Reading...
![]()
Play button
![]()
Play button
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
Seizures
|
- A seizure is a single event characterized by sudden, excessive, and disorderly discharge of neurons resulting in a variety of clinical signs
- Seizures can arise from any condition that heightens the excitability of brain tissue and may be associated with high fever, drug use, drug withdrawal, and metabolic disorders - Epilepsy requires the presence of at least two unprovoked seizures (i.e. occurring in the absence of acute systemic illness) |
|
|
Use of "ictus" (Latin) to describe a seizure.
|
- "pre-ictal" = period before seizure
- "post-ictal" = period after seizure - "inter-ictal” = period between seizures |
|
|
Aetiology of seizures
|
- Seizures indicate brain abnormalities
- Frequent neuropathologies causing seizures: a) Vascular diseases b) Intracranial tumours c) Traumatic brain injury d) Degenerative disorders |
|
|
Idiopathic seizure
|
- Unknown cause, presumed to be genetic
- May result from inherited mechanism that leads to a lowered seizure threshold - In some cases, the causal brain lesion is to small to be seen on images |
|
|
Symptomatic seizure
|
- Caused by identifiable brain pathology (e.g. stroke, TBI, timor, infection)
|
|
|
Cryptogenic seizure
|
- Hidden cause, almost always due to some form of cortical abnormality acquired during fetal development (e.g. as indicated by learning difficulties or abnormal EEG readings)
|
|
|
Epidemiology of seizures
|
- About 1 in 10 adults sometime during life
- Epilepsy: Lifetime incidence is 2%-5% |
|
|
Classification of seizure types
|
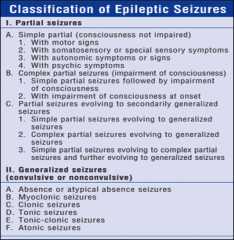
|
|
|
Classification of epilepsy syndromes
|

- Epileptic syndrome: Epileptic disorder characterised by a cluster of signs and symptoms customarily occurring together
- Classification into idiopathic (unknown cause), symptomatic (identifiable cause), or cryptogenic (hidden cause) aetiologies and on whether the seizures have a focal or generalized onset |
|
|
Incidence of seizure types
|
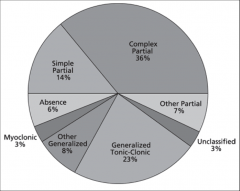
|
|
|
Simple partial seizures
|
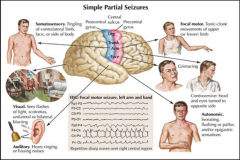
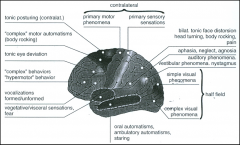
- Abnormal neural firing restricted to a focal brain area
- Usually last for several seconds to a few minutes - During seizure, patient is alert and maintains awareness and memory for the entire event - Clinical signs of a seizure (motor, sensory, autonomic or psychic signs) depend on where in the brain the excessive neuronal discharges are taking place - Sometimes called "Aura" and may be a warning signal to patients that they are about to have a seizure |
|
|
Complex partial seizures
|
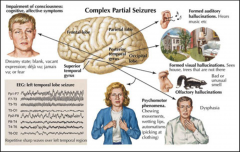
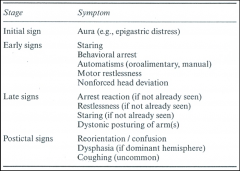
- Differ from single partial seizures by
a) the patient’s decreased awareness of environment b) lack of responsiveness c) absence of recall for events occurring during seizure - Typically lasts for several minutes - Post-ictal period: -> Usually consists of 2 to 10 minutes of disorientation, inattention, inactivity, and headache, which resolves gradually - Begin as simple partial seizures (Auras) and progress to impairment of consciousness or with impairment of consciousness at onset - Automatisms during complex partial seizure: -> Commonly exhibited -> Repetitive involuntary motor activities occurring during a state of reduced awareness and responsiveness -> Include acts like repetitive picking movements, lip smacking, chewing or swallowing motions, drooling, or tapping or rubbing hand movements -> Usually last for 2 to 5 minutes and occur at any point during a seizure (i.e. beginning, middle, or end) -> No recollection of automatism's in most patients |
|
|
Aura
|
- Warning signal to patients that they are about to have a seizure
- Typically sensations such as epigastric distress, an urge to urinate or defecate, or a feeling of intense fear - Usually last seconds to minutes - Most patients have the same aura consistently at the start of each of their seizures - Most patients remember their particular aura since it occurs before the onset of loss of awareness - Over time can be subject to classical conditioning and elicit a separate set of responses in the patient often involving an anxiety and panic reaction |
