![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
What are the gram positive anaerobes we need to know? The gram negatives?
|
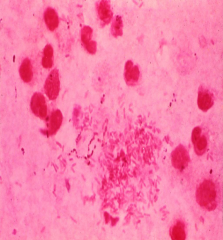
Gram Negative = Bacteroides Fragilis, which is a non spore forming bacilli is a virulent form that often produces beta lactamases. It is aerotolerant through SOD like many pathogenic anerobes.
Gram smear of pus from an abdominal abscess showing polymorphonuclear leukocytes, large numbers of Gram-negative anaerobes, and some peptostreptococci. Gram Positive = Clostridia |
|
|
How does clostridium perfringens present clinically?
|

Cellulitis
gas gangrene (myonecrosis w/ crepitus) Food poisoning -------------------------- Arm of a drug abuser with ulcers and swelling traced to needle tracks. B. Radiographs from the same patient demonstrating gas (clear spaces) in the tissues. |
|
|
What can be seen on radiographs in cases of clostridium perfringens?
|
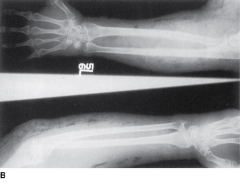
Arm of a drug abuser with ulcers and swelling traced to needle tracks. B. Radiographs from the same patient demonstrating gas (clear spaces) in the tissues. These may causes crepitations on palpation.
|
|
|
How are anaerobes cultured?
|

Selective media
Anaerobic condition - A chemical rxn in a jar consumes all o2 This is a environment w/ low redox potential |
|
|
What are found in gross specimens of pseudomembraneous colitis? What is causative agent?
|
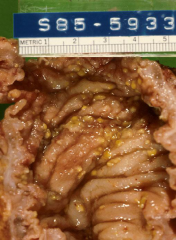
Plaques are seen in both gross and micro histo of pseudomembraneous colitis
More than 95% pseudomembraneous colitis is caused by clostridium difficle |
|
|
Describe the microscopic appearance of pseudomembraneous colititis?
|
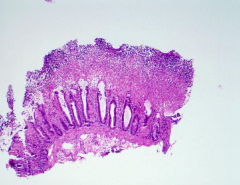
Plaques are present
|
|
|
What are the differences between botulinum and tetanus?
|
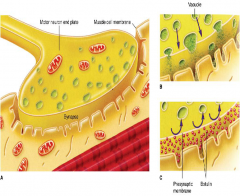
Clostridial tetanus and botulinum neurotoxins.A. The motor neuron endplate, synapse, and neuromuscular junction are shown. For tetanus toxin, the neurons have an inhibitory function; for botulinum, they are active motor neurons. B. Vesicles releasing neurotransmitters across the synapse to the muscle cell membrane are shown. C. In the presence of toxin, the release of neurotransmitter vesicles into the synapse is blocked. For botulinum toxin, the neurotransmitter is acetylcholine, and motor neurons are blocked giving flaccid paralysis. For tetanus toxin, release of neurotransmitters activating inhibitory neurons is blocked resulting in spasmodic contractions
|
|
|
What are the steps leading to gas gangrene?
|
Generally speaking: Traumatic event -> anaerobic environment contamination by displacement from own flora OR enviromental spores -> Feed on dead, poorly vascular tissue requiring surgical debridement
|
|
|
How is bacteroides fragilis different from other gram negative anaerobes?
|
It is the only gram negative anaerobe we are learning. It is the only gram negative WITHOUT endotoxin
It has a polysacchraide capsule that: 1-by itself can form abscesses 2-resists phagocytosis |
|
|
How does bacteroides fragilis differences change the clinical disease and treatment?
|
It needs to be treated with antibiotics that treat gram positive rather than gram negative organisms.
Bacteroides is always resistant to: penicillin (beta lactams), |
|
|
How can we prevent tetanus?
|
A vaccine is available and given as the DTap.
|
|
|
How can we prevent botulinism?
|
Pasteurize possible contaminated foods.
Spores are often found in anerobic food sources. Honey, BOTles of food (swollen cans = gas formation) |
|
|
What are the factors that enable clostridium difficile to produce intestinal disease?
|
Spores are resistant to antibiotics and geminate in the absence of competitive anaerobes
It produces 2 exotoxins 1. Enterotoxin A - causes watery diarrhea 2. Cytotoxin B - cell death and pseudomembrane |
|
|
How do oxygen defense mechanisms found in some anaerobes contribute to virulence?
|
SOD and Catalse protect against free radical oxygen species
Majority anaerobes that cause disease can survive exposure as opposed to non-pathogenic species. |
|
|
When is gas gangrene found clinically?
|
Generally it is found in deeper trauma with soil spore exposure. Deep lacerations allow myonecrosis.
|
|
|
What are the mechanisms for gas gangrene formation?
|
Spores are introduced to deep laceration -> spores germinate in anaerobic environment -> releases 2 toxins -> lead to gangrenous muscles that create black fluid exudate -> Shock may follow
Muscles are a low redox envirmonet w/ CHO that are metabolized to gas |
|
|
What are the 2 toxins formed in gas gangrene?
|
Alpha toxin - a phospholipase that breaks down lechitin causing myonecrosis & hemolysis
Degraditive enzymes - cause subcutaneous bubbles that cause crepitations. (collagenasse, hyaluronidase, lechitinase) |
|
|
What are the differences in factors that contribute to anaerobe vs. aerobe infection?
|
anaerobes want an internal enviroment that has
Anaerobic Dead tissue Compromised vasculature Synergistic faculative anaerobes |
|
|
What is the difference in the clinical setting that aerob and anaerobe infections are found?
|
Anaerobe is generally abcess that is adjacent to mucosal surfacce.
?????????????????/ |
|
|
What is the virulence factor required for clostridium food poisoning?
|
Not all strains produce Enterotoxins. Which cause diarrhea, gastric pain, nausea (absent of fever/vomiting)
|
|
|
What are the epidemiological circumstances of clostridial food poisoning?
|
The steak searing story
Meats, rich sauces that are left non refrigerated. |
|
|
What disease are associated with Bacteroides fragilis?
|
Deep pain and tenderness below the diaphragm (GI/pelvic abscesses)
Peritonitis |
|
|
How do virulence factors of bacteroidees fragilis contribute to disease?
|
Polysacchraide capsule
prevents phagocytosis stimulates abscesses formation Produces beta lactamases |
|
|
How does exotoxin tetanus work?
|
Tetanospasmin: Blocks the release of GABA & glycine from interneurons of Renshaw in spinal cord. This is loss of the inhibitory neurotransmitters.
|
|
|
How does exotoxin botulinium work?
|
Boulinum toxin - this is a neurotoxin that blocks the release of Ach in peripheral nerves
|
|
|
What are the steps that lead to antibiotic-diarrhea & pseudomembraneous colitis that is produced by clostridium difficile?
|
Anitbiotic disrupts normal flora & spore survives -> spores germinate in absence of antibiotics -> grow rapidly -> secrete 2 toxins = pseudomembraneous colitis
|
|
|
How is clostridium difficile primarily diagnosed?
|
Detect the B toxin in species
Often associated clinically post antibiotic administration |
|
|
How does tetanus present clinically?
|

