![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
203 Cards in this Set
- Front
- Back
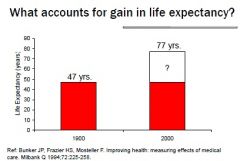
What accounts for gains in life expectancy?
|
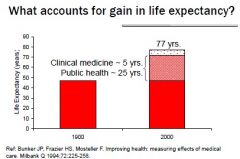
Clinical medicine ~ 5 years
Public Health ~ 25 years |
|
|
Factors Contributing to Gains in Life Expectancy
|
1. Clean water and air
2. Improved sanitation 3. Safer foods, improved nutrition 4. Expanded immunizations 5. Safer environment and workplaces 6. Improved medical care. |
|
|
Preventive Medicine
|
- To protect, promote, maintain health and well-being and prevent disease, disability, and premature death.
- in US, it is its own medical specialty and own Board Certification - The principles of preventive medicine are used in most clinical specialties - The field of Preventive Medicine covers both clinical preventive care and public health. |
|
|
Community vs. Preventive Medicine
(US Perspective) |
Community - promote health in populations thru application of organized community efforts
(Public Health) Preventive - enhances lives of individuals by helping them improve own health (on individual level. What Clinicians do) |
|
|
Community vs. Preventive Medicine
(UK Perspective) |
Integrated approach to Preventive and Community Medicine.
- Branch of medicine concerned with total health of individual, at home and in the community. Applying comprehensive care to prevent and treat illnesses in entire community |
|
|
Public Health Services to Clinicians
|
– Laboratory testing
– Public health surveillance results – Health alerts, e.g., anthrax, influenza – Selected vaccines, antitoxins, etc. – Prevention materials |
|
|
Clinicians' responsibilities to agencies
|
– Public health surveillance reporting
– Completing death certificate – Reporting of suspected child or elder abuse |
|
|
Core Aspects of Preventive Medicine
|
Screening
Counseling Immunization |
|
|
Screening
|
testing in persons without evidence or suspicion of disease to identify early disease or susceptibility when it is more easily / more successfully treated
(secondary prevention) |
|
|
Goals of Preventive Medicine
|
To advance health by
– promoting health-enhancing policies, environments, and behaviors, – preventing disease and injury injury, – making possible early diagnosis and treatment – fostering rehabilitation to minimize disabilities. |
|
|
Primary Prevention
|
prevention of disease by eliminate causes of disease or by increasing resistance to it
- before it happens ie. vaccines Stage of Disease: Pre-disease |
|
|
Secondary Prevention
|
- Early detection and prompt treatment before it becomes symptomatic.
- Treat it before it becomes serious ie. Screening and treatment Stage of Disease: Latent |
|
|
Tertiary Prevention
|
Limitation of impact (eg. disability)
- damage control ie. treatment, disability limitation, rehabilitation Stage of Disease: full swing. Symptomatic |
|
|
Health Promotion
|
- efforts to prevent disease and enhance health in general
- multiple applications (exercise, don't smoke) type of primary prevention |
|
|
Specific Protection
|
- efforts aimed at specific disease, deficiencies, injuries, toxic exposures
ie. get tested for HIV, Don't Drink and Drive |
|
|
Elements of Health Promotion
|
Social Marketing
Counseling Environmental Modification Other Structural changes |
|
|
Social Marketing
|
applications of commercial marketing principles to programs designed to influence behavior and improve personal and societal welfare.
Ie. MADD - mothers against drunk driving Know your numbers - your systolic, diastolic A.B.C. - Abstinence, Be Faithful, Condoms (Strategy for HIV Prevention) (Primary Prevention) |
|
|
Specific Protection
|
Prevention of:
- specific disease (mostly infectious) - specific deficiencies - injuries - toxic exposures - latrogenic disease and injuries |
|
|
Latrogenic
|
Caused by physicians
|
|
|
Nosocomial Infections
|
Hospital-Acquired Infections
- #1 problem = handwashing by healthcare workers |
|
|
Screening
|
Test a healthy population
Goal: to identify disease or susceptibility in it is easier/more successfully treatable - Classifies people as likely or unlikely to have disease. if they are likely referred to → Diagnostic test |
|
|
Diagnostic
|
testing among individuals suspected to have the disease to confirm presence or absence of disease
(secondary) |
|
|
Screen If
|
- Important health problem
- Decent acceptable Test - Available effective early treatments - Based on best available data and unbiased reviews (USPSTF) |
|
|
Criteria for Screening Program: Characteristics of Disease ( A CURE)
|
1. Condition is important public health problem
2. Understanding of natural history of condition (need to know what to look for) 3. Recognizable latent or early symptomatic stage 4. Accepted treatment 5. Early treatment influences course and prognosis of disease (Does catching it early make a difference) |
|
|
Criteria for Screening Program: Characteristics of Screening Test (ASS R&D)
|
Suitable Screening Test or Examination
1. Relatively Sensitive and Specific 2. Detects Disease at Latent or Early symptomatic Stage 3. Simple and Inexpensive 4. Safe 5. Acceptable to Population and Providers |
|
|
Criteria for Screening Program: Health Care System
|
1. Available facilities for diagnosis and treatment
