![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
292 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is the brain made of? |
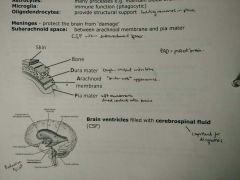
Neurons = functional units - Sensory: periphery > CNS - Motor: CNS > periphery - Interneurons: sensory > motor
Glial cells (not axon or dendrites) - Astrocytes: many processes (maintain BBB) - Microglia: immune function (phagocytic) - Oligodendrocytes: provide structural support (hold neurons in place)
Meninges: protect brain from 'damage' Subarachnoid space: between arachnoid membrane and pia mater |
Brain Structure and Function |
|
|
Prenatal brain development |

Invagination of neural tube
Birth defects: - Failure of neural tube folding may give rise to various birth defects of brain + spinal cord • Spina bifida: Spinal column does not fold completely/properly, surgery required • Anencephaly: incomplete development of brain+skull, low survival - Folic acid recommended to prevent |
Brain Structure and Function |
|
|
Formation of neurons and glial cells |

Stem cells (derived from ectoderm - embryonic tissue that is precursor for CNS) > Progenitor > Differentiation into cells |
Brain Structure and Function |
|
|
Tour of Brain |
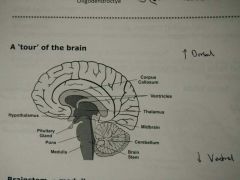
Brainstem: medulla, pons and midbrain - Medulla: centre for respiration + circulation - Pons: bridge between different brain regions, autonomic function, sleep + arousal - Midbrain: body movement, substantia nigra, relay auditory + visual info
Cerebellum - 'Little brain' - Coordinates fine muscle movement + balance - Impairment results in ataxia (lack of coordination)
Hypothalamus - Regulates body temp, feeding, sexual behaviour, sleep (homeostasis) - Pituitary gland > hormones
Thalamus - Sensory switchboard - Relays sensory info to and from cortical regions
Corpus callosum - Connects left+right hemispheres - Agenesis = no/partial development of corpus callosum > seizures |
Brain Structure and Function |
|
|
Cerebral cortex |
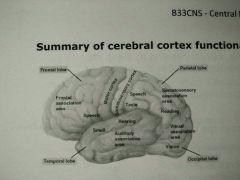
- Largest and most highly developed region of brain - Divided into multiple lobes
Frontal lobe (Motor) - Prefrontal cortex: intellectual, emotional (suppresses aggressive behaviour) - executive decision making - Motor cortex: premotor + primary motor cortex
Parietal lobe (sensory) - Process sensory info - taste, temp, touch; numbers; orientation
Occipital lobe (visual) - Visual info only
Temportal lobe - Primary auditory cortex - Visual cognition due to close association with occipital lobe |
Brain Structure and Function |
|
|
Basal ganglia |
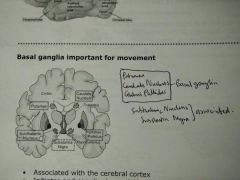
- Important for movement - Associated with cerebral cortex - Initiates and coordinates activities such as walking - Inhibits unwanted or unnecessary movements - Death of basal ganglia neurons > disruption of movement control = Parkinson's (Tremor) |
Brain Structure and Function |
|
|
Limbic System - 'emotional brain' |
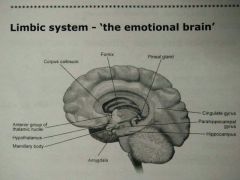
Hippocampus - Long term memory, inhibition of behaviour, spatial navigation, Alzheimer's
Cingulate gyrus - Cingulate gyrus > Hippocampus > Hypothalamus - Coordinates sensory input with emotions (delivers emotions to right areas)
Amygdala - Aggression, anger, memory, anxiety, sadness, sex drive, fear
Hypothalamus and thalamus - Involved in emotions as well
|
Brain Structure and Function |
|
|
How do neurons communicate? |

Electrical synapses (gap junctions) - Bidirectional flow of ions between cells - Connexon: made up of 6 connexins
Chemical synapses (neuron-neuron) - main mode of communication 1. Vesicle: synthesis of NT in presynaptic neuron 2. Packed into vesicle 3. Action potential permits vesicle to move towards synapse 4. Vesicle fusion with neuron membrane > release of NT (exocytosis) 5. NT binding to receptor on postsynaptic membrane 6. Initiate downstream signalling + action potential 7. Reuptake: transporter to recycle NT 8. Termination: enzyme that breaks down NT into metabolites |
Neurotransmission and drug mechanisms |
|
|
Excitatory/Inhibitory Chemical Synapses |
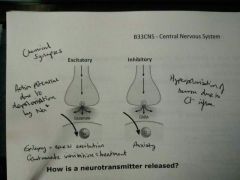
Excitatory = Glutamate (Na+ influx - depolarisation) Inhibitory = GABA (Cl- influx - hyperpolarisation)
Epilepsy = excess excitation > glutamate inhibition treatment |
Neurotransmission and drug mechanisms |
|
|
Acetylcholine NT |
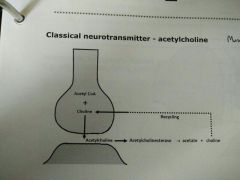
Synthesis = acetyl CoA + choline via choline-acetyltransferase Storage = vesicles in presynaptic Release = via exocytosis Termination via enzyme acetylcholinesterase >> acetate + choline |
Neurotransmission and drug mechanisms |
|
|
Glutamate NT (Excitatory) |
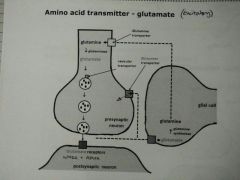
- Glutamine > Glutamate via glutaminase - Stored in vesicles in presynaptic - Release > activate NMDA + AMPA receptors - Glial cell recycles glutamate > glutamine via glutamine synthetase - Glutamine transporter recycles glutamate from synapse |
Neurotransmission and drug mechanisms |
|
|
GABA NT (Inhibitory) |
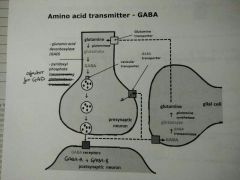
- Glutamate > GABA via glutamic acid decarboxylase (GAD) and co-factor pyridoxyl phosphate - Stored in vesicles in presynaptic - Release > activates GABA-A and GABA-B receptors - Glial cells recycles GABA into glutamate via GABA transaminase - GABA transporter recycles GABA from synapse |
Neurotransmission and drug mechanisms |
|
|
Biogenic amines |
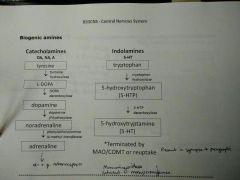
Catecholamines (dopamine, noradrenaline, adrenaline) Indolamines (5-HT serotonin) |
Neurotransmission and drug mechanisms |
|
|
Nitric oxide NT (atypical) |
- Promote dilation - L-arginine > NO via nitric oxide synthase - Not stored in vesicles - Diffuses freely across cell membranes - Not released via exocytosis - Termination is a passive process - Not confined to presynaptic-postsynaptic direction - retrograde messenger (bidirectional) |
Neurotransmission and drug mechanisms |
|
|
Ionotropic receptors/ligand gated ion channels |
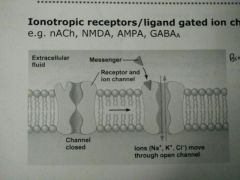
- Fast transmission - nACh, NMDA, AMPA, GABA-A - Binding induces conformational change allowing ion influx/efflux |
Neurotransmission and drug mechanisms |
|
|
Metabotropic receptors/G-protein coupled receptors |
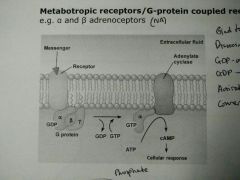
- Fairly fast transmission - a + b-adrenoceptors (NA) - Bind to GPCR - Dissociation of B + Y subunits - GDP-a subunit: GDP>GTP - Activate adenylate cyclase - Conversion of ATP into cAMP > response |
Neurotransmission and drug mechanisms |
|
|
Tyrosine kinase |
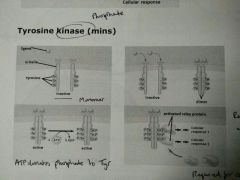
- Minutes - Ligand binds, forms dimer - Conversion of ATP>ADP, phosphorylation of tyrosine residues - Relay proteins associate with phosphate > cellular response - Cellular growth |
Neurotransmission and drug mechanisms |
|
|
Nuclear receptors |
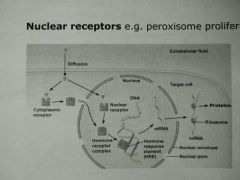
- Long transmission - Peroxisome proliferatos activated receptor (PPAR) - Diffusion into cell > cytoplasmic receptor or nuclear receptor - Hormone-receptor complex - Hormone-response element > Alters gene expression - mRNA > protein production |
Neurotransmission and drug mechanisms |
|
|
Brain Exracellular Fluid (ECF) |
- Occupies extracellular space - Interacts with CSF, neurones, glial cells - Solute concentration fluctuates with neuronal activity, and changes in ECF composition affect behaviour - Three methods of controlling composition: • CSF synthesised by choroid plexus influences ECF composition • BBB protects ECF from fluctuations in blood composition, and limits entry of compounds into ECF • Glial cells condition ECF |
BBB and CSF |
|
|
Cerebral Spinal Fluid (CSF) |
- Fills ventricles and forms thin layer around brain and spinal cord in subarachnoid space - 150ml with 500ml produced /day, turn over 3x /day - Secretions push existing CSF into subarachnoid space - Acts as cushion/shock-absorber; renders brain buoyant - Local environment for neurones and glia (buffer) - Exchange medium between ECF and blood - Removal of waste products: metabolism, drugs, NT metabolites - Interface between brain and Peripheral Endocrine Functions (e.g. hormones released from hypothalamus) |
BBB and CSF |
|
|
Ventricles |

|
BBB and CSF |
|
|
CSF Movement |

- Lateral Ventricles (Cortex) - Foramina of Monroe - Third Ventricle (Thalamus) - Cerebral aqueduct of Sylvius - Fourth Ventricle (Brain Stem) - Two foraminae of Luschka and Foramina of Magendie - Subarachnoid space |
BBB and CSF |
|
|
CSF Circulation |
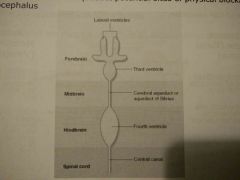
- Structures of ventricle system are embryologically derived from centre of neural tube during development - Rostral = caudal CSF circulation - 3 foramina projecting into the subarachnoid space permit CSF circulation around brainstem, cerebellum + cerebral cortex - Foramina and cerebral aqueduct potential sites of physical blockage = hydrocephalus |
BBB and CSF |
|
|
CSF Secretion |
- Formed via two processes: • Ultrafiltration of plasma across fenestrated capillary wall into ECF beneath basolateral membrane of choroid epithelial cell • Choroid epithelial cells secrete into ventricles |
BBB and CSF |
|
|
Mechanism of CSF secretion |

|
BBB and CSF |
|
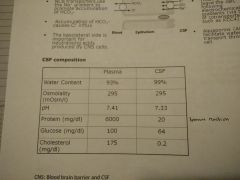
CSF Composition |
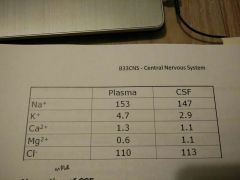
|
BBB and CSF |
|
|
Absorption of CSF |
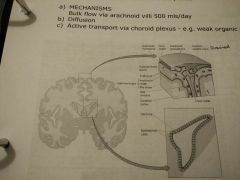
SITES: - Arachnoid villi within the subarachnoid space (via diffusion) - Vascular epithelium of the choroid plexus MECHANISMS - Bulk flow via arachnoid villi 500ml/day - Diffusion - Active transport via choroid plexus |
BBB and CSF |
|
|
Pial and parenchymal vessels |
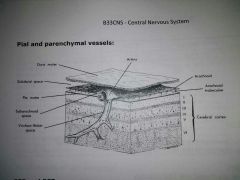
|
BBB and CSF |
|
|
CSF and ECF pathway |
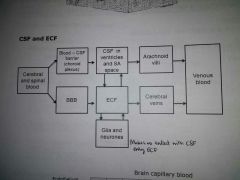
|
BBB and CSF |
|
|
Diagnostic use of CSF |
- Spinal tap or lumbar puncture allows sampling of CSF - pathogens/CSF pressure (hydrocephalus, subarachnoid haemorrhage) - Routine clinical prodcedure at L3-5
- Spinal block to anaesthetise spinal nerves distal to site, intrathecal (routine) - Injection into third ventricle, unlimited access to ECF > neurones + glia (not routine) |
BBB and CSF |
|
|
Blood Brain Barrier |
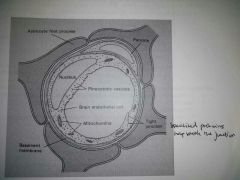
- CNS requires ultrastable internal environment, regulate transport between blood + brain > BBB - Endothelial cells provide physical barrier - Metabolic barriers - Capillary endothelium cells have tight junctions, not fenestrations - Limit molecules >2000 MW
- Lipid solubility (more lipid soluble, more access) - Degree of ionisation (more ionised, less access) - Degree of plasma protein binding (bound, no access)
- Facilitated transport of monosaccharides - Specific to D-glucose - Competitive |
BBB and CSF |
|
|
Amino Acid Transport |
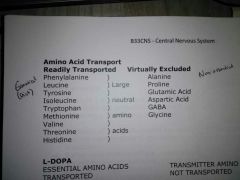
Essential aa = transported Non-essential aa = virtually excluded |
BBB and CSF |
|
|
BBB Metabolic Barriers |
- Endothelial cells, rich in certain metabolic enzymes (MAO) - Unable to use dopamine for Parkinson's beacuse ionised + metabolised by MAO - Use precursor L-DOPA + peripheral DOPA decarboxylase inhibitor, enters unionised - Inhibitor prevents cnversion of L-DOPA to dopamine in periphery, cannot enter BBB as ionised |
BBB and CSF |
|
|
BBB Disorders |
- Tumours: Leaky, increased nutrients, increased growth - Infiltration: Infection, increased antibiotic permeability - Ischaemia: Cellular damage, increased water oedema |
BBB and CSF |
|
|
Non-barrier Regions |
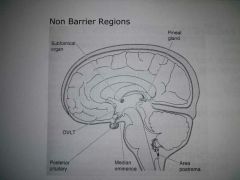
- Brain areas lacking BBB = circumventricular organs - tight junctions replaced by fenestrated endothelia - Posterior pituitary - hormones have access to general circulation - Median eminence: oxytocin+vasopressin - pick up releasing hormones for variage via pituitary portal system to anterior pituitary - Area postrema - cheomreceptor zone (vomiting) - Organum vasculosum of lamina terminalis (OVLT) - important for actions of cytokines in periphery (fever) |
BBB and CSF |
|
|
Introduction to Schizophrenia (SZ) |
- Onset = late adolescence + early adulthood (acute onset over 2-3 weeks) - Median M=23, F=28 - Prevalent in M > F ? Oestrogen plays role in regulating DA receptor sensitivity |
Schizophrenia |
|
|
Aetiology of SZ (Environmental) |
- M in urban areas (unknown cause) - Countries further away from equator - Perinatal complications: severe malnutrition, stressful events, birth complications, altered brain development - Cannabis use? |
Schizophrenia |
|
|
Aetiology of SZ (Genetic) |
