![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
How many deaths/year d/t alcohol?
|
79,000
|
|
|
What percent of US adults meet criteria for an alcohol-use disorder?
|
9%
|
|
|
Alcohol use disorder defination
|
2 or more within a 12 month period
–Drinking more/for a longer period than intended –Persistent desire or unsuccessful efforts to cut back/quit –Spend a great deal of time to obtain, use, or recover from alcohol –Craving or strong desire/urge to use –Recurrent use resulting in a failure to fulfill major obligations at work, school, or home Withdrawal Tolerance |
|
|
drivers have driven under the influence of alcohol in the last year (#1)
|
26%
|
|
|
CAGE screening tool
|
•C – Have you ever felt the need to Cut down on your drinking?
•A – Have you ever felt Annoyed by criticism of your drinking? •G – Have you ever felt Guilty about your drinking? •E – Have you ever felt the need to drink a morning Eye-opener? |
|
|
MS consequences of alcohol
|
Osteoporosis
–Heavy alcohol use decreases bone density –Combined with an increased fall risk increased fracture risk Rib fracture in men think alcohol problem Gout –Especially in men – beer and spirits (not wine |
|
|
CV consequences of alcohol
|
Atrial fibrillation
–Occurs in up to 60% of binge drinkers –“Holiday Heart” Hypertension –More than 2 drinks/day 1.5 to 2-fold increase in incidence of hypertension –Dose-related effect Dilated cardiomyopathy Due to direct toxicity of alcohol and its metabolites (acetaldehyde), and thiamine deficiency; all 4 chamber dilation |
|
|
Renal/Respiratory consequences of alcohol
|
Aspiration pneumonia
–Severe intoxication-->inability to protect airway Respiratory depression –Severe intoxication, combination with pills |
|
|
Heme/Lymph consequences of alcohol
|
Direct toxicity of alcohol on hematopoesis +/- splenic sequestration (big spleen) in pts with liver cirrhosis
–Anemia – multiple additional mechanisms •Nutritional folate deficiency -->#1 cause is alcoholism •Increased bleeding risk with alcoholic cirrhosis –Leukopenia –Thrombocytopenia |
|
|
Endo/Repro consequences of alcohol
|
•Hypoglycemia
•Teratogenicity –Fetal alcohol syndrome –More subtle constellation of behavior/growth effects –Low birth weight •Spontaneous abortion Gynecomastia |
|
|
Neuro/Psych consequences of alcohol
|
•Peripheral Neuropathy
•Intoxication •Wernicke-Korsakoff Syndrome •Cerebellar degeneration •Alcohol Withdrawal •Seizures |
|
|
Major targets of alcohol
|
GABA and NMDA
|
|
|
GABA receptors
|
Suppress neuronal transmission
Help maintain resting membrane potential in some neurons |
|
|
NMDA receptors are used in
|
Learning and memory
Alcohol is an antagonist |
|
|
Activation promotes hyperpolarization via chloride flux
Contains 2 alpha, 2 beta, and 1 gamma subunit |
GABA-A receptors
Alcohol is a positive allosteric (non-competitive) modulator of the GABA-A receptor Chronic alcohol use results in cross tolerance to sedative hypnotics |
|
|
Ions in flux of NMDA
|
inward flux of Na+ and Ca++ and efflux of K+
Activated by glutamate |
|
|
Legal driving limit set at
|
80 mg/dL or 17 mM
|
|
|
Tolerant individuals may appear sober
|
at 300-400 mg/dL
|
|
|
90-98% of ethanol is metabolized
|
to acetaldehyde
|
|
|
What is induced in alcoholics?
|
MEOS 2E1
|
|
|
What enzyme is reduced in asians?
|
Aldehyde dehydrogenase
Genetic polymorphisms |
|
|
availability of what limits ethanol metabolism
|
NAD+
|
|
|
Major Metabolic consequences of alcohol
|
–Increased NADH inhibits TCA cycle
–Increased acetaldehyde •Generates adducts •Decreases glutathione •Inhibits microtubules |
|
|
Euphoric effects of alcohol are d/t?
|
Euphoric effects via elevation of dopamine and opiate neurotransmission
|
|
|
What are the neuro effects of alcohol and where are they in the brain?
|
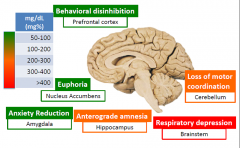
|
|
|
Ethanol saturation is what order kinetics?
|
Zero order
|
|
|
Dry beriberia
|
Thiamine deficiency
Polyneuropathy •Nonspecific peripheral neuropathy with myelin degeneration •Motor, sensory, and reflex arcs •Usually appears first in legs (foot drop) |
|
|
Dilated CM
|
Wet beriberi
|
|
|
Presentation of Wernicke encephalopathy
|
Clinical presentation
–Confusion, ophthalmoplegia, ataxia (triad) nystagmus, coma |
|
|
Area of brain affected by Wenicke encephalopathy
|
Mammillary bodies (will be discolored and atrophic can see petichae hemorrhages), dorsomedial thalamus, around 3rd and 4th ventricles
|
|
|
Korsakoff psychosis
|
Irreversible, hypothesized to result from repeated episodes of Wernicke enceph.
–Inability to acquire new information (anterograde amnesia), confabulation, preserved intelligence and learned behavior |
|
|
Ataxia is associated with?
|
Vermis atrophy
Dropout of purkinje cells, internal granular cells and astrocytosis |
|
|
Alcohol increased cancer of the?
|
mouth, larynx, pharynx, esophagus, liver (hepatocellular)
usually squamous Acetaldehyde-DNA adducts have been detected in some tumors |
|
|
Asterixis; Liver Cirrhosis, acute liver disease or both?
|
Both
|
|
|
Spider Angiomas ;Liver Cirrhosis, acute liver disease or both?