2. Screening costs are economically balanced with possible expenditure on medical care 3. Is the treatment/diagnostic test worse than the disease? 4. Ongoing case-finding. Not one time shot |
|
|
Reliability
|
Findings can be replicated
|
|
|
Validity
|
ability of test to detect who has the disease and who doesn't
|
|
|
True Negative
|
Healthy with normal test
|
|
|
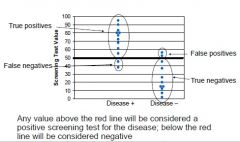
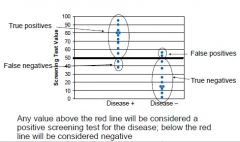
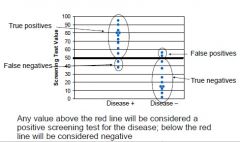
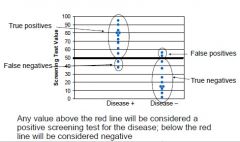
Sensitivity
|
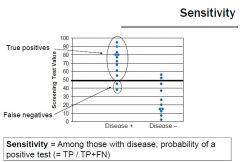
Among those with disease, probability of a positive test
(True Positive / True Positive + False Negative) |
|
|
Specificity
|
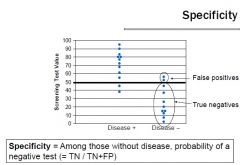
Among those without disease, probability of a negative test
(True Negative / True Negative + False Positive) |
|
|
Screening
|
Test a healthy population
Goal: to identify disease or susceptibility in it is easier/more successfully treatable - Classifies people as likely or unlikely to have disease. if they are likely referred to → Diagnostic test |
|
|
Diagnostic
|
testing among individuals suspected to have the disease to confirm presence or absence of disease
(secondary) |
|
|
Criteria for screening
|
- Important public health problem
- Decent acceptable Test - Available effective early treatments - Based on best available data and unbiased reviews (USPSTF) |
|
|
WHO Criteria for Screening Program: Characteristics of Disease (A CURE)
|
1. Condition is important public health problem
2. Understanding of natural history of condition (need to know what to look for) 3. Recognizable latent or early symptomatic stage 4. Accepted treatment 5. Early treatment influences course and prognosis of disease (Does catching it early make a difference) |
|
|
WHO Criteria for Screening Program: Characteristics of Screening Test (ASS R&D)
|
Suitable Screening Test or Examination
1. Relatively Sensitive and Specific 2. Detects Disease at Latent or Early symptomatic Stage 3. Simple and Inexpensive 4. Safe 5. Acceptable to Population and Providers |
|
|
WHO Criteria for Screening Program: Health Care System
|
1. Available facilities for diagnosis and treatment
2. Screening costs are economically balanced with possible expenditure on medical care 3. Is the treatment/diagnostic test worse than the disease? 4. Ongoing case-finding. Not one time shot |
|
|
Reliability
|
Findings can be replicated
|
|
|
Validity
|
ability of test to detect who has the disease and who doesn't
|
|
|
True Positive
|
Sick with abnormal test
|
|
|
False Positive
|
Health person with abnormal test
|
|
|
False Negative
|
Sick with a normal test
|
|
|
How does Prevalence affect Predictive Value of Positive Test
|
If ↑ Prevalence, ↑ Predictive Value of Positive Test
↓ Prevalence, ↓ Predictive Value of Positive Test |
|
|
Who makes recommendation on Screening?
|
US Preventive Services Task Force
- independent panel of private sector experts in primary care and prevention - Recommendations are "the gold standard" - Evidence Based recommendations |
|
|
Prophylaxis
|
medical or public health procedure to prevent, rather than cure of treat a disease
(Primary Prevention) |
|
|
Chemoprophylaxis
|
administer drug for purpose of preventing disease or infection
ie. Anti-malarial, Antibiotics prior to surgery, Aspirin, Vaccines |
|
|
What is the only disease to be eradicated worldwide?
|
Smallpox
|
|
|
Vaccine
|
biologically derived substance that elicits a protective immune response when administered to susceptible host
|
|
|
Vaccination
|
administration of vaccine
|
|
|
Immunization
|
Development of immunity of vaccine (your body's response to the vaccine → making antibodies)
|
|
|
Antigen
|
Substance that stimulates immune response
ie. production of antibodies eg. toxins, microorganism, foreign blood cells |
|
|
Antibody (immunoglobulin)
|
Protein produced by B Lympocytes in response to antigen stimulus
- destroys foreign substances |
|
|
Immunological Memory
|
After exposure to antigen, specific memory B cells circulate are able to antibodies upon re-exposure
- Don't need to be exact. ie. Cowpox vaccine was good for smallpox |
|
|
Vaccine Preventable Rash Illnesses
|
- Chickenpox/Varicella
- Measles - Rubella |
|
|
Vaccine Preventable Childhood Disease
|
- Mumps
- Diphtheria - Pertussis (Whooping Cough) |
|
|
Vaccine Preventable Neuromuscular Disease
|
- Polio
- Tetanus |
|
|
Passive Immunity
|
- immunity products (antibodies) given to a person, rather than producing it themselves
- Short Term = body breaks down the proteins - EG. maternal antibodies in milk or across placenta - Immune globulin (immune blood) - Hyperimmune globulin - specialized blood with specific antibodies - Antitoxins (antibodies formed in response to poisonous substances. usually made from horses) - Anti-venoms |
|
|
Active Immunity
|
- Producing antibodies from your own immune system
- Long lasting |
|
|
Live Attenuated Vaccine
|
- live virus that is weakened in a lab (by physical or chemical processes) so it will elicit an immune response without causing the clinical disease
- must replicate in host to be effective - needs to stay cold (maintain cold chain) - culture viruses so they become accustomed to the lab environments and evolve away from human body - Interference from circulating antibodies - need fewer doses - Rare: can convert back to virulent strain (OPV-associated Polio in Dominican Republic) e.g. influenza / measles / mumps / rubella / yellow fever / BCG / **oral Polio ** ** if not handled carefully, may revert back to virulent strain -> OPV ** |
