![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
24 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Rheumatic Fever
|
acute, recurrent inflammatory dz that develops 1-6 weeks post *group A Strep* infection
-occurs primarily in children 5-15 years -Pathogenesis: most likely antigen/antibody - - host anti-strep antibodies that are cross-reactive to cardiac antigens |
|
|
|
Dx of rheumatic fever
|
-Erythema marginatum - - macular lesions with erythematous rims & central clearing in a bathing suit distribution
-Sydenham chorea - - rapid, involuntary, purposeless movements -Carditis - - 50 – 75% of children & 35% of adults. Usually a pancarditis -Subcutaneous nodules -Migratory large joint polyarthritis - - 90% of adults but less common in children -Fever -Arthralgia |
|
|
|
Labs
|
Elevated acute phase reactants:
C- reactive protein Ceruloplasmin Alpha 1 antitrypsin C-3 complement Prolonged PR interval |
|
|
|
Clinical
|
Clinical: death is rare during the acute phase; if so, 2° to myocarditis. Usually myocarditis & arthritis are transient and resolve without complications. Valvular involvement may lead to deformation and scarring (particularly mitral valve)with permanent dysfunction → chronic rheumatic heart disease → CHF.
|
|
|
|
Chronic rheumatic heart disease is most likely when:
|
-1st attack is in early childhood
-1st bout of rheumatic fever is severe -Have recurrent attacks |
|
|
|
Physical → changes 2° to mitral stenosis
|
-Left atrial hypertrophy & enlargement
-Chronic congestive changes in lungs -Right ventricle hypertrophy -CHF |
|
|
|
Gross/ Micro
|
-acute vasculitis with formation of beady fibrinous vegetations
|
|
|
|
Gross/Micro: Chronic Valve Dz
|
--fibrous thickening of leaflets
--briding fibrosis across commisures --thickened, fused and shortened mitral valve chordae |
|
|
|
Gross/Micro: Calcification deep in leaflets
|
--* Solitary Mitral involvement 65 – 70%; combined aortic & mitral 20-25%; tricuspid & pulmonic valves are less frequently affected
--* Histo the Aschoff bodies are pathognomonic - - these are foci of fibrinoid necrosis in the myocardium. Initially surrounded by lymphs, macrophages & a few plasma cells, they slowly become a fibrous scar |
|
|
|
Aschoff nodules
|
microscopic mark of acute rheumatic carditis; peculiar form of granulomatous inflammation seen best in myocardium; centered in interstitium around vessels
|
|
|
|
Aschoff giant cell
|
large cells with two or more nuclei that have prominent nucleoli. Scattered inflammatory cells accompany them and can be mononuclears or occasionally neutrophils
|
|
|
|
Anitschkow myocyte
|
This is a long, thin cell with an elongated nucleus.
|
|
|
|
rheumatic valvulitis
|
acute endocardial inflammation along with fibrosis, especially of the mitral valve; seen with shortened, thickened chordae tendineae
|
|
|
|
chronic rheumatic scarring
|
fish mouth mitral valve
|
|
|
|
most commonly affected valves in RHD
|
-mitral
-mitral+aortic -aortic -mitral+aortic+tricuspid |
|
|
|
Acute Pericarditis: Serous
|
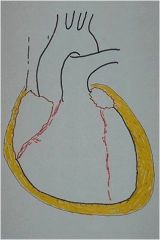
50 – 200 cc of slowly accumulating fluid – typically 2° to nonbacterial involvements – frequently unknown etiology
|
This diagram depicts the appearance of a serous pericarditis. The amount of inflammation is minimal, so no exudation of fibrin occurs. The dark stippled dots in the yellow fluid and on the epicardial surface represent scattered inflammatory cells. Serous pericarditis is marked by fluid collection. Rarely, the fluid collection may be large enough to cause tamponade
|
|
|
Acute Pericarditis: Fibrinous & Serofibrinous
|
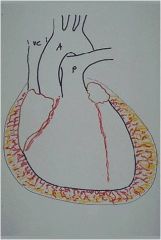
most common- seen with MI & produces friction rub – usually completely resolves without sequelae
|
This diagram depicts the appearance of a fibrinous pericarditis. The red-pink squiggly lines extending from the epicardial surface into the yellow fluid represent the strands of fibrin. This type of pericarditis is typical of uremia with renal failure, underlying myocardial infarction, and acute rheumatic carditis
|
|
|
Acute Pericarditis: Purulent
|
usually 2° to bacterial, fungal or parasitic infection which has reached the pericardium by direct extension – most common causative organisms - - gram (+) staph, strep & pneumococci. Usually 4-500 cc of fluid which organizes & may → constrictive pericarditis
|
|
|
|
Acute Pericarditis: Hemorrhagic
|
most often follows cardiac surgery or associated with TB malignancy; TB can also lead to a granulomatous pericarditis that may calcify and produce a "constrictive" pericarditis.
|
|
|
|
Acute Pericarditis: Caseous
|
2° to TB & usually direct extension from lymph nodes (rarely from mycotic infection) → fibrocalcific constrictive pericarditis
-really just fibrinous pericarditis with hemorrhage. Without inflammation, blood in the pericardial sac would be called "hemopericardium". |
|
|
|
Chronic Pericarditis 1.
|
Healing of the acute lesions may yield resolution or pericardial fibrosis which varies from a thick, nonadherent epicardial plaque (soldier’s plaque) to thin, delicate adhesions, to massive adhesions
|
|
|
|
Chronic Pericarditis 2.
|
Adhesive mediastinopericarditis is of clinical significance because the pericardial sac is obliterated & the parietal surface is tethered to mediastinal tissue. Results in hypertrophy & dilation
|
|
|
|
Chronic Pericarditis 3.
|
Usually 2° TB or purulent pericarditis
|
|
|
|
Chronic Pericarditis: Constrictive
|
TB most common cause – clinically significant because of thick, dense, fibrous obliteration of the pericardial sac- often calcification – limits diastolic expansion & restricts output
|
|

