![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
103 Cards in this Set
- Front
- Back
|
these are precursors to steroid hormones & bile salts?
|
cholesterol
|
|
|
what are the 4 types of lipids?
|
Cholesterol, TG, phopholipid, & CE
|
|
|
what are the 5 types of lipoproteins?
|
CM, LDL, IDL, HDL, & VLDL
|
|
|
w/c lipoprotein is synthesized in the liver?
|
VLDL
|
|
|
w/c lipid contains hyrophilic & hyrophobic components?
|
|
|
|
this type of lipid is a storage form of energy?
|
TG
|
|
|
these lipids are more hydrophobic than cholesterol ?
|
cholesterol esters
|
|
|
these lipoproteins are synthesized from FA of dietary TGs & cholesterol? how is it affected by the diet?
|
CM; if someone has been fasting, they will not be found in the diet
|
|
|
w/c 2 lipoproteins transport cholesterol? know how & to where?
|
LDL: transports cholesterol to liver & peripheral cells. HDL transports cholesterol from tissue to liver
|
|
|
% of TC transported by LDL?
|
60-70% of TC
|
|
|
These are VLDL remnants?
|
IDL
|
|
|
Of all of the lipoproteins, w/c has the highest protein? w/c has the highest fat?
|
HDL; CM
|
|
|
W/c LP are hyrolized by LPL?
|
The TG contained in CM & their remnants and in VLDL are hydrolyzed by LPL
|
|
|
Their major constituent is hepatic TG?
|
VLDL
|
|
|
Site of synthesis of HDL?
|
Intestine, liver & plasma
|
|
|
Their major lipid constituent is dietary TG &Ch?
|
CM & their remnants
|
|
|
Their major lipid constituent is hepatic TG?
|
VLDL
|
|
|
Their major lipid constituent is CE & hep TG?
|
IDL
|
|
|
Their lipid constituent is CE?
|
LDL
|
|
|
Their major lipid constituent is phospholipids & CE?
|
HDL
|
|
|
This LP is converted to LDL by hepatic lipase (HL) & taken up by liver?
|
IDL
|
|
|
These apolipoproteins are synthesized in the liver?
|
ApoA-I, ApoB-100, ApoC-II, & ApoE
|
|
|
These Apo are synthesized in the intestine?
|
ApoA-I, Apo-B48
|
|
|
Where is ApoE synthesized?
|
Liver, brain, skin, & gonads
|
|
|
These Apo help to clear blood from lipids?
|
ApoE
|
|
|
These Apo are LPL cofactor?
|
ApoC-II
|
|
|
This Apo is the structural protein of CM?
|
Apo-B48
|
|
|
Fxn of ApoB-100?
|
Structural protein of VLDL, IDL, LDL; it’s also an LDL receptor ligand
|
|
|
Fxn of ApoA-I?
|
structural in HDL; reverse Ch transport.
|
|
|
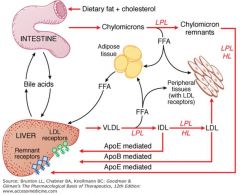
Describe the Exogenous system of lipids?
|
What we eat gets absorbed in the intestine then CM are synthesized & broken down by LPL into CM remnants
|
|
|
After CM gets synthesized from the food we eat, what are different things that can happen to it?
|
1)broken down to CM remnants by LPL 2)can be broken down FFA to go either to the adipose tissue for storage, to peripheral tissues for energy or can be taken up by the liver & w/ the help of CM remnant R, it gets cleared from the blood & excreted.
|
|
|
What mediates the excretion of FFA from the liver?
|
ApoE
|
|
|
Describe the endogenous system?
|
VLDL is synthesized from the liver then broken down by LPL to IDL w/c is further broken down by LPL to LDL
|
|
|
What are the 2 things that can be produced from VLDL?
|
IDL & FFA
|
|
|
Describe the Exogenous system of lipids?
|
What we eat gets absorbed in the intestine then CM are synthesized & broken down by LPL into CM remnants
|
|
|
Once LDL is made, what 2 things can happen to it?
|
It can be taken up by peripheral tissues w/c contain LDL R or it can be taken up the liver (via ApoB mediated) & bind to LDL R on the liver to be cleared from the blood.
|
|
|
Describe the Exogenous system of lipids?
|
What we eat gets absorbed in the intestine then CM are synthesized & broken down by LPL into CM remnants
|
|
|
After CM gets synthesized from the food we eat, what are different things that can happen to it?
|
1)broken down to CM remnants by LPL 2)can be broken down FFA to go either to the adipose tissue for storage, to peripheral tissues for energy or can be taken up by the liver & w/ the help of CM remnant R, it gets cleared from the blood & excreted.
