Reading...
![]()
Play button
![]()
Play button
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
Incidence of Intracranial Tumours
|
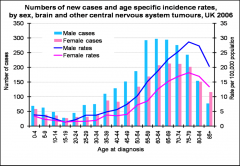
- Intracranial tumours account for approximately 2% of all cancer diagnosis
- Small peak in incidence in early childhood and major peak in people in their 60s to 70s -> Main cause of death in children (after accidents) - Gender differences: meningiomas more frequent in women, gliomas more frequent in men |
|
|
Causes of Intracranial Tumours
|
- Exact causes unknown
- Discussion about: Genetic factors Hormonal factors Exposure to radioactivity Weakened immune system Oncogenic viruses Exogenous carcinogens Brain injuries Exposure to chemicals |
|
|
Cellphone usage and Intracranial Tumours
|
- Early study: for people who have used a modern cellular phone for more than 2000 hours in their lifetime, the risk of getting a brain tumours rose by 270 percent.
- However, no change in incidence trends were observed from 1998 to 2003, the time when possible associations between mobile phone use and cancer risk would be informative about an induction period of 5–10 years - Newer study: No higher risk |
|
|
Types of Intracranial Tumours
|
- WHO grade I: Benign, slow growth rate, possibility of cure following surgical resection alone
-> e.g. Meningioma and Astrocytoma I - WHO grade II: Still benign (semi-benign), tend to recurrence, some tumours types tend to progress to higher grades of malignancy -> e.g. Oligoastrocytoma, Atypical menimgiomas, and Oligodendrogliomas - WHO grade III: Malignant, quick spreading, infiltrative capabilities, radiation and chemotherapy after surgical resection -> Anaplastic meningiomas, Anaplastic astrocytomas, and Anaplastic Oligodendrogliomas - WHO grade VI: Malignant, most aggressive tumour, very fast growth rate, generally associated with a rapid preoperative and postoperative evolution of disease, radiation and chemotherapy after surgical resection -> e.g. Glioblastoma and Gliosarcoma |
|
|
Important difference between intracranial tumours and other tumours
|
- Brain embedded in the solid bony skull
- Hardly any alternatives - Increase of intracranial pressure (pressure on brain tissue) with growing of tumour, so that even benign tumours may lead to serious consequences |
|
|
Tonsillar herniation
|
- A intracranial tumour may increase the pressure in the skull, so that the cerebellar tonsils are forced down into the spinal canal through the foramen magnum
- Consequence: Cerebellar tonsils put pressure on the brain stem and spinal cord - Clinical symptoms can be rapid cardiovascular and respiratory arrest or slow progression over a day or two |
|
|
Clinical presentation of intracranial tumours
|
- Single dramatic and alarming event (e.g. seizure (in 26% of patients), episode of confusion, paraphasic spech)
- Focal neurological signs (numbness, motor weakness (in 45% of patients) - Signs of increased intracranial pressure (headaches (in 54% of patients), nausea, vomiting, drowsiness, visual abnormalities) - Hormonal disorders - Cognitive deficits |
|
|
Frequent delay of detection of intracranial tumours
|
- Unawareness of patient, in particular when prefrontal cortex affected
- Misinterpreatation by family and friends: Attribution of alterations in cognition and personality to aging, stress or depression - In retrospective: Patients and relatives often able to identify subtle signs that were observed long before the presence of disease was suspected |
|
|
Patients' self assessment of cognitive functioning
|
- Loose relationship between test data and patients’ self report due to concealment by or unawareness of patients
|
|
|
Changes of personality in patients with a Intracranial Tumour
|
- Often slow development, in particular in slow growing tumours
- Often misleading character: mimicking psychiatric psychopathology - A case report: man's interest in child pornography had a positive relationship with the growth and regrowth of a intracranial tumour, hemangiopericytoma = meningeal tumor |
|
|
Localisation of Intracranial Tumour
|
- before imaging techniques: clinical npsy assessment
- today: Precise characterisation of tumours by neuroimaging techniques, e.g. location, size, mass effect, oedema and haemorrhage |
|
|
Challenges for clinical neuropsychology in the field ear Intracranial Tumours
|
- 90% with cognitive impairments
- Tumour develop in virtually any brain region - Whole brain may be affected by a single intracranial tumor (e.g. increased intracranial pressure) - Can involve any neurological or neuropsychological symptom - Cognition often but not always conform with principles of localisation expectancies -> Variability in consequences of lesions in the same area that is confirmed by MRI -> Only slight impairments possible although tumour is located in area associated with certain function -> Unpredictable cognitive deficits resulting from intracranial tumours, e.g. language problems with right hemisphere tumour - Npsy assessment is a snapshot since neurophysiological milieu is dynamic (e.g. oedema) - Need of tests with parallel versions since retesting very likely |
|
|
Cerebral Oedema
|
- Extracellular fluid accumulation in the brain