- Family history of SZ - Twin studies validate genetic contribution - Susceptibility genes: Neuregulin + Dysbindin - Influence neurodevelopment + synaptic functioning |
Schizophrenia |
|
|
Clinical Presentation of SZ |
Positive Symptoms (acute) - Thought insertion - 3rd person auditory hallucinations - Thought disorder - Delusional perception - > 1month - Not mood disorder/organic disease Negative symptoms (chronic) - Flattened mood - Indifference + loss of drive - Social isolation - Poor self care - Poverty of speech Cognitive impairment - Attention, working + semantic memory Working memory - Temporary storage + manipulation of info - Necessary for tasks such as language comprehension, learning + reasoning Semantic memory - Long term memory > ideas/concepts - Inclusion of common knowledge |
Schizophrenia |
|
|
SZ sub syndromes |
Paranoid SZ - Auditory delusions + hallucinations Disorganised SZ - Thought disorder, odd behaviour, inappropriate mood Catatonic SZ - Rare form - Due to treatment of condition • Unable to move/speak • Staring • Body in rigid position • Unaware of surroundings |
Schizophrenia |
|
|
SZ Diagnosis |
One or more of following if clear-cut: - Delusions - Hallucinations
- Delusions - Hallucinations - Disorganised speech - Catatonic behaviour - Negative symptoms - flattened mood, inability to speak, general lack of drive |
Schizophrenia |
|
|
Dopamine + SZ |
Theory: - Excess DA and DA receptors Evidence: - Antipsychotic drugs = D2 receptor antagonists - DA agonists (amphetamines, levodopa) > paranoid psychosis - CSF + brain studies = abnormal DA levels, metabolites, enzymes or receptors DA not sole contributor ? DA changes glutamate downstream transmission - Signalling via NMDA is implicated (NMDA antagonists - ketamine- produce SZ-like syndrome) |
Schizophrenia |
|
|
Other SZ Theories |
Functional imaging studies - Abnormalities in cerebral blood flow + metabolism = impairment of neuronal circuits - Specific impairment in frontal cortex (decisions), hippocampus (memory), thalamus + cerebellum Structural brain changes - Enlargement of lateral ventricles - Slight decrease in brain size - Altered neuronal + synaptic organisation - Affected white matter - No gliosis (neurodegenerative process) SZ = neurodevelopmental =/= neurodegenerative (no cell death) |
Schizophrenia |
|
|
Antipsychotic medication |
Management strategy - Intervention: physical, psychological, social - Initial assessment: complusory admission required, drug-free if possible - Antipsychotics effective against most positive symptoms (2-3 week onset) - Investigate patient context (substance misuse) - Family support is key |
Schizophrenia |
|
|
Pharmacological management of SZ - antipsychotics |
- Inhibit D2 receptors - Reverse excess DA activity in mesolimbic system (site for psychosis symptoms) - Single SZ episode > continue for 12-24 months - Improvement = tail off treatment (tardive dyskinesia, s/e) - Informed by presentation of patient - Patient's choice - s/e profile - Treatment history - 6 week trial at adequate dosage - Avoid use with anticholinergic agents (exacerbate anti-muscarinic s/e) - Minor effects on negative + cognitive symtoms |
Schizophrenia |
|
|
Atypical antipsychotics |
- No extrapyramidal s/e • Risperidone • Olanzapine > metabolic syndrome • Amisulpride > some against negative • Quetiapine > very sedating • Aripiprazole > stabilises DA (partial agonist) - Weight gain - Hyperglycaemia + T2 diabetes (drug induced hyperglyc + insulin resistance) - Metabolic syndrome (dyslipidaemia, hypertension) Clozapine - Effective in 30% resistant patients - no response to two 6 week trials - Reduce suicide risk - Agranulocytosis (bone marrow suppression) - Reserved as last choice treatment - Weekly blood tests - Weight gain, metabolic syndrome, hypersalivation, sedation, seizures (high dose) |
Schizophrenia |
|
|
Typical antipsychotics |
- Chlorpromazine, haloperidol - Extrapyramidal s/e - motor abnormalities relted to receptor blockade in basal ganglia Acute dystonia - Painful contractions in neck, jaw, eye muscles - Young men high doses - Intramuscular/intravenous anticholinergic agents Parkinsonism - Decreased facial movements, stiffness, tremor - Common in early weeks - Reduce dose or anticholinergic agent Akathisia - Restlessness/need to walk around - First months of Tx - Lower dose or propanolol (b-blocker) Tardive Dyskinesia - Uncontrollable grimacing movements of face, tongue, upper body - 5% patients long term - No prediction - Can be irreversible - No treatment, lower dose Neuroleptic malignant syndrome - 1 in 500 - Pyrexia, stiffness, autonomic instability > coma - Raised serum Cr kinase (muscle damage), metabolic acidosis, leucocytosis - Stop drug + monitor - Restart Tx gradually with atypical Prolongation of QT interval - Serious arrythmia - Inhibition of specific cardiac K+ channels |
Schizophrenia |
|
|
Other antipsychotics |
Benzodiazepines: short term Antidepressants: Tx as NICE recommendation Electroconvulsive Treatment: only catatonic SZ Non-pharmacological (family) - Focus: educate family - Modest effectiveness - Difficult to implement widely (finance) Cognitive Behavioural Therapy - Against auditory hallucinations + delusions - Integral component of SZ Tx - Simple practical methods (earplugs) |
Schizophrenia |
|
|
Anxiety introduction |
- Feeling of unease, such as worry or fear, that can be mild or severe - Diagnosis made if feeling occurs all the time |
Anxiety and depression |
|
|
Types of anxiety |
Panic disorder - Intense and abrupt feeling of frear or discomfort • Sudden temperature changes • Chest pain • Nausea + dizziness • Overwhelming feelings Obsessive Complusive Disorder - Combiantion of obsessive thoughts and compulsive activity - Obsession: unwanted/unpleasant thoughts that cause anxiety - Compulsion: repetitive behaviour to relieve unpleasant feeling Post-traumatic Stress Disorder - Experience of trauma - Immediately or over years - Interferes with normal functioning - Insomnia, nightmares, flashbacks, isolation Phobias - Intense fear of something of little danger (specific) - Fear of social situations from negative judgements, avoid situation (social) |
Anxiety and depression |
|
|
Generalised Anxiety Disorder |
- Excessive uncontrollable worry about every day things: job, chores, finances, health, family - Intensity, duration and frequency are disproportionate - Occur with other conditions - Physical symptoms |
Anxiety and depression |
|
|
Anxiety diagnosis |
- Rule out organic disease - Mental health history - Environmental stressors - Medical and drug history - Degree of distress and functional impairment - Suicide |
Anxiety and depression |
|
|
Management of Anxiety - Non-pharmacological |
- Relieve symptoms, improve quality of life and prevent relapse • CBT • Meditation + relaxation • Mindfulness • Exercise |
Anxiety and depression |
|
|
Management of anxiety - Pharmacological |
Beta blockers (propranolol) - Reduces autonomic effect - Used on as required basis - Do not withdraw abruptly Selective Serotonin Reuptake Inhibitor (SSRI - Sertraline, Escitalopram, Paroxetine) - If no improvement: • Switch SSRIs • Consider Serotonin-Noradrenaline Reuptake Inhibitor (SNRI - venlafaxine, duloxetine) • Consider anti-convulsant pregabalin (last choice) Benzodiazepines - Anxiolytic - Hypnotic - Sedative - No enzyme induction - Some tolerance - Dependence + withdrawl symptoms > Short term usage - Metabolism = oxidation + conjugation > older patients prolonged - Active metabolites - Relatively safe in overdose Hypnotics (temazepam, nitrazepam, zolpidem) - Short half life (1-10hrs) Anti-anxiety (diazepam, chlordiazepoxide, lorazepam) - Longer half-life (1-4 days) - BDZs best avoided by use restricted to 2-4 weeks + taper |
Anxiety and depression |
|
|
GABA and Anxiety |
- GABA is main inhibitory NT in CNS - Causes Cl- influx - BDZs occupy GABA-A site, greater flow of Cl-, hyperpolarisation |
Anxiety and depression |
|
|
Depression introduction |
- Amongst top 10 most common GP consultations - Suicide remains most common cause of death in young men - Risk factors: • History of depression + suicide attempt • Illness • SZ or dementia • Family history - No single genetic defect in depression has been conclusive in its identification |
Anxiety and depression |
|
|
Depression Diagnosis |
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 1. Depressed mood 2. Loss of interest or pleasure 3. Fatigue 4. Feelings of worthlessness, guilt or inappropriate grief 5. Recurrent thoughts of death or suicide 6. Reduced ability to think or concentrate 7. Psychomotor agitation or retardation 8. Altered sleep 9. Significant weight change Subthreshold - At least 2 but less than 5 symptoms - One 'core' symptom Mild -Few but in excess of 5 symptoms - Minor functional impairment Moderate - Some marked symptoms - Presence of functional impairment Severe - Multiple symptoms - Markedly interfere with functioning |
Anxiety and depression |
|
|
Bipolar disorder |
- Cycle between depressed mood and mania - Depressed: at least 2 weeks with core symptoms with at least 4 other symptoms - Mania: elevated mood, increased energy, incomprehensible speech, racing thoughts, poor concentration - First episode before 30yo with peak between 15-19 - Mostly ethnic minorities - Differential diagnosis - Confirmed by specialist mental health professional Treatment - Mania: antipsychotics (haloperidol, olanzapine, quetiapine, risperidone), add lithium or sodium valproate if ineffective - Depression: quetiapine > Fluoxetine + Olanzapine > Olanzapine > Lamotrigine Maintenance: continue treatment as above, lithium or sodium valproate, psychological intervention |
Anxiety and depression |
|
|
Science of depression |
- Decrease size of thalamus, hippocampus and amygdala - Decrease in 5-HT - Decrease in NA - Decrease in tyrosine > decrease in DA |
Anxiety and depression |
|
|
Management of depression |
- Manage suicide risk, improve QoL, prevent relapse - CBT, good sleep hygiene - Patient choice for drugs - Adverse effect profile - Toxicity in overdose - Interaction with other treatments Generic SSRIs (first line) - Citalopram, fluoxetine, paroxetine, sertraline - Favourable s/e profile + less toxic in overdose - Symptoms worse before improving - Vigilant on suicidal ideas especially when commencing or changing medication - 2-4 weeks for improvement - Taken for no less than 6 months after recovery to prevent relapse - 6-8 week weaning - s/e: nausea, vomiting, diarrhoea, dizziness - Antidepressants avoided in <18yo but fluoxetine if needed - Lifestyle advice including positive coping strategies |
Anxiety and depression |
|
|
Selective-serotonin reuptake inhibitors (SSRIs) |
- Inhibition of 5-HT reuptake in pre-synaptic - Increase stimulation of 5-HT receptor due to increase NT in synapse - Delayed effect - 5-HT1 autoreceptor prevents 5-HT exocytosis - Continuous use, downregulation of 5-HT1 autoreceptor, inccrease release 5-HT - Some 5-HT broken down by MAO and COMT |
Anxiety and depression |
|
|
Other depression treatment |
SNRI (serotonin-noradrenaline reuptake inhibitor) - Venlafaxine, duloxetine - Similar to SSRIs TCA (tricyclic antidepressants) - Amitriptyline, imipramine - Inhibit 5-HT and NA reuptake - Sedative (H1 antagonism) - Anticholingeric s/e: dry mouth, blurred vision - CV and epileptogenic effects can be fatal in overdose - Lofepramine associated with lowest risk in overdose - Not used anymore - s/e MAOI (monoamine oxidase inhibitor) - NOT USED - Phenelzine, tranylcypromine - Increase NA in synapse > hypertensive crisis NaSSA (Noradrenergic and specific serotonergic antidepressant) - Mirtazapine - a2 auto- and heteroreceptor antagonism - increase 5-HT and NA release NARI (noradrenaline reuptake inhibitor) - reboxetine St John's Wort - Herbal remedy - Insufficient evidence - No prescribe |
Anxiety and depression |
|
|
Insomnia |
Don'ts - Daytime naps - Caffiene - Heavy meal at night - Gadgets before sleep Do's - Sleep mask - Exercise Complement sleep hygiene: - Sleeping tablets - Benzodiazepines • Hypnotics: temazepam, nitrazepam, restricted 2-4 week use, 2/3 nights/week not daily • Z-meds: zolpidem, zoplicone, zaleplon (same as BDZs) - TCAs - Melatonin |
Anxiety and depression |
|
|
How do antipsychotics work? |
- Dopamine - Increased dopamine in mesocortical and mesolimbic areas linked to psychotic symptoms - Antipsychotics block D2 receptors - Mesocortical/mesolimbic: antipsychotic - Nigrostriatal: movement s/e (extrapyramidal) - Tuberoinfundibular: hyperprolactinaemia |