|
|
|
After CM gets synthesized from the food we eat, what are different things that can happen to it?
|
1)broken down to CM remnants by LPL 2)can be broken down FFA to go either to the adipose tissue for storage, to peripheral tissues for energy or can be taken up by the liver & w/ the help of CM remnant R, it gets cleared from the blood & excreted.
|
|
|
What mediates the excretion of FFA from the liver?
|
ApoE
|
|
|
What mediates the excretion of FFA from the liver?
|
ApoE
|
|
|
Describe the endogenous system?
|
VLDL is synthesized from the liver then broken down by LPL to IDL w/c is further broken down by LPL to LDL
|
|
|
Describe the endogenous system?
|
VLDL is synthesized from the liver then broken down by LPL to IDL w/c is further broken down by LPL to LDL
|
|
|
What are the 2 things that can be produced from VLDL?
|
IDL & FFA
|
|
|
What are the 2 things that can be produced from VLDL?
|
IDL & FFA
|
|
|
Once LDL is made, what 2 things can happen to it?
|
It can be taken up by peripheral tissues w/c contain LDL R or it can be taken up the liver (via ApoB mediated) & bind to LDL R on the liver to be cleared from the blood.
|
|
|
Once LDL is made, what 2 things can happen to it?
|
It can be taken up by peripheral tissues w/c contain LDL R or it can be taken up the liver (via ApoB mediated) & bind to LDL R on the liver to be cleared from the blood.
|
|
|
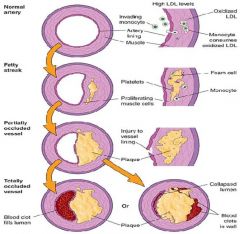
What is the problem w/ high levels of LDL or cholesterol?
|
If there is too much in the blood, they will not be all cleared from the liver so they will be retained in the peripheral tissues where they will go into arterial walls.
|
|
|
What happens to LDL or cholesterol in arterial walls?
|
They will be oxidized w/c will recruit monocytes to consume the oxidized LDL. These consume the LDL to become MQ or foam cells. This turns into an inflammatory response that just keeps going & gets worse w/ time.
|
|
|
What will happen to the foam cells once they are formed?
|
They will form fatty streaks w/n the arterial wall; when there is more oxidation & inflammation, the fatty streak will get bigger & will partially occlude the vessel, eventually forming a plaque that could rupture into the arterial wall.
|
|
|
What is the problem w/ high levels of LDL or cholesterol?
|
If there is too much in the blood, they will not be all cleared from the liver so they will be retained in the peripheral tissues where they will go into arterial walls.
|
|
|
What happens in the arterial wall if the formed plaque ruptures?
|
It will recruit the accumulation of platelets & RBC that will lead to a blood clot.
|
|
|
What happens to LDL or cholesterol in arterial walls?
|
They will be oxidized w/c will recruit monocytes to consume the oxidized LDL. These consume the LDL to become MQ or foam cells. This turns into an inflammatory response that just keeps going & gets worse w/ time.
|
|
|
What will happen to the foam cells once they are formed?
|
They will form fatty streaks w/n the arterial wall; when there is more oxidation & inflammation, the fatty streak will get bigger & will partially occlude the vessel, eventually forming a plaque that could rupture into the arterial wall.
|
|
|
What happens in the arterial wall if the formed plaque ruptures?
|
It will recruit the accumulation of platelets & RBC that will lead to a blood clot.
|
|
|
This HyperLipidemia Rx is a Ch absorption inhibitor?
|
Ezetimibe
|
|
|
This Rx is a bile acid sequestrants?
|
Resins
|
|
|
What does HMG-CoA reductase do?
|
Converts HMG-CoA to mevalonate w/c eventually makes Ch.
|
|
|
This HyperLipidemia Rx is a Ch absorption inhibitor?
|
Ezetimibe
|
|
|
This Rx is a bile acid sequestrants?
|
Resins
|
|
|
What does HMG-CoA reductase do?
|
Converts HMG-CoA to mevalonate w/c eventually makes Ch.
|
|
|
Some of these products are found to be contaminated w/ citrinin toxins?
|
Red yeast rice
|
|
|
What are the bile acid sequestrants?
|
Cholestyramine, colestipol HCL, & colesevelam
|
|
|
What is the MOC BAS on the GB?
|
Increase Ch 7 alpha hydroxylase, increase conversion of Ch to BA & increase BA secretion
|
|
|
What is the MOC of BAS on terminal ileum?
|
Increase BA excretion
|
|
|
What the MOA of BAS on liver?
|
Increase LDL R & increase VLDL & LDL removal.
|
|
|
These are large non absorbable polymers that bind bile acids in the intestine?
