![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
194 Cards in this Set
- Front
- Back
|
Neonate return electrode specifications:
1. weight 2. preferred site 3. power limits |
1. 1-5lbs
2. back, inferior to shoulders 3. max 300 milliamps, < 30 continuous seconds |
|
|
Timing of preop protocols
1. H&P 2. labs 3. ECG |
1. 30 days
2. 30 days 3. 1 year if normal |
|
|
Who needs a prep BMP?
Who needs a prep ECG? |
BMP: age 65+, diabetic, diuretic use, dialysis
ECG: diabetic, cardiac disease, HTN, morbid obesity, CHF |
|
|
RBC, H&H normal values
|
RBC: F: 4.2 to 5.4 million cells/μL
M: 4.7 to 6.1 million cells/μL HGB: F: 12-16 g/dL, M: 14-18 g/dL Hct: F: 37-47%, M: 42-52% |
|
|
WBC normal value
Platelet count normal value |
WBC: 4,000-11,000/μL
Platelet: 150,000-400,000/μL |
|
|
Normal arterial blood gas values
pH PaCO2 HCO3 SaO2 (arterial O2 sat) PaO2 (pp O2 dissolved in blood) |
pH: 7.35-7.45
PaCO2: 35-45 mmHg HCO3: 22-26 mEq/dL PaO2: 80-100 mmHg SaO2: 95-100% |
|
|
Electrolyte values
K+ Creatinine Na+ BUN Ca2+ Urine specific gravity Cl- Total albumin |
K+ 3.5-5.0 mEq/dL Creatinine 0.5-1.5 mg/dL
Na+ 135-145 mEq/dL BUN 10-20 mg/dL Ca2+ 9-11mg/dL USG 1.01-1.03 Cl- 95-105 mEq/dL total albumin 3.5-5.5 g/dL |
|
|
Medications most likely to cause anaphylaxis
|
Abx: PCN, cephalosporins, tetracycline, sulfa, streptomycin, vanco
Insulin, vasopressin, protamine lido, procaine, marcaine opiates |
|
|
Preop guidelines
1. clear liquids 2. breastmilk 3. formula, non-human milk, light breakfast 4. autologous blood donation |
1. cl liq: 2hrs
2. breast milk: 4hrs 3. all others: 6 hrs 4. 2 pints, 2 weeks apart |
|
|
Herbal medications that increase bleeding time
|
garlic,
ginseng, ginko biloba, ginger |
|
|
Herbal medications
Ecchinacea Ephedra St. John's Wort |
Ecchinacea: ↓ immuno suppressants
Ephedra: ↑HR and BP, risk of stroke St. John's Wort: ↓ effects of warfarin, CCBs, ↓digoxin levels |
|
|
ASA classification system
|
P1: normal, healthy
P2: mild systemic disease P3: severe systemic disease P4: disease that is a constant threat to life P5: not expected to live without surgery P6: organ donor |
|
|
General anesthesia
|
reversible, unconscious state
amnesia analgesia depression of reflexes muscle relaxation homeostasis or specific manipulation of physiologic systems and functions |
|
|
Monitored anesthesia
|
local augmented with sedation
|
|
|
Conscious sedation/analgesia
|
specific, short tern procedures
depression of consciousness during which patients respond purposefully to verbal commands pt maintains own airway if pt only responds to pain, then too far sedated |
|
|
Nerve blocks and target regions
1. interscalene 2. infra/supraclavicular 3. continuous lumbar plexus & single sciatic 4. continuous femoral and sciatic 5. continuous sciatic alone 5. continuous paravertebral 6. single paravertebral |
1. shoulder
2. hand, wrist, arm 3. hip 4. knee 5. foot, knee, above/beloe knee amputation 6. pelvic |
|
|
Early signs of local anesthetic toxicity
|
circumoral numbness, metallic taste, dizziness, blurred vision, tinnitus, decreased hearing
|
|
|
Administering blood products
|
verified by 2 RNs
use filter run with NS |
|
|
Signs of transfusion reaction
|
fever, chills, chest/flank pain, nausea
bleeding diathesis, hypotension, hemoglobinuria |
|
|
Inhalation gasses (idiosyncrasies)
|
N2O: no relaxation, causes N/V, can be mixed with other gasses
Desflurane: needs heated vaporizer Halothane: MH |
|
|
Opioids (idiosyncracies)
|
-fentanil (or -fentanyl)- short duration 0.5 hr
morphines - long duration (4-5h) DepoDur - morphine for epidural (48hrs) |
|
|
IV anesthetics (idiosyncrasies)
|
diazepam - long duration (residual effects 20-90hr)
ketamine - short acting, hallucinations midazolam - amnesia, short acting propofol - rapid onset, half life 34-64 min Pentothal - apnea, CV depression, laryngospasm |
|
|
Non-depolarizing muscle relaxants, which are long acting?