|
|
Generalized tonic-clonic (grand mal) seizures
|

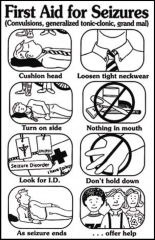
- Begins with tonic phase: crying out and an increase in tone across multiple muscle groups and upward deviation of the eyes
-> Typically lasts between 10 and 30 seconds - Followed by clonic phase: repeated bilateral, symmetric jerking of the arms and legs, stopped breathing -> Usually lasts between 30 to 90 seconds (duration of entire ictus = only between 1 and 2 minutes) -Possible increase of blood pressure, heart rate and salivation and loss of bladder control - High risk of injury due to potential for falling to ground and the sometimes violent jerking movements - Post-ictal period: -> Patient may gradually awaken by passing through stages of coma to confusion to drowsiness -> Alternatively, patients may fall asleep immediately after the seizure for varying lengths of time - Patients with generalized tonic-clonic seizures frequently complain about generalized, tiredness, headache and muscle soreness after a seizure |
|
|
Status epilepticus
|
- Prolonged seizure (> 5 minutes) or a series of brief seizures occurring so quickly that patients do not have time to recover from one before another has begun
- Status epilepticus most common in generalized tonic-clonic seizure (also the most life threatening) - Medical emergency -> Without appropriate treatment = Irreversible brain damage or death after 30 to 45 minutes after onset |
|
|
Mesial temporal lobe epilepsies
|
- Most common form of temporal lobe epilepsy (TLE) and the best characterized type of epilepsy
- Temporal lobe is is the most frequent site of localisation-related seizures (about 60-70% of partial epilepsy cases) - Mesial temporal lobe structures: Include the amygdala, the hippocampus, and entorhinal cortex - Most common pathology underlying mesial temporal lobe epilepsy (MTLE): Hippocampal sclerosis -> Cell loss and hardening of the hippocampus -> Discussion whether hippocampal sclerosis is cause OR consequence of chronic, pharmacoresistant seizure activity |
|
|
Reflex epilepsies
|
- Reflex epilepsies elicited by some specific stimulus or event
- Thought to be due to hyperexcitable neurons in either primary sensory cortices or secondary association areas as caused by structural or biochemical abnormalities -> Entrance of particular stimulus (e.g. flickering lights) into these cortical regions presumably activates hyperexcitable neurons, which initiates a seizure - Eating epilepsy: seizures in response to the sight or smell of food, by the digestion process after eating food, and sometimes by exposure only to specific foods - Reading epilepsy: seizures are triggered by either silent, or more commonly, during oral reading - Musicogenic epilepsy: seizures in response to listening to music, may be precipitated by a particular piece of music - Hot water epilepsy: seizures are precipitated by having cups of hot water poured over the head or by bathing in hot water (sometimes ecstatic feelings) - Imagination of stimuli might already trigger seizures |
|
|
Electroencephalography (EEG) and Seizures
|
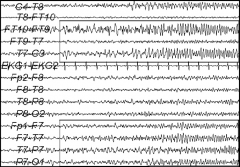
- Indicating abnormalities in about 95% of cases
- specific EEG patterns are associated with many epilepsy syndromes and assist in formal diagnosis - In about 30% of cases: Epileptic abnormalities in routine recordings (20-30 minutes duration) in the time between seizures -> EEG recordings of value in time between seizures, not only during a seizure |
|
|
Treatment of Epilepsy
|
- 70-80% of patients with epilepsy become seizure-free
- Anti-epileptic drugs - Surgery - Psychoeducation - Lifestyle changes |
|
|
Acute management of Epilepsy
|
|
|
|
Anti-epileptic drugs (anti-convulsant drugs)
|
- Suppress neuronal excitability
