![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
What is Shearing Forces? |
....results when one tissue layer slides over another. |
|
|
Microthrombi |
Microthrombi impede blood flow, and result in ischemia & hypoxia of tissues. |
|
|
During inflammatory response, patient can experience.... |
Increased : Temperature, pain, WBC's |
|
|
A pressure (decubitus) ulcer is? |
.... A specific type of tissue injury from unrelieved pressure or friction over bony prominences that results in ischemia and damage to the underlying tissue. |
|
|
Why does drainage (exudate) occur? |
It occurs as a result of the healing process and occurs during the inflammatory and proliferative phases of healing. 1g = 1mL of drainage. Most accurate measurement is to weigh the dressing. |
|
|
Primary intention healing |
Example-- surgical incision. |
|
|
Secondary intention healing |

|
|
|
Tertiary or delayed primary intention healing |
|
|
|
Patients with greatest risk of pressure ulcers are: |
Those with spinal cord injuries, hospitalized patients, and patients in LTCF |
|
|
Factors affecting skin integrity |
Genetics & heridity, age, chronic illness & its treatment, medications, poor nutrition |
|
|
Risk Assessment Scales |
Norton and Braden scales Braden - for predicting pressure sore risk 23 is total points... 18 or lower is at risk. Norton- pressure area risk assessment form scale Possible score of 24 & 15-16 = viewed as indicators of pressure ulcer development |
|
|
Stages 1 Pressure Ulcer |

NONBLANCHABLE erythema signaling potential ulceration |
|
|
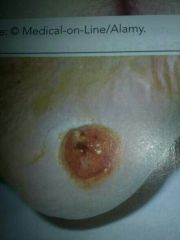
Stage 2 Pressure Ulcer |
Partial- Thickness skin loss involving epidermis and possible dermis. Presents as a shallow open ulcer WITHOUT SLOUGH. |
|
|
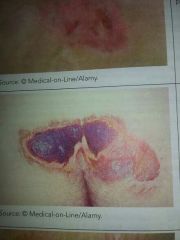
Stage 3 Pressure Ulcer |
Full-thickness skin loss involving damage or necrosis of subcutaneous tissue - slough may be present in this stage. Appears as a deep crater with or without undermining or tunnelling |
|
|
Stage 4 Pressure Ulcer |

Full- thickness skin loss with tissue necrosis or damage to muscle, bone, or supporting structures - bone, tendons, muscles are exposed and palpable- slough and eschar may be present. |
|
|
Inflammatory Phase |
Swelling Begins directly after the injury occurs - typically lasts about 3-6 days, phagocytosis, |
|
|
Proliferative Phase |
Scabs over Begins approx. On day 3 or 4 and continues until around day 24. Collagen synthesis begins in this phase. Granulation tissue forms in this phase as well. Contracts the wounds edges. Resurfaces new epithelial cells. -susceptible to bleed easily!!!!! |
|
|
Maturation phase or remodeling phase |
SCARS Occurs on day 21 and can last up to one to two years from when injury occurred. Wound is remodeled- scar tissue is formed and strengthing.. Will never be the same as it was before it was injured. |
|
|
Hemmorhage |
EXCESSIVE BLEEDING! not normal. |
|
|
Infection |
-difficult to determine when it happened and the underlying cause.. Impossible to keep EVERYTHING sterile.
Hand hygeine. -total hip replacement- infection- severe infection- can lead to futher surgery or implants be removed completely.... So no hip joint. Etc. |
|
|
Assessment/ Data Collection |
Red: healthy regeneration of tissue. (Protect, cover) Yellow: presence of purulent drainage or slough. (Clean) Black: presence of eschar that hinders healing and requires removal. (Debride, removal of necrotic tissue) Use a clock face with 1200 towards the clients head to document the location of sinus tracts. |
|
|
Serous Drainage |
Portion of the blood that is watery and clear or slightly yellow in appearance. (Fluid in blisters) |
|
|
Sanguineous |
Serum & red blood cells. Thick and red. Brighter= fresher drainage. |
|
|
Serosanguineous |
Serum and blood. Watery and appears blood streaked or blood tinged. |
|
|
Purulent Drainage |
The result of infection. Thick. Contains white blood cells, tissue debris, and bacteria. Yellow, tan, brown, depending on infectious organism. Foul odor!!! |
|
|
Purosanguineous |
Mixed drainage of pus and blood such as a newly infected wound. |
|
|
Protein Foods |
Meat, fish, poultry, eggs, dairy, beans, nuts, whole grains. |
|
|
Albumin. |
If below 3.5 = lack of protein means increase in delay of wound healing and infection. |
|
|
Wound Cleansing |
|
|
|
Wound Dressings |

|
|
|
Dehiscence & evisceration |
"Re-opened." Partial or total rupture (seperation) of a sutured wound, usually with seperation of underlying skin layers. Typically 4-5 days post op. {Sterile towel with normal saline} |

