![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
7 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is septation?
|
-occurs in two axes and multipule directions
-Protrusions from the lateral walls (endocardial cushions) form the atriventricular septum (transverse) -Migration downward toward the cushions forms the atrial septum -The atrial septum is two layers with offset openings; the ostium secundum, together with a flap of septum primum. This forms the foramen ovale, through which fetal blood flows R --> L. -Upward migration between the future ventricles forms the muscular ventricular septum -A spiral downward migration from the outflow tract (truncus arteriosus) aligns the ventricles with the developing great arteries. |
|
|
|
Fetal-Neonatal Transition
-Rapid Changes: |
- Pulmonary vascular resistance drops (so flow increases)
--in part mechanical (air fills lungs) --in part chemical (increased pO2 relaxes vessels) -Pulmonary venous return enlarges LA and functionally closes foramen ovale - Systemic resistance increases - Ductus arteriosus flow reverses |
|
|
|
Fetal-Neonatal Transition
- Slower changes |
- Foramen ovale closes fully
- Ductus venosus closes (and becomes ligamentum venosum) - Ductus arteriosus closes (and becomes ligamentum arteriosum) - LV grows and thickens in response to increased pressure and volume load (now pumping to the entire body) |
|
|
|
Congenital Heart Disease Incidence:
|
-Incidence
--0.5-0.8% of all live births ---excluding mitral valve prolapse, preterm PDA and bicuspid aortic valve - Up to 25% of stillborns - 2% of preterm infants -- Excluding PDA - Overall, about 0.2% of infants will show symptoms of CHD (majority of infants with CHD are not symptomatic) |
|
|
|
Describe fetal blood flow:
|
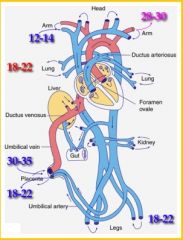
Red = High vascular resistance
Blue = Low vascular resistance # indicates pO2 (mmHg) |
|
|
|
Congenital Heart Disease Etiology:
|
Unknown in most cases
Genetic associations - Trisomy 18 (edwars Syndrome) - 90% have CHD - Trisomy 21 (Down Syndrome) - 50% - 45, XO (Turner Syndrome) -40% Teratogen exposure or adverse maternal condition - 2-4% of CHD |
|
|
|
Congenital Aortic Stenosis
|
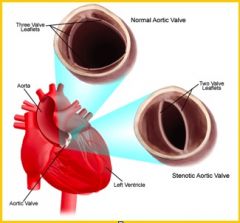
Anatomic pathology:
|
Clinical Presentation:
-Depends on location (valvular, subvalvular, supravalvular) and severity. - Bicuspid aortic valve (2% of adults) usually asymptomatic in childhood - Possible physical findings --Decreased pulse intensity --Early systolic ejection click --Paradoxically split S2 --Systolic ejection murmur RUSB Outcomes - Very good, unless critical obstruction - Even then, good - Disease progresses over 5-10 years can present very late in life Treatment options - Balloon valvuloplasty - Aortic valve replacement |