-> Either by enhancing inhibitory neurotransmission or by suppressing excitatory transmission - No response to anticonvulsant medication in up to 30% of epilepsy patients - No evidence that AEDs have any independent cognition-enhancing properties -> However, Improvements in cognition can occur as a consequence of better seizure control - AED act not selective and also affect normal acting neurones - Can cause cognitive impairments: Speed of processing, Attention, Executive functions, Memory and Language functions -> possible explanation: Suppression of neuronal excitability or the enhancement of inhibitory neuro-transmission in certain brain areas -> Side effects depend on Substance, Number of AEDs, Dose, Titration speed and Efficacy with regard to seizure control |
|
|
Surgery for epileptic patients
|
- Successful treatment option for patients with refractory epilepsy (meds don't work)
- Recommended a) When patients are pharmacoresistant b) When patients have a resectable (removable) epileptogenic zone c) When surgery in the affected brain structures will not lead to any serious negative side-effects - Most commonly performed operation is anterior temporal lobectomy - Complete seizure control in two-thirds of cases - Significant seizure reduction in 80% of patients with mesial temporal lobe epilepsy (MTLE) - fewer seizures does not necessarily mean better outcome, because there's a negative effect on cognition |
|
|
Psychoeducation in Epilepsy
|
- Teaching programmes considering basic information, treatment, psychosocial aspects and coping with epilepsy
- Improvement of quality of life - Reduction in seizure frequency |
|
|
Beneficial lifestyle changes in epilepsy
|
- No alcohol
- No drugs - No stress - Much sleep - No flickering lights - Ketogenic diet (high in fat and low in carbohydrate and protein) |
|
|
Seizure response dogs
|
- Warn people with epilepsy of an oncoming attack minutes (sometimes hours) before it occurs
- Allows patient time to take seizure blocking medication, get to a safe place, or call for assistance - Seizure response dogs respond appropriately when the seizure occurs (e.g. may bring pillows from the bed) - Controversy about usefulness (conditioning) |
|
|
Role of neuropsychology in epilepsy evaluation
|
- Localisation
- Pre-surgical assessment - Treatment evaluation - Description of neuropsychological impairments, e.g. for planning of functional trainings |
|
|
Cognition in patients with epilepsy
|

---- Picture: Factors influencing cognition
FCD = focal cortical dysplasia HS = Hippocampal sclerosis - It's unclear whether seizures cause cognitive decline per se - Seizure related variables and cognitive decline are not really related - longstanding drug use is associated with mild cognitive decline - memory seems to be the most affected measure - Hippocampal and extrahippocampal damage in patients with temporal line epilepsy - in idiopathic epilepsy no relation between cognitive impairment and seizure frequency, but with interictal epileptiform activity |
|
|
Neuropsychological tests and epilepsy
|
- No standard pattern of neuropsychological test results characteristic of specific epilepsy subtypes
-> because many different neurological diseases can cause epilepsy across countless brain regions -> often underlying neuropathology causing the seizures (e.g. brain tumour, stroke or TBI) has a stronger influence on cognition than epilepsy itself - Example: Tumour located in left temporal lobe may be more responsible for verbal memory deficits than the seizures originating from scar tissue surrounding the tumour |
|
|
Intellectual functions in epileptic patients
|
- Intellectual deterioration is most likely related to the severity of seizure disorder and underlying aetiology
- Increase of likelihood of intellectual impairment: a) Presence of symptomatic epilepsy (a known neuropathological aetiology) b) Earlier age of onset c) Longer duration of seizure disorder d) Higher frequency of seizures e) Antiepileptic drug polypharmacy |
|
|
Memory in epileptic patients
|
- In adults: Memory appears to be the most vulnerable cognitive function