Spastic paralysis, sustained muscle contraction
Tetanus progresses from head to trunk. The masseter is the most sensitive muscle ------------------------------- Tetanus. Opisthotonic posturing caused by involvement of the spinal musculature in a child with generalized tetanus. |
|
|
Summary table from book
|

|
|
|
Summary table from book
|

|
|
|
What does pseudomembrane colitis look like grossly? Microscopically?
|

Clostridium difficile pseudomembranous colitis. A. Colon with discrete plaques of pseudomembrane. B. Histopathology demonstrates the pseudomembrane above the mucosa. It is "pseudo" because it is composed of only fibrin and inflammatory cells.
|
|
|
What medical intervention can stop the course of gas gangrene production?
|
surgical debridement
Penicillin or clindamycin (minor infections) Hyperbaric oxygen |
|
|
What is unique about clostridium perfringes compared to all the other clostridium species?
|
It is the only non-motile member of this gram (+) obligate anaerobic group
C. tetani, C. botulinum, & c. difficle are all motile members of this group. |
|
|
Why were MASH units developed in Korean war? What are other situations where this disease arises?
|
MASH units provided quick treatment that helped to decrease the shock and death that would occur in <12H from gas gangrene
Gas Gangrene requires trauma + delay This disease also arises in natural disasters & wilderness accidents |
|
|
What is the progression of clostridium perfringesn causing food poisoning?
|
spores in meat/poultry/rich sauces -> survive initial cooking -> delay w/o refirgeration occurs -> germination and multiply -> release heat labile enterrotoxin -> in ileum enterrotoxin inhibits glu transport & damages epithelium -> diarrhea about 12H later
|
|
|
How is clostridium perfringes diagnosed?
|
Presence of gram (+) rod, strict anaerobe, that is non motile
|
|
|
How can botulinum toxin present clinically?
|
Adults
cranial nerve palsy symmetric descending paralysis (NMJ) dizziness, dry throat, ptosis (post gang parasympathetic) Infant floppy baby -baby ingests as GI flora developing. Slow release and generally not fatal |
|
|
Will botulinum have a fever?
|
No, because the bacteria do not invade to become bacteremic. Only Toxin does. Same for tetanus.
|
|
|
Where is tetanus found? How do we treat it?
|
Spores are often found in "rusty nails"
Prophylaxis is best Antitoxin is available to neutralize Diazepam (GABA agonist) clean wound Penicillin or metranidazole |
|
|
Why do aminoglycosides not work on anaerobes?
|
It requires a transporter that is found in aerobic ETC. Thus the rx never enters the bacteria
|
|
|
What type of redox enviroment do anaerobes prefer?
|
Grow in low redox potential and low oxygen enviroments
Many human species are aerotolerant with SOD & catalse |
|
|
How is clostridium difficle treated?
|
PO vancomycin which does NOT cross the GI barrier due to large MW.
Colectomy may be in order, consider this is the leading cause of fatal diarrhea in US & it may reoccur MANY times. Fecal transplant may prove helpful |
|
|
How can hospital workers prevent the transmission of C diffe?
|
Washing hands, only good way to prevent sine spores are resistant to EtOH
|
|
|
Mnemonic for obligate anaerobe?
|
anaerobes Can't Breathe Air
A-actinomyces B-bacteroides C-clostridia |
|
|
Why is bacteroides fragilis important to our flora?
|
makes vitamin K for the host.
Very common among normal GI flora |
|
|
How does Bacteroides fragilis get seeded in a host to cause pathology?
What type of pathology does it create? |
Ruptured intestine mucosa -> spills into peritoneum w/ faculative anerobes that use up all the O2 -> (B. Fragilis survives w/ presence of SOD & oxidase) ->Now organism thrives -> may spread from abcess but does NOT cause DIC (it is gram - BUT lacks endotoxin) but rather shock
|
|
|
How would you treat a bacteroides fragilis abcess?
|
need to drain & repair lesion then antibiotics
|