|
|
BCG
|
Live attenuated vaccine
- made from cow form of Tuberculosis - Not used in US/Canada - will test positive for TB Skin Test |
|
|
Inactivated Vaccines
|
- Inactivated by heat or chemicals
- Cannot replicate or revert - Not as effective as Live-attenuated vaccines - Less interference from circulating antibody than live vaccines - Fewer side effects (localized, if any) - Requires 3-5 doses - Immune response usually humeral - Antibody may dimish over time, requiring boosters e.g. HepA / polio / rabies / HepB / HPV / cholera / anthrax / plague / tetanus ** may be given as whole OR fractional (protein or sugar based) ** |
|
|
Inactivated Polio Vaccine (IPV)
|
- Given by Intramuscular injection
- Can be used for immunocompromised persons - Used in U.S., Canada, UK - Very low risk of getting polio |
|
|
Live Attenuated Oral Polio Vaccine (OPV)
|
- Given orally - on a sugar cube
- no health professional needed (Cheap, Easy) - Provides longer lasting immunity than IPV - Used in developing countries - can lead to Vaccine-induced polio |
|
|
Combination Vaccine
|
- Combination of two or more vaccines
ie. Diphyheria/tetanus/Pertussis (whooping Cough) |
|
|
conjugate vaccine
|
Vaccine in which a polysaccharide antigen is chemically joined with a protein molecule to improve immunogenicity of polysaccharide
|
|
|
Adjuvant
|
- substance that is used in vaccine to improve the immune response so that less vaccine is needed to produced a non-specific stimulator of the immune response
|
|
|
Polysaccharide Vaccine
|
- not consistent in children <2 years of age
- No booster response - Antibody with less functional activity - Immunogenically improved by conjugation to a protein - ie. Meningococcal and pneumococcal |
|
|
Recombinant Vaccine
|
- Genetic modified organism to make live attenuated or inactivated vaccines
- Insert antigen-producing gene into yeast to produce large quantities of antigen - Delete or modify pathogenicity (rotavirus) |
|
|
WHO Vaccines Recommended for Children
|
- DTP (Dipheria, Tetanus, Pertussis)
- Hepatitis B - Haemophilus influenzae type B (HIB) - Human Papillomavirus (HPV) - Measles or MMr -Pneumococcal (Conjugate) - Oral Polio Vaccine (Live) - BCG, Japanese Encephalitis, Yellow Fever |
|
|
US Vaccines Recommended for Children
|
- Hepatitis B
- Haemophilus influenzae type B (HIB) - Human Papillomavirus (HPV) - Measles or MMr -Pneumococcal (Conjugate) Differences from WHO recommended - DTaP (Dipheria, Tetanus, acellular form of pertussis) - Inactivated Polio Vaccine (Live) - (no BCG, Japanese Encephalitis, Yellow Fever) + Varicella +Influenza + Rotavirus + Hepatitis A |
|
|
Vaccines recommended for adolescents (11-12 yrs old)
|
- Meningococcal (MCV4)
- Booster against Tetanus, Diphtheria, Pertussis (Tdap) - Human Papillomavirus (for girls) - Influenza (annual) |
|
|
Vaccines Recommended for Adults
|
- Catch up on HPV, MCV, VZ, MMR
- Every 10 years - Booster agains Td or Tdap Annually - Influenza Age 60 years - Zoster Age 65 - Pnemococcal (polysaccharide) |
|
|
Vaccines Recommended for Healthcare workers
|
- Hepatitis B
- Influenza (annually) - Measles, Mumps, Rubella* - Varicella* Tetanus, Diphtheria, Pertussis Meningococcal (only for microbiologists - only if no evidence of immunity |
|
|
Uses for a Death Certificate
|
1. Burial Permit
2. Settlement of Deceased Estate 3. Life Insurance Claim 4. Obtain Death Benefits 5. Termination of Govt services or obligations 6. Closure, Peace of mind ie. determine official cause of death. - Michael Jackson (homicide) vs. Heath Ledger (OD) |
|
|
Physician's responsibility in signing death certificate
|
- legal document
- (Liberace was gay, had AIDs but doctor wrote down pneumonia -> lost license) - Must be familiar with state/local regulations regarding medical certifications - complete relevant portion of death certificate - deliver death certificate to funeral director answer questions from state or local registrar if asked -provide supplemental report if autopsy reveal different cause of death |
|
|
What level of government can modify the death certificate outline?
|
States
|
|
|
Who signs the death certificate
|
Physician and Funeral Director
|
|
|
Why is a death certificate important in public health?
|
- Characterize and access general health of population
-Target and measures results of interventions - Follow up on infant, maternal, and other deaths -Calculate life expectancy |
|
|
What is included in the "Cause of Death Section" of a death certificate?
|
1. Sequence of Events leading up to death
- Immediate Cause (not mode of death - ie. cardiac arrest/respiratory arrest) - As A Consequence of - Other Significant Conditions 2. Underlying cause of death (Disease or injury that initiated events resulting in death listed LAST) 3. Only one cause per line 4. Duration of each |
|
|
What is an ICD code is used for?
|
ICD = International Classification of Diseases
- Published by WHO - Codes for every cause of death worldwide |
|
|
Nosologist
|
someone who is an expert at ICD Codes
|
|
|
What are the most common causes of death?
|
1. Heart Disease
2. Cancer 3. Stroke Same in Caribbean, UK and US |
|
|
The top 3 causes of death can be attributed to what?
|
Behaviors.