Antipsychotic prescribing and monitoring |
|
|
Typical antipsychotic doses |
- Chlorpromazine: 300mg - 1000mg - Trifluoperazine: 10mg - 50mg - Haloperidol: 3mg - 20mg - Sulpiride: 800mg - 2400mg |
Antipsychotic prescribing and monitoring |
|
|
Extrapyramidal s/e |
- Muscle spasms (dystonia) - Parkinsonian tremor, joint stiffness - Disturbance of DA/Ach balance in nigrostriatal pathway - Lower dose - Use anticholinergic - dry mouth, blurred vision, constipation, urinary hesitancy, confusional states [procyclidine, orphenadrine] - Switch to atypical |
Antipsychotic prescribing and monitoring |
|
|
Tardive Dyskinesia |
- Facial and tongue movements, tongue protrusion, grimacing, quick jerky limb movements - Can be irreversible, prompt recognition is essential - Long term antipsychotic usage - Upregulation and increased DA receptor sensitivity? |
Antipsychotic prescribing and monitoring |
|
|
Tubero-infundibular pathway |
- Hyperprolactinaemia - Galactorrhoea - Amenorrhoea - Fertility issues - Bone demineralisation - Gynaecomastia - Sexual dysfunction - Weight gain |
Antipsychotic prescribing and monitoring |
|
|
Atypical Antipsychotics doses |
- Amisulpride: 400-1200mg - Aripiprazole: 15-30mg - Olanzapine: 10-20mg - Quetiapine: 300-750mg - Risperidone: 4-16mg |
Antipsychotic prescribing and monitoring |
|
|
Atypical antipsychotic s/e |
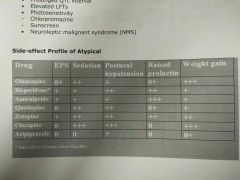
- Weight gain - Raised blood sugar level - Type-2 diabetes - Seizures - Hyperprolactinaemia - Blood dyscrasias (neutropenia) - Raised lipids - Cardiac arrhythmias - Prolonged QT interval - Elevated LFTs - Photosensitivity - Neuroleptic malignant syndrome |
Antipsychotic prescribing and monitoring |
|
|
Receptor activity profiles of antipsychotics |
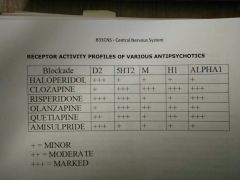
|
Antipsychotic prescribing and monitoring |
|
|
Rapid Tranquillisation |
- Quickly control extreme agitation, aggression, violence that put individual and others at risk of physical harm - Sedate person to minimise risk without person losing consciousness - Haloperidol + Promethazine - Lorazepam Antipsychotics risk: - Excessive sedation - Loss of consciousness - Respiratory depression/arrest - CV complications/collapse - Seizures - Akathisia (restlessness) - Dystonia (muscle contractions) - Dyskinesia (tremor) - Neuroleptic malignant syndrome BDZs risk: - Excessive sedation - Loss of consciousness - Respiratory depression/arrest - CV collapse > Access to flumazenil |
Antipsychotic prescribing and monitoring |
|
|
Treatment-resistant SZ + Clozapine |
- Ineffective 2x antipsychotics (1x atypical) for at least 6-8 weeks - Explore reasons for failure Clozapine: - Full blood count - Weekly bloods first 18 weeks - Fortnightly bloods to 1 year - Then monthly bloods > Bone marrow suppression - CI with other drugs causing bone marrow suppression - Metabolised by c1A2 and c2D6 > smoking induces enzymes - faster metabolism - Drowsiness - Hypertension/hypo + dizziness - Increased HR - Raised body temp - Hypersalivation >> Gradual dose titration If clozapine does not work: - At least 6 month assessment - Gradually increase dose - Monitor plasma conc. - Augment with 2nd antipsychotic |
Antipsychotic prescribing and monitoring |
|
|
Antipsychotic patient monitoring |
Baseline investigations: - Weight, BMI, waist circ. (weight gain) - Pulse, BP, glucose, lipids - Prolactin - ECG if CV risk - Movement disorders? - Nutritional status, diet, physical activity - Smoking? Routine monitoring: - Response - s/e - Weight + waist circ. - Pulse/BP - Blood glucose/lipids - Adherence - Physical health - 'Shared-care' w./ GP |
Antipsychotic prescribing and monitoring |
|
|
Good antipsychotic prescribing |
- Record indication, benefits/risks, expected response time - Lower dose, slowly titrate - Therapeutic trial for 4-6 weeks - Justify dose above BNF recommendations - Record rationale for changes - Avoid polypharmacy, except short period |
Antipsychotic prescribing and monitoring |
|
|
Parkinson's introduction |
- Neurodegenerative: death of dopamine-containing cells of substantia nigra (in basal ganglia) - Substantia nigra: origin of dopaminergic afferents implicated in Parkinson's |
Parkinson's Disease |
|
|
Parkinson's Pathophysiology |
- Dopamine neuron loss in substantia nigra - Loss of noradrenergic and serotonergic neurons - Accumulation of protein deposits in substantia nigra, locus coeruleus and other brain regions > Lewy body |
Parkinson's Disease |
|
|
Parkinson's Aetiology - Genetic |
- Earlier age of onset, greater familial occurrence - 15-25% have relative with Parkinson's - Odds increased if parent or sibling a-Synuclein - autosomal dominant - Major constituent of Lewy bodies - Too much or abnormal a-Synuclein produced ? Inhibit NT release LRRK2 - autosomal dominant - Leucine-rich repeat kinase 2 - ~2% of Parkinson's in Western Parkin - autosomal recessive - aka Juveline Parkinsonism <30yo - Acts as a ubiquitin-protein ligase (labels cells for metabolism) - Portrayal of a protective role |
Parkinson's Disease |
|
|
Parkinson's Aetiology - Environmental |
Rural: - Pesticides known to be potent mitochondrial inhibitors - Mitochondrial complex 1 extracts energy from NADH - Complex deficient in patients who had Parkinson's - Insecticide rotenone in rats caused dopaminergic cell death, Lewy bodies, motor deficit MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) - Synthetic form of heroin MPPP - Parkinson's symptoms, responsive to treatment - Death revealed destruction of substantia nigra (less DA neurons) but lacking in Lewy bodies Ageing: - Increased prevalence in older - Loss of striatal DA and DA cells in substantia nigra - Precise role unclear |
Parkinson's Disease |
|
|
Parkinson's Motor Symptoms |
- Bradykinesia (slowness of movement) - Resting tremor - Rigidity - Postural instability - Drooling - Fatigue - Loss of facial expression - Speech problems - Dysphagia (swallowing issue) |
Parkinson's Disease |
|
|
Parkinson's Non-Motor Symptoms |
GI dysfunction - Constipation - Incomplete bowel evacuation/incontinence Genitourinary dysfunction - Urinary urgency, frequency, incontinence - Sexual dysfunction CV dysfunction - Cardiac sympathetic denervation > orthostatic light-headedness + hypotension - Postural hypotensions > DA medication Cognitive dysfunction - Slowness of thought and executive dysfunction Sleep disorder - Rapid eye movement disorder - Restless legs syndrome - Periodic limb movement of sleep - Insomnia - Excessive daytime sleepiness Mood disorders - Depression - Psychosis - Anxiety Pain - Muscularskeletal - cramp, ache, skeletal deformities - Radicular neuropathic - into lower extremities - Dystonic - neck muscles, medication cause - Central/primary - 'stabbing', 'burning', scalding pain |
Parkinson's Disease |
|
|
Parkinson's Pharmacological Treatment |
- Replenish DA - Prevent, delay, reverse neurodegeneration
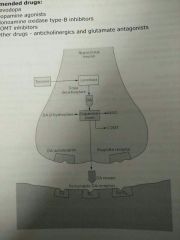
- Levodopa, DA agonist, MOA-B inhibitors, COMT inhibitors - Anticholinergics, glutamate antagonists
- Levodopa first-line - Against bradykinesia and rigidity - Levodopa > DA via DOPA-decarboxylase - With DOPA-decarboxylase inhibitor, reduce peripheral s/e
- DA agonists (ropinirole, pramipexole) - First line in younger due to reduced motor complications - Combination with levodopa - Agonists for D2 and D3 post synaptic receptors - Nausea, sleepiness, dizziness, hallucinations (↑DA)
- MOA-B inhibitors (selegiline, rasagaline) - Prevents degradation of DA - excitement, anxiety, insomnia, generally well tolerated
- COMT inhibitors (entacapone) - Prevents degradation of DA - Effective in advanced Parkinson's
Levodopa + Carbidopa + Entacapone > Stalevo (Improving compliance) |
Parkinson's Disease |
|
|
Other Parkinson's Drugs |
Amantadine - Initially anti-viral - Mild anti-parkinsonian - Unclear mixed dopaminergic + anti-glutamatergic actions - Confusion/insomnia Antimuscarinics (benzhexol) - Inhibit dopamine suppression > compesnatory for ↓DA |
Parkinson's Disease |
|
|
Parkinson's Non-Motor Management |
GI dysfunction - Constipation: osmotic laxative (macrogol) Cognitive dysfunction - Dementia: rivastigmine (hallucinations >> amnesia) Mood disorders - Depression: DA agonist, TCA, SSRIs - Psychosis: Atypical antipsychotics |
Parkinson's Disease |
|
|
Parkinson's Surgical Management |
Deep brain stimulation - Excellent response to levodopa - Young - No/mild cognitive impairment - Absence/well controlled psychiatric disease - Permanent implantation of leads into subthalamic nucleus or globus pallidus - Deliver high frequency electrical impulses controlled by stimulator - Alleviate motor symptoms - Decrease levodopa dose |
Parkinson's Disease |
|
|
Parkinson's Non-Pharmacological Management |
Cell replacement therapy - No current available - Research: embryonic, mesenchymal - Effective restoration of DA release in vivo Exercise/physiotherapy - Dance, martial arts adjunct - ↓DA degeneration when forced to use limb Vit D - Low in Parkinson's patients - Bone health - Related to severity - Neuroprotective in animal studies |
Parkinson's Disease |
|
|
Parkinson's Treatment Complications |
Levodopa - Decreasing dose with adjuncts - DA agonist, MAO and COMT inhibitors Dyskinesia - Involuntary writhing - Amantadine or clozapine Fluctuations in clinical state - Hypokinesia (decrease body movement) and rigidity worsening then improve - Levodopa-SR or + COMT inhibitor > stable plasma levels Nausea - Administer with food, Domperidone DA agonists - Implusive compulsive behaviour: exacerbated in patient with OCD - Discontinue/reduce DA agonist - Anticonvulsant zonisamide ↓implusive behaviour Clozapine - Psychosis: improve - Blood monitoring > agranulocytosis |
Parkinson's Disease |
|
|
Comorbidities of Parkinson's |
Depression - Widespread in patients with early onset - Symptom overlap - Abnormalities of serotonergic, noradrenergic and dopaminergic function - Antidepressants Cognitive impairment - Cholinergic dysfunction over time - Acetylcholinesterase inhibitor (rivastigmine) Orthostatic (postural) hypotension - Autonomic dysfunction or adverse effect of dopaminergic medication - Corticosteroid, Cholinesterase inhibitor, NSAID - Increase salt + fluid consumptom ↑BP, monitor for hypertension |
Parkinson's Disease |
|
|
Anaesthesia introduction |
- Provision of insensibility to pain during surgical, obstetric, therapeutic and diagnostic procedures - Monitoring and restoration of homeostasis during postoperative period - Application of pharmacology, pathophysiology, biotechnology |
Anaesthetics |
|
|
Local anaesthetics (LAs) |
- Block generation and conduction of nerve impulses at local contact site - Consciousness maintained - Lignocaine, bupivacaine, ropivacaine - Topical: nasal mucosa, wound margins - Infiltration: vicinity of peripheral nerve endings and major nerve trunks in dental - Regional: intravenous injection leading to numbing of large area |
Anaesthetics |
|
|
Mechanism of action of LAs |
- Charged LA blocks voltage-gated Na+ channels - No Na+ influx - No depolarisation - No action potential generated |
Anaesthetics |
|
|
General anaesthetics (GAs) |
- Alters central neural processing - Readily reversible loss of consciousness with ↓response to painful stimuli + muscle tone - Inhalation + intravenous - 'Knock-out' blows to head - Carotid artery compression - Ingestion of ethanol and herbal mixtures |
Anaesthetics |
|
|
Stages of anaesthesia |
A: Induction: Inhalation or IV B: Maintenance: volatile agents C: Recovery: monitoring |
Anaesthetics |
|
|
Depth of anaesthesia |
I - Analgesic stage - ↓higher cortical function - Consciousness not lost, but thoughts blurred - Reflexes present - Smell and pain lost at end stage II - Excitement stage - Cortical inhibitory centres depressed - Increased muscle tone - Vomiting - Temperature control lost - Arhythm of EEG desynchronised - Respiration increased/irregular III - Surgical anaesthesia stage - Slow syncronised EEG rhythms - Regular slow breathing - Medullary centres depressed - respiration > artificial ventilator - Reflexes lost - Pupils dilated IV - Medullary paralysis stage - Loss of respiration - EEG waves > small > lost - Death |
Anaesthetics |
|
|
Types of GA |
Inhalation Gas - Nitrous oxide Volatile liquids - Halothane - Enflurane - Isoflurane - Sevoflurane - Desflurane IV Inducing - Methohexitone/methohexital - Propofol - Etomidate BDZs - Diazepam, lorazepam, midazolam Dissociative anaesthesia - Ketamine |
Anaesthetics |