|
BAS
|
|
|
T/F: BAS cause BA to be absorbed & taken to the liver?
|
FALSE, they prevent BA absorption & recycling
|
|
|
Effect of BAS on lipid/LP?
|
Decrease TC & LDL, no change or may increase TG & increase HDL
|
|
|
Administration of BAS?
|
It’s a powder/granule that is administered as a suspension
|
|
|
BAS can be given w/ what type of food?
|
Water, milk, juice, may be mixed w/ applesauce, soft cereal.
|
|
|
Relate administration of BAS w/ meal time & other Rx time?
|
Taken w/n 1 hr of meal. Give other meds at least 1 hr before or at least 4-6 after.
|
|
|
This type of antihyperlipidemia Rx is not significantly absorbed?
|
BAS
|
|
|
BAS decrease the absorption of what drugs?
|
Anticoagulant (warfarin) BB, carbamazepine, Digoxin, Diuretics (thiazide), levothroxine, & mycophenolate. “The ABCDs of lipid meds
|
|
|
MC SE of BAS?
|
Constipation is the MC SE. it’s usually transient but can also lead to impaction.
|
|
|
May get increased TG from this antihyperlipidemic drug?
|
BAS
|
|
|
SE of BAS?
|
GI effects (bloating, nausea, vomiting flatulence & constipation), pancreatitis, increased TG
|
|
|
What is an absolute CI in BAS?
|
Biliary obstruction & TG >400mg/dL
|
|
|
Effect of BAS on lipid/LP?
|
Decrease TC & LDL, no change or may increase TG & increase HDL
|
|
|
What is a relative CI in BAS?
|
TG >200mg/dL
|
|
|
Administration of BAS?
|
It’s a powder/granule that is administered as a suspension
|
|
|
BAS can be given w/ what type of food?
|
Water, milk, juice, may be mixed w/ applesauce, soft cereal.
|
|
|
What is a precaution w/ BAS?
|
Some of the formulations contain aspartame so must be avoided in PKU pts.
|
|
|
Relate administration of BAS w/ meal time & other Rx time?
|
Taken w/n 1 hr of meal. Give other meds at least 1 hr before or at least 4-6 after.
|
|
|
This type of antihyperlipidemia Rx is not significantly absorbed?
|
BAS
|
|
|
BAS decrease the absorption of what drugs?
|
Anticoagulant (warfarin) BB, carbamazepine, Digoxin, Diuretics (thiazide), levothroxine, & mycophenolate. “The ABCDs of lipid meds
|
|
|
MC SE of BAS?
|
Constipation is the MC SE. it’s usually transient but can also lead to impaction.
|
|
|
May get increased TG from this antihyperlipidemic drug?
|
BAS
|
|
|
SE of BAS?
|
GI effects (bloating, nausea, vomiting flatulence & constipation), pancreatitis, increased TG
|
|
|
What is an absolute CI in BAS?
|
Biliary obstruction & TG >400mg/dL
|
|
|
What is a relative CI in BAS?
|
TG >200mg/dL
|
|
|
What is a precaution w/ BAS?
|
Some of the formulations contain aspartame so must be avoided in PKU pts.
|
|
|
What are the Regular release niacin?
|
Nicor as Rx & niacin as supplement
|
|
|
What are the ER niacin?
|
Niaspan (Rx) & slo-niacin as supplement
|
|
|
What are the combo Rx w/ niacin?
|
Simvatatin/Niaspan & lovastatin/Niaspan
|
|
|
What is the MOA of niacin?
|
1)inhibits Lipolysis of TG in adipose, 2) reduces transport of FFA to the liver, 3) decrease hepatic TG synthesis, 4) reduces hepatic VLDL production 5) increases apoB degradation, 6) reduces hepatic clearance of HDL so raises HDL
|
|
|
This drug has extensive 1st pass metabolism?
|
Niacin
|
|
|
What are the peak [ ] of niacin?
|
45 min for RR & 4-5 for ER
|
|
|
What are the DI of niacin?
|
Alcohol: exacerbate flushing, BAS: decrease niacin absorption so separate dosing, Warfarin: may increase INR
|
|
|
What must be monitored w/ niacin?
|
Hepatic enzymes
|
|
|
What are the SE of niacin?
|
Cutaneous flushing, GI effects (nausea, dyspepsia, vomiting, diarrhea), hepatotoxicity, hyperglycemia, hyperuricemia
|
|
|
How do we decrease Cutaneous flushing w/ niacin?
|
Give ASA ½-1 hr before niacin. Tolerance develops 7-14 days
|
|
|
How does niacin work in causing flushing?
|
Niacin activates the AA pathway w/c causes the production & release of PG where they act on the smooth mm & cause flushing.
|