1. Tobacco 2. Poor Diet/Non-Activity 3. Alcohol |
|
|
Death (Mortality) Rate
|
Frequency of death in a defined population during a specified period of time
|
|
|
Crude Death Rate
|

NOTE: Grenada has a lower mortality rate because younger population
|
|
|
Cause Specific Death Rate
|
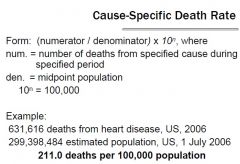
|
|
|
Age-Specific Death Rate
|
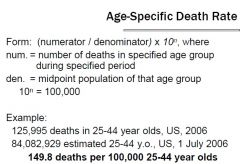
|
|
|
Infant Mortality Rate
|
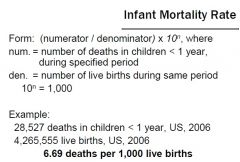
Used around the world to measure health and healthcare
U.S. = 43rd in the world. Cuba = above us. |
|
|
How to Deliver Prevention in the Clinical Setting? (5 A's)
|
1. Assess/Ask - about behavior risk and factors affecting those behaviors
2. Advise - give personalized, clear, specific advice on behavior change. talk about harms/benefits. 3. Agree - work with the patient to find things they are willing to do to change their behavior. 4. Assist - support the patient in achieving the agreed upon behavioral changes. 5. Arrange - schedule on-going follow ups. check their progress. adjust treatment as needed. |
|
|
What has the greatest potential of decreasing morbidity/mortality?
|
Changing Behaviors:
esp. 1. Smoking 2. Exercise 3. Alcohol |
|
|
What 3 Behaviors are linked to the most mortality?
|
1. Smoking
2. Not enough Exercise/Poor Diet 3. Alcohol Abuse ... 4. Illicit Drug Use 5. Risky Sexual behaviors |
|
|
Health risk profiles
|
are tools to help office staff and clinicians identify whether age, gender, or health-related behaviors put the patient at risk for cardiovascular disease, diabetes, certain types of cancer, certain infectious diseases, and other conditions.
The identification of risk factors guides the clinician in deciding which screenings, immunizations, patient education, and follow-up to provide each patient. ie. RealAge.com (The HRP is not a patient health history. |
|
|
Transtheoretical Model
(Stages of Change Model) |
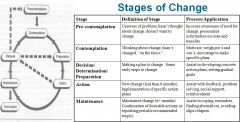
Note: Relapse is often a natural part of the change process, and can happen at any point along the continuum
1. Change is a process that takes time 2. Patients may benefit from different messages, depending upon where they are |
|
|
Ready (for change)
|
Recognition on the part of the individual that there is a need to make the desired behavior change and that he or she is mentally prepared to attempt the behavior change.
|
|
|
Willing (for change)
|
The strong desire and the decision of an individual to make the behavior change.
|
|
|
Able (for change)
|
The actual ability and confidence an individual has about his or her potential to accomplish the desired behavior change and the commitment and planning to make it happen.
|
|
|
Motivational Interviewing
|
Definition:
A directive, patient-centered counseling style - enhances motivation for change by helping patients clarify - resolve ambivalence about behavior change. Goal: To identify and resolve discrepancies between current behavior and broader values and goals. |
|
|
3 Components of Motivational Interviewing
|
Collaboration – working together with patients in a partnership
Evocation – eliciting thoughts and feelings from patients about what they want and need Autonomy – respecting the patient’s ability and right to make his or her own decisions about health behaviors. |
|
|
4 Principles of Motivational Interviewing
|
Express Empathy -
Support Self-Efficacy - a client's belief that change is possible is an important motivator to succeeding in making a change Roll with Resistance - accept setbacks. don't let it get you off the bandwagon. Develop Discrepancy - a discrepancy between where they are and where they want to be |
|
|
Advice on behavioral changes need to be:
|
1. Clear
2. Personalized 3. Strong |
|
|
Purposes of Public Health Surveillance
|
To portray the ongoing pattern of health-related states and events, to
- Assess public health status - Trigger public health action (ie. Swine Flu) - Define public health priorities - Evaluate Programs |
|
|
Health Insurance Portability and Accountability Act (HIPAA)
|
- protects the privacy of individually identifiable health info
- regulates how health plans, hospitals, docs, use and disclose individually identifiable health info - specifically does not interfere with state public health reporting, investigations, interventions |
|
|
WHO's Quarantine-able Diseases
|
- small pox
- poliomyelitis (wild-type) - human influenza caused by new subtype (ie. avian flu, swine flu) - severe acute respiratory syndrome (SARS) Unexpected or “impactful” cases of - cholera – pneumonic plague – yellow fever – viral hemorrhagic fevers – West Nile fever – diseases of regional concern, e.g., dengue, rift valley fever, meningococcal disease - Any event of potential international PH concern |
|
|
What data must be reported? (if found with a flagged diseased)
|
- Identifying info (name, address, phone)
- Demographic info (age, sex, occupation) - Clinical info (disease, date of onset, lab results) - Epidemiological info (usually disease specific risk factors) - Reporter info (name of doctor, facility) +/- Contact info |
|
|
Process of Public Health Surveillance
|
1. Data Collection – PCP, hospital, etc.
2. Data Tabulation/Analysis – descriptive/analytic/by place 3. Data Interpretation – crosses epidemic threshold 4. Data Dissemination – to those who need to know 5. Link to Action – case investigation/disease control/development of policies |
|
|
Uses of Public Health Surveillance
|
1. Describe the burden of or potential for disease
2. Monitor trends and patterns in disease, risk factors, agents 3. Detect sudden changes in disease occurrence and distribution 4. Provide data for program, policies, priorities 5. Evaluate prevention/control efforts |
|
|
Do physicians need informed consent to report data?