|
tubocurarine
pancuronium |
|
|
Depolarizing muscle relaxants
|
Succinylcholine
|
|
|
Cholinergics
|
neostigmine
reverses effects of non-depolarizing neuromuscular blockers give with atropine of glycopyrrolate |
|
|
Anticholinergics
|
atropine
Glycopyrrolate - prolonged duration, lower incidence of arrhythmias than atropine do not give to narrow-angle glaucoma |
|
|
Local anesthetics - duration
1. bupivacaine 2. chlorprocaine (Nesacaine) 3. lidocaine 4. ropivacaine 5. tetracaine |
1. 120-240min
2. 30-45min 3. 60-120min 4. 2-8hr 5. 60-180min |
|
|
Local anesthetics - max dose
1. bupivacaine 2. chlorprocaine (Nesacaine) 3. lidocaine 4. ropivacaine 5. tetracaine |
1. 2.5mg/kg
2. 600mg 3. 7mg/kg with eli, 5mg/kg plain 4. 200-250mg 5. 1.5mg/kg |
|
|
When to reassess patient position
|
when patient or environmental variables change
|
|
|
Pre-positioning focused assessment
|
skin integrity, ROM, prostheses, medical conditions, implants
|
|
|
Supine position
1. nerves 2. pressure points 3. complications |
1. brachial plexus, ulnar
2. occiput, scapulae, olecranon, thoracic vertebrae, sacrum, coccyx, calcaneus 3. vena cava and aortic compression (bump under Rt hip of pregnant pt) |
|
|
Trendelenburg position
1. nerves 2. complications |
1. brachial plexus
2. ↑ICP, ↑IOP, venous thrombosis (cerebral), retinal detachment, cerebral edema, ↑work of ventilation, shearing, atelectasis, pulmonary congestion/edema Do not use shoulder braces if arms on arm boards |
|
|
Reverse Trendelenburg position
1. nerves 2. complications |
1. common peroneal
2. DVT (need SCDs), hypotension, CV overload at return to supine shearing, padded footboard |
|
|
Fracture bed position
1. nerves 2. pressure points |
1. perineal, pudendal, ulnar
2. one foot in traction - distal pulses before, during, after positioning ulnar nerve (arm on op side secured across body over post - post and holder should be distal to elbow - avoid pressure on cubital tunnel) |
|
|
Lithotomy position
1. nerves 2. complications |
1. common peroneal, tibial, sciatic, femoral, obdurator, saphenous (depending on stirrups)
2. hip fx, dislocation, diminished lung capacity, DVT (SCDs >2hrs), crushed fingers, severe hypotension returning to supine knee crutch stirrup: common peroneal and tibial nerves candy cane stirrups: tibia leans against post - common peroneal nerve -> foot drop when hips abduct >90 degrees, stretch sciatic and obdurator |
|
|
Fowler's (sitting) position
1. nerves 2. pressure points 3. complications |
1. sciatic
2. scapulae, sacrum, coccyx, ischial tuberosity, backs of knees, calcanei 3. DVT, venous air embolism, stretch injury to sciatic, displacement of ET tube during positioning |
|
|
Semi-Fowler's (Beach chair) position
1. nerves 2. pressure points 3. complications |
Same as Fowler's, but not as severe
|
|
|
Prone position
1. nerves 2. pressure points 3. complications |
1. optic, facial, lingual, buccal, brachial plexus, radial(arms hanging over sides of bed), ulnar (from too tight tucking or flexing greater than 90 degrees)
2. cheeks, eyes, ears, breasts, genitalia, patellae, toes, iliac crests 3. ET tube displacement, diminished lung capacity, conjunctival edema, corneal abrasion |
|
|
Jackknife position
1. nerves 2. pressure points 3. complications |
same as prone plus DVT - check distal pulses before, during, after procedure, SCDs or TED hose
|
|
|
Kneeling (knee to chest) position
1. nerves 2. pressure points |
same as prone plus extreme pressure on knees and ankles, DVT in lower extremities
palpate pedal pulses |
|
|
Lateral/lateral chest/lateral kidney position
1. nerves 2. pressure points 3. complications |
1. brachial plexus, common peroneal
2. ear, acromion, ribs, ilium, greater trochanter, medial and lateral condyles, malleolous 3. vena cava occlusion, iterference with cardiac action, ptosis of eyelid, renal artery thrombosis. may need to use PEEP do ventilate dependent lung, DVT |
|
|
Type of surgical site infections
|
Superficial incisional - only skin or subQ tissue
Deep incisional - involves deep soft tissues Organ/Space - involves any part of the anatomy other than the incision which was opened or manipulated For infections in multiple spaces, report the deepest one Do not report stitch abscess, infection of episiotomy or circumcision, infected burn |
