![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
68 Cards in this Set
- Front
- Back
|
Taxonomic classifcation Clostridium spp? (6)
|
Kingdom - Bacteria
Phylum - Firmicutes Class - Clostridia Order - Clostridiales Family - Clostridiaceae Genus - Clostridium |
|
|
Clostridium spp. characteristics? (6)
|
1. GPR - obligate anaerobic spore forming
2. Spore deforms cell 3. Spore variations to spp. 4. Flagella (+) (not C. perfringens) 5. Loci: soil + normaflora (i.e. gut, feces) 6. Lecithinase (+) 6. LT survival 7. Gas produces + high biochemical activity |
|
|
Clostridium spp. are distinguished based on? (3)
|
Pathomechanism:
i. gas gangrene/histolytic - C. perfringens ii. Neurotoxic - C. tetani + C. botulinum iii. Enteric - C. difficile |
|
|
Clostridium perfringens characteristics ? (6)
|
1. GPR - obligate anaerobe spore forming
2. Flagella (-) 3. Capsule (+) 4. Central spore, pear-shaped rod 5. Double hemolytic zone (blood agar) 6. High gas producer |
|
|
C. perfringens VFs: EXOENZYMES? (3)
|
1. Collagenase
2. Hyaluronidase 3. DNAse |
|
|
C. perfringens VFs: SURFACE MOLECULES?
|
Capsule (12 different capsular AGs)
|
|
|
C. perfringens VFs: EXOTOXINS (membrane damaging)? (5)
|
Nercotizing and hemolysing toxins
- alpha toxin (lecithinase, PLC --> *lysis) - beta toxin (necrotizing) - epsilon toxin (increases vascular permeability of GI) - Iota toxin (*ADP-ribosylation of actin --> *necrosis) Enterotoxin (*food poisoning, GI diseases) |
|
|
What is a spp. specific variant of the Lecithinase rxn?
|
Nagler-reaction (target = C. perfringens)
|
|
|
Nagler-reaction?
|
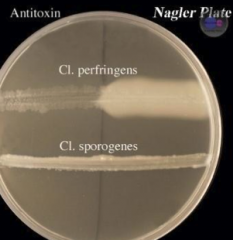
- Egg yolk medium
- Antitoxin blocks lecithinase prod. via C. prefringens - turbidity opalescence due to lecithinase prod. |
|
|
Toxinogenic strains: C. prefringens?
|
Types: A-E
|
|
|
What are the most freq. causative agents of GAS GANGRENE? (2)
|
1. C. perfringens (most freq)
2. C. septicum |
|
|
Pathogenesis: C. perfringens?
|
1. Endogenous infections (rare)
2. Exogenous infections - wound contaminated w/ spore-soil (1 cause) 3. AC, septic abortus (rare) |
|
|
C. perfringens wound infection manifestations? (5)
|
1. Foul discharge
2. Malignant edema 3. Gas-phlegmone 4. Myositis 5. Cellulitis |
|
|
Causes of endogenous C. perfringens infection? (4)
|
1. Colon surgery + carcinoma
2. Gut rupture 3. appendicitis perforata 4. Post-amputation |
|
|
General symptoms: C. perfringens? (7)
|
1. Malaise
2. Hypotonia 3. Fever 4. Vomiting 5. Toxemis 6. Shock 7. Death |
|
|
Necrotizing enterocolitis (NEC), caused by? (4)
|
1. C. perfringens, TYPE C, B-toxin producing
2. Prevention: Type C toxoid immunization 3. *necrotic lesions jejunum, bloody diarrhea, peritonitis 4. via pork meat |
|
|
Incubation period: C. perfringens?
|
1-3 days
|
|
|
What strain of C. perfringens produces enterotoxin that causes FOOD POISONING?
|
TYPE A C. perfringens (via meat)
|
|
|
Type A C. perfringens causes?