|
No, they don't need informed consent or notification of patients, even if sensitive info
|
|
|
Health Agencies uses info to
|
1. monitor health of community
2. feed info back to clinicians about: - current trends in disease occurrence - antibiotic resistance - treatment - prevention |
|
|
Other than disease, what do physicians need to report?
|
- Impaired driving (DUIs)
- Abuse (child abuse, elder abuse, rape) - Injuries (from weapons, crimes) - Burns over 5% of the body |
|
|
What does the ap in DTap stand for?
|
ap = acellular Pertussis vaccine. (reduced dose - doesn't use the whole cell. only parts of the cell)
both DTap and DTP are inactivated vaccines. |
|
|
10 Great Achievements in Public Health:
|
1. Vaccination
2. Motor-Vehicle Safety 3. Control of Infectious Disease 4. Decline of CHD and Stroke 5. Safer/Healthier Foods 6. Safer Work Places 7. Healthier mothers/babies 8. Family planning 9. Fluoridation of drinking water 10. Recognition of tobacco use as health hazard |
|
|
Healthy People 2010
|
U.S. National Prevention Initiative
2 overachieving goals: 1. Increase quality of years of healthy life 2. Eliminate health disparities |
|
|
What is different about prevention services?
|
- Future oriented
- lag time between program & health effects - program for all regardless of need - program usually in absence of medical crisis - quality of life: current participation vs. future benefits |
|
|
Describe the goals of preventative medicine
|
- To advance health by promoting health enhancing policies, environments, & behaviors
- Preventing disease & injury - Making possible early diagnosis & treatment - Fostering rehabilitation to minimize disabilities |
|
|
Isolation vs. Quarantine vs. Social Distancing
|
Isolation - separation/restriction of movement of persons who are ILL
Quarantine - separation/restriction of movement of persons who are NOT ILL (asymptomatic but may be exposed) Social Distancing - prohibit large groups gathering. |
|
|
WHO Prerequisites for successful screening program:
|
1. Condition is important public health problem
2. Decent acceptable test 3. Available effective early treatment based on the best available data and unbiased review |
|
|
Describe the attributes of a good screening test
|
- Relatively sensitive & specific
- Detects disease at latent or early symptomatic stage - Safe - Simple and inexpensive - Acceptable to population and providers |
|
|
Predictive value positive (PVP)
|
– among those testing +ve, prob. of actually having disease (= TP / TP + FP)
|
|
|
Predictive value negative (PVN)
|
among those testing -ve, prob. of not having disease (= TN / TN + FN)
|
|
|
List 5 sources of screening recommendations
|
1. Government agencies
2. Panels convened by government agencies 3. Medical specialty associations 4. Special interest organizations 5. Individual experts |
|
|
Assess
|
ask about behavior health risks and factors affecting choice of behavior change goals
|
|
|
Advise
|
give clear, specific, & personalized behavior change advice, including information about personal health harms/benefits (express empathy/support self-efficacy / roll with resistance)
|
|
|
Agree
|
collaboratively select appropriate treatments goals & methods based on patient’s interest & willingness to change the behavior
|
|
|
Assist
|
using behavior change techniques to aid the patient in achieving agreed-upon goals by acquiring the skills, confidence, and social/environment supports for behavior change
|
|
|
Arrange
|
schedule follow-up contacts to provide ongoing assistance/support and to adjust the treatment plan as needed, including referral to more intensive or specialized treatment
|
|
|
Pre-contemplation
|
unaware of problem / increase awareness of need for change
|
|
|
Contemplation
|
thinking about change but hasn’t / motivate, weight pro’s and con’s
|
|
|
Decision
|
making a plan to change / assist in developing concrete action plans
|
|
|
Action
|
new change or implementation of specific action plan / assist with feedback, problem solve
|
|
|
Maintenance
|
maintained change / assist in coping, reminders, avoiding relapse
|
|
|
Naked DNA
|
antigen-producing gene injected, incorporates host DNA -> produce antigen
--- Edible vaccines or skin-patch vaccines --- vaccines against HIV, TB, Malaria, HSV, other STDs --- more combination vaccines (MMR + VZV) |
|
|
Occupational Hazards:
|
1. Physical: awkward posture, prolonged static posture, high repetition, vibration, noise, temp extremes
2. Chemical: toxins, asphyxiates, mutagens, teratogen (effects group of cells), carcinogens 3. Biological: viral infections agents (AIDS, SARS), vector-borne diseases (malaria, dengue fever) 4. Safety: struck by, caught in, struck against, fall from 5. Psychosocial: stress, organization structure, shift work |
|
|
Occupational Health
|
multidisciplinary approach to the
- recognition - diagnosis, - treatment, - prevention - control of work-related diseases, injuries, & other conditions |
|
|
5 Key Parts of Occupational History: Questions to ask patient
|
1. Description of all jobs held
2. Work exposure history 3. Timing of symptoms in relation to work 4. Epidemiology of symptoms or illness among coworker 5. Non-occupational exposures and other factors |
|
|
Initiating Preventative Action:
|
1. Advise the patient
2. Contact the patient’s union or other labor org. 3. Contact the patient’s employer 4. Inform the appropriate gov. authority 5. Contact appropriate research/expert group |
|
|
Death Certificate:
Part I Line (a) Immediate Cause |
- final disease, injury, or complication directly causing death
- NOT mode of dying or terminal event - Cannot be left blank - List duration - if immediate cause due to complication/error in medical/surgical treatment, report complication or error, procedure and condition being treated |
|
|
Death Certificate:
Part I Line (b) Due to (or as a consequence of) |
- Report any disease, injury, or complication that gave rise to or prepared way for cause of death
- Underlying cause of death should be listed LAST - If immediate cause arose as complication of/error in medical treatment, report complication or error, procedure, and condition being treated |
|
|
What are the 3 subspecialties of Preventive Medicine?