|
|
Characteristics of a surgical site infection
|
1. occurs within 30 days of surgery (1 year for implants)
2. related to the surgery 3. AND at least one of the following - drainage (inflammation with incisional site SSI) - opens spontaneously or by surgeon with signs of infection (unless negative culture) - abscess - diagnosis by physician |
|
|
four components of care to reduce SSIs
|
1. abx: selection, timing, d/c within 24 hrs
2. hair removal: clippers, as close to incision time as possible, outside the OR (except for hair on head, then shave under anesthesia) 3. post op glucose control: cardiac patients 4. postop normothermia: colorectal patients |
|
|
Skin prep (general)
|
1. clean umbilicus before rest of abdomen
2. clean traumatic orthopedic injuries with pulse lavage 3. prep donor site first if applicable 4. if possible malignancy, do not scrub 5. clean areas of highest bioburden last: axilla, vagina, anus, open skin lesions, soiled traumatic woulds, stomas 6. if stoma part of incisional site, cover with sterile gauze, clean around stoma, then clean stoma last 7. if stoma in operative area (but will be draped out), cover with tegaderm then begin skin prep |
|
|
Skin prep - eye
|
1. topical eye drop if pt awake
2. 5% povidone-iodine drops to eye surface (contraindicated for pts with topical iodine allergy) 3. May use hexachlorophene for pts with allergy, but NOT on surface of eye) 4. clean lid margins with Qtip by everting 5. irrigate with sterile, tepid NS 6. blot dry periorbital, eyelid, lashes, at least 1 inch diameter beyond periphery begin at center of eyelid |
|
|
skin prep - lower face and nose
|
1. begin at bridge of nose
2. move outward to hairline and down to mandible 3. use Qtips to cleanse nostrils 4. paint from nose to periphery most wounds considered clean-contaminated |
|
|
skin prep - ear
|
1. secure hair and define op site with drapes or towels
2. squeeze sponges almost dry to prevent pooling 3. prepare from center of ear 4. extend to face and neck 5. cotton may be used to absorb prep in external ear 10% povidone iodine safe for middle ear space swab, do not let prep pool in ear other preps are ototoxic - do not use inside ear often prep face, neck, down to nipple line |
|
|
skin prep - neck and head/neck
|
1. cleanse from incision to periphery
2. prep neck anteriorly and laterally from mandible to mid sternum, including tops of shoulders 3. for head/neck also cleanse lower portion of face and head around ears |
|
|
skin prep - chest or breast
|
1. prep from top of shoulder to below diaphragm
2. prep from edge of non-op breast to table line, including upper arm to elbow and axilla 3. breast biopsy: prep incision and 3 inches diameter |
|
|
skin prep - abdomen
|
1. prep breast line to groin, table line to table line
|
|
|
skin prep - back/prone
|
1. prep shoulders to top of buttocks, table line to table line
|
|
|
skin prep - chest and kidney, lateral position
|
1. shoulders to ileum and anterior and posterior chest wall for thoracic
2. mid chest to hip, anterior to posterior for kidney |
|
|
skin prep - perineum/vagina
|
Always prep the abdomen before beginning vag prep
Remove clots in vaginal vault and any gross blood before beginning prep 1. pubis to anus, inner aspects of thighs 2. cleanse pubis down to anus and discard swab 3. scrub labia majora to inner thighs, working out 4. prep vagina 2-3 times with prep stick (not CHG) 5. if foley, prep first, change gloves, put in foley |
|
|
skin prep - hand/forearm
|
1. begin at fingertips, move to elbow
|
|
|
skin prep - elbow and upper arm
|
1. cleanse from incisional site to periphery
|
|
|
skin prep - shoulder
|
1. prep from mid neck to elbow including shoulder, scapula, chest to nipple
2. cleanse axilla last |
|
|
skin prep - hip, semi-lateral
|
1. impervious adhesive U-drape to isolate perineal area
2. prep from waist to mid-buttocks and to lower outer aspect of abdomen 3. leg from hip to ankle |
|
|
skin prep - knee
|
1. cleanse knee to tourniquet, discard stick
