![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
131 Cards in this Set
- Front
- Back
|
what is tx for basal cell ca of anal margin? |
Basal cell carcinoma of the anal margin is appropriately treated with WLE.
|
|
|
Pt presents c/ anal mass
-Bx shows cloacogenic cancer -Next step = _ |
Cloacogenic anal ca:
-variant of sq cell ca -Tx = same as sq cell: chemo 1st line - Nigro protocol = 5-FU + mitomycin + XRT -If inguinal adnopathy, get FNA beforehand -> extend radiation field if (+) -80% cure rate -Persistant or recurrent ca => APR |
|
|
pt diagnosed c/ sq cell anal ca below dentate line.
What is the tx? |
Anal cancer below dentate line - better prognosis than above:
-Sq: WLE if <3 cm, 0.5 cm margin. APR otherwise. +/- inguinal LN dissection -Basal cell: WLE usually sufficient. APR if sphincter involved -Bowen's dz (malignant): intraepidernal sq cell. WLE. many develop primary internal malignancies, skin cancer -Paget's dz (rare)L: intraepidermal apocrine gland ca. Slow growing. PAS (+). WLE +/- groin dissection. Many develop rectal or colon ca. |
|
|
A 60-year-old man has rectal pain and a tender 2-cm mass at the anal canal. Sigmoidoscopy shows normal rectosigmoid mucosa. Biopsy of the mass shows squamous cell carcinoma of the anus. The most appropriate management is
|
Anal canal = above dentate line, so Tx = Nigro protocol = 5-FU + mitocycin + XRT
(sq cell ca below dentate line treated surgically) |
|
|
Initial tx for anal fissure = _
|
Anal fissure;
-Caused by split in anoderm -90% in posterior midline. 73% intersphincteric, 23% transspincteric -Pain, bleeding c/ defecation. -Chronic fissures have sentinel pile -Tx: Sitz baths, bulk, lidocaine jelly, stool softener, nitrate paste -Surgery: lateral subcutaneous internal sphincterotomy -Biggest complication from surgery = fecal incontinence -NO surgery if pt has UC or Crohn's -Lateral or recurrent fissures => suspect Crohn's > anal cancer (UC doesn't involve anus) |
|
|
50M c/o pain c/ defecation, blood streaks c/ BM.
-Anosocopy shows piled-up anoderm in posterior midline -tx = _ |
Anal fissure;
-Caused by split in anoderm -90% in posterior midline. 73% intersphincteric, 23% transspincteric -Pain, bleeding c/ defecation. -Chronic fissures have sentinel pile -Tx: Sitz baths, bulk, lidocaine jelly, stool softener, nitrate paste -Surgery: lateral subcutaneous internal sphincterotomy -Biggest complication from surgery = fecal incontinence -NO surgery if pt has UC or Crohn's -Lateral or recurrent fissures => suspect Crohn's > anal cancer (UC doesn't involve anus) |
|
|
Tx for anal fissue refractory to medical mgmt
|
Anal fissure;
-Caused by split in anoderm -90% in posterior midline. 73% intersphincteric, 23% transspincteric -Pain, bleeding c/ defecation. -Chronic fissures have sentinel pile -Tx: Sitz baths, bulk, lidocaine jelly, stool softener, nitrate paste -Surgery: lateral subcutaneous internal sphincterotomy -Biggest complication from surgery = fecal incontinence -NO surgery if pt has UC or Crohn's -Lateral or recurrent fissures => suspect Crohn's > anal cancer (UC doesn't involve anus) |
|
|
Sq cell ca of anal canal
-Tx: _ -Indication for APR |
Sq cell ca of anal canal
-Tx: Nigro protocol (chemo-XRT), not surgery -APR for recurrent disease |
|
|
"
|
5-FU, mitomicin, XRT
SCCA of the anal canal generally presents as a mass, sometimes bleeding and pruritus. -APR if chemo-XRT fails or if radiation contraindicated |
|
|
For a patient with normal sphincter function, appropriate treatment for a squamous cell carcinoma of the anal canal would be
|
The Nigro protocol, which combines chemoradiotherapy, has been shown to have equal efficacy when compared with APR with regards to overall survival (OS), while preserving sphincter function in those that had normal function prior to undergoing treatment.
-APR for persistent or recurrent disease. -If it were rectal carcinoma not involving the sphincter, would do LAR with TME |
|
|
what is the treatment for anal sq cell ca?
|
Chemotherapy and radiation is the primary treatment for anal CANAL SCC but wide local excision is the main treatment for anal MARGIN SCC.
|
|
|
patient w/ hx aortic stenosis presents c/ LGI bleed
Suspect _ |
angiodysplasia bleeding:
-RIGHT colon most common -venous bleeding. less severe than diverticular bleed but more likely to recur (80%) -Angiogram: tufts, slow emptying -20-30% have aortic stenosis |
|
|
what side is angiodysplasia bleeding most likely to come from?
venous or arterial? what comorbidity is associated (which anesthesia might want to know about)? |
angiodysplasia bleeding:
-RIGHT colon most common -venous bleeding. less severe than diverticular bleed but more likely to recur (80%) -Angiogram: tufts, slow emptying -20-30% have aortic stenosis |
|
|
what is the #1 cause of pediatric appendicitis?