|
- Public health and general preventive medicine
- Occupational Medicine - Aerospace Medicine |
|
|
Food Fortification Against Dental Caries?
|
Fluoride in water
|
|
|
Food Fortification against rickets?
|
Vitamin D in milk
|
|
|
Food fortification against neural tube defects?
|
folic acid in cereal grain products
|
|
|
Food fortification against goiter?
|
iodine in salt
|
|
|
What are the interventions used to reduce the risk of diabetes or its complications?
|
1. Screening using fasting plasma glucose (II°)
2. Measurement of glycosolated hemoglobin (HbA1c) every 3–4 months in diabetic patients (III°) 3. Counseling obese non-diabetic patient to lose weight (I°) 4. Annual eye exam in diabetic patients to look for diabetic retinopathy (III°) |
|
|
Diagnosis
|
testing among individuals suspected to have the disease to confirm presence or absence of disease
|
|
|
Consequences of false-positive test result
|
– Unnecessary follow-up tests
(inconvenience, morbidity, expense) – Labeling, anxiety – Over-treatment of questionable abnormalities – Fear of future tests |
|
|
Consequences of false-negative test result
|
– Delayed diagnosis, more advanced disease,
premature death / disability – Disregard of early signs / symptoms – False reassurance – Exposure of others to infection |
|
|
Is smoking and intravenous drug use listed as Part I or Part II on a death certificate?
|
Part II.
- Smoking is a RISK FACTOR for bronchitis, emphysema, lung cancer. - Intravenous drug use is a RISK FACTOR for HIV and Hepatitis B |
|
|
Is alcohol abuse listed as Part I or Part II on a death certificate?
|
Part I.
Alcohol abuse is the CAUSE of Alcoholic Cirrhosis |
|
|
What is the importance of reporting Part II on a death certificate?
|
1. Report conditions that co-existed or pre-existed AND contributed to death
2. Report conditions that resulted from underlying cause of death and contributed to death, but was parallel to the immediate cause of death. 3. To report risk factors (ie. smoking, intravenous drug use) |
|
|
What is the single most used measure to measure health around the world?
|
Infant Mortality Rate
= measure deaths in children under 1 year. - not all countries measure death rate. But all countries Infant Mortality. |
|
|
Where is the U.S. ranked for infant mortality? How do we compare to other countries?
|

43rd - infant mortality rate = 6.4
- we are below Cuba (41st, 6.1) Good = below 5. UK (29th, 5.0) Canada (24th, 4.6) Developing country = in teens and 20s not bad. BAD = above 50. Pakistan = 68.5 Afghanistan = 157.4 Infant mortality rate = deaths per 1000 live births |
|
|
What is a "good" infant mortality rate for a developing country? What is a "bad" infant mortality rate for a developing country?
|
Developing country =
Good = 10-20s 91. Grenada = 13.9 134. Trinidad & Tobago = 24.3 152. Guyana = 31.4 BAD = above 50. 194. Pakistan = 68.5 226. Afghanistan = 157.4 228. Angola = 184.4 Infant mortality rate = deaths per 1000 live births |
|
|
What is a "good" infant mortality rate for a developed country?
|
5.0
UK = 29th with 5.0 Canada = 24th with 4.5 Singapore = 1st with 2.3 Infant mortality rate = deaths per 1000 live births |
|
|
Where does the data for mortality rates come from?
|
Death certificates
|
|
|
Describe the authority that physicians report reputable diseases to. What do they report?
|
Authority = States or Province (Canada)
- Physican/Hospital => Local Health Agency - Local health agency will do investigation, action if necessary. - Local health agency forwards up to state. - Mostly communicable diseases, animal bite, occupational illness, others - Every other state has similar request - Some states specify penalty for failing to report, some do not |
|
|
Health is a ____________ rights issue.
(Level of Govt) |
State's
ie. federal govt (CDC) has to ask permission to enter a state to investigate |
|
|
Thyrotoxicosis
|
Overactive thyroid from elevated levels of
- thyroxine (T4) - triiodothyronine (T3) - or both - more common in women than men Symptoms: - rapid pulse, weight loss, palpitations, heat intolerance, tremors, moist skin |
|
|
Endemic
|
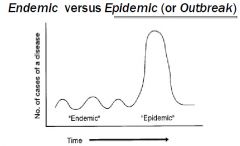
The amount of disease that is normally present in a community.
|
|
|
Epidemic
|
Amount of disease greater than expected number.