- Regions specialized for learning and memory, e.g. hippocampus, appear most prone to seizures - Patients with mesial temporal lobe epilepsy (both left and right) typically have more severe memory impairments than patients without temporal lobe onset -Memory impairment most extensive in patients with bilateral temporal lobe damage - Unilateral temporal lobe epilepsy is associated with material-specific memory disorders -> Verbal memory deficit following left temporal lobe lesion -> spatial memory deficits following right temporal lobe lesion - Individuals with left temporal lobe seizures are more likely to present multiple memory and cognitive deficits than those with right temporal lobe seizures -> However, of course other factors could contribute to poor memory test performance (e.g. language difficulties or inattention) |
|
|
Language in epileptic patients
|
- Not been examined as thoroughly as memory and intellectual functions
- Fronto-temporal seizure focus: More likely to impair expressive functions - Posterior temporal lesions: More likely to impair comprehension - Parietal lesion: May impact reading and spelling |
|
|
Executive functions in epileptic patients
|
- Rapid seizure propagation is characteristic for frontal lobe epilepsy
- Neurons in contralateral frontal lobe and mesial temporal regions are frequently recruited - Frontal lateralizing cognitive deficits are rarely found - Executive dysfunction not only in frontal lobe epilepsy, but also in epilepsies with other localisations (e.g. mesial TLE) |
|
|
Risk factors for poor outcome of surgery on epileptic patients
|
- surgery to the language dominant hemisphere
- with greater collateral brain damage due to surgery - persistent seizures - with good preoperative memory performance - with an older age at the onset of epilepsy - with an older age at the time of surgery - with a larger extent of the resection - and with lower mental reserve capacities |
|
|
Emotion and personality epileptic patients
|
- Emotional problems are common
-> More common in patients with symptomatic epilepsy (known brain injury) than in patients with idiopathic seizures - More frequent in patients with temporal lobe epilepsy than any other seizure group - Identity crisis - Aggression: less frequent than reported in past - Depression: most common emotional concern found in epilepsy - Increased stress, e.g. fear of seizures |
|
|
Temporal lobe personality
|
- Permanent alteration of personality in some patients
- Characterized by increased emotional intensity a) Overemphasizing trivia and the petty details of daily life b) pedantry (excessive concern with minor details and rules) c) Hypergraphia (intense desire to write) d) Preoccupation with religion e) Humourlessness f) Egocentricity - However, vast majority of persons with seizures emanating from the temporal lobes do not show this behavioural pattern |
|
|
Historical view on epilepsy
|
- Early Greeks: Visitation from gods and thus a sacred disease
- For centuries: Laypeople have viewed people with epilepsy as odd, as having unusual powers, and as being in close touch with the divine - Many religious figures might have suffered from temporal lobe epilepsy (e.g., Moses, St Paul, and Joan of Arc) |
|
|
Psychosis or psychotic-like conditions in epileptic patients
|
- Incidence of psychosis elevated
- Psychosis may present as a transient ictal phenomenon (e.g. disturbing hallucinations and paranoid thoughts) -> However, psychosis can develop between seizures |
|
|
Stigma associated with Epilepsy
|
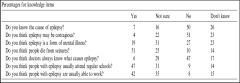
- In a study of children with new-onset seizures and their parents, concerns about stigma were top of the list
- Children reported that they feel different from their peers and fearful of being teased about having a seizure in front of their friends - Only few adolescents in general population familiar with epilepsy - Adult people with epilepsy may stigmatised: barred from marriage and employment |
|
|
Legislation and Epilepsy
|
- In China and India, epilepsy is commonly viewed as a reason for prohibiting or annulling marriages
- In the United Kingdom, a law forbidding people with epilepsy to marry was repealed only in 1970 - In the USA, 18 States provided eugenic sterilisation of people with epilepsy until 1956. Until the 1970s, it was also legal to deny people with seizures access to restaurants, theatres, recreational centres and other public buildings |
|
|
H.M.
