Reading...
![]()
Play button
![]()
Play button
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
Prevalence and Epidemiology
|
- Second most common neurodegenerative disorder after Alzheimer´s disease
- Females = Males - Prevalence 200 per 100,000 (0.2%) - Incidence: -> 30 per 100,000 persons aged 55-65 -> 44 per 100,000 persons aged 85 and older - Life expectancy is about the same as for people without the disease |
|
|
Neurodegeneration
|
- progressive loss of structure or function of neurons, including death of neurons
|
|
|
Effect of Age in Parkinson's Disease
|
- Peak of onset in sixth decade
- Positive correlation between incidences and age - Disease is connected to certain age-related brain alterations - However, PD also in young people: about 10% of all patients develop symptoms before age 50 -> Young onset PD: with onset between 21 and 40 years -> Juvenile PD: with onset at < 20 years |
|
|
Causes of Parkinson's Disease
|
- Genetic factors: 17 genes
- Exposure to toxins or certain viruses may trigger Parkinson's signs and symptoms (e.g. pesticides, herbicides) - Designer drug MPTP |
|
|
Lack of Dopamine in Parkinson's Disease
|
- degeneration of cells of subtantia nigra results in a decreased amount of dopamine
- Result: Dysfunctioning of corpus striatum (part of basal ganglia) -> dysfunctioning of brain areas connected to the striatum (fronto-striatal circuits), e.g motor and premotor cortex and dorsolateral prefrontal cortex |
|
|
Risk factors for Parkinson's disease
|
- age
- positive family history (heritage) - male gender (?) - Environmental exposure (e.g. herbicide and pesticide exposure, metals (manganese, iron), well water, wood pulp mills, steel alloy industries) - Life experiences (trauma, emotional stress, personality traits such as shyness and depressiveness)? - Inverse correlation between cigarette smoking and caffeine intake |
|
|
Motor Symptoms os Parkinson's Disease
|
- PD-symptoms tend to be mild at first and can sometimes be overlooked
- For some people symptoms evolve slowly over 20 years - Motor symptoms do not correlate well with cognitive symptoms - Rigidity - Tremor (usually of the hands) - Bradykinesia - Postural instability |
|
|
Tremor
|
- Resting tremor: Usually occurs in a finger or hand when the hand is at rest, but not when the hand is in use
- Rhythmic shaking: usually four to six beats per second - Or in a "pill-rolling" manner: as if rolling a pill between thumb and index finger - Early symptom in about 70% patients - Mostly begins unilaterally - Suppressed by activity, sleep, concentration - Intensified by stress, fatigue |
|
|
Bradykinesia
|
- Slowness/paucity of movement/motion
- Inability to change direction while walking/difficulty walking around obstacles - When patients want to move, their body may not respond right away, patients may suddenly stop or "freeze" -> E.g. Difficulty getting out of a chair or rolling over in bed - Shuffling walk - "Mask-like" face sometimes found in patients can be due to bradykinesia (also affects facial muscles) - Considerable impairment of daily life - Clumsy or weak limb maybe early sign - Also is expressed as micrographia (small handwriting) |
|
|
Rigidity
|
- Occurs when muscles stay stiff and do not relax
-> E.g. arms may not swing when a person is walking - Possibly cramping or pain in the muscles - Increased muscle tone in both flexor and extensor muscles providing a constant resistance to passive movements of the joints - Most devastating symptoms for many sufferers |
|
|
Postural instability
|
- Stooped posture, with drooping shoulders and their head jutted forward
- Along with other movement issues, patients have a problem with balance (frequent falling and increased risk of falling) - Emerges late in the disease (usually after 8 years or more) |
|
|
Symptoms beyond motor impairment in Parkinson's Disease
|
- Wooden face
- Insomnia (60%), restless sleep or daytime fatigue - Akathisia: unpleasant sensations of inner restlessness manifesting in an inability to sit still - Dysphagia: difficulty swallowing - Oily skin and dandruff - Hypokinetic dysarthria - Dystonia - Hypersalivation, also called ptyalism or sialorrhea - Autonomic dysfunction, e.g. constipation, incontinence - Olfactory dysfunction, decreased sense of smell - Cognitive dysfunction, dementia in later stages of disease - Depressive Symptoms (40% of PD sufferers, "only" 25% major depression) |
|
|
Hypokinetic dysarthria
|
- reduced vocal loudness, harsh or breathy vocal quality and abnormal speaking rates (slow speaking rates but rushes of fast speech)
