![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
22 Cards in this Set
- Front
- Back
|
List and describe the four periods of lung development
|
1. Embryonic
2. Pseudo- Glandular 3. Canalicular 4. Terminal Saccular Stage 5. Post Natal or Alveolar |
|
|
Describe the two cell types formed during the Terminal Sac stage
|
Epithelium lining alveoli differentiates
into two cell types 1. Type I pneumocyte -Form part of the blood-air barrier 2. Type II pneumocyte- Secretory cells that produce surfactant, Reduces surface tension, and Facilitates alveolar expansion |
|
|
What are some clinical developmental malformations in thiese syndromes?
1. Infant Respiratory distress syndrome (IRDS) 2. Congenital neonatal emphysema- |
1. Infant Respiratory distress syndrome (IRDS)- absences of insuffiecency of surfactant causes atelectasis (incomplete expansion or collapse part of lung)
2. Congenital neonatal emphysema- overdistension of lung caused by collapsed bronchi, due to lack of bronchiole cartilage development |
|
|
What are some clinical developmental malformations in these syndromes?
1. hyaline membrane disease 2. congenital neonatal emphysema 3. oligohydramnios |
1. alveoli filled with debris in a near uniform distribution, which leads to ground glass appearance on chest x-ray
2. Over distension with air of one or more lobes of lung caused by collapsed bronchi, bronchial cartilage wont develop 3. low amniotic fluid, associated with renal agenesis and obstructive uropathy, causes pulmonary hypoplasia and limb defects |
|
|
Identify the clinical malformation by the following signs...
a. atelectasis and ground glass on x-ray b. honey comb appearance on x-ray c. due to lack of bronchiole cartilage development d. due to deficeincy or absence of surfactant |
a. IRDS- infant respiratory distress syndrome
b. congenital bronchial cysts (bronchiectasis) c. Congenital neonatal emphysema d. IRDS- infant respiratory distress syndrome |
|
|
What are some clinical developmental malformations in these syndromes?
3. Congenital bronchial cysts (bronchiectasis) 4. Pulmonary agenesis 5. Pulmonary hypoplasia |
3. Congenital bronchial cysts (bronchiectasis)- (abnormal destruction and dilation of the large
airways) due to developemental arest of bronchial tree 4. Pulmonary agenesis- Complete absence of lungs, bronchi & vasculature, Bilateral or unilateral Bronchial buds do not develop 5. Pulmonary hypoplasia- Poorly developed bronchial tree, Partial (small segment) or Total (entire lung), Bilateral renal agenesis Insufficient amniotic fluid (oligohydraminos) & increased pressure on fetal thorax |
|
|
Identify the clinical malformation by the following signs...
a. Complete absence of lungs, bronchi & vasculature, Bilateral or unilateral b. Bilateral renal agenesis Insufficient amniotic fluid (oligohydraminos) c. no kidneys, flattened face d. high volume of amniotic fluid |
a. Pulmonary agenesis
b. Pulmonary hypoplasia c. potter syndrome d. polyhydramnios |
|
|
What is the most commonly associated developmental malformation during tracheal developement?
Describe this malformation |
Tracheoesophageal Fistula
- Caused by improper formation of tracheoesophageal septum (from Tbx4 misexpression) - results in abnormal communication between trachea and esophogus Symptoms: 1. increased drooling 2. Gagging/cyanosis after swallowing milk 3. All include laryngotracheoesophogeal cleft, tracheal stenosis and atresia and treacheal lobes Treatment: 1. Balloon dilation 2. Tracheal stent |
|
|
Summarize the development of the trachea
|
i. Laryngotracheal (respiratory) diverticulum grows out from foregut into splanchnic mesoderm around developing pharanx.