2. cleanse knee to ankle |
|
|
skin prep - foot/ankle
|
1. start with toes and move to mid-calf
|
|
|
skin prep - open heart
|
1. chin to toes including both legs, circumferential
2. begin at torso, move out 3. on leg, begin at incision and continue out 4. prep groin separately and isolate with impervious towel |
|
|
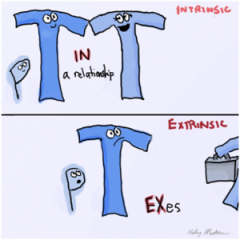
Prothrombin Time (PT)
|
11-13 sec
measures: extrinsic clotting - time it takes for clotting to occur measures factor VII elevated with anticoagulant, ASA, NSAIDs (The 7 year itch caused the 2 T's to become ex's) |
|
|
Partial Thromboplastin Time (PTT)
|
30-40 sec
measures intrinsic and common clotting pathways all factors except VII and thrombin (XIII) used to assess Heparin therapy |
|
|
Counts:
1. sharps 2. sponges |
1. count when the possibility exists that one could be left in a patient
2. count for all procedures |
|
|
Tourniquet placement
|
1. upper arm and thigh: point of maximum circumference
2. forearm: midforearm 3. calf: proximal edge on largest part of calf 4. ankle: over lower third of lower leg, with distal edge proximal to malleoli |
|
|
Max tourniquet times
|
1. upper limb: < 1hr
2. lower limb: <2hrs 3. reperfusion: 5 minutes for every 30 minutes |
|
|
tourniquet inflation pressure
|
LOP: limb occlusion pressure
add 40mmHg for LOP <130mmHg add 60 mmHg for LOP 131-190mmHg add 80 mmHg for LOP > 190mmhg add 50 mmHg for children |
|
|
Types of patient return electrodes (idiosyncrasies)
|
1. dry adhesive: do not touch adhesive, fluid invasion
2. water based gel: must be stored flat, do not touch adhesive 3. hydrophilic conductive adhesive: shorter shelf life 4. reusable capacitive: grounding pad, do not use on pts < 25lbs, cover only with a single layer of linen |
|
|
smoke evacuation
|
triple filter system
1. prefilter 2. ultra low penetrating air filter (ULPA) 3. charcoal filter |
|
|
Cleaning/storing endoscopic equipment
|
1. high-level disinfection ok if sterilization not possible
2. loosely coil during packaging 3. warm lens prior to use to prevent fogging 4. illuminated light cord gets hot enough to ignite drapes in O2 rich environment |
|
|
Laparoscopic insufflation pressures
|
1. maintain pressure between 14-16mmHg
2. deliver CO2 15-20L/min 3. cover trochar openings when inserting/removing instruments 4. too high pressure can force CO2 into the blood 5. ETCO2 is very important |
|
|
Veres needle placement, verification
|
Patient in Trendelenburg position
place needle at 45 degree angle Verify placement by negative blood and bowel return on aspiration and by saline instillation that meets little resistance |
|
|
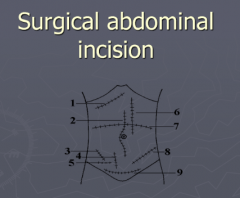
1. subcostal
2. midline 7. tranverse abdominal 3. McBurney 8. oblique 4. Battle 9. Pfannestiel (suprapubic) 5. lower oblique inguinal 6. paramedian - Rt: gallbladder, biliary system, pancreas, Lt: spleen Also, thoracoabdominal - lateral position, for proximal stomach, distal esophagus, anterior spine Midabdominal transverse - retroperitoneal approach |
|
|
Controlled substance categories
|
I high potential for abuse, no medical use
II high abuse, Rx needed, cannot be renewed III high psychological dependency IV low potential for abuse V subject to state and local regulations |
|
|
Pregnancy categories
|
A. no risk
B. no risk in humans C. fetal risk cannot be ruled out D. fetal risk X. contradindicated |
|
|
Most important variable in dosage
|
patient weight
|
|
|
Types of drug reactions
|
1. toxicity - too much drug
2. allergy - must be sensitized, not dose dependent 3. idiosyncrasy - no prior sensitization (MH) |
|
|
Process of hemostasis
|
1. vascular response
2. platelet aggregation 3. coagulation 4. fibrinolysis |
|
|
D/C guidelines for anticoagulants
|
Warfarin: 3 days
ASA, NSAIDS: 3-5 days Plavix 5-7 days |
|
|
Symptoms of hypersensitivity to contrast
|
flush, warm feeling, urticaria, pain at injection site
|
|
|
Allergic cross reactions
|
paromycin, kannamycin, streptomycin, gentamicin
|
|
|
how long to apply pressure to inner canthus?
|
30-60 seconds
|
|
|
how long to remain on side for otic medications?
|
2-3 minutes
|
|
|
what to do after giving nasal med?
