![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
What is the name of the fibrous rings formed by the dense connective tissue of the valves condensing around the attached margins? |
Valvus annulus. These 4 rings form the fibrous skeleteon of the heart |
|
|
What do the chordae tendinae merge into when they attach onto the leaflets? |
Lamina fibrosa. |
|
|
What causes varicose veins? |
Valvular incompetency due to dilation of poorly supported superficial veins -> retrograde blood flow -> tortuous dilatation and lengthening of veins. |
|
|
Describe the pathogenesis of atherosclerosis. |
1. Chronic endothelial injury - hyperlipidaemia, hypertension, smoking, homocysteinaemia, haemodynamic factors, toxins, viruses, immune reactions 2. Endothelial dysfunction - increased permeability, leucocyte adhesion, monocyte adhesion and emigration 3. Smooth muscle recruitment to intima, macrophage activation. Macrophages and smooth muscle engulf lipid 4. Smooth muscle proliferation, collagen and other ECM deposition, extracellular lipid + fibrous cap. |
|
|
What is in a) the fibrous cap, b) the necrotic centre? |
a) SM cells, macrophages, foam, lympho, collagen, elastin, proteoglycans b) cell debris, cholesterol crystals, foam cells |
|
|
What period of time is required for permanent damage to occur? |
At least 2-4 hours. |
|
|
At what point is the post-MI heart most prone to rupture? |
5-10 days as solid muscle is being replaced with granulation tissue |
|
|
Describe the appearance of the myocardium 12 hours post MI. |

Necrotic stains darker - coagulative necrosis |
|
|
Describe the appearance of the myocardium 3-4 days post MI. |
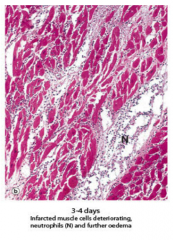
Neutro and oedema |
|
|
Describe the appearance of the myocardium 10 days post MI. |

Necrosis mainly removed by neutro, loose oedematous mesh w/ macro lympho and plasma. |
|
|
Describe the appearance of the myocardium 14 days post MI. |
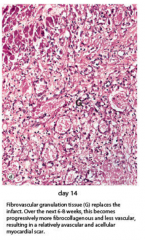
Fibrous granulation tissue replaces infarct. More fibrocoll less vascular -> scar |
|
|
What nodular inflammatory lesions are found in interstitial connective tissue of the myocardium of acute rheumatic fever patients? |
Aschoff bodies. Fibrinoid change with lymphocytes and large distinct macrophages and central areas of necrosis. |
|
|
What happens when there is chronic mitral valve damage during rheumatic fever? |
Rheumatic mitral stenosis. Fibrotic thickening leaflets, fusion commissures (where leaflets come together at insertion to annulus) Chordae tendinae fusion and shortening. Can get acute mitral valvulitis -> chordae fusion. |
|
|
Where does the atherosclerotic PLAQUE occur? |
In the tunica intima. |
|
|
When does the respiratory epithelium change? |
Simple columnar in bronchioles Simple squamous in alveoli. |
|
|
What causes pseustrat columnar -> strat squamous metaplasia? |
Irritant e.g. cigarrete smoke - less functional because less mucous. |
|
|
What can squamous metaplasia lead to? |
Squamous cell carcinoma in main bronchi or other major bronchi |
|
|
How can you divide lung carcinoma? |
Small cell - 20-25% Non small cell: 75-80% - more localised: 25-40% Squamous cell 25-40% adenocarcinoma - bronchioalveolar carcinoma 10-15% large cell carcinoma - large cell neurendocrine carcinoma |
|
|
What are features of small cell carcinoma? |
Small ovoid oat cell like tumours - highly malignant |
|
|
Which stain can stain keratin and thus identify squamous cell differentiation? |
Papanicolaou - stained orange. |
|
|
What do primary tumours of the lung often stain for? i.e. how do you differentiate primary and secondary lung tumours? |
Thyroid transcription factor in primary |
|
|
Describe a mycobacterium TB granuloma. |
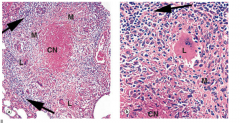
Caseous granuloma: central area of caseous necrosis surrounded by 'epitheliod' macrophages - fuse and form multinucleate Langerhan's giant cells. Rim of lymphocytes (arrows) around macrophages. |
|
|
What happens to the lymphocyte layer of the tubercle as it progresses? |
Fibroblasts in the lymphocyte layer - stimulated to lay down collagen in the ECM to wall off tubercle |
|
|
What happens in a successful macrophage-lymphocyte-fibroblast defensive reaction of TB? |
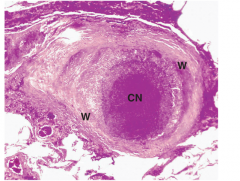
Usually the case in primary TB, tubercle wall thickened with fibroblast prolif and deposition dense fibrocollagenous tissue -> fibrocaseous tubercular nodule, often calcifies. |
|
|
How does TB enter the lung tissue? |
Gravitate to lower parts of conducting airways, destroy bronchial wall -> enter the peribronchial tissue - form tubercles and destroying large areas of lung tissue |
|
|
What are the 3 types of TB? |
Primary - restriction to subpleural areas in midzone of lung and the draining hilar lymph nodes. - Gohn foci Postprimary/secondary - focus of apical, usually bilateral lesions - Assman foci Miliary - disseminated granulomas |
|
|
What is the main defence cell found in the alveolar spaces? |
Neutrophils |
|
|
What is hereditary eliptocytosis? |
AD, if heterozygous then mild Failure of spectrin heterodimers -> heterotrimers. Homozygous -> severe haemolysis. |
|
|
When would you find Howell Jolly bodies? |
Nuclear remnants in RBCs. Normally removed by spleen, salient in hyposplenism/post splenectomy. |
|
|
What is autoimmune thrombocytopoenic purpura? |
Highest incidence woman 15-50 Upon bone marrow aspiration - normal/increased megakaryocytes. Purpuric rash, increased tendency to bleed. Thrombocytopoenia. |
|
|
When can target cells appear in the blood? |
Liver disease, post splenectomy, fe deficiency, haemaglobinopathy |
|
|
What are features of myelo/lymphoblasts? |
Larger than red cells, normally found in marrow, if acute leukaemia, are found in blood.
Myeloblasts are granulated, lympho are not. CD differentiation for precision. |
|
|
How does chronic lymphocytic leukaemia cause pancytopaenia? |
BM infiltrates by lymphocytes -> reduced synthesis other lineages. |
|
|
What is AML? |
Promyelocytic = M3, t(15:17) DIC is common - aggravated by chemo. Alltrans retinoic acid to treat DIC Pancytopaenia. Easy bleeding from gums |
|
|
What is leucoerythoblastic anaemia? |
Leucocytosis, erythoblastosis, tear drop pear cells in blood film. Extramedullary haematopoesis -> hepatosplenomegaly -> primary myelofibrosis. BM biopsy shows hypercelllular marrow - Jak2 mutation - also in bone marrow infiltration breast/prostate cancer |
|
|
What is multiple myeloma? |
Clonal proliferation of B cells in BM w/ evidence monoclonal Ig/ light chains in serum/urine + tissue damage e.g. bone/renal Anaemia + rouleux formation due to raised Ig levels, background blue staining due to increased Ig + neutro + thrombocytopoenia |
|
|
What are features chronic leukaemias have that acute leukaemias do not? |
Chronic - hepatosplenomegaly - extramedull haemato Plus no blast cells in film e.g. all cells look like lymphocytes and granulocytes. |