|
|
Ideal Inhalation anaesthetic |
- Stable over range of temps - Not degraded by light - Odourless - Analgesic, anti-emetic, muscle relaxation - Minimal respiratory depression - Minimal CV effects - Excreted completely by respiratory system - Not metabolised and no active metabolites |
Anaesthetics |
|
|
Potency of inhalation anaesthetics |
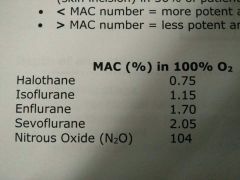
- Minimum alveolar concentration (MAC) - Inhaled dose that prevents movement to a standard surgical stimulus (skin incision) in 50% patients - ↓MAC = more potent; ↑MAC = less potent
|
Anaesthetics |
|
|
Journey of inhalation anaesthetic I |
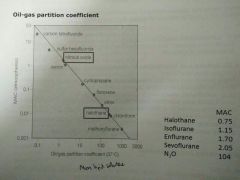
- Anaesthetic gains access into alveoli - Partial pressure important in driving anaesthetic from respiratory > brain - Steady state for maintenance, dependent on partial pressures of alveoli, blood, brain
- Higher MAC, more lipid soluble |
Anaesthetics |
|
|
Journey of inhalation anaesthetic II |
Phase I: anaesthetic wash-in - Equilibrium between gas present in functional residual capacity and anaesthetic Phase II: uptake + distribution - Blood-gas partition coefficient • High = greater amount of anaesthetic must be dissolved in arterial blood to equilibrate alveoli • Low = minimal amount to equilibrate • Relevance: influence speed of anaesthetic induction where NO quickly saturates blood - Cardiac output • High = faster removal from alveoli to peripheral, slow access to brain • Low = slower removal, faster to brain • Relevance: influence speed of induction - Alveolar-to-venous partial pressure gradient of anaesthetic • Transferred to peripheral tissues from arterial blood due to pressure gradient • Depleted venous returns to lungs with more gas moving into blood due to gradient • > concentration difference, higher uptake, slower induction Phase III: uptake and distribution to brain - Steady state to maintain (alveolar-arterial-brain) - Cerebral blood flow • As brain is highly perfused, rapidly achieves steady state with partial pressure of blood anaesthetic Phase IV: elimination/recovery - NO exit faster than halothane - Minimal amount dissolved |
Anaesthetics |
|
|
Journey of IV anaesthetic |
- Bloodstream, binds to plasma proteins or remains unbound - Venous blood > systemic > cerebral circulation - Partial pressure gradient permits entry to brain = effect - Unbound, lipid soluble, unionised molecules cross BBB quickest |
Anaesthetics |
|
|
IV anaesthetics |
Propofol - Short acting, 30sec onset, rapid recovery - ↓BP + intracranial pressure - No analgesia - Excitatory phenomena - muscle twitching, yawning, hiccups - Some antiemetic in post Thiopental - 1min onset - Apnoea, coughing, chest wall spasm, laryngospasm, bronchospasm - Better tolerated agents Etomidate - Hypnotic: anaesthesia but no analgesia - No CV effects - Used in CV dysfunction Ketamine - Unconscious but appears awake, amnesia - dissociative anaesthesia - ↑BP + cardiac output - Bronchodilator - Not for young > hallucinations |
Anaesthetics |
|
|
Mechanisms of action of GAs |

Agonise inhibitor receptors - GABA-A (GABA/Cl-) - Strychnine-sensitive glycine (Glycine/Cl-) Antagonise excitatory receptors - 5HT3 (5HT/Na+) - Nicotinic (Ach/Na+) - NMDA/AMPA (Glut/Na+)
- Uncharged anaesthetic molecules concentrate in lipid membranes, causing membrane expansion |
Anaesthetics |
|
|
Target site for GA |

|
Anaesthetics |
|
|
Practical anaesthesia |
No single agent is ideal - Premed: atropine ↓secretions; BDZs: sedation - Fast induction: thiopental (IV) - Maintain: isoflurane (inhalation) - Muscle relaxation: neuromuscular blocking drug - Reduce pain: analgesic (opiate); post-op |
Anaesthetics |
|
|
Exelon Patch |
- Only Alzheimer's treatment as patch - 24hr treatment, better compliance - Overcomes swallowing problems - Reduced s/e to oral 1. Backing layer 2. Drug in adhesive layer 3. Contact adhesive layer (stick) 4. Release liner - Rivastigmine susceptible to oxidation, light + humidity degradation in patch - Packaged in sealed pouches to protect from light + humidity - Replace air with inert gas such as nitrogen (↓ oxidation) - Include antioxidant in formulation - exelon uses alpha-tocopherol (Vit E) - peroxide and free radical scavenger |
Novel Formulations for Drug Delivery |
|
|
ADHD/ADD Formulation |
- Methylphenidate: control behaviour
- Immediate release: • 2-3 times a day • Compliance issues • Abuse potential • Social stigma at school - Extended release: • Single dose • Better social acceptance • Less control at end of day > accending release (osmotic drug delivery) |
Novel Formulations for Drug Delivery |
|
|
Novel drug delivery to brain |
Glioblastoma multiforme - One of most rapidly progressive brain cancer - Uniformly fatal disease - Carmustine or BCNU has short plasma half life and is extremely toxic - IV requires crossing BBB - Radiotherapy 14 days after surgery - Biodegradable poly(anhydride) polymer wafer implant at tumour - Degrades by surface erosion - cannot be too hydrophobic otherwise only surface erosion - Labile anhydride group, hydrophobic monomer - Place after removal of tumour - more drug delivered at sites required, polymer protects BCNU |
Novel Formulations for Drug Delivery |
|
|
BBB ADME |
- Extreme form of lipid barrier with: • Few intercellular pores • Numerous tight junctions • Surrounded by glial cells - Lipid soluble drugs penetrate: access to brain + CNS effects - Water soluble/polar drugs have limited access - Sedating antihistamines have access > CNS effects - BBB less effective in meningitis > allows more drugs to pass through >> treatment too - Can give antibiotics that do not normally pass through - benzylpenicillin |
ADME |
|
|
Domperidone vs metoclopramide |
- Both anti-emetics - Both DA receptor antagonists - Metoclopramide penetrates BBB and can cause drug-induced Parkinsonism, Domperidone does not - more charged |
ADME |
|
|
Intrathecal |
- Access to CNS is tightly regulated - Chemo can be intrathecal to achieve drug access to CNS - Injected in CSF and reaches brain - This has lead to fatal drug administration errors (Vincristine instead of methotrexate = fatal) |
ADME |
|
|
Single compartment model |
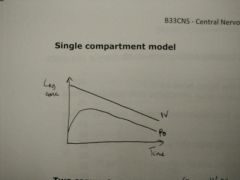
|
ADME |
|
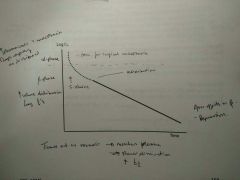
Two compartmental model |
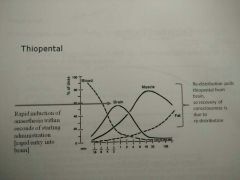
- Some IV GAs (thiopental) - Induction anaesthetic given by IV infusion, then replaced with maintenance anaesthetic - Highly lipid-soluble drug - Unconsciousness occurs within 20secs and lasts for 5-10mins - Elimination half-life = 10hrs - Tissue acts as reservoir - re-enters plasma > slower elimination - Redistribution pulls thiopental from brain so recovery to consciousness is due to this |
ADME |
|
|
Zero order kinetics |
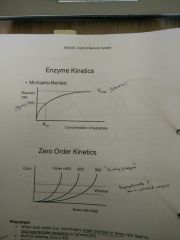
- Most drugs show 1st order kinetics - rate of elimination proportional to [drug] - But some (phenytoin, ethanol) the enzymes become saturated so the rate of elimination is no longer proportional to [drug] |
ADME |
|
|
Phenytoin |
- When zero order (non-linear) small changes in dose rate lead to disproportionate increases in [phenytoin] - Normal loading (Css x Vd) - Maintenance dose: (SxFxDose/t)=(Vmax x Css)/Km + Css |
ADME |
|
|
Pregnancy and anti-epileptics |
- Need tobe maintained during pregnancy to prevent seizures: benefits vs risks - Phenytoin - Craniofacial abnormalities - Hyoplasia of distal phalanges - Growth deficiency - Mental deficiency - Valproate - Neural tube defects - Learning difficulties - Carbamazepine - Similar to phenytoin but decreased risk - Continuation of treatment preferable - Or planned discontinuation - Carbamazepine preferred - 5mg folic acid to reduce chances of neural tube defects - NICE: lamotrigine first line generalised tonic-clonic seizures to avoid teratogenic/interacting drugs - Lamotrigine favoured but PK are altered in pregnancy making it more difficult to use * AVOID PHENYTOIN and VALPROATE |
ADME |
|
|
Pregnancy and anti-depressants |
- Depression: 20% of pts in pregnancy - SSRIs (especially citalopram and sertraline) associated with cardiac septal defects - Increased risk in 1st trimester |
ADME |
|
|
Foetal Alcohol Syndrome |
- Thin upper lip - Short palpebral tissues - Flat nasal bridge - Short nose - Elongated philtrum - Microcephaly - Mental retardation - Cardiac malformations - Joint malformations |
ADME |
|
|
CNS Drug interactions |
- Many CNS drugs are long term - CNS often lead to sedation - enhanced by alcohol - Some anti-epileptics are enzyme inducers: Oral contraceptives - CYP450 inducing agents lead to failure > no protection > Phenytoin > Carbamazepine > Phenobarbital = inducers - Favour non-inducing agents or use alternative contraceptive methods - Lamotrigine: oral contraceptives can reduce plasma concentrations of lamotrigine - caution dose |
ADME |
|
|
Serotonergic syndrome |
Clinical features - Headache - Confusion - Nausea - Twitching - SSRIs and 5HT1 agonists (triptans) lead to ↑5HT St John's Wort - SSRI-like actions - Can cause serotonergic syndrome if used with SSRIs - Enzyme inducer can affect: - Oral contraceptives - Anti-HIV - Ciclosporin (immunosuppression for organ rejection) |
ADME |
|
|
Lithium |
- Bipolar disorder - Narrow therapeutic window - Plasma concentration determined by eGFR and electrolyte balance - Therapeutic Drug Monitoring: 0.4-1mmol/L |
ADME |
|
|
Commonly Encountered Mental Health Problems |
- Mood disorders: depression, bipolar - Anxiety: OCD, agoraphobia, panic - Psychoses: SZ - Substance misuses/addictions - Personality disorders - Neurodevelopmental disorders: ADHD, Aspergers - Others: dementia, somatoform disorders |
Talking therapies/ placebo effect |
|
|
Treatment of Mental Health Problems |
- Holistic approach - Biopsychosocial model - Biomedical: medication, ECT - Psychological: talking therapies - Social: occupational therapy, social inclusion, wellbeing |
Talking therapies/ placebo effect |
|
|
Psychological-therapeutic talking interactions |
- Self help groups - GP consultation - Everyday social networks - Friends and family - Formal psychotherapy with trained therapist - Internet, books (self-help) - Counselling |
Talking therapies/ placebo effect |
|
|
What are talking therapies? |
- AKA Psychotherapies, Psychological Therapies, Counselling - Use of language/verbal interaction - Many involve face-to-face interaction with therapist, some self-help - May be 1:1, group work, couples, families - Aim to offer support to improve an indentified difficulty or distress - Explore thoughts, feelings (moods) behaviour, look for patterns - Reflect, understand, evaluate, move forward - Many different types/models |
Talking therapies/placebo effect |
|
|
General Principles of Talking Therapies |
- Formalised structure-time, venue, number of sessions, ground rules and boundaries - Patient understands and agrees to work with model, motivated to participate - Often, motivation to work outside the therapy session - Requires the patient to be an active participant, rather than passive recipient of care - More than 'just talking' - Facilitate patient ultimately to be own therapist - Trusting therapeutic relationship very important |
Talking therapies/placebo effect |
|
|
Who are Talking Therapies for? |
- Bereavement, anxiety, chronic pain, smoking, depression, substance misuse, personality disorder - CBT - Psychodynamic psychotherapy - Supportive psychotherapy - Mindfulness based cognitive therapy - Motivational interviewing - Dialectical behavioural therapy - Select carefully, some therapies are not indicated for some conditions, insufficient evidence base, may be harmful - Careful assessment of patient suitability before committing |
Talking therapies/placebo effect |
|
|
Cognitive Behavioural Therapy (CBT) |
- Views of self, world, future - How behaviour, thoughts, physical feelings and mood affect each other - Aim: Identify unhelpful cycles of thought, mood, behaviour (and physical feelings) and consider how these cycles may be broken - Depression, anxiety, psychoses, anger, bulimia, low self-esteem, chronic physical health problems - Delivery: time limited to face to face sessions, self-help - Explain model - Agree time (frequency, time, length, how many, venue) - Boundaries (who to contact if unwell between appointments, confidentiality) - Identify difficulties, goals - Begin to identify unhelpful vicious cycles and triggers - 'Homework' - On return, review homework - Encourage patient to find own solutions and devise 'experiments' - Regular review of progress - Patient may keep notes/workbook for future reference - Speed of progress will depend on individual patient |