-over a particular period of time |
|
|
Role of clinician in an outbreak investigation
|
– see and diagnose patients
– report cases to health department – provide medical records as needed to – health department investigators – incorporate health department alerts, findings, etc. into his/her clinical practice |
|
|
What is the importance of comparison (control) in analytical studies?
|
Need a control group. Just because something is common doesn't mean it is the culprit.
ie. how many people drink water? how many of them breathe the air? Need a control group to infer causation. |
|
|
Odds Ratio
|
compares exposure and illness.
Odds ratio of 1 = no diff between control and diseased. No association. Odds ratio below 1 = protective. prevents you from getting the disease Odds ratio of above 1 = bad for you. causes the disease. |
|
|
Outbreak
|
An epidemic limited to localized increase in the incidence of disease
(eg. village, town) |
|
|
Describe the approach and list the key steps of an outbreak investigation
|
1. Confirm existence of an outbreak: endemic v. epidemic / outbreak v. epidemic
Epidemic: occurrence of more cases of disease than expected in a given area or among a specific group of people over a particular period of time Outbreak: an epidemic limited to localized increase in the incidence of disease 2. Verify the diagnosis (need field investigation?) – rule out lab error/review med record 3. Prepare for field work 4. Construct a working case definition – loose (sensitive) versus tight (specific) case def. Categories of certainty: e.g. confirmed, probable, possible 5. Find cases systematically and record information – try to identify all cases / collect data on case-patients / create line listing 6. Perform descriptive epidemiology – time, place, person, “person data” (transmission method) 7. Develop Hypotheses – subject matter knowledge / review / outliers / talk to patients 8. Evaluate Hypotheses epidemiologically – key = comparison group 9. Refine Hypotheses and execute additional studies as necessary 10. Reconcile with lab/environmental studies 11. Implement control / prevention measures – the earlier, the better! - create mechanisms to evaluate both short and long-term effectiveness of control 12. Initiate or maintain surveillance – monitor for additional cases/evaluate effectiveness of control 13. Communicate findings – legal documentation / justify recommendations |
|
|
Risk Factors for Diabetes
|
- obesity
- poor diet and physical activity - family history and genetics - history of gestational diabetes - impaired glucose metabolism - Dyslipidemia (elevated lipids in blood) - History of gestational diabetes (or baby > 9 lbs) - race/ethnicity (African American, Asian American, Pacific Island, Hispanic/Latinos) |
|
|
Secondary Prevention for Diabetes
|
SCREEN adults who are overweight (BMI > 25) and have at least one risk factor:
- physical inactivity - 1st degree relative with diabetes - members of high risk popn (Black, Hispanic, Asian, Native American, Pacific Islander) - Women who delivered a baby >9 lbs or diagnosed with gestational diabetes - Hypertension (>140/90) - HDL < 35 and TG > 250 |
|
|
Gestational Diabetes
|
diagnosed glucose intolerance during pregnancy
frequently diagnosed in: - obese pregnant women - Pregnant Black, Hispanic, Native Americans - requires treatment to normalize in infants - 5-10% will develop type 2 soon after pregnancy -40-60% will develop type 2 within 5-10 years post delivery |
|
|
1-5% of diagnosed diabetes results from:
|
- genetic conditions
- surgery - drugs - malnutrition - infections - pancreatic disorders |
|
|
Impaired Fasting Glucose (IFG) - Pre-Diabetes
|
condition where fasting blood glucose is elevated (100-125 mg per dL) after an overnight fast
|
|
|
Impaired Glucose Tolerance (IGT)
- Pre-Diabetes |
condition where fasting blood glucose is elevated (149-199 mg per dL) after a 2 hour oral glucose tolerance test
|
|
|
Tertiary Prevention for Diabetes
|
Screen person with diabetes for:
- yearly eye exam - Periodic foot exam - HbA1c levels - Psychosocial assessment Vaccination - influenza, pneumococcal Exercise, Diet counseling (Damage Control) |
|
|
Complications of Diabetes
|
- Heart Disease and Stroke
- High Blood Pressure - Blindness - Kidney Disease - Nervous system neuropathy (impaired sensation to hands, feet, slow digestion of food in stomach, erectile dysfunction, carpal tunnel) - Amputations - Dental disease (Periodontal Gum disease) - Pregnancy Problems - Susceptibility to Infection |
|
|
metformin
|
- Diabetes Prevention Program
- reduced risk of getting diabetes - most effective in younger and more overweight people (25-40 years and 50-80 lbs overweight) |
|
|
acarbose
|
STOP-NIDDM Trial
- treatment of people with Impaired Glucose Tolerance (IGT) - reduced risk of developing diabetes by 25% - lifestyle changes and medication works to bring it back to normal glucose tolerance |
|
|
Antigen "drift"
|
minor mutations in flu virus
ie. point mutation |
|
|
Antigenic "shift"
|
larger immunological change (reassortment) of flu virus
-new virus subtype - ie. genetic reassortment (human and animal viruses) or direct animal (poultry) to human transmission |
|
|
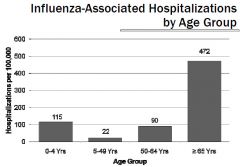
What does H stand for in H1N1?
|
Hemagglutinin - surface antigens (glycoproteins)
-protein that allows virus to attach to respiratory cells. |
|
|
What does N stand for in H1N1?
|
Neuraminidase - surface antigens (glycoproteins)
- helps release newly formed virons from infected cell. |
|
|
Pandemic
|
epidemic occurring in multiple continents
Requirements: 1. A new influenza type A subtype 2. Causes serious illness 3. Spreads easily from human-to-human |
|
|
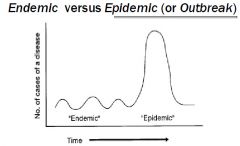
Influenza has what "shaped pattern" for hospitalizations and death?
|
J-Shaped Pattern. Mostly young children and elderly (65+) affected.
|
|
|
What are the 2 types of influenza virus? What are the hosts for each?
|
Type B. is very mild.