|
remain supine 1 min, breathe through mouth
|
|
|
heparin compatibility
|
not compatible with anything
bolus can cause transient decreased BP |
|
|
Mydriatic drugs
contraindicated for angle closure glaucoma |
anticholinergics: atropine
cold medicine: phenylephrine benzodiazapines |
|
|
Where to use epi 1:100,000/1:200,000
|
high concentration 1:100,000 - scalp, face
low concentration 1:200,000 - back, extremities |
|
|
Methemoglobinemia
|
from using hurricane spray (bezocaine, lidocaine)
hemoglobin unable to bind and transport O2 SpO2 and blood gasses appear normal but pt cyanotic treat with methylene blue |
|
|
Common anticoagulant hypersensitivity
|
Dextran 40 - antiplatelet
|
|
|
Common hypersensitivity to local anesthetic
|
esthers - procaine, chloroprocaine, tetracaine
|
|
|
1. Isotonic fluids
2. hypotonic fluids 3. hypertonic fluids |
1. NS, LR, 5% dextrose in water
2. 0.45% saline, 2.5% dextrose in water 3. 5% dextrose in NS, 10%, 20%, 50% dextrose in water, 3% saline |
|
|
1. Amount of air for air embolus airlock
2. precautions to prevent air embolus 3. interventions |
1. 50mL
2. Trendelenburg position during central line insertion 3. clamp tubing, place pt in Trendelenburg on left side |
|
|
Hypothermia temperatures
|
Normothermia: 96.8-100.4
Hypothermia: under 96.8 deterioration of vital functions: under 91.4 |
|
|
OR temp and humidity parameters
|
Temp: 68-73 F
Humidity: 30%-60% positive pressure air exchanges: 15 per hour |
|
|
How often should electrical devices be inspected?
|
regularly, per facility policy
|
|
|
How often should lead aprons be inspected?
|
once a year
|
|
|
Concentration to make an O2 rich environment
|
21%
also, N2O and O2 together |
|
|
Managing fires
1. small fire 2. large fire 3. airway fire 4. equipment fire |
1. smother with wet towel
2. remove burning materials, extinguish away from the field, stop breathing gases, 3. remove ET tube, stop O2, reintubate and use room air 4. cut off ignition source |
|
|
Cut and coag currents
|
Cut: heats cellular contents to boiling so they explode
Coag: gradual rise in temp causes denatured proteins |
|
|
Laser safety
|
identify hazard zone with signs
eye protection high filtration masks ET tube cuffs filled with tinted water, designed for laser use apply moistened sponges around ET tube wet sponges around target tissues do not use alcohol based skin prep |
|
|
Types of latex allergies
|
Irritant contact dermatitis: erythema, dryness, cracking
Allergic contact dermatitis:rash 24-48 hours, away from area exposed Allergic reaction: hives, ariway |
|
|
What if you don't have a latex safe environment?
|
schedule pt first case of the day, premeditate with antihistamine or corticosteroids
|
|
|
When to perform terminal cleaning?
|
At the end of each day and each 24 hour period of the regular workweek
|
|
|
How often to clean a sterilizer?
|
weekly or monthly according to facility policy
|
|
|
Items that need to be cleaned weekly
|
Ice scoop
patient refridgerator aerators and faucets eye wash stations |
|
|
Prepping items for a washer/sterilizer
|
remove gross debris in cold water
|
|
|
Prep instruments for sterilization
|
place broad instruments and those with concave surfaces in side position
disassemble open hinged instruments flush lumens and channels with distilled, demineralized, sterile water before steam remove stylets max weight of a single tray = 25lbs |
|
|
Order of operations for cleaning flexible endoscopes
|
1. preclean at point of use (flush with enzymatic)
2. transport to decontamination area 3. perform leak test 4. manually clean with enzymatic 5. high-level disinfection/sterilization 6. flush channels with water 7. flush with 70% or 90% ethyl or isopropyl alcohol 8. visually inspect 9. store vertically, all attachments detached, in cleanable cabinet, not touching other endoscopes 10. reprocess before use if not used for more than 5 days |
|
|
Gravity displacement sterilization times
|
250F (121C) 270F (132C) Dry
Wrapped 30min 15min 15-30min Textile 30min 25min 15min |
|
|
Dynamic air removal times
|
270F (132C) 275(135) Dry
Wrapped 4min 3min 15-30/16min Textile 4min 3min 15/3min |
|
|
Flash: gravity displacement
|
no lumen: 3 min at 270-275
lumen, porous, mixed: 10 min at 270-275 |
|
|
Flash: dynamic air-removal
|
non-lumen: 3 min at 270-275
lumen, porous, mixed: 4 min at 270, 3 min at 275 |
|
|
Ethylene oxide key points
|
clean and DRY items before sterilization
open door immediately after cycle runs aerate and cool monitor with Bacillus atropheaus in every load |
|
|
Ethylene Oxide sterilization parameters
|
Time: 105-300 min
Temp: 99-145 F Humidity: 45-75% Concentration: 450-1,200 mg/L |
|
|
Liquid chemical (paroxyacetic acid)
|
highly corrosive
do not need to dry instruments before sterilization rinse instrument after sterilization 30 minute cycle immediate use nontoxic monitor daily with BI |
|
|
low temp gas plasma
|
no need for aeration
DRY items before sterilization package items before sterilization items are dry at end of cycle monitor every load with BI |
|
|
Ozone sterilization
|
no aeration required
monitor every load with BI |
|
|
Types of chemical indicators
|
Class I: outside of package
Class II: Bowie-Dick (test daily) Class III-IV: reacts to 1+ parameters of sterilization Class V: reacts to all critical parameters (correlated with BI) Class VI: reacts to all critical parameters of specific cycle |
|
|
Monitor routine load release - non implants
|
physical monitoring
external and internal indicators optional process challenge device |
|
|
Monitor routine load release - implants
|
physical monitoring
external and internal indicators process challenge device |
|
|
What makes up a process challenge device?