Talking therapies/placebo effect |
|
|
Mindfulness Based Cognitive Therapy |
- Mindfulness: meditation, Eastern philosophies - Mindfulness/cognitive therapy exercises combine to help manage problems with depression + stress - Increased awareness of 'here and now' - Being aware of, but neither engaging with nor actively dismissing the thoughts that arise - looking at thoughts/worries from outside perspective - Other ways of experiencing consciousness than thought - 'Present' more of the time - Enable to notice and disengage from negative thoughts - More kindness to self - Vulnerable to recurrent depression - Longstanding depression symptoms - Stress - Staff in-reduce stress, better clarity of mind, problem solving, mood regulation - Mostly group sessions, secondary care - Books + internet - NICE: recurrent depression |
Talking therapies/placebo effect |
|
|
Psychodynamic Psychotherapy |
- Emotional and relationship problems - Pain from past - hidden, still affects emotions/behaviour/relationships in present - Depth psychology - primary focus to reveal unconscious content of patients mind to facilitate alleviation of psychological tensions and distress - Gain insight, understanding of dysfunctional patterns, work through them - Patient talks, safe environment - Therapist 'blank screen', transference of feelings from significant person in past onto therapist - Interpretations - Interations in therapy mirror those with significant figures in past and present behaviour patterns outside therapy • Freud-psychoanalysis • Jung, Klein, others • Length - month to years • 1:1 group, family • 50 mins, often weekly • Careful assessment of suitability - Psychologically minded, committed - Unsuitable if chaotic, fragile sense of self, risk of decompensation or psychosis |
Talking therapies/placebo effect |
|
|
Talking Therapies + NICE |
- Talking therapies for many mental health problems - CBT - phobias, depression, OCD, eating disorders, PTSD, long term illness, psychosis - Mindfulness - recurrent depression |
Talking therapies/placebo effect |
|
|
Access to Talking Therapies |
- Self-help, computers, library - Increased access to psychological therapies, primary care - Mental health services (CBT, specialised CBT, MBCT, dynamic psychotherapy) - Private providers - various, may increase |
Talking therapies/placebo effect |
|
|
IAPT (Improving Access to Psychologcal Therapies) |
- Government aim to provide NICE compliant psychological services for all ages - First line referral for mild to moderate depression and anxiety - With or w/o medication - Aims to reduce long term costs - Not appropriate for severe, complex illness or high risk (suicidality) |
Talking therapies/placebo effect |
|
|
What goes wrong during a seizure? |
- Abnormal hyper-synchronised activity within a neural network - There are many different types of epileptics seizure - Different seizures vary according to: • Circuits involved • Likely cause • Drugs used • Chance of cure |
Epilepsy |
|
|
Why are some people prone to seizures? |
- Brain lesions and disorders of channels and receptors - Many different epilepsies - Vary a great deal as to outcome |
Epilepsy |
|
|
How do anti-epileptics work? |
Target neuronal channels and NT receptors - Na+, K+, Ca2+ - GABA, Glut - SV2a - Cannabinergic mechanisms |
Epilepsy |
|
|
What is a seizure? |
The clinical manifestation of a disordered and hypersynchronised discharge in a network of cerebral neurons - Patient and witness history - Home videos of seizures - Combined video-EEG - Result > Classification of seizures - Location of onset - Type of discharge - Pattern of spread |
Epilepsy |
|
|
Types of seizures |
- Generalised seizures - simultaneously in both hemispheres • Typical absence • Myoclonic • Tonic-clonic - Focal seizures - start in a focus then spreads |
Epilepsy |
|
|
Absence Seizures |
- Mainly childhood onset - Frequent brief attacks (1-30secs) - Sudden loss and return of consciousness - No aura and no post-ictal state - Some involuntary movements |
Epilepsy |
|
|
Myoclonus |
- Sudden, brief, shock-like muscle contractions - Usually bilateral arm jerks - Often worse in the mornings - Precipitated by sleep deprivation and alcohol - Occurs in: • Epilepsy syndrome (JME) • Certain non-epileptic causes (CJD) |
Epilepsy |
|
|
Tonic-Clonic |
- Sudden onset, gasp, fall - Tonic phase with cyanosis (stiff) - Clonic phase (shaking) - Post-ictal phase (confused, muddled, tired) -Tongue bitten and incontinence - Noisy breathing - Headache and muscle pain afterwards |
Epilepsy |
|
|
Uncommon generalised seizures |
- Atypical absence - Tonic - Atonic Usually associated with severe epilepsy |
Epilepsy |
|
|
Focal (Partial) seizures |
- Focal onset means there is often an aura - As seiures spread a 'complex partial seizure' develops with loss of awareness and automatisms - Simple partial: awareness present - Complex partial: awareness lost - Secondary generalised: evolves to tonic-clonic - Temporal Lobe - Frontal lobe - Occipital lobe - Parietal lobe Onset zone determines symptoms |
Epilepsy |
|
|
Temporal Lobe (Focal) |
Auras - Epigastric rising sensation - Olfactory and gustatory - Deja vu Complex partial seizure - Arrest reaction and blank stare - Oral automatisms (lip-smacking) - Manual automatisms |
Epilepsy |
|
|
Pathophysiology of epilepsy |
- Neurophysiology of seizures: what happens in a neuronal network during a seizure? (Ictogenesis) - What changes make a brain epileptic: what molecularchanges make a group of neurons liable to seizures (Epileptogenesis) |
Epilepsy |
|
|
Key regulators of neuronal excitability |
- Non gated ion channels - Voltage gated ion channels - Ligand gated ion channels - Metabotropic receptors - Glia - Neuro-modulators (endocannabinoids, hormones) |
Epilepsy |
|
|
Non-gated ion channels |
Resting membrane potential |
Epilepsy |
|
|
Voltage-gated ion channels |
- Na+, K+, Ca2+, Cl- - Dendrite information processing - Action potential and repolarisation • Excitatory: depolarisation • Inhibitory: hyperpolarisation - Regular firing - Burst firing > excessive in epilepsy |
Epilepsy |
|
|
Ictogenesis |
- The inter-ictal spike: a short burst of epileptiform activity lasting 200ms - A seiure: a more prolonged event lasting many seconds - Micro-domains: possible basis of focal seizures - High frequency oscillations (ripples) |
Epilepsy |
|
|
Focal epilepsy: inter-ictal spikes |
- Characteristic of EEG signature of focal epilepsy (but is not a seizure) - Lasts about 200ms, paroxysmal depoarlisation shift (PDS) |
Epilepsy |
|
|
How does neural activity differ from normal? |
- Burst firing behaviour of neurons - Hyper-synchronised firing of networks |
Epilepsy |
|
|
Micro-domains |
- Decreased inhibitory leads to spread of excitatory |
Epilepsy |
|
|
Cortico-thalamic loops |
Sensory input: 1. Sensory information > Thalamic relay cell > Cortex > thalamic relay cell 2. Thalamic relay cell > thalamic reticular cell > thalamic relay cell 3. Lots of inter-neurons also |
Epilepsy |
|
|
Firing of thalamic neurons |
1. Tonic mode 2. Burst mode |
Epilepsy |
|
|
Intra-thalamic loops |
Connections bewteen regions of brain |
Epilepsy |
|
|
Absences: some observations |
- Making cortex hyper-excitable with penicillin causes spike and wave - Stimulating frontal cortex or intra-laminar thalamic nucleus causes spike and wave - During human spike and wave discharges can be recorded in thalamus |
Epilepsy |
|
|
Absences: pathophysiology |
1. Connections between thalamus - cortex contains loops 2. Connections within thalamus contain loops 3. The membrane and synaptic properties of neurons in these loops cause oscillations 4. Distrubances of these oscillations may cause spike and wave firing |
Epilepsy |
|
|
What goes wrong in absence seizures? |
- Not fully understood - Primary abnormality may be bursts of abnormal activity from cortex to thalamus - Thalamus may have a role in synchronising - Reticular nucleus inhibiting TC relay cells may underlie 'absence' - Low threshold 'T' Ca channel may play a role |
Epilepsy |
|
|
Other seizure types |
- Tonic-clonic: basal ganglia/brain stem involved in seizure, substantia nigra has gating function for severity of seizure |
Epilepsy |
|
|
Epileptogenesis: what changes occur? |
- Neuronal channels: Na, K, Ca, Cl, HCO3 - Receptors: GABA, AMPA, NMDA, ACh - NT transporters - Neuromodulators (peptides + endocannabinoids) - Gap junctions - Glia: buffering of extracellular environment - BBB and inflammation - Loss and reorganisation of synapses - Cell loss inhibitory (interneurons and new neurons - Inherited channel defeccts can cause epilepsy (GEFS+ and Dravet syndrome) - Some acquired epilepsies show changes in dendritic channel functions |
Epilepsy |
|
|
Channelopathies and epilepsy |
- NA+ GEFS+ SMEI increased Na - K+ familial neonatal convulsions - Ca2+ involved in CAE? - Cl- in JME? - Nicotinic ACh receptor - GABA gated Cl- channel: families of JME |
Epilepsy |
|
|
Acquired Channelopathies of epilepsy |
- Animal models of TLE associated with K+ and HCN channelopathy of dendrites - Na+ channels in epileptic animals may become somewhat resistant to blocking effects of carbamazepine, phenytoin and lamotrigine |
Epilepsy |
|
|
Sodium channels |
Resting state (closed) > Activated state (open) > Inactivated state - Action potentials - Transmitter release - Subthreshold neuronal properties Na channels are anti-epileptic target - Use and voltage dependent - Prolongs inactivated state of channel - Block increases with repetitive activation - Reduces burst firing - Drugs bind poorly to resting Na+ channel - Fast inactivation (normal) not affected - Binding with prolonged depolarisations - The onset of block is slow, allowing some bursting to occur (spikes still occur) - Main action may be to stop spread of seizure -Persistent Na current may be important in epilepsy - Some antiepileptics slectively bind to Na(p) - Lacosamide - Some epilepsies caused by mutations in Na channels with increased NaP (gain of function) - Outcome of mutations quite hard to predict given the distribution of different Na channel subtypes across the neuron and across inhibitory versus excitatory neurons - Some brain lesions causing epilepsy may have I NaP channels (acquired channelopathy) - Patients with loss of function mutations in Na channels might have epilepsy worsened by lamotrigine - Genetic differences in sensitivity to antiepileptics |
Epilepsy |
|
|
GABA receptors |
-Some antiepileptics promote inhibition by enhancing Cl- current at GABA receptors - Some reduce GABA degradation or reputake • Vigabatrin: GABA transaminase inhibitor • Tiagabine: GABA reuptake inhibitor |
Epilepsy |
|
|
Other antiepileptics |
- Retigabine augments potassium channel > withdrawn due to possible retinal s/e - Perampanel blocks AMPA receptor - Some antiepileptics are poorly understood (valproate, gabapentin, pregabalin, levetiracetam) |
Epilepsy |
|
|
Epilepsy Management |
- Many implications with being epileptic - Ensure correct diagnosis - Determine cause - Decide on treatment - Lifestyle issues - Videos? - Cause of blackouts • Fainting • Cardiac issues • Attacks with psychological causes • Rarities Epilepsy syndrome - Seizure type - EEG results - MRI findings - Family history - Associated causes > treatment and prognosis |
Epilepsy |
|
|
Types of epilepsy |
Idiopathic epilepsies - No associated neurological damage - Often respond well to treatment - Genetic component suspected Symptomatic epilepsies - More treatment resistant - May have associated neurological deficits - Cortical malformations - Cerebral palsy - Genetic and metabolic disorders - Hippocampal sclerosis - Trauma and infection - Tumours/Stroke - Classification under revision |
Epilepsy |
|
|
Generalised Epilepsy Treatment |
- Sodium valproate - Lamotrigine |
Epilepsy |
|
|
Focal Epilepsy Treatment |
- Lamotrigine |
Epilepsy |
|
|
Lamotrigine |
- Broad spectrum - Very often now used first line - Focal and generalised - May be helpful for myoclonus and absences - Well tolerated - Serum levels drop with combined oral contraceptives + pregnancy |
Epilepsy |
|
|
Carbamazepine |
- Acts at Na channels - Suppresses burst activity and spread of seizures - 1st line for partial and generalised seizures - Not helpful fr myoclonus and absences (can exacerbate) - Relatively well tolerated - Interactions due to enzyme induction |
Epilepsy |