#1 cause in adults? general physiologic process? |
Appendicitis:
-Anorexia -> periumbilical pain -> vomiting, RLQ pain 2/2 peritonitis -usually 20-35% y/o. can have normal WBC count. -CT: appendix >7mm diameter or >2 mm thick, fat stranding, no contrast in appendiceal lumen -midpoint of antimesenteric border = most likely to perforate -Hyperplasia = #1 cause in kids. can follow a viral illness -Fecalith = #1 cause in adults. -Luminal obstruction -> distension -> venous congestion, thrombosis -> ischemia -> gangrene, necrosis -> rupture -If CT shows walled-off perforated appendix => percutaneous drainage, appy at later date as long as sx improving. may need barium enema or colonoscopy to r/o perforated colon ca. |
|
|
what is most common reason for appendicitis in kids? in adults?
|
Appendicitis:
-Anorexia -> periumbilical pain -> vomiting, RLQ pain 2/2 peritonitis -usually 20-35% y/o. can have normal WBC count. -CT: appendix >7mm diameter or >2 mm thick, fat stranding, no contrast in appendiceal lumen -midpoint of antimesenteric border = most likely to perforate -Hyperplasia = #1 cause in kids. can follow a viral illness -Fecalith = #1 cause in adults. -Stasis of luminal contents, then obstruction -> distension -> venous congestion, thrombosis -> ischemia -> gangrene, necrosis -> rupture -If CT shows walled-off perforated appendix => percutaneous drainage, appy at later date as long as sx improving. may need barium enema or colonoscopy to r/o perforated colon ca. |
|
|
What tumor suppressor gene is mutated as one of the preliminary steps in the adenoma-to-carcinoma sequence in colon cancer?
|
- APC gene: tumor suppressor. early mutation in 60% of sporadic colon cancer
- K-ras mutation (proto-oncogene, chromosome 12p): 65% of sporadic colon cancer. Important event in the dysplastic changes from adenoma -> carcinoma. Thought to occur after the APC mutation and in addition. -hMSH2 (one of the HNPCC mutations, DNA repair gene) -DCC and p53: tumor suppressor genes. occur later in the transition to carcinoma. |
|
|
During an elective resection of the sigmoid colon for a diverticular stricture in a 65-year-old woman, a solid, 6-cm right ovarian mass is found. The most appropriate management is
|
Incidental ovarian mass on laparotomy:
-Post-menopausal => [oophorectomy, frozen section] -> TAH, BSO, and omentectomy -Pre-menopausal => PARTIAL oophorectomy, frozen section -> remove tube + ovary -> if patient done with childbearing, do TAH in 2nd procedure |
|
|
During APR, the vessels located in the lateral stalks are the _ arteries
|
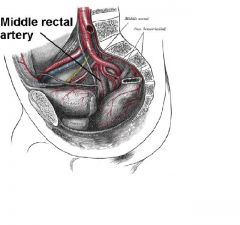
APR anatomy:
-Exicise anal canal + rectum -For malignant lesions not amenable to LAR: invading sphicter complex, fixed to pelvic floor, spread to adjacent organs, <6-8 cm from anal verge -High rate of impotence 2/2 nerve disruption -Higher risk of recurrence c/ rectal than colon ca -MIDDLE RECTAL arteries are in lateral stalks (off the hypogastrics) -If unresectable large liver mets found in OR, proceed c/ APR if pt was c/o bleeding or rectal pain. Otherwise place colostomy + mucus fistula to reduce morbidity. |
|
|
During metastatic w/up in preparation for APR, pt found to have unresectable large liver mets
-Proceed c/ APR only if… |
During metastatic w/up in preparation for APR, pt found to have unresectable large liver mets
-Proceed c/ APR if pt is obstructed, nearly obstructed, significant bleeding or pain |
|
|
"
|
APR
Recurrent cancers usually do so within 2-3 years. -R/o mets (CT A/P, CXR, LFTs, CEA) -> Surgery has best cure rate, should be offered when possible. |
|
|
Rectal ca metastasizes directly to spine via __
|
Rectal ca metastasizes directly to spine via Batson's plexus (venous)
-colon ca rarely metastasizes to bone |
|
|
What is Bowen's disease?
-Tx = _ |
Bowen's disease:
-intraepidermal squamous cell ca only 5% invasive => wide local excision |
|
|
Apthous ulcers seen on colonoscopy => suspect infectious colitits 2/2 organism _
|
Campylobacter colitis:
-may see apthous ulcers on colonoscopy |
|
|
default tx for carcinoid tumor of rectum
-have to do _ if ... |
Carcinoid tumor of rectum:
-Transanal excision = default -Radical resection (APR/LAR) if large or doesn't fit the transanal criteria for polyp (i.e. max T1, <40% circumference, w/in 8-10 cm of anal verge, no lymphovascular invasion, not high grade) |
|
|
Carcinoid of appendix:
when is R hemicolectomy indicated? |
Carcinoid of appendix:
-if 2 cm or invading base, do R hemicolectomy -otherwise appendectomy is sufficient |
|
|
Cecal volvulus:
-tx = _ (alternative = _) |
Cecal volvulus:
-less common than sigmoid volvulus. more prone to gangrene. -Presentation: 20-40 y/o c/ SBO-like sx. 10% of pts are pregnant. Dilated cecum in RLQ -only 20% decompressed by colonoscopy -Usually needs R hemicolectomy with ileo-transverse anastomosis -alternative = cecopexy if colon viable + pt frail |
|
|
50M presents c/ anal mass above dentate line. Bx shows cloacogenic cancer.
-next step = _ |
Anal cancer above dentate line - worse prognosis than below:
Squamous, basaloid (cloacogenic), mucoepidermoid => Nigro protocol = 5FU, mitomycin, XRT +/- extend XRT to inguinal nodes -Adenoca: APR (WLE if <3 cmm, <1/2 circumference, T1, well-diff), post-op chemo-XRT like rectal ca. -Melanoma (#3 site for melanoma): APR c/ margins dicated by melanoma. Most tumors not heavily pigmented. |
|
|
65M presents c/ pneumoturia, Imaging shows thickened sigmoid colon, no diverticuli
-Dx most likely ... |
Colovesical fistula 2/2 colonic adenocarcinoma
|
|
|
65M presents c/ pneumoturia, thickened sigmoid colon, no diverticuli
-Suspect _ |
65M presents c/ pneumoturia, thickened sigmoid colon, no diverticuli => likely adenoca (since no diverticuli)
|
|
|
Colon actively secretes 2 electrolytes ...
|
Colon actively secretes HCO3 and K
|
|
|
55M undergoing sigmoid resection for colonic adenoca and mass is incidentally found in the liver.