|
one of the following:
- BI - BI + Class V indicator - Class V indicator - Class VI indicator |
|
|
Routine sterilizer efficacy testing
|
Physical monitoring
external and internal chemical indicators weekly (pref daily) BI daily Bowie-Dick for pre-vac for sterilizers >2cubic feet, monitor fullyloaded chamber for IUSS cycles, monitor empty chamber |
|
|
When to monitor with BI
|
Steam: all implants, weekly (pref daily)
EO: every load Peracetic acid: daily H2O2 plasma: every load Ozone: every load |
|
|
Sterilization for which instruments must be dry
|
EO
H2O2 plasma |
|
|
Sterilization processes for immediate use only
|
Flash
Peracetic Acid |
|
|
Sterilizer efficacy testing with BI
1. weekly 2. daily 3. every load |
1. Steam
2. Peracetic acid 3. EO, H2O2 plasma, O3 |
|
|
Run times for prions
|
instruments that cannot be adequately cleaned or require low temp sterilization should be discarded
immerse in 1Normal sodium hydroxide for 1 hour, rinse, steam as follows: gravity displacement: 60min at 272F dynamic air removal: 18 min at 272F |
|
|
Corrosive sterilization techniques
|
Paracetic acid
H2O2 |
|
|
High level disinfection (exposure time depends on concentration)
1. Glutaraldehyde (HLD) 2. Ortho-phthaldehyde 3. also par acetic acid, H2O2 |
1. respiratory irritation, fixes blood and tissue to surfaces
2. stains protein grey, eye irritation |
|
|
Tissue banking - storage unit monitoring
|
monitor and log daily
annual calibration checks alarm system |
|
|
Wound classifications
|
I clean
II clean contaminated III contaminated IV dirty contaminated |
|
|
Clean wounds (Class I)
|
uninfected operative wound
no inflammation encountered respiratory, alimentary, genitourinary tracts not entered no signs of infection breast biopsy, total hip, open heart |
|
|
Clean contaminated (Class II)
|
respiratory, alimentary, or genitorurinary tract is entered under CONTROLLED conditions
no signs of infection no break in surgical technique non perforated appendectomy, hysterectomy, thoracotomy |
|
|
Contaminated (Class III)
|
open, fresh, accidental wounds or operations with major breaks in surgical technique
signs of infection gross spillage from GI tract penetrating abd trauma involving bowel, gunshot wound to abdomen |
|
|
Dirty/infected (Class IV)
|
old, physically induced wounds with retained devitalized tissue
wounds that involve a clinical infection or perforated viscera I&D of abscess, delayed primary closure after ruptured appendix |
|
|
Spaulding classification system
1. critical 2. semicritical 3. non-critical |
1. enter bloodstream or sterile tissues - needs to be sterilized
2. contact mucous membranes and non-intact skin - HLD if sterilization not available, kill everything except high numbers of spores 3. contact intact skin - intermediate level disinfection - does not kill spores 4. items that do not contact patient - low level disinfection - does not kill mycobacteria, spores, non lipid viruses |
|
|
Specimens
1. bladder/gallstones 2. frozen section 3. pap 4. bone marrow biopsy 5. Gram stain 6. spinal tap 7. acid fast TB 8. fungal cultures |
1. no formalin. send dry or in saline
2. call when procedure begins, send dry 3. write on slide in pencil 4. 2 samples: aspiration and core biopsy 5. aerobic culturette, transport immediately 6. use tubes provided in kit - send 3 separate tubes 7. aerobic, send immediately 8. swabs acceptable for vag cultures only, send immediately |
|
|
Absorbable sutures
|
gut, polyglactin (Vicryl), Monocryl, Maxon, PDS, Panacryl (longest time before absorption)
Use rapidly absorbable suture in urinary and biliary tracts - can precipitate stone formation |
|
|
Non-absorbable sutures
|
silk, stainless steel, nylon, Mersilene, Ethibond, Prolene
|
|
|
What sutures are more prone to infection?
|
multifilament
continuous suture line Use monofilament or absorbable suture in contaminated areas |
|
|
Cutting sutures
|
surgical gut - 6mm
synthetic - 3mm |
|
|
Staples
|
-reduce tissue trauma
- uniform tension on suture line - usually in 5-6 day for chest or abdominal |
|
|
PT vs PTT mnemonic
|
|
|
|
When to discontinue anticoagulants?