|
|
Valproate |
- Uncertain mode of action - GABA, inhibits excitatory transmission? - 1st line for partial and generalised - Powerful against muoclonus, absences and photosensitive seizures - Affects female fertility - Malformation in children - Associated with low IQ and autism |
Epilepsy |
|
|
Phenytoin |
- Acts at Na channels - Supresses burst activity and spread of seizures - 2nd line for partial and generalised seizures - Not helpful for myoclonus and absences - Complex kinetics and interactions - Some important s/e - Useful IV in emergencies - Variable absorption - Rate limiting para-hydroxylation - High protein binding - Some co-medications both induce and inhibit enzymes - Age variability in metabolism |
Epilepsy |
|
|
Levetiracetam |
- Potent broad spectrum - Targets synaptic vescile protein 2a - Well tolerated - No interactions - Mood s/e in 10-20% |
Epilepsy |
|
|
Topiramate |
- Broad spectrum - Multiple mechanisms - Rather prone to s/e: sedation, psychiatric, weight loss |
Epilepsy |
|
|
Clobazam and Clonazepam |
- Useful add-on or occassional use agent - Tendency to tolerance, sedative - Particularly good against absence and myoclonus |
Epilepsy |
|
|
Gabapentin |
- Weak add-on agent for partial - High doses may be required |
Epilepsy |
|
|
Ethosuximide |
- Potent anti-absence agent - Not useful for other - s/e: GI upset, headache, psychiatric disturbances |
Epilepsy |
|
|
Antiepileptic interactions |
Enzyme inducing drugs - Combined oral contraceptive - Antimicrobials - Anti-virals - Analgesics - Oncology drugs - Warfarin Immunosuppressants, psychotropics - Oestogens ↓ lamotrigine CYP inhibitors (erythromycin) - ↑ carbamazepine Other issues - When to start/stop treatment - Bone health - Compliance - Sudden Unexpected Death in Epilepsy |
Epilepsy |
|
|
Withdrawing antiepileptics |
- Withdrawing can lead to relapse of seizures - Better to keep on medication |
Epilepsy |
|
|
Status epilepticus |
- Medical emergency - Rapid treatment: • IV benzodiazepine + phenytoin • IV levetiraceteam or valproate or lacosamide • General anaesthesia Nonpharmacological - Resection of epileptic focus - Vagal nerve stimulation - Ketogenic diet Future treatments - Gene therapy: delivering adenosine, NPY using viral vectors - Deep brain stimulation - Optogenetics: harnessing power of light |
Epilepsy |
|
|
Epilepsy Treatment Summary |
Absence - Valproate - Ethosuximide - Lamotrigine - Benzodiazepines Myoclonus - Valproate - BDZs - Levetiracetam Generalised Tonic Clonic - Carbamazepine - Lamotrigine - Valproate - Phenytoin - Topiramate Focal - Carbamazepine - Lamotrigine - Topiramate - Levetiracetam |
Epilepsy |
|
|
Consequences of epilepsy |
- Loss of driving licence - Loss of employment - Stigmatisation and anxiety - Needing antiepileptics - Problems with contraception and conception - Injuries and mortality |
Epilepsy |
|
|
Understanding epilepsy |
- Seizure = too many brain cells/neurons become excited at the same time (few secs-mins) - Involved parts of brain cannot function normally > movement, sensations, awareness, behaviour - End of seizure = transition back to normal > post-ictal period, gradual improvement - Epilepsy = spontaneously recurring seizures |
Epilepsy YT |
|
|
Types of seizures |
- Partial = electrical discharge in one limited area > spread - Generalised = widespread electrical discharge both hemispheres |
Epilepsy YT |
|
|
Partial/Focal Seizures |
- Simple Partial = awareness, memory, consciousness preserved - Complex Partial = impairment - Aura = signs of bigger seizure incoming - Depends on area and spread |
Epilepsy YT |
|
|
Generalised Seizures |
- Tonic-clonic = cry, stiff (tonic), shaking (clonic) incontinence, drowsiness, confusion, cyanosis > can be only tonic/clonic - Absence = blanks/daydreaming, >30secs/lots of movement = atypical absence - Myoclonic = short jerking/loss of consciousness - Atonic = drop seizure, loss of muscle tone |
Epilepsy YT |
|
|
Causes of epilepsy |
- Common during childhood and elderly - Brain injuries: trauma, infection, injuries, alcohol, drugs, tumours, strokes, malformation - Chemical imbalance: substance, ↓blood glucose, ↓Na/Ca, kidney/liver damage - May remain ideopathic - unknown cause - Genes = generalised Diagnosed through: - Examination - EEG (spikes) - MRI |
Epilepsy YT |
|
|
Dependence Syndrome |
- Strong desire or sense of compulsin to take substance - Difficulties in controlling use (amount, onset, termination) - Physical withdrawal state ? - Tolerance ? - Progressive neglect of other interests, increasing time spent obtaining and taking substance - Persistence with substance despite detrimental effects: social, cognitive, physical |
Reward/drugs of abuse/legal highs |
|
|
Brain Reward Pathways |
- Mesolimbic dopamine pathway (cell bodies in ventral tegmental area, VTA, terminate in the nucleus accumbens, NAC) - Many drugs of abuse increase DA release in NAC > opiates, nicotine, amphetamine, cocaine, cannabis - Enhance serotonin (5HT) function > LSD, Ecstasy - Block NMDA receptors > phencyclidine, ketamine |
Reward/drugs of abuse/legal highs |
|
|
Dopamine + Serotonin Pathways |

Dopamine - Reward (motivation) - Pleasure, euphoria - Motor function (fine tuning) - Compulsion - Perserveration
Serotonin - Mood - Memory processing - Sleep - Cognition
- Drugs of abuse > ↑DA release from VTA neurons - GABA inhibits |
Reward/drugs of abuse/legal highs |
|
|
Bromocriptine |
- DA agonist - Stopping breast milk production > medical reason, incorrect prolactin levels - Treating non-cancerous tumours in brain (prolactinomas) - Treating Parkinson's (↑DA) - Impulse control disorders - Addictive gambling, excessive eating or spending, high sex drive - Also Ropirinole |
Reward/drugs of abuse/legal highs |
|
|
Drugs and dependence liability |
V strong - Morphine (narcotic) - Heroin (narcotic) - Cocaine (Psychomotor stim) - Nicotine (Psychomotor stim) Strong - Ethanol (CNS depressant) - Barbiturates (CNS depress) - Benzodiazepines (Anxiolytic) - Amphetamines (Psychomotor) Moderate - Anaesthetics (CNS depress) - Phencyclidine (Hallucinogen) Weak/absent - Cannabis (CNS depress) - Caffeine (Psychomotor) - Ecstasy? - LSD (Hallucinogen) - Mescaline (Hallucinogen) |
Reward/drugs of abuse/legal highs |
|
|
Opiates |
- Morphine, heroin, methadone, codeine - G-protein opioid receptor agonists, ↓NT in brain/periphery - Analgesia, euphoria, +ve reinforcement, respiratory depression, dysphoria, sedation Acute: - Euphoria, tranquility, miosis, drowsiness, itching, nausea Chronic: - Anhedonia, constipation, depression, insomnia, dependence Withdrawal: - Cold flashes with goosebumps - Kicking movements |
Reward/drugs of abuse/legal highs |
|
|
Cocaine (benzomethylecgonine) |
- Alkaloid extracted from coca tree -Euphoria and excitement, ↑capacity for work - ↑catecholamine NT function by preventing reuptake (DA) - High doses = overactive sympathetic, hypertension, tachycardia, hyperpyrexia, dilated pupil - Strong psycholiglca dependence |
Reward/drugs of abuse/legal highs |
|
|
Amphetamines |
- Phenylethylamine - Increased wakefulness + concentration - Performance enhancing? - ↑monoamine release + ↓reuptake, ↑DA, NA, 5HT - Euphoria, libido, energy, confidence, aggression, power - Chronic/high dose = psychosis - ↑CV tone, ↑BP, ↑HR |
Reward/drugs of abuse/legal highs |
|
|
Cannabis |
- Active agent THC mimics small endogenous lipid messengers - Inhibits NT release via Gi protein-coupled cannabinoid receptors - Mild euphoric effect, dysphoric in high doses - Low acute toxicity, psychosis in heavy users? - Stimulates appetite through hypothalamus + gut |
Reward/drugs of abuse/legal highs |
|
|
Treatment: agonist substitution |
Methadone - Opiate abuse - Long acting synthetic opiate agonist, PO to prevent opiate withdrawal - Blocks effects of illicit opiate use, ↓craving - Stabilised = jobs, avoid crime/violence, ↓HIV Nicotine replacement - Multiple formulations for preference |
Reward/drugs of abuse/legal highs |
|
|
Treatment: antagonist |
Naltrexone - Opiate addiction - Must be detoxified/opiate-free for few days before Mecamylamine - NACh receptor antagonist - Blocks reward of nicotine/cue-induced craving - Antagonist overcome by increased drug dose - Patient non-compliance |
Reward/drugs of abuse/legal highs |
|
|
Treatment: anti-craving |
Acamprosate - Adjunct in maintaining abstinence in alcohol-dependence pts Naltrexone - Reduce alcohol craving by interfering with +ve reinforcement - ↓DA release by blocking opioid disinhibition of GABA |
Reward/drugs of abuse/legal highs |
|
|
Vascular dementia |
- Blood supply to brain interrupted by blocked or diseased vascular system - Reduced cerebral perfusion (strokes), thromboembolism, small blood vessel disease in brain, bleeding - Distinguishable from AD - Confirmed lesions caused by vascular disease through MRI/CT - No approved treatments, treat vascular element |
Alzheimers/dementia |
|
|
Dementia with Lewy bodies |
- Prominence of a-synuclein in DA neurons of substantia nigra (protein deposits found in neurons) - Fluctuating cognition - varying attention/alertness - Visual hallucinations - Movement disorder - Dementia preceding onset of movement disorder by one year - Parkinson's disease dementia = in prescence of existing movement disorder - Cholinesterase inhibitors (↑ACh), NMDA blocker (↓Glut) - Levodopa ↑DA - Antipsychotics CI - Memory prompts, education of caregivers, mobility aids |
Alzheimers/dementia |
|
|
Fronto-temporal dementia |
Frontal lobe - Reasoning, judgement, personality > loss of emotional warmth, apathy, selfishness Temporal lobe - Speech, language, memory > decline in language - Mutation in tau protein (phosphorylation) - Disrupts normal nerve cell processes leading to death |
Alzheimers/dementia |
|
|
AD Pathophysiology |
Beta-amyloid plaques - Beta/gamma-secretase produce harmful protein fragment from amyloid precursor protein - Alpha-secretase normal = amyloid precursor protein > harmless P3 protein fragment Neurofibrillary tangles - Mutation in tau protein cause tangles in microtubules - Affect micronutrient movement > neurodegeneration NT - Cholinergic pathways incolved in cognition/memory - Use ACh as treatment? - Glut = learning - 5HT = mood/psychosis - GABA = anxiety/lethargy - NA = aggression - Significant cell death |
Alzheimers/dementia |
|
|
AD Aetiology: genes |
Icelandic study - Variant of amyloid precursor protein gene Familial AD - Autosomal dominant mutations in chromosome 14,1 and 21 Late onset AD - Isolated apolipoprotein E gene, lipid metabolism and tissue repair, APOE4 > dementia |
Alzheimers/dementia |
|
|
AD Aetiology: environment |
Head trauma - Survivors > ↑amyloid precursor protein > ↑ amyloid plaques Diet/malnutrition - ↑cholesterol = amyloid plaques - Vitamin B12 deficiency |
Alzheimers/dementia |
|
|
Mild AD |
Cognitive - Short term memory impairment - Aphasia - inability to communicate in speech Behavioural - Reversal changes - Depression - Acute episodes of confusion, disorientation, agitation, hallucinations |
Alzheimers/dementia |
|
|
Moderate AD |
Cognitive - Poor retention of recent memories > visual cues - Chronological sequences of events affected - Effects on language - Comprehension - Executive/intellectual function - ↓ self-care capacity Behavioural - Neurobiological alterations in brain - 5HT, DA, NA implicated in aggression, agitation and psychoses - ↓function in frontal lobes > apathy, depression, psychosis - Sleep disturbance due to pons changes |
Alzheimers/dementia |
|
|
Late AD |
Cognitive - Memory function severely impaired - Language skills lost, no speech - Executive/intellectual lost - No self-care/incontinent - Dysphagia - Mobility issues Behavioural - Aggression - Agitation - Sleep disturbance - Psychoses - Depression |
Alzheimers/dementia |
|
|
Advanced AD |
- As functional impairment increases, physical function declines and eventually diminishes - Die - Dependent - Mute - Swallow - Incontinence - Pneumonia - Influenza - Cardiac - Stroke |
Alzheimers/dementia |
|
|
Mini Mental State Examination (MMSE) |
- Assesses mental impairment rather than diagnosing - Accuracy - influenced by education - Orientation to time - Registration - Naming - reading - Clock drawing test - Blood test - Scans include MRI and CT - Cell loss = enlarged ventricles and shrinking of brain tissue |
Alzheimers/dementia |
|
|
Pharmacological management of AD |
- Improve symptoms but do not treat underlying cause - Indistinguishable between different forms of dementia - Main s/e is ↑confusion - Delay in efficacy - Significant s/e before =ve, discontinue |