|
FOOD Poisoning
- *watery diarrhea, abdominal cramps - 9-15hr incubation - Detect: enterotoxin in stool - Diagnosis: 10^5 colonies/g cultivaiton |
|
|
C. perfringens: DIAGNOSTICS? (7)
|
(usually clinically)
1. Sample - necrotic tissue 2. Microscopically (Gram) 3. Anaerobic cultivation 4. Blood agar (double hemolysis) 5. Nagler rxn 6. Gas chromatography 7. Phage typing |
|
|
C. perfringens: PREVENTION? (4)
|
Wound cleansing:
- efface necrotized material - rinse w/ H202 - hyperbaric 02 treatment - amputation |
|
|
C. perfringens: TREATMENT (antibiotics) (2)
|
High dose AB
1. Penicillin G +/- clindamycin 2. Imipenem or Cephalosporins (III) - SEVERE CASES |
|
|
C. perfringens: TREATMENT (antitoxin)? (3)
|
Polyvalent antiserum (1 to neutralize existing toxins)
1. C. perfringens antitoxins 2. C. septicum antitoxins 3. C. novyi antitoxins |
|
|
C. perfringens rod + spore shape?
|

|
|
|
C. tetani contains what type of spore?
|

Terminal spore
|
|
|
C. tetani characteristics? (6)
|
1. GPR obligate anaerobe spore forming
2. Terminal spore 3. Peritrichous flagella + swarming 4. B-Hemolytic 5. Mild gas production 6. Neurotoxic |
|
|
C. tetani virulence factor?
|
EXOTOXIN = tetanospasmin
|
|
|
Effect of C. tetani exotoxin tetanospasmin?
|
1. Enhances ACh effect --> *tetany
2. Exotoxin --> blocks inhibitory Renshaw interneurons from releasing GABA + glycine (CNS) |
|
|
C. tetani loci? (3)
|
1. Soil + dust
2. Animal feces 3. Gut normaflora (sometimes) |
|
|
C. tetani: port of entry? (5)
|
1.injury
2. burn + deep wounds 3. umbilical wounds 4. abortion 5. surgery, injections, ointments (exogenous infections) |
|
|
Incubation period: C. tetani?
|
4d-several weeks (LONG
|
|
|
Latency of spasms: C. tetani?
|
5-7d
|
|
|
Clinical findings: C. tetani? (7)
|
1. Lockjaw
2. Spasms 3. Hydrophobia 4. Respiratory dysfunciton 5. Opisthotonus (dorsal mm. sustained spasm) 6. Risus (facial mm. spasms) 7. Fully concious |
|
|
Localized type of C.tetani?
|
Neonatal tetanus (entry: umbilical stump)
|
|
|
C. tetani: Diagnosis? (4)
|
1. Clinical symptoms
2. Anaerobic cultivation 3. Direct smear 4. Animal inoculation |
|
|
C. tetani: PREVENTION?
|
DPTa (dipetheria, pertussis, tetanus, acellular)
- combined vaccine containing toxoid - active immunization |
|
|
C. tetani types of treatments? (4)
|
1. Symptomatic
2. Toxoid recall injection 3. Antitoxin 4. Antibiotics |
|
|
C. tetani: Symptomatic therapy? (5)
|
1. Surgical debridement (no hyperbaric 02)
2. Cleansing wounds 3. Muscle relaxants 4. Sedation 5. Assisted ventilation |
|
|
C. tetani: Toxoid recall injection therapy?
|
Toxoid vaccine + antitoxin iv
|
|
|
C. tetani: Antitoxin therapy?
|
Treat for those born before 1941, give before toxin is fixed in nerves
|
|
|
C. tetani: Antibiotic therapy?
|
Penicillin G
|
|
|
How do you treat elderly C. tetanus infected patients?
|
1. Toxoid vaccine (*slow immunity development)
AND 2. Antitoxic serum (to provide fast therapy) (booster shot + antitoxic serum) |
|
|
C. botulinum characteristics? (5)
|
1. GPR obligate anaerobe spore forming
2. Flagella (+) 3. Subterminal or central pore 4. High gas production 5. Loci: everywhere, maybe gut flora |
|
|
C. botulinum: CULTIVATION?
|
Blood agar + anaerobic
|
|
|
C. botulinum virulence factors?
|
EXOTOXINS (A-H; A,B,E, F = human pathogens)
|
|
|
C. Botulinum exotoxin mech?
|
1. Neurotoxin (circ --> nerve endings --> *flaccid paralysis)
2. Heavy chain - binds motor endplate 3. Light chain - endocytosed --> cleaves SNAREs = block ACh vesicular release (no fusion) |
|
|
Toxic dose of C. tetani and C. botulinum?