-Intraop US shows tumor deep in R lobe, would require R lobectomy -What surgery should be done? |
Sigmoid resection only (would require major liver resection)
-complete metastatic w/u in 6-8 weeks, then bring pt back for liver resection if (+) -if mets were small, could wedge out at time of initial surgery -25% 5-yr survival after removal of isolated liver mets -liver mets are fed primarily by hepatic artery = route for inta-arterial chemo or embolization |
|
|
65M c/ hx T3N1M0 rectal adenoca 8 cm from anal verge undergoees XRT and Leukovorin.
-Restaged c/ imaging and biopsies, no residual tumor found -Tx is _ |
Proceed c/ LAR b/c 15-20% still have cancer on final path
-Similar strategy for APR patients, although there are some studies to just follow them non-op |
|
|
what is the most common location for colon ca?
|
SIGMOID = #1 location for colon cancer
|
|
|
what is the treatment for colon ca invading into adjacent organs?
|
can resect colon ca growing into adjacent organs en bloc with a portion of the organ
-Since it's T3, stage 3, also needs post-op chemo |
|
|
Transformation from colon polyp -> cancer takes ~_ years
|
Transformation from polyp -> cancer takes ~8 years
|
|
|
Colonic AVM:
-_% of patients have aortic stenosis -_% of patients have CAD |
Colonic AVM:
-25% of patients have aortic stenosis -50% of patients have CAD |
|
|
_ = #1 bacterium in feces = _% of fecal bacteria
Colonic anaeobes outnumer aerobes _:1 |
B. vulgatas = #1 bacterium in feces = 12% of fecal bacteria
E coli, Klebsiella, E. faecalis are ~ 0.06% Colonic anaeobes outnumer aerobes 1000:1 |
|
|
#1 location for colon ca = _
|
Colorectal ca:
-#2 cause of cancer death -Sx: anemia, constipation, bleeding -RF: dietary fat (-> O2 radicals), Clostridium septicum infection -Gene mutations: -SIGMOID = #1 site for primary -Spreads to nodes 1st -NODAL STATUS = #1 prognostic facto |
|
|
most R colon cancers can be treated c/ _
|
Most R colon cancers can be treated c/ partial colectomy, primary anastomosis, no ostomy
|
|
|
Management of R colon cancer invading ~ 0.5 cm into liver
|
Colorectal cancer invading into adjacent organs =>
resect en bloc (e.g. with liver wedge or partial cystectomy) |
|
|
Stage _ colorectal ca = into muscularis propria
|
Stage 1 colorectal ca:
-T1: into submucosa -T2: into muscularis propria (not through) -N0, M0 |
|
|
Stage _ colorectal ca = through muscularis propria
(defined as T_) |
Stage 2 colorectal ca:
-T3: into serosa or through muscularis propria if no serosa present -T4: through serosa into free peritoneal cavity or adjacent organs/structures -N0, M0 |
|
|
Stage _ colorectal ca = N1
Tx is _ |
Stage 3 colorectal ca = N1 = 1-3 nodes (+)
(N2 = 4 nodes (+), N3 = central nodes (+)) |
|
|
Stage _ colorectal ca = M1
-Tx is _ |
Stage 4 colorectal ca = M1 = distant mets
-Tx: 5FU + Leukovorin -If rectal, add XRT +/- surgery |
|
|
Tx for colon ca that is N1
|
Stage 3 colon ca = N1:
-Surgery, then post-op chemo (5-FU, leukovorin), no XRT (unlike rectal ca) |
|
|
Tx for colon ca that is M1
|
Stage 4 colon ca = M1:
-5FU + Leukovorin -Resect primary + hepatic mets only |
|
|
2 main malignancies ass'd c/ Cowden's dz
|
Cowden’s Disease = hereditary hamartomatous polyposis syndrome.
-Hamartomatous polyps of the colon and stomach. Mucocutaneous lesions, thyroid adenomas and goiter, fibroadenomas and fibrocystic disease of the breast, uterine leiomyomas, and macrocephaly. 10% risk of thyroid cancer. up to 50% risk of breast adenocarcinoma in affected women. -Hamartomatous polyps are not premalignant. no increased risk of colon cancer in these patients. No increased risk of pancreatic, lung, or small bowel cancers |
|
|
Following a 23 year history of Crohn’s disease, a 54 year old male patient presents with a history of abdominal pain, vomiting and weight loss. Upper GI study reveals a 4 cm stricture within his duodenum. What is best surgical treatment option?
|
Gastrojejunostomy is a more durable repair than stricturoplasty which has a high likelihood of recurrence. Jejunal stricture maybe treated with stricturoplasty.
|
|
|
If performing appendectomy and Crohns is found instead, what do you do?
|
If performing appendectomy and Crohns is found instead, continue with appy unless cecum involved in inflammation
-does not increase fistula rate |
|
|
tx for perianal abscess in Crohn's is _
|
tx for perianal abscess in Crohn's =
I+D just like any other abscess |
|
|
DCC (deleted in colon cancer) gene is present in _% of colon cancer
|
DCC (deleted in colon cancer) gene is present in 70% of colon cancer
|
|
|
The incidence of diverticulitis is about _% to _% in patients with colonic diverticula.
|
Diverticulitis:
- 10-25% of pts c/ colonic diverticula get diverticulitis -LLq pain, fever, leukocytosis. - 2/2 infection, inflamm of colonic wall + surrounidng tissue -Tx if uncomplicated: Flagyl + Bactrim, bowel rest x 3-4 days -Get CT if worried about complication. F/u barium enema to r/o cancer. -25% get complications: abscess most common (obstructive sx, fluctuant mass, peritoneal signs, temp>39, WBC>20). Percutaneously drain abcess -Indications for surgery: recurrent dz (2nd attack has 50% recurrence rate), obstruction, perforation, abscess not amenable to drainage, can't r/o cancer -Some argue that any patient c/ complicated diverticultis or young age should get sigmoid colectomy -R hemicolectomy for R diverticulitis. 80% discovered on planned appendectomy |
|
|
30M presents c/ recurrent UTIs, thickened sigmoid colon, diverticula
-Suspect _ |
Diverticula: in 35% of people, 80% over age 85
-Intraluminal pressure (e.g. straining) -> herniation of mucosa through colon wall @ sites where arteries enter muscular wall -See thickening of circular muscle adjacent to diverticulum, with luminal narrowing -Elevated elastin levels often @ colon wall sites containing diverticula. -80% of diverticula on L (sigmoid) -Bleeds more likely c/ R diverticula: 50% of bleeds are on R -DiverticulITIS more likely on L. Can cause COLO-VESICAL FISTULA |
|
|
55M presents c/ an episode of bleeding 2/2 sigmoid diverticulosis confirmed by colonoscopy, resolves c/ conservative mgmt.