- linked with basal ganglia control circuit pathology - Manifests itself in any or all levels of speech production; respiratory, phonatory, resonatory, and articulatory |
|
|
Dystonia
|
- ustained muscle contractions cause twisting and repetitive movements or abnormal postures
- painful - Usually occurring in early morning - Very uncommon in untreated patients and more frequently seen as a complication of treatment |
|
|
Cognitive dysfunctions in Parkinson's Disease
|
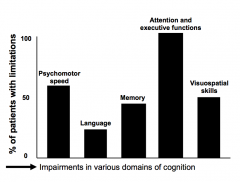
- Cognitive deficits already present at time of diagnosis in about 40% of patients
- 100% of those patients with cognitive impairments (impairments in 3 or more tests) show deficits in attention and "frontal lobe" impairments (i.e executive function deficits, e.g. difficulties changing mental sets) - motor problems may result in poor performance in other cognitive tasks - Also frequent impairment in psychomotor speed - memory impairments on tests requiring spontaneous recall, but NOT on recognition memory tests - likely cause: disruption of the frontal-subcortical (front-striatal) circuits |
|
|
Cognitive dysfunctions BEFORE Parkinson's Disease diagnosis
|
- Cognitive alterations may already be present at very young age
-> controls performed significantly better than individuals with a hyperechogenic SN |
|
|
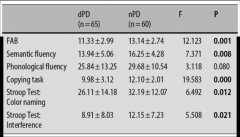
Neuropsychological assessment supporting differential diagnosis
|
- Verbal fluency tasks may be a sensitive measure to differentiate between Parkinson's Disease, Multiple system atrophy and supra nuclear palsy
|
|
|
Course of Parkinson's Disease
|

- gradual and progressive over time
- at different rates across individuals and with different clusters of symptoms across individuals - PD does not cause sudden changes in cognitive functioning - Progression of impairment with course of disease |
|
|
Dementia in Parkinson's Disease
|
- Subcortical dementia
- main aspect: executive problems ("frontal lobe" syndrome) - additional aspects: psychomotor slowing, memory retrieval deficits, alterations in personality and mood - Serious loss of global cognitive ability - Insidious onset and progressive decline - Commonly affects 30 - 40% of patients during course of disease - Affects 17% within first 5 years of disease -> 4 times higher than the incidence in the general population - not tied closely to progression of motor symptoms |
|
|
Features of Dementia in Parkinson's Disease II
|

|
|
|
Features of Dementia in Parkinson's Disease I
|

|
|
|
Depression in Parkinson's Disease
|
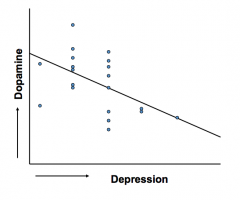
- Prevalence of 40%
- More common in PD than in other chronic, disabling disorder - Not just a psychological reaction to having PD - PD patients with depression show decreased activation in different areas of the brain: A: locus ceruleus B: thalamus C: ventral striatum D: amygdala - Negative relationship between symptoms of depression and levels of dopamine in the striatum in PD |
|
|
Influence of depression on cognition in Parkinson's disease
|
- PD patients with apathy showed a lower global cognitive status and more impairments in executive functioning
- After 18 months: 40% of PD patients with apathy showed a dementia, relative to 5% of PD patients without apathy - co-morbid depression had a negative impact on the number of problems with executive functions in daily life |
|
|
Treatment of Parkinson's Disease
|
- Treatment is aimed to increase dopaminergic input to the two basal ganglia-thalamocortical circuits
- Levodopa (L-dopa) (possibly with with Cardidopa) - Neuroprotection - Surgery: Deep Brain Stimulation - Exercise - "Tricks" to help overcome physical symptoms, e.g. swinging arms to begin walking - Education of caregiver and elimination of non-essential meds is important - Since choline acetyltransferase (ChAT) activity is decreased to 40-60%, there is a good rationale for using acetylchilnesterase inhibitors in individuals with Parkinson's Disease Dementia |
|
|
Levodopa (L-dopa)
|
- Chemical precursor to dopamine
- Most commonly used drug in PD patients - Most effective drug currently available for PD - However, efficacy wears off quickly and taking l-dopa for long may result in ON/OFF syndrome, so that it's important to delay taking L-dopa as long as possible - Common side effects: Nausea, vomiting, and drowsiness - May promotes hallucinations, delusions and confusion - Hallucinations, paranoia and involuntary movements (dyskinesias) may occur with long-term use or overdosage - Best results in combination with Carbidopa, which allows more L-dopa to cross the blood-brain barrier and as the added effect of reducing side effects |