ii. TBX4 (transcription factor) from endoderm of gut tube controls formation of lungs iii. First opening (laryngeal orifice), mesenchyme around it becomes thyroid, and cartilages that support larynx. iv. Respiratory divertaculum grows and is separated from esophagus by tracheoesophogeal septum |
|
Label parts of the primitive lung
|
|
|
|
Summarize the formation of primary, secondary and tertiary bronchi
- what tissue is all lung tissue derived from? |
primary- at distal end of laryngotracheal diverticulum left and right lung buds divide into 2 bronchial buds (become primary bronchi)
secondary- result of primary branches dividing... 3 right and 2 left, each buds many times until respiratory bronchioles have formed tertiary- further branching developes tertiary bronchi Lung Tissue- splanchnic mesoderm |
|
|
Describe in detail the embryonic stage of lung development
|
Weeks 4-7
- initial formation of respiratory diverticulum up to formation of all major bronchopulmonary segments -Lungs grow into and fill bilateral pleural cavities and become covered with visceral pleura, while parietal pleura line the pleural cavities |
|
|
Describe in detail the (pseudo glandular) stage of lung development
|
Weeks 8-16
- Major formation & growth of duct systems within bronchopulmonary segments - No respiratory components, no gas exchange - Histological structure resembles a gland - Induction of vasculogenesis of pulmonary veins may be mediated (VEGF), expressed in epithelium of terminal buds in fetal lung late in phase |
|
|
Describe in detail the Canalicular stage of lung development
|
Week 17-26- most important phase due to determining whether a pre-term baby can survive (depending on if alveoli have started to form)
Formation of respiratory bronchioles & terminal sacs (primitive alveoli) - Vascularization increases - Capillaries found in walls |
|
|
Describe in detail the terminal saccular stage of lung development
|
“Alveolar” (postnatal)
“Saccular” (week 26- birth) - Alveoli – or terminal sacs – develop from respiratory bronchioles - Epithelium lining alveoli differentiates into two types of pneumocytes types |
|

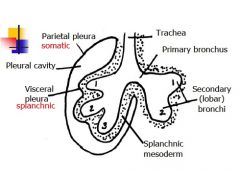
What is this picture showing?
|
1. Respiratory Bronchiole
2. Terminal Bronchiole 3. Splanchnopleuric mesoderm 4. Terminal sac 5. 28-36 weeks 6. 36 weeks- early childhood 7. mature alveolus |
|
|
Describe the two types of pneumocytes
|
Type I- forms blood- air barrier
type II- secretory cell produces surfactant over alveoli and reduces surface tension and facilitates alveolar expansion |
|
|
Explain what supernumerary bronchi or lobules and ectopic lobes are and how they form...
|
Supernumerary bronchi- from abnormal division and libation, usually bronchus coming from upper right trachea, close to carina
Ectopic- formed from additional respiratory buds of the foregut |
|
|
Describe how the body cavity is partitioned (3)
|
1. Intraembryonic coelom is a
continuous space that Divides into thoracic cavity and abdominopelvic cavity 2. Further divided thoracic cavity into 1 pericardial cavity and 2 pleural cavities 3. Pleuropericardial membranes & diaphragm |
|
|
What four things make up with diaphragm?
|
1. Septum transversum forms central
tendon 2. Pleuroperitoneal membranes – sheets of somatic mesoderm from dorsolateral body wall (muscular part of diaphragm) 3. Crura develop from mesenchyme around the foregut (dorsal mesentery) 4. Peripheral portions from somatic body wall mesoderm (innervated by intercostal nerves) |
|
|
Briefly describe the diaphragm happenings during week 4 and 8
|
Week 4: diaphragm becomes innervated by the phrenic nerve (C3-5). Phrenic nerve runs within the
pleuropericardial membranes Week 8- descent of diaphragm to L1 |
|
|
What happens if there is a failure of pleuroperitoneal membranes to fuse with other components?
Where is this most common? What are clinical signs? |
causes Congental Diaphragmatic Hernias
- most common on left posterolateral side - signs include: flat abdomen, breathlessness and cyanosis |