Bleeding recurs in 2 wks. -Tx = _ |
Diverticulosis = #1 cause of LGI bleed. Usually significant bleeding.
-75% self-limited. 25% recur -2/2 disrupted vasa rectum -> arterial bleeding. -Dx: colonoscopy + coagulation (or angio + vasoporessin or highly selective coil embolization if large bleed) - can be therapeutic, will localize bleed -OR if unstable for subtotal colectomy -Tagged RBC scan for intermittent bleed that is hard to localize. NG tube to r/o UGI source -If recurrent bleed, resect the area if it can be localized or subtotal colectomy if not able to localize |
|
|
diverticular bleeds come from what vessels?
|
Diverticulosis = #1 cause of LGI bleed. Usually significant bleeding.
-75% self-limited. 25% recur -2/2 disrupted vasa rectum -> arterial bleeding. -Dx: colonoscopy + coagulation (or angio + vasoporessin or highly selective coil embolization if large bleed) - can be therapeutic, will localize bleed -OR if unstable for subtotal colectomy -Tagged RBC scan for intermittent bleed that is hard to localize. NG tube to r/o UGI source -If recurrent bleed, resect the area if it can be localized or subtotal colectomy if not able to localize |
|
|
External anal sphincter is innervated by __ branch and __ branch of the perineal branch.
S_ branch |
External anal sphincter is innervated by inferior rectal branch of internal pudendal nerve and perineal branch. S4
|
|
|
A 30-year-old woman is admitted with obstructive symptoms and bleeding per rectum. She is found to have a 6x8 cm mesenteric mass on initial CT. She undergoes colonoscopy, and is found to have hundreds of small polyps throughout her colon. Upon further questioning, patient thinks she may indeed have a strong family history of colon cancer.
-What kind of a tumor is that? -What is the tx for that tumor type? |
FAP with a desmoid tumor.
-mutation in the APC gene on xsome 5q. -75% will have a family history of the disease. -Develop 100s-1000s of polyps after puberty. ~100% cancer risk by age 50. -1st deg relatives should be screened by flex sig starting at age 10-15yrs; EGD from age 25 due to risk for adenomas anywhere in the GI tract. Operative options include: 1. total proctocolectomy + end ileostomy, 2. total abdominal colectomy + ileorectal anastomosis, 3. proctocolectomy + ileal pouch-anal anastomosis. -Continued lifetime surveillence if rectum left behind. -Desmoid tumors are responsive to tamoxifen, COX-2 inhibitors (sundilac, celecoxib), NSAIDS. |
|
|
FAP:
-__ gene -inheritence -Tx is __ -Don't forget to check for _ -medication _ makes polyps recede |
FAP = autosomal dominant
-2/2 mutation in APC mismatch repair gene => colon ca by age 40 -Many small polyps on LEFT colon Therapy is total abdominal colectomy c/ mucosal procectomy + ileoanal pullthrough -Also have upper GI polyps => survey duodenum for cancer -Also develop desmoids - benign but difficult to manage -Sundilac makes polyps recede |
|
|
_ = autosomal dominant dz
-2/2 mutation in mismatch repair gene _ -Many small polyps on LEFT colon Therapy is _ |
FAP = autosomal dominant
-2/2 mutation in APC mismatch repair gene => colon ca by age 40 -Many small polyps on LEFT colon Therapy is total abdominal colectomy c/ mucosal procectomy + ileoanal pullthrough -Also have upper GI polyps => survey duodenum for cancer -Also develop desmoids - benign but difficult to manage - treat c/ doxorubicin, other chemo -Sundilac makes polyps recede |
|
|
what is the treatment for FAP?
|
FAP = autosomal dominant
-2/2 mutation in APC mismatch repair gene => colon ca by age 40 -Many small polyps on LEFT colon Tx: TOTAL AB COLECTOMY + MUSCOSAL PROCTECTOMY + POUCH -Also have upper GI polyps => survey duodenum for cancer -Also develop desmoids - benign but difficult to manage -Sundilac makes polyps recede |
|
|
Following total proctocolectomy for FAP, leading cause of death = _
|
FAP = autosomal dominant (but 20% spontaneous)
-Mutation in APC gene (TUMOR SUPRESSOR) on xsome 5-> many small polyps on L colon by puberty -> cancer by age 40 -Flex sig for surveillance (not colonscopy) -Tx by age 20: proctocolectomy, rectal mucosecotmy + ileoanal pouch (or total proctocolectomy + end ileostomy) -Need surveillance of residual rectal muscosa, EGD q2 yrs for DUODENAL POLYPS -#1 cause of death after proctocolectomy = PERIAMPULLARY DUODENAL TUMORS |
|
|
FAP is an autosomal dominant inherited disease that carries a 100% lifetime risk of colon cancer for affected individuals. What other cancer are these patients at risk for?
|
Familial Adenomatous Polyposis (FAP) is an autosomally dominant inherited disease that results in a 100% lifetime risk of colorectal cancer due to a germline mutation in the APC gene located on chromosome 5. These patients are at increased risk for peri-ampullary cancers and it is recommended that they undergo routine surveillance upper-endosocopy starting when colon polyps initially appear.