- Swelling |
|
|
Cognitive deficits in patients with intracranial tumours
|

- Large variations in prevalence of cognitive deficits, ranging from 29% in low grade tumours to 90% in other tumours
-> may be explained in measurement population, tumour and treatment differences - No specific neuropsychological profile or deficit is indicative of an intracranial tumour - Comprehensive assessment of all areas of cognition advisable, at least screening of all major domains of cognition - Deficits don't only depend on location, including lateralisation, but also on characteristics of growth and treatment - Possible impairments: a) language b) memory c) visuospatial perception d) time-space orientation e) attention f) executive funtion - Tucha et al. found in pare-surgical investigation impaired executive functions, memory, and attention in 91% pf patients, reporting specific tumour-related effects. |
|
|
Emotional states and Personality in Ptientes with Intracranial Tumours
|
- Depression
- Social Withdrawal - Agitation - Lethargy - Anxiety - Aggression - Appropriateness, e.g. unrealistic optimism - Direct influence of tumour or psychological reaction to diagnosis |
|
|
Pharmacotherapy of Intracranial Brain Tumours
|
- Symptome based initial therapy, involving
a) Steroids: Reduction of cerebral edema surrounding intracranial tumours b) Anticonvulsant medication: Reduction of likelihood of seizures |
|
|
Obstructive hydrocephalus
|
-
- normal flow of cerebrospinal fluid is impaired - associated with extension of cerebral ventricles - occurs when one or more of the ventricles become blocked or trapped by obstructions such as a tumour |
|
|
Conditions and aspects that may accompany intracranial tumours and disrupt functioning
|
- Accompanying conditions
- Epilepsy - Surgical treatments, e.g. intact tissue harmed by accessing the tumour - Neurotoxicity of treatments, e.g. chemotherapy, radiation - Effects of pharmacological treatments, e.g. anticonvulsants - These conditions and aspects interact with age, Premorbid capacities and Environmental demands |
|
|
Treatment of Intracranial Tumours
|
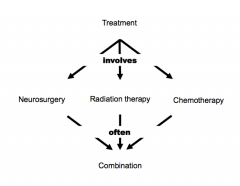
A) Small meningioma
-> Neurosurgical resection with no further treatment -> Focal lesion -> Associated profile remains stable for decades B) Glioblastoma multiforme -> Neurosurgical resection, radiation and chemotherapy -> Widespread lesion -> Dynamic course, e.g. fast re-growth of tumour tissue - Also consider -> Success of treatment, e.g. neurosurgery: Complete removal versus resection in part -> importance of timing and evaluation, e.g. radiation therapy: Long-term consequences of radiation may be different from short-term consequences -> Dynamics: Improved, continued but also evolving cognitive deficits |
|
|
Aims of npsy consultations and assessments of patients with Intracranial Tumours
|
- Analysis of cognitive and emotional functioning
- Monitoring treatment effects, both beneficial and neurotoxic - Screening for evidence of tumour re-growth - Monitoring of recovery - Determination of competencies, both strength and weaknesses - Guidance of rehabilitation |
|
|
Meningioma
|
- diverse set of tumors arising from the meninges, the membranous layers surrounding the central nervous system
|
|
|
Glioblastoma multiforme
|
- most common and most aggressive malignant primary brain tumour
- single most prevalent symptom is a progressive memory, personality, or neurological deficit due to temporal and frontal lobe involvement - also nausea and vomiting, headache,memory loss, and hemiparesis |
|
|
Neurosurgery in patients with Intracranial Tumours
|
- Main aims:
-> Diagnosing the type of intracranial tumour (biopsy) -> Total tumour removal as an attempt to cure from intracranial tumour -> Debulking: Removal of as much of the tumour as possible to slow down growth, improving other treatment response, control of symptoms -> Putting in a small plastic capsule under the scalp (so-called Omaya reservoir) so that chemotherapy can be injected into the tumour - Risk of cognitive deficits related to extent of surgical treatment -> In some tumours, surgery improves or preserves certain functions, e.g. for WHO grade III, neurosurgery is rarely a significant cause of cognitive deficits - Awake neurosurgery (JUNGE!) |
|
|
Neuropsychological improvements following resection of intracranial “space-occupying” tumours
|
- Preoperative impairments of patients (e.g. memory, executive functions)
- In postoperative assessments, patients on average reached at least their preoperative level (e.g. memory, executive functions) - Improvements in attentional functions following neurosurgery (alertness, devided attention, flexibility, processing speed, shifting) - Still impairments despite improvements (attention, executive functions) -> Importance of rehabilitation programmes |
|
|
Awake neurosurgery
|
- Safer approach to the removal of tumours lying on/near important areas (e.g. language or motor centres)
- The key is controlled conscious sedation: Advances in anaesthetic agents have enabled development of the technique - Patients are awake but heavily sedated - Requires awake brain mapping (using electrodes and observing behaviour/functioning) |