|
- removal of parts of anterior medial temporal lobes
-> reduced H.M.'s epileptic seizure -> he became globally amnesic - anterograde amnesia - retrograde amnesia for 11 years - intelligence and other areas largely unimpaired |
|
|
Damage to medial tempral line of the hemisphere dominant for language (usually left)
|
- may result in impairments on new learning and memory for verbal material
- intact memory abilities may compensate for those lost, so that a person can live independently |
|
|
Global amnesia
|
- inability to learn new information, whether verbal, nonverbal, visual, auditory
- usually includes retrograde amnesia - usually results from bilateral damage to particular structures on the internal aspects of the cerebral hemispheres - other causes: -> herpes simplex -> Korsakoff's syndrome (but after damage to mamillothalamic region and cues can aid recall) |
|
|
Mechanism of Epilepsy
|
- balance between excitatory and inhibitory neurone is disrupted
- result: more and more neurone become excited - At some point seizure threshold is reached and the storm of electrical activity in the brain results in a seizure |
|
|
Absence seizure
|
- sudden transient lapse of consciousness
- often barely perceptible to an observer - restricted to childhood years and can result in learning difficulties |
|
|
Wada test
|
- Sodium amytal is injected into one hemisphere, which anaesthetises the hemisphere for 5min
- Before injection: baseline tests - During anaesthesia: tests for awake hemisphere to asses how well it copes with speech, naming and memory - It's used for screening for neurosurgery in epilepsy |
|
|
Methodological difficulties when studying cognition in epileptic patients
|
- differentiation of effect of seizure and effect of underlying lesion
- cross-sectional research cannot measure long-term effects -> Longitudinal studies need to appreciate the influence of several factors in combination: (cumulative) effect of the seizures, effect of drugs, seizure related closed-head injuries, psychological issues |
|
|
Different studies on cognition in epileptic kids
|
1) IQ drop when combination frequent, toxic drug levels, early onset
2) no losses in intelligence 3) no significant IQ drop, but 24% losses more than 9 IQ points 4) lower IQ before study, gained less IQ, especially with longer duration. No association between seizure frequency and full-scale IG. 5) decrease in performance IQ and full-scale IQ. After surgery, no further decline in IQ. 6) increased proactive interference. No epilepsy-related variables had effects on cognition and behaviour 7) Younger age of onset, higher seizure frequency, 2+ anti epileptic drugs were associated with lower IQ and 26% of variance. Generalised symptomatic epilepsy had worst IQ scores. 8) non-verbal intelligence problems, especially with symptomatic epilepsy, early onset, high frequency, polytherapy 9) lower IQ & linguistic abilities 10) frequency = predictor for behaviour difficulties 11) Frequency -> attention deficits and inability to inhibit impulsive responses |
|
|
Different studies on cognition in epileptic adults
|
1) Less IQ improvement in patients with prior status epilepticus
2) normal IQ improvement and no decline in memory in patients with TLE 3) No IQ change, but decrease in visual memory, attention, problem solving, perception 2 other variables. 4) Less cognitive improvement. Nor correlation of frequency and change in performance 5) 50% showed decline in verbal and figural memoir 6) Baseline IQ, lower and no change, whereas control increased. Also lower baseline verbal and visuospatial memory, and decrease verbal memory. No association with seizure related variables. 7) Impaired performance in memory, language, executive function, motor speed. 8) Some studies: correlation of degree of neuropsychological morbidity and duration of epilepsy. Others did not find this correlation |
|
|
Cognition in children with epilepsy
|
- reduced brain volume, especially white matter tissue, extending to extra- temporal regions among childhood-onset patients
-> poorer cognitive status - Studies with children are limited to IQ -> may underestimate changes -> only one study found IQ group change -> cognitive decline in subgroup of 10-25%, which is associated with higher frequency, high drug use, early onset and psychological factors - generalised symptomatic epilepsy has higher risk of intellectual and educational deficits |