|
|
|
FAP:
-inheritence is __ -what type of gene is mutated? -most tumors are R or L sided? |
FAP is Autosomal Dominant. The gene involved is the APC gene, which is a tumor suppressor gene. In HNPCC, the gene mutated is a DNA mismatch repair gene, hMLH1 or hMSH2. In FAP, most tumors are LEFT sided, whereas in HNPCC, most tumors are RIGHT sided. FAP has 100% penetrance by age 35. Even after removing the entire colon and rectum, FAP patients have a higher rate of desmoid tumors, periampullary tumors, hepatobiliary tumors and others, which reduce life expectancy versus the unaffected population
|
|
|
Fissure in ano:
-_% are anterior in women rest are located __ |
Fissure in ano:
-10% are anterior in women; rest are posterior-midline -if fissure not midline, consider IBD, TB, syphilis -Tx: sitz baths, regular loose BM (water, fiber) -if persists, then lateral internal sphincterotomy -may try nitroglycerine creams (increased O2 relieves ischemia) or Botox to relax sphincter |
|
|
Fissure in ano;
treatment is ... |
Fissure in ano:
-10% are anterior in women; rest are posterior-midline -if fissure not midline, consider IBD, TB, syphilis -Tx: sitz baths, regular loose BM (water, fiber) -if persists, then lateral internal sphincterotomy -may try nitroglycerine creams (increased O2 relieves ischemia) or Botox to relax sphincter |
|
|
botox is effective in healing _% of anal fissures
|
"For Fistula in Ano, Goodsall's rule states that anterior fistulas connect with rectum in a straight line, while posterior fistulas curve towards a midline internal opening in the rectum. ANAL FISSURES are linear tears in the anal mucosa. The symptoms usually include pain and bleeding. Nearly all cases occur in the posterior midline. When the rare case of anterior fissure occurs, it is prudent to looks for IBD or HIV. While the lateral internal sphincterotomy IS the surgical treatment of choice, it is unnecessary unless medical treatment is ineffective after six weeks of treatment, usually with botulinum toxin (or nitroglycerin). Botulinim toxin has been shown to be effective in healing of anal fissures in 95% of patients.
|
|
|
what is Gardner's syndrome?
|
Gardner's syndrome =
colon cancer (APC tumor supressor mutation like FAP) + desmoid tumors/osteomas |
|
|
A sigmoid adenocarcinoma is resected as part of a low anterior resection. The pathology report states that there is tumor invading the muscularis propria but no lymph node involvement.
What stage is it? -5-yr survival = _-_% |
Stage I colon cancer (T2N0M0) and has a 5-year survival greater than 80 or 90%
Dukes A. Does not require adjuvant chemotherapy 2-3 cm longitudinal margins are adequate, as long as the entire mesorectal tissue radially is resected. A resectable liver lesion is associated with a 25% 5-year survival |
|
|
48 year old female presents with a history of anemia. On CT she is found to have numerous liver masses suggestive of metastatic disease and has adeno carcinoma of the cecum on colonoscopy. The best treatment for her is:
|
Right hemicolectomy, primary anastamosis and liver biopsy
Since the patient presents with anemia, she will require removal of the cause of anemia (the colon cancer) and reestablish GI continuity (primary anastamosis). If she has a solitary liver met that was amenable to wedge resection, then this would be an option. However, this patient requires control of the anemia, without a curative procedure. |
|
|
A 49 yo female underwent a left hemicolectomy for carcinoma 18 months ago, and is now found to have a 2cm mass at edge of right lobe. The most appropriate management is:
|
Wedge resection of the mass. do NOT have to do an anatomic resection of the mass. A wedge resection will prolong the patients survival and there is no benefit to a formal anatomic resection.
|
|
|
_ = autosomal dominant dz
-2/2 DNA mismatch repair mutations in genes hMSH2, hMLH1, hPMS1, hPMS2 Diagnostic criteria are known as… |
HNPCC aka Lynch Syndrome
= autosomal dominant dz -2/2 DNA mismatch repair mutations in genes hMSH2, hMLH1, hPMS1, hPMS3 Amsterdam 1 criteria = 3 relatives c/ colon ca, inc. 2 generations, 1 before age 50, can't have FAP Amsterdam 2 criteria include ca of sm bowel, stomach, ovary, pancreas, biliary tree, skin, larynx |
|
|
HNPCC:
-Cancer usually presents @ location _ -Appropriate therapy is _ |
HNPCC:
-Colon cancer usually on RIGHT (70% proximal to splenic flexure) HNPCC2 can have multiple synchronous cancers -Total colectomy |
|
|
What are the Amterdam criteria for HNPCC?
|
Hereditary non-polyposis colon cancer syndrome = Lynch syndrome:
-5% of population, autosomal D -DNA mismatch repair gene mutation -> RIGHT-sided colon ca, multiple primaries -Lynch 1 => colon ca only -Lynch 2 => colon, ovarian, endometrial, bladder, stomach -Amsterdam criteria: 3 first-deg relatives, over 2 generations, 1 with cancer <50 y/o -Colonscopy starting @ 25, or 10 yrs before 1st relative got cancer -50% have metachronous lesions w/in 10 yrs -Women: annual pelvic exams, endometrial bx q3 yrs, early mammograms. consider TAH + BSO after childbearing -Consider subtotal colectomy for 1st cancer operation |
|
|
what is the difference b/w Lynch I and Lynch II?