Alzheimers/dementia |
|
|
Cholinesterase inhibitors (cognitive) |
Cholinesterase inhibitors - Effective for mild to moderate - Slow down ACh breakdown - Donepazil (Aricept) - Rivastigmine, Galantamine - 1/3 temporary improvement - 1/3 stabilise - 1/3 little benefit - GI disturbances - Cardiac problems ↓HR - Better concentration/alertness, improved short term memory and behaviour - Duration: as long as benefits > s/e - Decline in function: ↑ dose or alternative |
Alzheimers/dementia |
|
|
Memantine (cognitive) |
- NMDA receptor blocker - Treat moderate - severe - Protect brain nerve cells against Glut released by damaged cells - Gi disturbances, hypertension, dizziness |
Alzheimers/dementia |
|
|
Other cognitive treatments |
- Gingko biloba - Chinese herb improve circulation - Vit E - slows progression - Selegiline - treat PD, some AD - Huperzine A: moss extract similar to cholinesterase inhibitors |
Alzheimers/dementia |
|
|
Behavioural symptom treatment |
- Only if distressed or causing distress to others - Legal consent required - Ethical issues to psychotropic drugs - therapy or sedation? |
Alzheimers/dementia |
|
|
Antipsychotics + AD |
- Treat aggressive behaviour, agitation and other behavioural/psychological symptoms - Mixed results for risperidone/olanzipine due to ↑cerebrovascular stroke - Avoid in Lewy bodies > severe Parkinsonism - Duration dependenton observed benefits |
Alzheimers/dementia |
|
|
Antidepressants + AD |
- No overall beneficial effects over placebo - SSRIs (citalopram) first line - Minimum 6 months |
Alzheimers/dementia |
|
|
Mood stabilising + AD |
- Limited evidence of carbamazepine and sodium valproate against aggression - Sedation, liver dysfunction |
Alzheimers/dementia |
|
|
Hypnotics and anxiolytics + AD |
- Benzodiazepines limited due to oversedation - Useful in acute anxiety - Sleep disturbances: short acting temazepam, melatonin |
Alzheimers/dementia |
|
|
Memory Training (Mild) |
- Using external memory aids such as diaries and memo books - Person forms habit of using memory aids thus minimising impact of short term memory impairment |
Alzheimers/dementia |
|
|
Cognitive Stimulation Therapy (Mild) |
- Recommended by NICE for mild - Involves person attending multiple sessions at centre including games, food, money, current affairs - If new learning is required, events should stand alone within daily routine |
Alzheimers/dementia |
|
|
Validation therapy (Moderate-Severe) |
- Reassuringpatient about their hallucinations |
Alzheimers/dementia |
|
|
Reminiscence therapy (moderate-severe) |
- Using triggers such as music, photos, videos - Reduces depression symptoms |
Alzheimers/dementia |
|
|
Next gen diagnosis |
Blood tests - Beta amyloid protein - Difficult in translating changes in blood to brain CSF - Translatable - Beta amyloid protein decreased - Tau protein increased |
Alzheimers/dementia |
|
|
Next gen neuroimaging |
Structural neuroimaging - 3D brain map to track anatomical changes over time - Map brain degeneration by AD Functional neuroimaging - Early dementia - Ability to detect amyloid plaques to monitor neuropathological abnormality of AD |
Alzheimers/dementia |
|
|
Next gen treatment |
Secretase inhibitors - Gamma or beta-secretase involved in beta-amyloid protein - Disappointing Phase III trials Beta amyloid vaccination - ↑ Removal of beta-amyloid protein - Disappointing trials |
Alzheimers/dementia |
|
|
Gene therapy |
- Fibroblast > genetic modification > human nerve growth factor > injection into region where neurons are undergoing atrophy - NGF prevent cell death or enhance existing cells? |
Alzheimers/dementia |
|
|
Stem cell grafts |
- Controversial due to usage of foetal stem cells - Undifferentiated/immature stem cells transplanted with subsequent control cues derived from brain - Grow stem cells to desired neuronal type - Transplant back into patient - Used in PD with moderately encouraging results |
Alzheimers/dementia |
|
|
Key risks of poor injection use |
Soft tissue infections - Cellulitis - Ulcers - Thrombophlebitis Septicaemia - Bacteria in bloodstream = fever - Life-threatening Pulmonary problems - Pneumonia |
Drugs of abuse clinical |
|
|
Primary blood bourne viruses from needle sharing |
HepC - Major causes of liver disease - Issues + alcohol - B = vaccination HIV - Under-25s |
Drugs of abuse clinical |
|
|
Harm reduction |
Needle exchange - Sterile injecting equipment - Ideally one for one Maintenance replacement - Methadone - Subutex - CBT |
Drugs of abuse clinical |
|
|
Progression of CNS injury |
- Local swelling at site of injury pinches off blood perfusion > ischaemia - Excessive release of Glut and excitotoxicity of neurons and oligodendroytes at site of injury - Infiltration by immune cells - Free radical toxicity - Apoptosis/necrosis |
Brain and spinal cord repair |
|
|
Restructuring in response to damage |
- Astrocytes begin production and secretion of cytokines, reactivates proliferation; infiltrates lesion, form scar - Astrocytes express complex milieu of proteoglycans at scar boundary - Damage to axons result in retraction of resealed growth cone where it stalls indefinitely - Axons are demyelinated and degenerate or remain fixed in place for years |
Brain and spinal cord repair |
|
|
CNS injury |
- Regeneration of axons and functional recovery following damage in periphery - CNS-specific hostile environment due to two entities 1) reactive astrocytes 2) oligodendrocyte myelin-associated inhibitors (Nogo, MAG, OMgp, chondroitin sulfate proteoglycans) |
Brain and spinal cord repair |
|
|
Symptoms of spinal cord injury |
- Involuntary muscle spasms - Loss of voluntary movement • Sensation, balance • Control of breathing • Autonomic functions (BP) • Bladder, sexual, bowel control Due to destruction of long ascending or descending spinal pathways Axons must regrow, synaptic circuits must be reestablished |
Brain and spinal cord repair |
|
|
Restoring function |
"Complete" is not complete - Transection of cord is rare - <10% of axons can support substantial functional recovery - Even "complete" injuries recover some function Surviving axons need to be myelinated - 4-aminopyridine improves conduction - Stem and other cells remyelinate spinal axons Reversing learned "non-use" - Even a short period of non-use can turn off circuits - Intensive "forced-use" exercise to restore function |
Brain and spinal cord repair |
|
|
Cell biological reactions in damaged neuron |
- Presynaptic and postsynaptic neurons - If cell body is damaged, neuron is lost; there is no cell division in adult brain to replace lost neuron - The cell body is lost if axon is severed close to cell body, but there is chance of axon regeneration, even in CNS - Postsynaptic (and presynaptic) neurons are also affected and may degenerate |
Brain and spinal cord repair |
|
|
Response of neuron to injury |
A: All neurons, despite different morphologies, react similarly B: Principles - If cell body damaged, neuron dies and is not replaced by cell divison in mature brain - If axon is damaged or severed at a distance, good chance of regeneration, primarily in periphery - CNS neurons have capacity to regenerate - CNS tissue possess active property of specifically and actively inhibiting regrowth of axons through them |
Brain and spinal cord repair |
|
|
What can we do about CNS damage? |
FIX - Prevent cell death - Promote axon regrowth - Remove blockades BUILD AROUND IT - Brain-machine interfaces that can interpret neural codes and output activity to periphery (organic or machine) |
Brain and spinal cord repair |
|
|
Surgical advances |
Decompression and stabilisation of the spine - Anterior and posterior plates - Titanium cage vertebral repair - Delayed decompression restores function even years after injury Urological procedures - Suprapubic catheterisation - Mitrafanoff procedure - use appendix to allow catheterisation of bladder through belly button - Vocare sacral stimulation Syringomyelic cysts - Removing adhesions and untethering of cord will collapse synringomyelic cysts with lower rate of recurrence - Restoring CSF flow is key to preventing cyst development Peripheral nerve bridging - Implanting avulsed roots or nerves into spinal cord - muscle reinnervation, reduces neuropathic pain - Bridging nerves from above injury site to organs below |
Brain and spinal cord repair |
|
|
Promoting CNS regen with drugs |
- Inhibiting axon regeneration blockers in CNS myelin - Removing barriers formed by glial scars - Stimulating regrowth by signalling pathways - Replacement of neurons damaged during injury with embryonic stem cells - Engineering brain-machine interfaces to produce enhanced sensory feedback presthetics (bionic/cybernetics) |
Brain and spinal cord repair |
|
|
Myelin forming cells |
- Oligodendroglia in CNS - Schwann cells in PNS - Oligodendrocytes are inhibitory to axon regrowth in adult CNS regen - Schwann cells are supportive, as a growth surface and releaser of growth factors |
Brain and spinal cord repair |
|
|
Astroglia |
- Development: supports axon growth and cell migration - Mature: important for ion influx, synaptic function, BBB - Injury: accumlate in scar, release excess matrix, inhibit axon growth? |
Brain and spinal cord repair |
|
|
Microglia (resting) + macrophages (active) |
Cells of immune system, similar to monocytes - Injury, help or hinder? Not sure |
Brain and spinal cord repair |
|
|
Reactions to injury within neuron |
Immediately 1. Synaptic transmission OFF 2. Cut ends, pull apart, seal up, swell, due to axonal transport in both directions Hours 3. Synaptic terminal degenerates - accumulation of neurofilaments, vesicles 4. Astroglia surround terminal normally; after axotomy, astroglia interpose between terminal and target and cause terminal to be pulled away from postynaptic cell Days-weeks 5. Myelin breaks up and leaves debris (myelin hard to break down) 6. Axon undergoes Wallerian degeneration 7. Chromatolysis - cell body swells, nissl and nucleus eccentric *If axon cut in CNS or PNS, same result * Damaged neuron affected as well as pre/postsynaptic neurons to it |
Brain and spinal cord repair |
|
|
CNS neuron regeneration summary |
CNS axons can regrow but impeded b negative elements - Myelin prooteins (NOGO, MAG, OMgp) increase - Extracellular matrix (laminin) is sparse; inhibitory proteoglycans increase - Growth factors have different distributions compared to young brain - Intracellular growth elements such as GAP-43 (important for intracellular signalling/growth cone advance) are low - Glial cells inhibit growth • Oligodendrocytes (CNS myelin) most inhibitory • Astrocytes accumulate in scar around injury site • Macrophages also accumulate; role of microglia unclear |
Brain and spinal cord repair |
|
|
Working against myelin to promote regeneration |
- Immunisation against myelin promotes regeneration of axons through spinal cord lesion in rats - Antibodies that inhibit myelin promote axon regeneration |
Brain and spinal cord repair |
|
|
Nogo |
- Reticulon family protein - Isoforms: Nogo-A, Nogo-B, Nogo-C from differential splicing and alternate promoter usage - C-terminus contains two hydrophobic regions > transmembrane sequences required for ER membrane localisation in other reticulons - Localised to plasma membrane, endoplasmic reticulum, neuronal synapses - Nogo-A = CNS, Nogo-B = CNS, lung, liver, Nogo-C = SkeMus |
Brain and spinal cord repair |
|
|
MAG and OMgp |
- Myelin associated inhibitors - Myelin-Associated Glycoprotein (MAG): transmembrane protein with 5 immunoglobulin like repeats in extracellular domain - Oligodendrocyte Myelin Glyprotein (OMgp): GPI linked containing leucine-rich repeat (LRR) domains with serine/threonine repeats |
Brain and spinal cord repair |
|
|
Nogo receptor |
- Receptor for Nogo, MAG and OMgp - GPI-linked protein with LRR repeats - No transmembrane motifs, requires coreceptor to transmit signal across membrane - p75 neurotrophin coreceptor - NGR convergent target of all myelin-associated inhibitors, lots of research to specifically inactivate it |
Brain and spinal cord repair |
|
|
Chondroitin sulfate proteoglycans (CSPGs) |
- Upregulated in glial scar following spinal cord lesion - Treatment with chondroitinase (which cleaves CSPGs from cell surface) enhances regrowth through the lesion |
Brain and spinal cord repair |
|
|
cAMP and MAG |
- cAMP pathway regulates MAG signalling ↑cAMP ↓MAG ↑regrowth |
Brain and spinal cord repair |