|
|
Radiation therapy in patients with Intracranial Tumours
|
- Huge impact on brain, in particular white matter
- Causes apoptosis = programmed cell death - Not all intracranial tumours respond to radiation therapy - Knowledge about immediate cognitive effects limited - Long-term effects on cognition well documented: late radiation effects even as late as 20 years after treatment |
|
|
Stereotactic radiosurgery in patients with Intracranial Tumours
|

- Highly precise form of radiation therapy used to treat intracranial tumours
- Minimally invasive: Access to most inaccessible areas of the brain, without extensive opening of skull and undesirable destruction of normal brain tissue lying above tumour - Limits amount of radiation delivered to adjacent normal brain tissue - Limits unwanted effects on cognition - Procedure 1) Mapping brain in a three dimensional coordinate system (neuroimaging) 2) Screewing of stereotactic frame into skull and fixation of head in place 3) Allow surgeons precise location of brain areas in 3D space 4) Computation of isodose distribution for radioactive seed implants |
|
|
Chemotherapy
|
- Destruction of cancer cells by using anti-cancer or 'cytotoxic' drugs
- Shrinkage of tumour that cannot be operated on or easement of operation - Not all intracranial tumours respond to chemotherapy - Considerable effect on cognitive functions of patients - Detectable changes often delayed by months - most long-term survivors of high-grade glioma will have significant cognitive difficulties, usually evident by the first assessment; some patients will develop profound impairment years later, and few are capable of fully independent living |
|
|
Rehabilitation of patients with Intracranial Tumour
|
- Cognitive and emotional disturbances as typical consequences of intracranial tumours
a) Patients have to cope with for rest of their lives b) Majority of patients require rehabilitation c) Rehabilitation should be individually tailored to needs of each patient (optimal timing and the intensity of interventions are difficult to determine) - Knowledge about rehabilitation in intracranial tumours limited -> only one published study has examined a cognitive-rehabilitation intervention for adults with brain tumors - Patients benefit from rehabilitation programmes -> better results in tests of attention and verbal memory and reported less mental fatigue after 6 months |
|
|
Causes and mechanisms of cognitive impairments in patients with intracranial brain tumours
|
- Tumours cause
a) focal neuro disruption b) mass effects c) alterations of brain connectivity - Focal tumours maybe related to certain cognitive patters, as expected, e.g. Occipotal-parietal tumours may impair visuospatial recognition, semantic competence and social cognition - Alterations of brain connectivity are associated with memory deficits, suggesting whole brain dysfunction - In slow growing tumours, compensation and substitution neural mechanisms tend to mask focal deficits - In high grade tumours, cognitive deficits my be surpassed bay confusion, headache and physical symptoms - clinical-pathological variables, treatment and emotional-behaviourals distress may provoke non-localised cognitive patterns, manifested as mental slowing, poor psychomotor coordination, "frontal" behaviour, personality changes and memory failures |
|
|
Objectives of neuropsychological assessment
|
- need to adept individuals
-> for patients with high grade tumour and short life expectancy assessment may be additional burden - vary according to pahse of disease and treatment, e.g. -> early assessment characterises effects of tumour -> later assessment guides treatment and further decision making as well as monitors changes - Quantification of deficits (inexpensive, non-invasive, repeatable) - Monitoring tumour status and treatment effects - Determination of competencies and planning of rehabilitation, e.g. Cognitive status as predictor of survival in patients with recurrent malignant gliomas - prognosis and predictions |
|
|
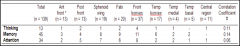
Neuropsychological tests that assess cognitive deficits in patients with intracranial brain tumours
|
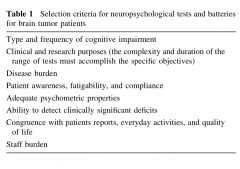
- tests for attention, executive function and memory can detect the main tumour related cognitive deficits
-> Some have clinical and prognostic significance - multidimensional testing enables comprehensive characterisation of the cognitive pattern - should be sensitive to highest and lowest levels of performance in different phases of disease and treatment - should detect changes, even if not statistically significant -> baseline pre-surgical testing is the bomb - Stepwise approach: screening followed by detailed tests -> Screening should not be longer than 30min |
|
|
Non-pharmalogical treatment of cognitive deficits in patients with Intracranial Tumours
|
- much variability in efficacy of cognitive training based on "holistic" memory empowerment
-> mean group improvement observers after 12 weeks -> subjectively perceived cognitive function and scores on verbal attention - Studies lack control groups and randomisation, baseline measures and follow-up evaluation |