|
Lynch I = RIGHT sided, multiple cancers
Lynch II = also ass'd c/ ca of ovary, bladder, stomach -Both a/w DNA mismatch repair gene mutations -Amsterdam criteria: 3 1st deg relatives over 2 generations, 1 before age 50 |
|
|
A 45 year old patient is referred to your colorectal clinic following recent diagnosis of her father and grandmother with colorectal cancer. A hereditary link is suspected and she asks you a question about Lynch Syndrome. She is particularly worried about Ovarian Cancer. Lynch 1 syndrome is associated with
|
Hereditary nonpolyposis colon cancer (HNPCC or Lynch's syndrome)
-1-3% but more common than FAP -Mismatch repair defect (MSH1/2, PMS2), autosomal dominant -70% get colorectal carcinoma, ave age 40-45 -Suspect if RIGHT sided (rare in sporadic colon ca). -40% risk of synchronous/metachronous colorectal carcinoma -Lynch 2 ass'd c/ ENDOMETRIAL, ovarian, stomach, bladder > pancreas, sm bowel, biliary -Amsterdam criteria: 3 1st deg relatives c/ colon adenoca, 2 generations, 1 dx before 50 y/o |
|
|
35F presents c/ cecal cancer
-Likely to have familial syndrome _ -Other major cancer risk is located ... |
Hereditary nonpolyposis colon cancer (HNPCC or Lynch's syndrome)
-1-3% but more common than FAP -Mismatch repair defect (MSH1/2, PMS2), autosomal dominant -70% get colorectal carcinoma, ave age 40-45 -Suspect if RIGHT sided (rare in sporadic colon ca). -40% risk of synchronous/metachronous colorectal carcinoma -Lynch 2 ass'd c/ ENDOMETRIAL, ovarian, stomach, bladder > pancreas, sm bowel, biliary -Amsterdam criteria: 3 1st deg relatives c/ colon adenoca, 2 generations, 1 dx before 50 y/o |
|
|
Pt c/ hx FAP returns to clinic 8 weeks after elective proctocolectomy + J pouch + loop ileostomy
-Must do _ before ileostomy takedown |
do BARIUM ENEMA before takeown of loop ileostomy to r/o stricture @ ileo-anal anastomosis
|
|
|
In average male patient, most distal extent of a rectal cancer to still allow LAR =
_ cm from anal verge |
Low anterior resection:
-Cancer must be at least 6 cm from anal verge (dentate line is ~2 cm from anal verge; levator ani muscles are ~2 cm from dentate line) -Need 2 cm rectal cuff to resect c/ end-to-end stapler -Easier to perform LAR in women b/c wider pelvic bones |
|
|
10 days after LAR, pt develops leukocytosis, mild abdominal tenderness.
CT shows 8x8 cm fluid collection near anastomosis -Next step = _ |
Anastomotic leak >7 days after APR c/ abscess formation =>
percutaneous drain if pt not clinically septic -Bad time to operate since adhesions are starting, but not yet mature |
|
|
5 days after LAR, pt deveops large amount of feculent brown drainage from abdominal wound
-Next step = _ |
Anastomotic leak <7 days after APR =>
Re-explore, take down anastomosis, place colostomy + Hartmann's (high level of contamination) -If leak were small, could consider primary repair of leak + diverting ileostomy |
|
|
6 hrs after LAR, pt develops fever + gray stinky drainage from wound
-Next step = _ |
High fever + gray stinky drainage in early post-op period is concerning for Clostridium perfringens (gram positive rods) =>
re-explore, debride if possible -High risk of myonecrosis, fasciitis |
|
|
10 days after LAR, pt develops clear yellow drainage from wound
-Fluid has Cr of 40 -CT abdomen shows pelvic fluid collection -Next step = _ |
Ureteral injury diagnosed >8 days after LAR =>
Percutaneous drain, then repair ureteral injury in 6-8 weeks (if injury recongized in <7 days, might be able to repair) |
|
|
A week after low anterior resection the patient develops fever, tachycardia and severe abdominal pain. The best treatment is:
|
LOOP COLOSTOMY
The point is to divert the fecal stream as easily as possible. -Hartmann’s procedure would require a re-exploration and would make the takedown more challenging. -Loop ileostomy might be a reasonable option, however because of it’s high output it is less convenient for the patient. -IR drainage is not aggressive enough considering that the patient is having severe abdominal pain. |
|
|
Pt c/ hx diverticulosis presents c/ 2nd episode of lower GI bleed.
Tx is _ |
Pt c/ hx diverticulosis presents c/ 2nd episode of lower GI bleed.
Tx: sigmoidectomy |
|
|
What is #2 site of colon ca mets?
-arrive via __ vein -after resection of isolated mets, _% 5-yr survival |
Lung = #2 location for colon ca mets
-via ILIAC vein -20% 5-yr survival if isolated lung mets resected (in selected patients) |
|
|
A 23-year-old woman with ulcerative colitis is hospitalized for severe diarrhea. She has no oral intake and receives only intravenous fluids. Over a 48-hour period, she develops muscle fasciculations and appears depressed. The most likely cause is a low serum concentration of
|
magnesium
|
|
|
A 70 year old male undergoes an appendectomy for a non perforated appendicitis. A wide based Meckles diverticulum is found. Should the Meckles be removed?
|
The indications for removing an ASYMPTOMIC Meckles are if its base is narrow compared to its total length, and if it is thick, which might be suggestive of ectopic tissue. In this patient of advanced age, the risk of a complication is greater than any potential benefit.
|
|
|
Pt is POD5 s/p open cholecystectomy, develops abdominal distension and pain
-Ab x-ray shows colon dilated to 12cm @ cecum -Tx is _ |
Ogilve's syndrome:
-Pseudo-obstruction of colon -RFs: opiates, bedridden, old + recent surgery, infections, trauma -Massive colon dilation -Check electrolytes (K, Mg), d/c drugs that slow the gut -Tx: colonoscopy + decompression, neostigmine (parasympatomimetic. cholinesterase inhibitor), +/- rectal tube -> cecostomy if that fails |
|
|
p53 is absent in _% of colon cancer
|
p53 is absent in 85% of colon cancer
|
|
|
what is therapy for perianal paget's dz?
|
Paget's disease is intraepidermal adenocarcinoma and can be adequately treated with WLE.
|
|
|
Perianal Paget's disease:
-rare intraepidermal neoplasm of _ type glands -short or long pre-invasive phase? -(+) or (-) PSA stain? |
Perianal Paget's disease:
-rare intraepidermal neoplasm of apocrine glands -long pre-invasive phase -(+) PSA stain |
|
|
What is Peutz Jeghers?
|
Peutz Jeghers = hamartoma polyposis (not colon ca) + mucocutaneous pigmentation esp. oral
-Autosomal D -2% risk of duodenal/colon ADENOcarcinoma (also est. 15x risk) => -endoscopic removal of polyps; no prophylactic colectomy -also ass'd c/ SEX CORD tumors in women, SERTOLI cell tumors in men, breast ca, biliary ca -2/2 serine/threonine kinase mutation. |
|
|
What is tx for colon polyps 2/2 Peutz Jeghers?