|
|
CNS repair clinical trials |
- Foetal cell transplants - 4-aminopyridine - Activated macrophage transplants - Porcine neural stem cell transplants - Alternating current electrical stimulation - AIT-082 - Peripheral nerve bridging with neurotrophic cocktail - Theophylline therapy to restore respiratory function |
Brain and spinal cord repair |
|
|
Stem cell transplants for CNS repair |
- Transplantation of oligodendrocyte progenitor cell to treat myelination disorders - Transplantation of phentypically restricted (unipotent) neuronal progenitors to treat neurodegeneration - Implantation of mixed progenitor pools or multipotent stem cells to reconstruct disorders with losses of several lineages - Mobilisation of endogenous neural precursors to replace neuronal loss in disease |
Brain and spinal cord repair |
|
|
What is stroke? |
- Acute onset of neurological deficits (lasting more than 24hrs) due to disturbance in blood supply to brain - Neurological symptoms • Aphasia: difficulty understanding speech • Dysphasia: speech impairment • Apraxia: muscles for speech • Hemiparesis: half paralysed • Facial weakness • Confusion, dizziness, vision impairments • Thunderclap headache: haemorrhage - 15mil suffer stroke, 5mil die, 5mil permanently disabled |
Stroke |
|
|
Stroke risk factors |
Non-modifiable - Age - Race - Genetics - Gender Modifiable - Hypertension - Smoking - Diabetes - High cholesterol - Obesity - Activity levels |
Stroke |
|
|
Types of stroke |
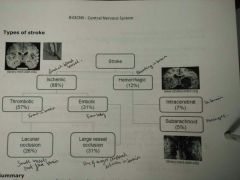
|
Stroke |
|
|
Cerebral blood supply |
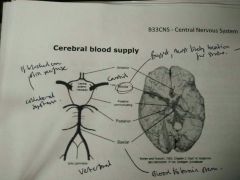
Anterior, middle, posterior communitcating, posterior, basilar, circle of Willis |
Stroke |
|
|
Arterial territories |
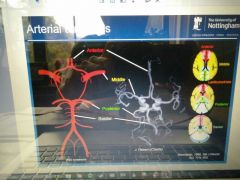
|
Stroke |
|
|
Subcortical blood supplies |
- Anterior cerebral artery - Lenticulostriate arteries > lacunar occlusion - Miiddle cerebral artery |
Stroke |
|
|
Aneurism |
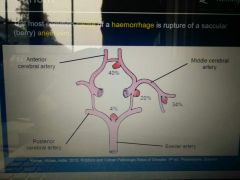
- Most common cause of haemorrhage is rupture of a saccular (berry) aneurysm - At junction, different flow causes pressure (creating aneurism)
Aneurism coiling - Wire into aneurism to displace blood - Clipping prevent more blood into bulge |
Stroke |
|
|
Diagnosis |
ROSIER: Recognition of Stroke in the Emergency Room - ↑score, ↑stroke ABCD: Age, BP, Clinical features, Duration, Diabetes - Check for TIA, assess risk of stroke |
Stroke |
|
|
Computed tomography (CT) |
- Easy, affordable - Sulcal effacement (blurred edges, not as defined) - Loss of basal ganglia definition - Old infarction (lacunar) - Hyperdense artery
- CT better at haemorrhage - Dark = dense, light = less dense |
Stroke |
|
|
Diffusion weighted imaging (MRI) |
- 95% effective at detecting acute ischaemic stroke |
Stroke |
|
|
Penumbra |
- Fate not decided, treatment to save - Areas of brain die over time, altering chances of survival - Work fast to save as much brain as possible - Recombinant issue plasminogen activator (Alteplase) is only treatment - 3hrs from onset |
Stroke |
|
|
Time course of events |
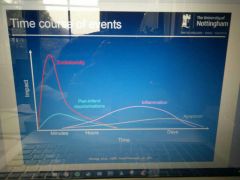
- Excitotoxicity - Peri-infarct depolarisations - Inflammation - Apoptosis |
Stroke |
|
|
Pathophysiology |
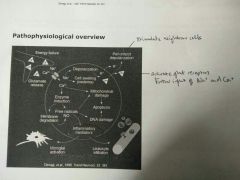
|
Stroke |
|
|
Excitotoxicity |
- Cell depolarisation results Na+ and Ca2+ ion influx and K+ efflux - Glut release and activation of Glut receptors - Ionotopic NMDA: • Most important for excitotoxicity • Voltage-gated channel permeable to Ca2+, Na+, K+ • Excessive Glut and Ca2+ displase Mg2+ ion leading to further influx - Ionotropic AMPA: • Voltage-gated channel permeable to Ca2+, Na+ and K+ - Metabotropic Glut receptors G protein mediated Ca2+ release |
Stroke |
|
|
Inflammation |

|
Stroke |
|
|
Migraine |
- Painful pulsing headache typically lasting 4hrs-3days, often unilateral and associated with photophobia - 7%M, 17%F at least 1 migraine/year - Middle age |
Migraine and emesis |
|
|
Migraine symptomology |
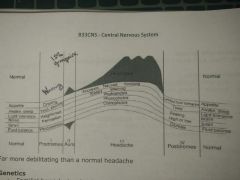
Up to 5 stages
Prodrome - Yawning, mood or appetite change
Aura = initial visual disturbance, 30mins - Visual area lost, surrounding area shimmers
Unilateral throbbing headache, 4-72hrs - Photophobia - Nausea and vomiting - Prostrate Resolution = usually deep sleep + loss of headache
Recovery = often get exhaustion
Far more debilitating than normal headache |
Migraine and emesis |
|
|
Migraine genetics |
- Familial hemiplegic migraine - with aura - Rare autosomal dominant disorder - 50% cases cause = point mutations in CACNA1A gene that encode pore-forming a1A subunit of P/Q voltage-gated calcium channel (Chromo19) - Mutations result in altered channel conductance and density of expression in vitro in cell lines - 30% pts might result from mutations in ATP1A2 gene that encodes Na+/K+ pump a2 subunit - Mutation in TRESK K2P K+ channel in spinal neurons |
Migraine and emesis |
|
|
Vascular Pathophysiology Theory |
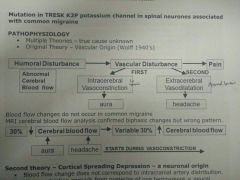
Humoral Disturbance (Abnormal Cerebral Blood flow) > Vascular Disturbance > Intracerebral vasoconstriction = aura >> Extracerebral vasodilation = headache > Pain
- Blood flow changes do not occur in common migraine - MRI cerebral blood flow analysis confirmed biphasic changes but wrong pattern > headache starts during constriction |
Migraine and emesis |
|
|
Cortical Spreading Depression Theory |
- Blood flow change does not correspond to intracranial artery distribution - Vasoconstriction spreads from posterior of one hemisphere = neural mediation (depression of cortical neurons in animals) - May cause aura but not migraine - Changes in blow flow driven by change in metabolic demand resulting from neuronal depression are thought to result in progressive change in MR signal in occipital cortex - Aura usually involves wave of electrical activity starting in occipital cortex and spreading slowly associated with visual hallucinations across visual field that is reproducible in same individual |
Migraine and emesis |
|
|
Sensory nerve activation |
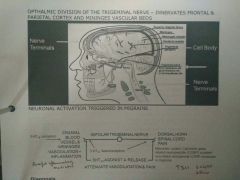
Migraine = Enhanced Trigeminovascular Neuron Activity
- Trigeminal nerve has 3 divisions forehead and eye (ophthalmic V1), cheek (maxillary V2) lower face and jaw (mandibular V3) Nerves sense facial touch, pain, temperature, as well as controlling muscles used for chewing
- Ophthalmic division of trigeminal nerve - innervates frontal + parietal cortex and meninges vascular beds |
Migraine and emesis |
|
|
Migraine Diagnosis |
- No definitive test or diagnosis - Careful assessment of patient history - Elimination of alternative causes of headache e.g trauma, other drug treatments or rare disorders |
Migraine and emesis |
|
|
Inernational Classification of Headache Disorders (ICHD-II) |
A At least 5 attacks fulfilling criteria B-D B Headache attacks lasting 4-72hrs (untreated or unsuccessfully treated) C Headache has at least two of the following characteristics: - Unilateral location - Pulsating quality - Moderate or severe pain intensity - Aggravation by or causing avoidance of routine physical activity D During headache at least one of the following - Nausea and/or vomiting - Photophobia and phonophobiba E Not attributed to another disorder |
Migraine and emesis |
|
|
Migraine Diaries |
Enourage patients to record details of migraine attacks - Help doctors make firm diagnosis - Recognise warning signs of attack - Identify triggers - Assessing whether acute or preventative meds is working Records may include info on - When pain begins and frequency - Symptoms - Length of attacks - Pain location and whether throbbing, piercing Record as many possibly relevant aspects of daily life - Diet, medication, vitamins or health products; exercise, sleep duration - Women should record details of their menstrual cycle |
Migraine and emesis |
|
|
Trigger factors |
- Mental stress - Refractory errors in glasses - Chocolate, eggs, fruit - Alcohol - Oral contraceptives - Time zone shifts - Physical exertion Counselling can have major benefit to establish self-care approach |
Migraine and emesis |
|
|
Migraine medication goals |
- Primary Acute relief from recurrent attacks - Secondary Effective prophylatic treatment |
Migraine and emesis |
|
|
Stepwise approach therapy: mild |
- Analgesics/NSAIDs, antiemetics from GP if required - Most effective early during attack - OTC meds appropriate - Rest + sleep - Triptans 5HT-1B/1D receptor agonists - vasoconstriction and CGRP inhibition but some CV risk - Available OTC - Short acting poor CNS penetration - Chest pain due to coronary artery vasoconstriction - CI in IHD - Will not prevent aura so during attack - CGRP receptor antagonists |
Migraine and emesis |
|
|
Stepwise approach therapy: prophylactic |
- Avoid triggers - Beta blockers, calcium channel blockers, anticonvulsants, amitriptyline, or premenstrual oestrogen can be effective - Acupuncture of gabapentiin and botulinum toxin type A recommended by NICE |
Migraine and emesis |
|
|
Emesis |
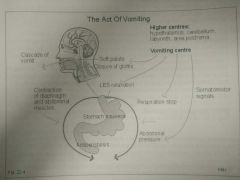
- Protective reflex (to expel ingested toxins) associated with nausea - Nausea = unpleasant sensation that immediately proceeds vomiting; cold sweat, pallor, salivation, self-absorption, loss of gastric tone, duodenal contractions - Vomiting = coordinated involuntary reflex involving powerful sustained contraction of ab, chest wall and diahragm - Epiglottis closes over trachea to prevent inhalation - Incomplete where sphincter doesn't open = retching |
Migraine and emesis |
|
|
Central control of emesis |
- Generated/coordinated by vomiting centre - neurons in medullary reticular formation - Generate motor components of vomiting reflex, and receive inputs that trigger the reflex |
Migraine and emesis |
|
|
Causes of nausea and vomiting |
- Iatrogenic (chemotherapy, radiotherapy, opiates, antibiotics) - Motion sickness and Meniere's disease - Pregnancy - Poisoning (alcohol) - Gastroenteritis and stimulation of pharynx - Meningitis and intracranial haemorrhage (raised pressure) - Bulimia nervosa |
Migraine and emesis |
|
|
Vomiting centre inputs |
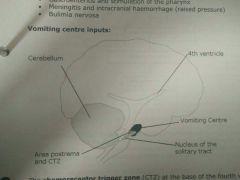
Chemoreceptor Trigger Zone (CTZ) at base of 4th ventricle has multiple receptors (D2, 5HT-3, opioid, ACh), substance P (neurokinin) is major output transmitter
- Area postrema: detects blood chemicals (no BBB) - Vestibular system via vestibulocochlear (8th cranial) nerve: major role in motion sicknes and rich in muscarinic cholinergic and histamine H1 receptors - Vagal nerve afferents: activated when pharynx is arritated > gag reflex; nucleus tractus solitarious has high 5HT-3 and NK1 receptors - Vagal/GI afferents: respond to irritation of gastroenteritis via gut 5HT3 receptor - Intracranial pressure receptors mediating nausea after head injury/meningitis - Descending inputs: higher centres from sight or smell of vomit, situations associated with vomiting |
Migraine and emesis |
|
|
Sensory inputs to vomiting centre |
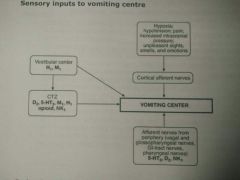
|
Migraine and emesis |
|
|
Induction of vomiting |
Sometimes nececssary to actively induce to aid elimination of poisons only if: - Still in stomach - Won't inhale poison - Emetic ipecacuanha directly activates CTZ |
Migraine and emesis |
|
|
Drugs controlling nausea/vomiting |
- 5HT-3 antagonists (ondansetron) - Eicosanoid synthesis inhibition (corticosteroids) (dexamethason) - Neurokinin1 antagonist [agonist: substance P] (aprepitant) - D2 antagonist (metoclopramide, domperidone) - Anticholinergics (scopolamine) - Antihistamines (cinnarizine) - Histamine H3 antagonist (betahistine) - Cannabinoid agonists (nabilone) - Multiple (olanzapine) |
Migraine and emesis |
|
|
Sites of drug action |
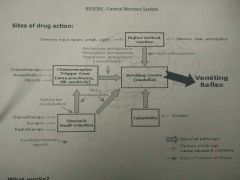
|
Migraine and emesis |
|
|
What works? |
- Single agent = NK1 antagonist aprepitant because substance P is major output transmitter from vomitingcentre, active against most causes of vomiting - Motion sickness = H1/H3 antagonists - Chemo-induced = corticosteroid + DA antagonist, 5HT-3 also effective - Combination therapy shows additive benefits: NK1 antagonist + 5HT3 antagonist + corticosteroid |
Migraine and emesis |
|
|
What does not work? |
- Nausea more difficult to control > interactions with higher centres - Combination of anti-emetics and mild sedation - Corticosteroids not effective for acute vomiting - 5HT-3 antagonists not effective against non-chemo - Some pts resistant to all anti-emetics, variant 5-HT receptors |
Migraines and emesis |