|
|
Surgery: Deep Brain Stimulation
|
- Implantation of electrodes into one of three areas of the brain (globus pallidus, thalamus or subthalamic nucleus - on one or both sides)
- A pulse generator goes in the chest - Electric pulses stimulate the brain to help reduce a patient's rigidity, tremors, and bradykinesia. - It does not stop/cure progression of PD or affect other symptoms - Not every patient suited for Deep Brain Stimulation - Possible side effects include tingling in head and hands, depression, slight paralysis, slurred speech, loss of balance and loss of muscle tone |
|
|
Exercise in Parkinson's Disease
|
- Exercise may have protective effect by enabling the brain to use dopamine more effectively
- Also helps improving motor coordination, balance, gait, and tremor - Working out on a treadmill or biking have been shown to have a benefit |
|
|
Neuroprotection
|
- Protecting neurons from cellular damage induced by biochemical processes associated with PD pathogenesis
- Neuroprotection only for dopamine agonists (drugs mimicking dopamine) - Dopamine agonists (e.g. bromocriptine, pergolide, pramipexole, ropinirole, apomorphine) slow down progression of PD |
|
|
Neuropathology in Parkinson's Disease
|
- primarily basal ganglia
- dysfunction in two of the basal ganglia-thalamocotical circuits: one direct and the other indirect a) direct pathway (facilitating movements) becomes less active b) indirect pathway (inhibits unwanted movements) becomes more active |
|
|
Hoehn and Yahr Scale
|
- 5-point scale of severity of Parkinson's Disease
- Stages refer to motor symptoms only (as it was developed in 1967) 1. Stage Unilateral involvement only, usually with minimal or no functional impairment 2. Stage Bilateral or midline involvement, without impairment of balance 3. Stage First sign of impaired righting reflexes. E.g. resulting in unsteadiness when turning. Demonstrated when pushed from staining equilibrium with the feet together and eyes closed. Patient is now somewhat restricted functionally, but may have some work potential. Patients is physically capable of leading independent lives, and their disability is mild to moderate. 4. Stage Fully developed, severely dieseling disease; the patient is still able to walk and stand unassisted but is markedly incapacitated. 5. Stage Confinement to bed and wheelchair unless aided. |
|
|
ON/OFF syndrome
|
- After 5-10 years on L-dopa patients experience severe side effects
- ON phase -> not long after taking L-dopa -> too much dopamine results in dyskinesias (involuntary movements of limbs, rather like in Huntington's Disease) -> also called "peak-dose dyskinesia" - OFF phase -> very severe Parkinsonian symptoms: severe rigidity, akinesia and tremor -> peak off dyskinesias often preferred over "frozen" OFF phase |
|
|
Huntington's Disease
|
- chronic and progressive
- hereditary disease - Mean onset between 25 and 44 years, however diagnosis usually 8-10 years after onset - Survival after ones 13-17 years - symptoms include motor abnormalities, e.g. chorea and rigidity, and a range of psychiatric, behavioural and cognitive disturbances and a progressive, inevitable decline to a severe dementia |
|
|
Mendelian autosomal dominant inheritance
|
- Huntington's Disease fits the criteria for Medelian autosomal dominant inheritance:
a) equal incidence in and transmission by both sexes b) 50% of the offspring of a parent with Huntington's disease wi become affected c) Offspring without Huntington's disease will not pass it to their descendants |
|
|
Stages of Huntington's disease
|
1. Stage
a) neurological or psychiatric symptoms b) chorea is most prominent motor symptom c) independency is minimally constrained d) death is rare 2. Stage a) motor disorder becomes more generalised, including rigidity and chorea b) individual becomes dependent on others d) death is not common and usually results from apparently unrelated causes 3. Stage a) severe physical disabilities b) demented c) totally dependent d) death may occur at any time, resulting from weight loss, immobility, tendency to aspirate food, increased vulnerability to pneumonia, cardiovascular disease and other diseases |
|
|
Molecular Genetics of Huntington's Disease
|
- in 1 out of 10.000 cases, the Huntington's gene carries a mutation that results in the production of a toxic protein in the striatum, which kills the cells of the striatum