|
Peutz Jeghers = hamartoma polyposis (not colon ca) + mucocutaneous pigmentation esp. oral
-Autosomal D -2% risk of duodenal/colon ADENOcarcinoma (also est. 15x risk) => -endoscopic removal of polyps; no prophylactic colectomy -also ass'd c/ SEX CORD tumors in women (granulosa cell), SERTOLI cell tumors in men (testosterone producing), breast ca, biliary ca -2/2 serine/threonine kinase mutation. |
|
|
What is the treatment for pouchitis?
|
Pouchitis: treat c/ Flagyl or short-chain fatty acid enemas
|
|
|
"
|
Primary sclerosing cholangitis (PSC)
-Temporary therapies: ERCP, choledochojejunostomy, PTC -Nearly all patients progress to cirrhosis and eventual liver failure even with treatment -Liver transplant= best treatment for long-term cure |
|
|
Pyoderma gangrenosum: Tx is _
|
Pyoderma gangrenosum: tx = Dapson and/or topical or systemic steroids
Thought to be 2/2 defective neutrophil function First-line therapy for disseminated or localized instances of pyoderma gangrenosum is systemic treatment by corticosteroids and cyclosporine. If ineffective, alternative therapeutic procedures include systemic treatment with corticosteroids and mycophenolate mofetil; mycophenolate mofetil and cyclosporine; tacrolimus; thalidomide; infliximab; or plasmapheresis |
|
|
Pt undergoes LAR then chemo-XRT
6 weeks after chemo, he c/o severe proctitis, rectal bleeding requiring transfusion -Best therapy is _ |
Radiation proctitis:
-Vasculitis, thrombosis, ulcers, strctures -If severe bleeding, treat c/ formalin fixation of rectum (XRT indicated for rectal ca if T3 or N1 = stage 2. decreases local recurrence, improves survival) |
|
|
_% of colon cancer has the ras mutation
|
50% of colon cancer has the ras mutation
|
|
|
Rectal ca can metastasize directly to _ via Batson's plexus
|
Colorectal ca mets:
#1: Portal vein -> Liver, 25% 5-yr survival if resectable c/ adequate liver fx #2: Iliac vein -> Lung, 20% 5-yr survival -Resect isolated liver, lung mets -5% get drop mets to ovaries -Recal ca metastasized directly to spine via veins of BATSON'S PLEXUS -Colon ca rarely goes to bone |
|
|
treatment for rectal cancer c/ pain
|
rectal ca c/ pain => APR
|
|
|
P thas T3N1M0 rectal ca ->
undergoes preop chemo-XRT -Restaging (biopsies of rectum and previous node), and no residual tumor found -Next step = _ |
P thas T3N1M0 rectal ca ->
undergoes preop chemo-XRT -Restaging (biopsies of rectum and previous node), and no residual tumor found -PROCEED C/ LAR (OR APR) AS PLANNED => 15-20% have cancer on final path |
|
|
Rectal ca:
-Transanal excision if ... -Chemo-XRT if ... |
-T1 (limited to submucosa) rectal adenoca can be excised transanally -Stage 2 or 3 => chemo-XRT |
|
|
50 yo male is diagnosed with rectal carcinoma that was determined to be 6cm from the dentate line. A Low Anterior Resection (LAR) was planned for this patients. What is the distance required from anal verge for this operation and what would be margin of resection?
|
8 cm from anal verge and 2 cm margin.
Rectal cancers 8-12cm (middle third) from anal verge (6-10cm from dentate line), as in this case, can be managed by LAR. A 2cm margin of resection from the tumor should be sufficient |
|
|
Compared with postoperative chemotherapy and radiation therapy, preoperative chemotherapy and radiation therapy for treatment of rectal cancer may be associated with lower rates of
|
lower rates of APR
|
|
|
A 58-year-old man undergoes low anterior resection of a rectal adenocarcinoma 5 cm from the anal verge. Pathologic examination shows the well-differentiated tumor invades but does not penetrate the muscularis propria and that four of 15 lymph nodes contain metastatic tumor. There are no liver metastases. The most appropriate postoperative management is
|
Stage 3 rectal ca => resect (if possible) then radiation therapy to the pelvis and chemotherapy (5-fluorouracil and levamisole)
-Chemo (5-FU, levamisole) for stage 2 rectal ca = T3-4N0 -XRT for stage 3 rectal ca = T3 and/or N1 |
|
|
How is rectal adenocarcinoma staged?
-what modality is most sensitive for T and M? -what modality is used for radial tumor eval (local invasion)? |
Rectal adenoca staging by EUS, CT
-EUS most sensitive for T, N -CT for radial tumor eval (local invasion), distant mets |
|
|
Preop chemo/XRT is indicated for rectal adenocarcinoma if... 2 things
|
pre-op chemo/XRT for rectal adenoca if T3/4 (through muscularis propria) or N+
(T1/2 managed by surgery primarily; need 2 cm distal margin) |
|
|
Stage _ rectal ca = M1
-Tx is _ |
Stage 4 rectal ca = M1
-Tx: chemo-XRT +/- surgery (usually just colosotmy) |
|
|
Stage _ rectal ca = through muscularis propria
-Tx is _ |
Stage 2 rectal ca:
-T3: into serosa or through muscularis propria if no serosa present -T4: through serosa into free peritoneal cavity or adjacent organs/structures -N0, M0 -Tx: Preop or postop chemo-XRT (same for stage 3 rectal ca) |
|
|
Tx for low rectal cancer invading into muscularis propria
|
Rectal ca:
-T2 (or higher) = into muscularis propria -Tx: APR or LAR |
|
|
Tx for rectal cancer invading into serosa or past muscularis propria or N1
|
Rectal ca:
-if T3 or N1, need LAR/APR and post-op XRT -Can do XRT pre-op to allow LAR instead of APR |
|
|
Stage 2 or 3 rectal ca.