1. ASA 2. NSAIDs 3. Plavix 4. Coumadin |
1. 3-5 days
2. 3-5 days 3. 7 days 4. 1-3 days |
|
|
How long does it take to clot a small vessel with direct pressure?
|
15-20 seconds
|
|
|
Hemostatic clips
|
decreased risk of FB reaction from suture
stainless steel or titanium |
|
|
Thermal coagulation sites of electrical burns
|
return electrode
ECG leads temperature probe sites positional pressure points where pt comes in contact with grounded metal use all plastic or all metal trocar systems to prevent burns |
|
|
Argon enhanced surgery
|
uses stream of argon gas to conduct electricity
blows blood off the tissue, use for non-contact coagulation, less tissue damage risk of gas embolisms |
|
|
Tissue fusion
|
collagen and elastin in vessel wal liquefy to form a seal
bipolar configuration |
|
|
ultrasonic devices
|
vibrates at 55,500 times per second
cut coaptation - adherence of tissue at low temp coagulation - rise in temp leads to release of water vapor cavitation - rapid volume changes of tissue and cell fluid - plane dissection and visibility produces infectious aerosols |
|
|
Chemical coagulants of bovine origin
|
microfibular collagen hemostat (Avitene)
absorbable collagen sponge (Instat, Hemopad) Thrombin Fibrin gel (glue, sealant, Floseal) |
|
|
Chemical coagulants that must be applied dry
|
microfibular collagen hemostat
absorbable collagen sponge oxidized regenerated cellulose (Surgicel) |
|
|
What chemical coagulant may cause burring, stinging, headache, sneezing?
|
oxidized regenerated cellulose
|
|
|
Which chemical coagulants impede the action of methyl methacrylate?
|
microfibular collagen homestat
absorbable collagen spone |
|
|
Inflammatory stage of wound healing
|
immediate to 2-5 days
hemostasis inflammation wound edges seal to bacteria in 4 hours |
|
|
Proliferation stage of wound healing
|
2 days - 3 weeks
granulation contraction epithelialization |
|
|
Remodeling stage of wound healing
|
3 weeks-2 years
collagen remodelling |
|
|
Surgical complications
|
POD 0-2 - pulmonary
POD 4-7 - surgical wound complications POD 6-9 - intraabdominal abscess, anastomotic leak, thrombophelbitis |
|
|
adynamic ileus
|
normal post and surgery 3-5 days
if persistent, suspect peritonitis, hypokalemia, wound dehiscence |
|
|
Max daily doses of common analgesics
1. acetaminophen 2. ASA 3. IBU |
1. 3000mg
2. 4000mg 3. 2400mg |
|
|
Peak/duration of common opioids
1, morphine 2. fentanyl 3. hydromorphone 4. meperidine |
Peak/duration
1. 20min/4-5hrs 2. 3-5min/30-60min 3. 0.5-1hr / 3-4 hrs 4. 5-7 min/ 2-4 hrs |
|
|
Guidelines for discharge from ASC
|
VSS
baseline orientation ambulation without dizziness minimal pain and PONV minimal bleeding at surgical site |
|
|
Discharge instructions should include:
|
medication use
when to contact HCP, include phone number activity, diet, wound care no driving, making decisions, operating heavy machinery 24 hours |
|
|
Motor vehicle crash
|
speed affects kinetic energy more than mass
|
|
|
What is Waddell's Triad?
|
pattern of injury seen in pedestrian children who are struck by motor vehicles.
fractured femoral shaft - hit side intra-thoracic or intra-abdominal injuries - hit side contralateral head injury - opposite side |
|
|
AMPLE method of trauma assessment
|
A - allergies
M - medications/drugs P - past Hx (medical/surgical) L - last meal, last tetanus E - events leading to injury |
|
|
How much is one unit of blood?