- Genetic marker for Huntington's gene, G8, which provides the possibility of pre symptomatic testing of asymptomatic members of an HD family and to prenatal diagnosis of at-risk pregnancies - All patients with Huntington's disease show expansion of the repeat CAG sequence, indication that this expansion on this gene was the causative mutation involved in Huntington's disease |
|
|
Neuropathology in Huntington's Disease
|
- generalised shrinkage of the brain, with preferred atrophy of the caudate nucleus and putamen, structures in the corpus stratum
- reduced levels of the inhibitory neurotransmitter gamma-Aminobutyric acid (GABA) - increased levels of excitatory neurotransmitters, which can have neurotoxic effect at high concentration - damage of front-striatal circuits resulting impaired executive functioning, e.g. switching mental sets |
|
|
Epidemiology of Huntington's Disease
|
- prevalence various form country to country, 10 times less in Japan compared to Europe
- All cases are the result of the same mutational mechanism: CAG repeat expansion |
|
|
Neurological symptoms of Huntington's disease
|
- chorea (normally among the earliest symptoms)
- dystonias - rigidity (major feature of advanced Huntington's disease) - Bradykinesia (resulting in freezing and gait abnormalities) - Eye movement abnormalities - Dysarthria (speech distortion) - Dysphagia (abnormalities in ingestion) - Loss of weight and muscle bulk in spite of adequate feeding, in later stages of Huntington's disease - Sleepiness during day and wakefulness at night, in later stages of Huntington's disease - incontinence in 20% in the terminal stages - Epilepsy in 1-3% of adults with Huntington's disease and much higher frequency in juvenile HD. |
|
|
Psychiatric symptoms of Huntington's disease
|
- generally very common
- may precede motor - depression experienced by 4-44% of patients - higher suicide rates than healthy population, 5.7% versus 1.5% - In order of decreasing frequency: Dysphoria, agitation, irritability, apathy anxiety, disinhibition and euphoria (30-69%) - Delusion, wired motor behaviour and hallucinations (1.0-11.5) - dementia, chorea and disease duration are NOT correlated with any neuropsychiatric symptom -> However, another study found a relationship between apathy and cognitive function |
|
|
Cognitive impairments in Huntington's disease
|
- Subcortical dementia that progresses to generalised atrophy, especially in the frontal lobes
- In early Huntington's disease, difficulties in planning ahead, switching mental set, impaired pattern recognition and impaired facial recognition as a result of damage to fronto-stratal circuits - Cognitive impairments worsen and gradually extend to affect many areas of cognition |
|
|
Genetic Counseling and Predictive Tests in HD
|
- ideally involves two or more interview spread over weeks or months
- no prediction, if person is at risk for suicide, severe depressive, mental illness - Some labs only people with 50% risk - usually no kids - prenatal prediction possible - Counselor needs to check for coercion for test |
|
|
Management and Therapy of Huntington's Disease
|
- no cure
- Chorea may be treated with neuroleptics that block central dopamine receptors (haloperidol) -> possible side effect: rigidity -> No medication for memory deficits and cognitive impairments -> Regular routines, reduction of environmental stimuli, avoidance of direct confrontation and clear, simple explanations may help to manage problematic behaviour -> Involvement in research can provide stimulation, information and personal support, for both patient and family |
|
|
Risk factors for Parkinson's Disease Dementia (PDD)
|
- advanced age
- severity of motor disease (especially bradykinesia) - early L-dopa associated confusion - depression - Atypical neurological features |
|
|
Dementia with Lewy Bodies (DLB)
|

- one key characteristic: change in alertness/arousal
-> excessive daytime sleepiness -> wide fluctuation in their attention and concentration ("good and bad days") - association with rapid eye movement sleep behaviour disorder - controversy whether Demntia with Lewy Bodies and Parkinson's Disease Dementia are different disorders or the same on a continuum -> Clinical features are similar: attentional deficits, executive abnormalities, frequent concomitant neuropsychiatric disturbances, including visual hallucinations and delusions - DLB better on confrontational naming and memory tests than a AP patient - DLB patients have worse executive functions than AD patients - DLB patients are more apathetic than AD patients |