In chest, face, neck |
Liver cirrhosis
|
|
|
Jaundice ;Liver Cirrhosis, acute liver disease or both?
|
Both
|
|
|
Hepatomegaly; Liver Cirrhosis, acute liver disease or both?
|
Both
More likely Acute liver disease |
|
|
Caput medusae; Liver Cirrhosis, acute liver disease or both?
|
Cirrhosis and portal HTN
|
|
|
Physical findings of liver cirrhosis
|
Splenomegaly
External hemorrhoids Dupuytren's contracture (claw hand) Palmar erythema Gyno Testicular atrophy Spider angioms Asterixis Hepatomegaly Caput madusae Jaundice |
|
|
Lipase elevation
|
acute pancreatitis
|
|
|
Alcohol increases GERD by
|
Alcohol decreases pressure at lower esophageal sphincter (also nicotine and caffeine)
•Alcohol volume increases intraluminal pressure of stomach (also big meals) •Alcohol makes people lay down-->decreases beneficial effect of gravity (also late-night eating) |
|
|
Primary mech of liver injury d/t alcohol is?
|
oxidative stress
Acetaldehyde leads to accumulation of intracellular proteins, lipids, water, electrolytes, and loss of the structural keratins (CK8/18) |
|
|
Statosis
|
•Enlarged, yellow greasy liver
•Macro- and microvesicular steatosis •Reversible if the patient abstains |
|
|
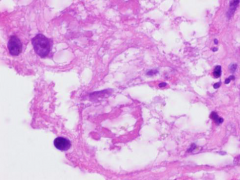
•Ballooning hepatocytes
•Mallory-Denk bodies (Mallory hyaline) –Intermediate filaments and ubiquitin •Pericellular/perivenular fibrosis Neutrophils can go around ballooning hepatocytes |
Steatohepatitis
|
|
|
Ballooning hepatocytes and mallory-denk bodies (condensation of intermediate filaments and ubiquitin; purple ring)
|
|
|
–Associated with insulin resistance, obesity, metabolic syndrome
–Estimated higher prevalence than ALD in the USA |
Non-alcoholic fatty liver disease/NASH
|
|
|
Other than alcohol and NASH what else can cause steatosis
|
•Drugs/toxins (methotrexate, corticosteroids, valproic acid, HAART)
•Kwashiorkor |
|
|
Cirrhosis mechanism
|
•Activated stellate cellsmyofibroblasts
•Chronic injury (>10 years) leads to DIFFUSE bridging fibrosis and regenerative nodule formation (micronodular) •End stage, IRREVERSIBLE, occurs in 10-15% |
|
|
Cirrhosis path consequences
|
–Coagulopathy (decreased production of coagulation factors II, VII, IX, X)
–Hyperestrogenemia (impaired estrogen metabolism) –Jaundice (impaired bilirubin conjugation) –Hypoalbuminemia (loss of synthetic function) •Extracellular matrix deposition and vascular reorganization –Portal hypertension –Encephalopathy –Edema/ascites/hydrothorax |
|
|
Effects of alcohol on the pancreas
|
Increase oxidative stress on acinar cells (direct toxicity),
Increase exocrine secretions, Increase sphincter of Oddi tone, Increaseprotein rich secretions (leads to inspissated secretions and small duct obstruction-->chronic pancreatitis) |
|
|
Mech of acute pancreatitis
Reversible! |
Acinar cell injuryenzyme activation-->autodigestion
–Inappropriate activation of trypsinogen to trypsin Calcium soaps Hemorrhagic fat necrosis Enzymatic digestion of stroma and vasculature |
|
|
Chronic pancreatitis
|
IRREVERSIBLE
Destruction of acini –Inflammation, fibrosis, and calcifications –Late destruction of islets Replaced by fibrous bands |
|
|
Walled off necrotic debris
|
Psuedocyts
|
|
|
Mallory-Weiss Tears
|
•Result of vomiting/retching, associated with alcohol abuse
•Linear tears/lacerations •Usually occur at gastroesophageal junction Present with hematemesis Esophageal rupture-->Boerhaave syndrome |
|
|
Gastric effects of alcohol?
|
acute hemorrhagic gastritis (neutrophilic inflammation) or gastropathy (mucosal injury without inflammation)
•Gastric erosions and ulcers may be present |
|
|
Alcohol withdrawal
|
NO pupil change!!
6-36 hours after last drink Autonomic hyperactivity – tachycardia, hypertension, diaphoresis –Headache –Tremor – fine, high frequency (not like asterixis) –Agitation/anxiety –Abnormal tactile sensations –Nausea |
|
|
Alcohol w/drawal can turn into?
|
Delerium Tremens
•Hallucinations – usually visual and tactile •Disorientation •Hypertension •Tachycardia •Fever •High risk for seizures and dangerous ventricular arrhythmias •2-4 days after the last drink •Untreated mortality – 30% (<5% with treatment) |
|
|
What drug is used to prevent seizures d/t alcohol withdrawal?
|
Benzodiazepine
|
|
|
Naltrexone
|
–Antagonist of opiate receptors
–Pharmacogenetic effect •SNP in exon 1 of mu opiate receptor (A118G) –SNP associated with higher rates of alcoholism –SNP associated with significantly lower relapse during naltrexone treatment Used for Alcoholism |
|
|
Acamprosate
|
–GABA mimetic, possible NMDA antagonist
–Significantly reduces craving of alcohol |
|
|
Dilsulfiram
|
–Blockade of aldehyde dehydrogenase: aversion therapy
–Clinical trial was unsuccessful |
|
|
What parts of the brain are activated in alcoholics
|
Cingulate, insula, and nucleus accumbens
|