Tx is_ |
Stage 2 or 3 rectal ca => chemo + XRT
|
|
|
XRT is indicated in rectal cancer if T_ or N_
|
XRT for rectal ca:
-T3 (into serosa or through muscularis propria) - i.e. Stage 2 -N1 (1-3 nodes positive) - i.e. Stage 3 -Decreases local reccurence, increases suvival when combined c/ chemo -Ses: rectal vasculitis, thrombosis, ulcers, strictures -Pre-op chemo-XRT may shrink tumor -> downstage, possibly allow LAR (vs. APR) |
|
|
Pt returns to clinic 6 mo s/p LAR for low rectal ca, c/o constipation
-Found to have mass @ suture line. Metatstatic w/up negative (CT A/P, CXR, LFTs, CEA) -Next step = _ |
Rectal ca local recurrence after LAR:
-Do APR unless pt also has mets that preclude surgery |
|
|
Rectal ca:
-T1 = limited to __. Tx = _ T2: __% are node (+) No transanal excision if __ |
Rectal ca:
T1 (limited to submucosa) => can be excised transanally T2: 20% of node (+), rec APR NO transanal if poorly diff, neuro/vasc invasion |
|
|
main source of nutrition for colonocytes = _
|
main source of nutrition for colonocytes = short chain fatty acids, e.g. butyrate
|
|
|
Elderly pt presents c/ abdominal pain, distension.
Ab x-ray shows distended colon, "ace of spades" shape pointing to LLQ. No peritoneal signs -Suspect _ -Tx is _ -> _% resolve, but _% of those recur |
Sigmoid volvulus:
-More common c/ high-fiber diets (Iran, Iraq) -Debilitated psych pts, neurologic dysfx, laxative abuse -Closed loop obstruction -> pain, distension, obstipation Ab x-ray: bent inner tube sign -Gastrograffin enema: bird's beak sign = tapered colon -No peritoneal signs => colonscopy for decompression (80% reduce, 50% will recur), give bowel prep and perform sigmoid colectomy during same admission -Peritoneal signs, gangrenous bowel => to OR for sigmoidectomy OR detorse + return for resection in 2 days |
|
|
Sigmoid volvulus:
Tx is _ |
Sigmoid volvulus:
-More common c/ high-fiber diets (Iran, Iraq) -Debilitated psych pts, neurologic dysfx, laxative abuse -Closed loop obstruction -> pain, distension, obstipation Ab x-ray: bent inner tube sign -Gastrograffin enema: bird's beak sign = tapered colon -No peritoneal signs => colonscopy for decompression (80% reduce, 50% will recur), give bowel prep and perform sigmoid colectomy during same admission -Peritoneal signs, gangrenous bowel => to OR for sigmoidectomy |
|
|
superior rectal artery = off _ artery
middle rectal artery = off __ -inferior rectal artery = off __ (which is off __) |
superior rectal artery = off IMA
middle rectal artery = off internal iliac -inferior rectal artery = off pudendal (off internal iliac) |
|
|
Tagged RBC scan:
requires bleed of _ cc/min |
Tagged RBC scan:
requires bleed of 0.1 cc/min -good for localizing intermittent slow bleed |
|
|
Criteria for transanal excision of polyp:
-no greater than T_ -<_% circumferential of rectum -W/in _ to _ cm of anal verge -If invasive, no lymphovascular invasion, not poorly differentiated (i.e. low risk of LN mets) |
Criteria for transanal excision of polyp:
-no greater than T1 -<40% circumferential of rectum -W/in 8-10 cm of anal verge -If invasive, no lymphovascular invasion, not poorly differentiated (i.e. low risk of LN mets) |
|
|
What is Turcot's syndrome?
|
Turcot's syndrome:
colon cancer (2/2 APC tumor supressor mutation like FAP) + brain tumors |
|
|
UC: what is the effect of proctocolectomy on extra-colonic manifestations?
|
Proctocolectomy for UC:
-improves pyoderma gangrenosum, erythema nodosum, arthritis, ocular problems -Does not help with sclerosing cholangitis, ankylosing spondylitis. -HLA B27 ass'd c/ sacroileitis |
|
|
A patient with known ulcerative colitis is admitted with a fever, leukocytosis, tachycardia, and abdominal pain with distention. On exam she demonstrates signs of peritonitis. An abdominal XR shows dilated colon throughout. What is next best treatment for this patient?
|
The best procedure in this non-elective case is a staged procedure with total abdominal colectomy and end ileostomy done initially. Eventually the patient can be brought back for completion proctectomy and ilial pouch-anal anastomsis (IPAA).
|
|
|
#1 location for bowel perforation in UC
|
transverse colon = #1 place for perforation in UC
(distal ileum most common in Crohns) |
|
|
60 year old male 5 days after hemicolectomy with extensive lysis of adhesions develops left flank pain and a palpable mass. On physical exam the patient has decreased breath sounds and severe pain. The WBC=13,000. CT scan shows fluid in the left retroperitoneum. The next step should be:
|
Placement of a percutaneous nephrostomy tube
This is a post-op uroma. The key concept is to allow the patient to heal while you drain the urine as simply as possible and then worry about connecting the ureter later with the help of a urologist. |
|
|
Patient has large, symptomatic, sessile colon polyp removed.
-Path: fingerlike projections of epithelium over lamina propria -Most likely it is _ type of polyp -This polyp type has _% rate of cancer inside |
Villous adenoma:
-only 10% of polyps, but most likely to produce sx -50% (+) FOR CANCER -usually sessile, larger than tubular adenomas -Path: fingerlike projections of epithelium over lamina propria |
|
|
GI tract = 2nd most radiosensitive organ (_ = #1)
-Damage @ 3000 rads |
GI tract = 2nd most radiosensitive organ (kidney = #1)
-Damage @ 3000 rads |
|
|
what is the treatment for anal sq cell ca?
|
Chemotherapy and radiation is the primary treatment for anal CANAL SCC but wide local excision is the main treatment for anal MARGIN SCC.
|
|
|
_ = intraepidermal SCC.
Can be adequately treated with WLE in most cases |
Bowen's disease is intraepidermal SCC and can be adequately treated with WLE in most cases.
|
|
|
treatment for rectal cancer c/ pain
|
rectal ca c/ pain => APR
|