|
450mL
normal adult has about 12 units of blood |
|
|
1. allodynia
2. hyperalgesia |
1. pain from stimulus that is not usually painful
2. stimuli that are normally painful produce exaggerated pain |
|
|
Nociception
1. A-delta fibers 2. C fibers |
1. skin, muscle - myelinated, well localized pain
2. muscle, peritoneum, viscera - poorly myelinateddiffuse, dull pain |
|
|
1. acute pain
2. chronic pain |
1. < 6 months, often had SNS component
2. > 6 months, rarely has SNS component |
|
|
Mu receptor
|
responsible for supra spinal analgesia, CV and reap side effects, constipation, euphoria, physical dependence
sufentanil - highest affinity for mu receptors meperidine - lowest affinity for mu receptors |
|
|
Influence of chronic opioid use on hormonal systems
|
reduced: cortisol, lutenizing hormone, FSH, testosterone, estrogen
increased: prolactin suppressed immune function |
|
|
Nursing considerations with meperidine
|
no more than 600mg/day for 48 hours
early signs of toxicity: myoclonus, confusion,potential for seizures |
|
|
epidural opioids
|
fentanyl - produces segmental anesthesia - catheter placement is very important
morphine - dissolves readily in CSF, braod spread of analgesia, long duration |
|
|
clonidine
|
prolong and intensify anesthesia, allow for decreased opioid doses
sedation, dry mouth, bradycardia, hypotension |
|
|
sedation scale
|
0 - alert
1 - occasionally drowsy, easily aroused 2 - frequently drowsy, easily aroused 3 - somnolent, difficult to arouse S - normal sleep |
|
|
Peds lung development
|
viable outside the womb at 24-26 weeks
alveoli increase in size and number until age 8 |
|
|
Differences in children
|
O2 consumption 2-3x adults
inc. respiratory rate higher anesthetic uptake primary nose breathers until 3-4 months susceptible to hypothermia - keep OR at 85 degrees inc risk of hypoglycemia inc risk of hypovolemia (evaporation, inability to concentrate urine) |
|
|
Separation anxiety
|
none until 4-8 months
greatest in children under 4 years old toddlers and older children benefit most from PPI |
|
|
Talking to children
|
<2 years - fear of mutilation, aware of body intactness - give a band aid
preschool - blame parents or others for illness, misinterpret meaning of procedures < 4 years - show equipment, may not need explanation of anatomy schoolage - blame self for illness, fears death, regression, discuss anatomy and why the procedure is happening |
|
|
Pediatric electrosurgery
|
1-6lbs - neonatal pads, on back inferior to scapulae, superior to sacrum
6-30lbs - infant pads, back or torso when size permits, use adult pads |
|
|
Intubation in peds
|
rolled towel under shoulders for head positioning
cricoid pressure 3-4kg |
|
|
Ramstedt procedure
|
pyloromyotomy
Rt transverse incision |
|
|
1. omphalocele
2. gastrochisis |
1. liver herniates in sac through abdominal wall
2. opening Rt of umbilicus, no sac, intestines herniate both - may have pressure on inferior vena cava post op - look for edema of lower extremities |
|
|
Repair of esophageal atresia
|
Lt lateral with Rt arm extended above head
|
|
|
Repair of diaphragmatic hernia
|
emergency surgery - acute respiratory distress
Lt subcostal or transthoracic approach |
|
|
Kasai procedure
|
Roux-en-Y for biliary atresia
Rt subcostal incision jejunum to liver hiles, end to side anastomosis to restore intestinal continuity -Post procedure: methylprednisolone (stimulates bile salts), ursodeoxycholic acid -cholangitis, portal hypertension, intestinal obstruction |
|
|
4 exceptions to informed consent
|
1. threat off immediate death or disability
2. pt waives right to full disclosure 3. provider withhold's info when it would be detrimental to treatment, then must give full disclosure when threat has passed 4. prior pt knowledge about procedure |
|
|
1. young old
2. middle old 3. old old |
1. 65-74
2. 75-84 3. over 85 |
|
|
Changes in the elderly (memory joggers)
|
- constipation more from lifestyle changes than physiologic changes
- diminished thermoregulation, tactile sensation, pain perception - decreased immunity - less efficient kinesthetic sense (balance problems) - decreased heat tolerance, increased cold tolerance |
|
|
1. ectropion
2. entropion |
1. lower eyelid rolls out
2. lower eyelid rolls in lenses thicken, yellow, cloudy, less elastic - dec night vision, narrowed visual field, diminished ability to distinguish colors yellow, red, orange easier on eyes |
|
|
Risks for the elderly
|
infection - dec immunity
fluid volume deficit impaired skin integrity hypothermia altered vital signs nutrition - pressure sores develop in 2 hrs |
|
|
causes of disturbed thought processes
|
hypoxia, glucose levels, altered metabolism, drug interaction, tumors, infarcts
should be able to remember 3-7 words and repeat them back |
|
|
teaching older pt
|
keep pitch of voice low
use visuals slow down, short segments have them practice cough, deep breathe, turn, ambulate they want sensory info about events that will happen rather than procedure information |