Type A is very virulent |
|
|
What is the distribution of Influenza A subtypes in humans, swine, horses, and birds?
|
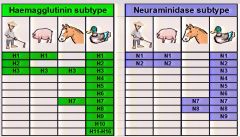
Birds can host all subtypes. Humans only have H1-3, N1-2
|
|
|
H5N1
|
Avian flu
- very lethal but not very contagious - need direct contact with birds - 60% mortality rate - No J-shaped curved. mostly <40 year olds. - wild birds - carriers - domestic birds - affected |
|
|
panzootic
|
pandemic in animals
|
|
|
What is the best way to not get the flu?
|
get vaccinated
|
|
|
Describe the flu vaccines
|
- WHO meets twice a year to decide
- Influenza is very specific = need to decide what strains to make vaccines against - Northern hemisphere - makes it in spring for following season Typical vaccine - trivalent (Type A: H1N1, H3N2, and Type B) 6-8 months to make it - inactivated for intramuscular - live attenuated nasal spray |
|
|
What is the current concern over avian influenza (H5N1) and swine flu (H1N1)?
|
The concern is there will be a strain with:
- contagiousness of H1N1 - deadliness of H5N1 (ie. 1918 Pandemic) |
|
|
What is the difference between the seasonal flu and the outbreaks of influenza?
|
Seasonal Influenza
- in the Fall - Contagious but not deadly - J-shaped curve (very young and elderly) Novel Influenza- - In Spring, - deadly but not contagious - affects mostly young people. no J-shaped curve |
|
|
H1N1
|
Swine Flu
- 8 genes (avian, human, swine) - contagious (human to human transmission) - does not cause severe disease - 1.1% mortality rate (most death had underlying conditions) - no vaccine yet - Antivirals available - but have side-effects. shorten duration of illness by 1 day - Mostly affects younger people <40 year olds |
|
|
CH2OPD2
|
Taking an Environmental Exposure History?
1. Community 2. Home 3. Hobbies 4. Occupation 5. Personal Habits 6. Diet 7. Drugs |
|
|
Occupational Exposure
|
1. Jobs and Tasks
2. Exposures (Physical, Chemical, Biological, Psychosocial) 3. Protection. |
|
|
What are the modifiable risk factors for heart disease?
|
- high blood pressure
- high cholesterol - smoking - obesity - diabetes - physical inactivity |
|
|
Risk factors for Coronary Heart Disease?
|
1. Cigarette Smoking
2. Overweight and Obesity 3. Hypertension 4. Dyslipidemia 5. Diabetes Mellitus +Male Sex (Gender) +Increasing age (>55 for men, >65 for women) +family history of CHD (men <55, women <65) +diet and nutrition |
|
|
Novel Risk factors for Coronary Heart Disease
|
1. Excess homocysteine in Blood
2. Inflammatory markers (C-reactive protein) 3. Abnormal blood coagulation (elevated levels of fibrinogen) |
|
|
Non-modifiable risk factors for CHD
|
- Increasing Age
- Heredity or family history - Gender - Ethnicity or Race (Low socioeconomic status) |
|
|
Lesser Modifiable Risk Factors
|
- Mental Ill Health (Depression)
- Psychosocial Stress - Heavy Alcohol Use - Use of Certain Medications - Lipoprotein A |
|
|
Primary Prevention for Coronary Heart Disease
|
- Maintain healthy lifestyle
- Exercise - Healthy Diet - Regular Exercise - Normal weight - Non-smoking - Control of Stress |
|
|
Secondary Prevention of Coronary Heart Disease
|
Screening (Early Detection) and treatment of symptomatic patients.
- medication to lower blood pressure |
|
|
Tertiary Prevention for Coronary Heart Disease
|
- Beta Blockers
- Stop Smoking - Treat for hyperlipidemia - Recommend low dose aspirin - ACE inhibitors - Revacularization (bypass surgery) - Thrombolytic drugs - Heart transplant |
|
|
Community Intervention for Coronary Heart Disease
|
- Organization based fitness and diet control
- Marketing healthy practices - Integration of traditional healing practices - Expanded clinic-based fitness and diet control interventions |
|
|
What are interventions used to reduce the risk of heart disease?
|
- Restricting sale of cigarettes to minors (I)
- Avaliabilty of playgrounds, sports, recreation (I) - Screening for hypertension (II) - Exercise Treadmill Test for ppl with diabetes and 3 other risk factors (II) - Daily Aspirin after having myocardial infarction (III) |
|
|
What are interventions used to reduce the risk of diabetes?
|
- Counseling obese patients about weight loss (I)
- Screening using fasting plasma glucose (II) - Measurement of glycosolated hemoglobin (HbA1c) (III) - Annual eye exam for diabetic retinopathy (III) |
|
|
Expected consequences of screening
|
True Positive Result
- early diagnosis - early (possibly less radical) treatment - reduce morbidity, mortality, disability - reduced cost - "labeling effect" True Negative Result - Reassurance |

