (esp. orthopedic of LE), trauma, stroke, heart failure, medical illness, critical illness, pregnancy, exogenous estrogens, malignancy, inflammatory disorders, nephrotic syndrome, APLA, smoking, age) |
|
|
clinical signs of PE
in terms of lung and heart and extremities |
increased RR
-hypoxemia, crackles, pleural friction rub cardiac: tachycardia, hypotension, right sided S4, elevated jugular venous pressure, increased P2 extremities: leg swelling, redness |
|
|
Adjunctive tests in PE:
-EKG? -CXR? -ABG? |
EKG: sinus tachycardia, T wave inversion, rightward axis, RBBB, S1Q3T3
-CXR: Normal, Atelectasis, Pleural effusion, Hampton's hump, Westermark's sign -ABG: hypocapnia and hypoxemia. A-a gradient not very useful |
|
|
describe the investigational approach to diagnosing a patient wih suspected PE
|
Well's critieria; if over 6 points 78% chance of PE
Diagnositc testing: D-Dimer and dead-space measurement -assessment of lower extremities for DVT -ventilation/perfusion scanning -CT angiography of pulmonary arteries -MRI thorax for PE -pulmonary angiography |
|
|
what is D-dimer?
|
quantitative measure of degraded, crosslinked fibrin
-levels lower than 200-500ng/ml are associated with a low chance of having a pulmonary embolism -levels can be elevated by about any inflammatory, malignant, infectious condition as well as pregnancy and recent surgery -performs best in patients with a low clinical supspicion and no risk factors |
|
|
when investigating for a PE how do you assess the lower extremities for DVT?
|
compression
doppler ultrasonography or venography -very useful in symptomatic patient -over half patients with PE may have negative compression ultrasound of LE -serial examinations may be useful to identify patients at low risk for subsequent PE |
|
|
Ventilation-perfusion scanning
-in theory areas with PE should have ____ventilation and _____perfusion |
normal ventilation
absent perfusion V/Q scan- advantages- longtime use, safety and availability disadvantages- frequent non-diagnostic results, radiation exposure |
|
|
describe CT angiogram of pulmonary arteries; useful for?
|
PE
-involves a rapid bolus of IV contrast and then rapid, high resolution CT scanning through the pulmonary arteries -in a positive study filling defects are seen within the pulmonary arteries |
|
|
gold standard test for diagnosis of pulmonary emboli
-invasive and potentially dangerous; measurable mortality, around 0.5% -negative test virtually excludes PE |
pulmonary angiography
|
|
|
treatment of pulmonary emboli
|
-anticoagulation with heparin or low molecular weight Heparin or Fondaparinux then coumadin
-removal of aggravating cause when possible -thrombolysis for hemodynamically unstable patients -IVC filters in cases of LE DVT in patients who cannot be anti-coagulated |
|
|
_____ ____ is a disease of insidious onset with protean physical findings
|
pulmonary hypertension
|
|
|
-the three major mechanisms of pulmonary hypertension are:
|
hypoxic vasoconstriction, loss of the pulmonary vascular bed and volume or pressure overload
|