|
C. tetani = 0.0001 ug (mouse lethal dose)
C. botulinum = 1-2 ug lethal |
|
|
C. botulinum antigens? (2)
|
1. Same O-AGs (somatic)
2. Different H-AGs (flagellar) |
|
|
Pathogenesis: C. botulinum?
|
1. Toxicosis (foodborne botulism)
2. Wound botulism 3. Infant botulism |
|
|
Toxicosis (foodborne botulism)?
|
meats/tin cans --> entry --> 3hrs to 1-2d latency --> gut absorbs toxin --> circulation = toxaemia
|
|
|
Neonatal botulism?
|
Spores in honey --> colonization in GI of infants < 1 year --> weakness, floppy baby, sudden death syndrome
|
|
|
Inhalation of botulism can be used as a?
|
Biological weapon
|
|
|
Clinical symptoms: C. botulinum? (5)
|
1. Double vision (initial symptom, due to brain nerves blocked)
2. Speech+swallow disorders 3. Ptosis (drooping lower eyelid) 4. Respiratory paralysis (-->*death) 5. Cardiac arrest |
|
|
Diagnostics: C. botulinum?
|
Toxin detection w/ animal inoculation:
- food sample - blood - stool |
|
|
C. botulinum: TREATMENT? (3)
|
1. Trivalent antitoxic serum (A, B, E) (-->*toxin neutralization)
2. Ventilation (100d, symptomatic) 3. Infants - pencillin 10-20MU/d |
|
|
C. difficile characteristics? (6)
|
1. GPR obligate anaerobe spore forming
2. Motile 3. Central spore 4. Resistant to many antibiotics 5. Nosocomial pathogen (primarily) 6. gut normaflora |
|
|
What is the most freq agent causing nosocomial diarrhea?
|
C. difficle
|
|
|
What does C. difficle cause? (2)
|
1. Pseudo-membranous colitis
2. Diarrhea |
|
|
C. difficle virulence factors?
|
1. Enterotoxin - toxin A (-->*watery diarrhea)
2. Cytotoxin - toxin B (-->*colon wall destruction) |
|
|
Pathogenesis: C. difficile
|
1. Endogenously - via gut normaflora (due to antibiotics effacing normaflora --> *overgrowth of C. difficle)
2. Exogenously - nosocomial infection --> *diarrhea |
|
|
C. difficile: TREATMENT induced resistance?
|
PROLONGED TREATMENT resistance build up (i think)
1. Clindamycin 2. Cephalosporin 3. Fluoroquinolone |
|
|
C. difficile: THERAPY?
|
1. Vancomycin
2. Metronidazole 3. Bacitracin |
|
|
C. difficile: DIAGNOSIS?
|
1. endoscopy
2. CCFA, blood agar 3. Phage typing 4. Toxin detection (ELISA, latex agglutination,PCR) |
|
|
What clostridum spp. is resistant to ethanol and soap needs to be used instead?
|
C. difficile
|
|
|
Which ribotype produces the binary toxin of C. difficile?
|
027 ribotype (A,B toxin with 027 = most lethal)
|
|
|
Dysbacteriosis?
|
disease caused by an imbalance of the normal flora
(i.e. C. difficile infections) |
|
|
Category A bioterrorisim agents? (4)
|
1. B. anthracis
2. C. botulinum (toxin) 3. Yersinia pestis 4. Francisella tularensis etc.. |
|
|
Category B bioterrorisim agents? (6)
|
1. Brucella spp.
2. Staphylococcus aureus (enterotoxin B) 3. E. coli (O57:H7) 4. V. cholerae 5. Shigella spp. 6. Salmonella spp. |

