![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
754 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are the 4 types of diarrhea?
|
secretory
osmotic exudative altered intestinal transit time |
|
|
|
What is the duration for acute and chronic diarrhea?
|
acute <2 weeks
chronic >2 weeks |
|
|
|
Define diarrhea.
|
increased number of bowel movements (>3 per day) or liquidity of feces
|
|
|
|
What may rust-colored sputum indicate?
|
pneumococcal pneumonia
|
|
|
|
What is the ddx for orchitis?
|
*orchitis is uncommon
complication of mumps complication of prostatic infection |
Mosbys p662
|
|
|
What is the etiology of acute diarrhea?
|
NON-INFLAMMATORY:
viruses → norovirus, rotavirus (schools, nursing homes, cruiseships) protozoa → giardia lamblia, cryptosporidium, cyclospora non-invasive bacteria: -preformed enterotoxin → s. aureus, b. cereus, c. perfringens -enterotoxin production → v. cholerae, ETEC INFLAMMATORY: viral → CMV protozoa → entamoeba histolytica invasive bacteria → shigella, campylobacter jejuni, salmonella, EIEC, yersinia, listeria, gonorrhea, chlamydia toxin-producing bacteria → CDIF (recent antibiotics), vibrio parahaemolyticus can also be caused by drugs |
|
|
|
What is the clinical presentation of acute diarrhea?
|
<2 weeks in duration
NON-INFLAMMATORY: diarrhea typically mild, large volume stool → watery, non-bloody nausea and vomiting periumbilical cramps and bloating INFLAMMATORY: fever diarrhea typically small volume (<1L/day) stool → bloody, pus LLQ cramps, urgency, tenesmus |
|
|
|
What is the diagnostic workup of acute diarrhea?
|
NON-INFLAMMATORY:
none unless severe or persists >7 days negative fecal leukocytes INFLAMMATORY: positive fecal leukocytes or lactoferrin stool culture O&P E coli 0157:H7 CDIF if risk factors |
|
|
|
What is the clinical presentation of epididymitis?
|
ACUTE:
fever scrotal pain → may radiate along spermatic cord or to flank epididymis enlarged and extremely tender, distinguishable from testis early in course scrotum erythematous and enlarged if associated urethritis → pain at tip of penis, urethral discharge if associated cystitis → irritative voiding symptoms if associated prostatits → possible tenderness positive prehn sign → elevation of scrotum above pubic symphysis provides relief (not reliable sign) |
Mosbys p663
Current ch23 |
|
|
What is testicular torsion?
|
disorder characterized by twisting of the spermatic cord, reducing blood supply to scrotum
|
|
|
|
What is the management, referral, and patient education for acute diarrhea?
|
NON-INFLAMMATORY:
1. self-limited within 5 days 2. rehydration therapy → 1 liter water, 1 tbsp sugar, 1 tsp salt 3. antidiarrheals → loperamide 4. peptol-bismol → traveler's diarrhea, viral enteritis 5. if persists >7 days → order fecal leukocytes or lactoferrin, stool culture, O&P INFLAMMATORY: 1. do not treat with antidiarrheals 2. antibiotic treatment depends on underlying cause -if empiric → consider if bloody stool, severe fever, tenesmus, fecal lactoferrin (but not due to E coli) -if specific → shigellosis, cholera, extraintestinal salmonellosis, traveler's diarrhea, C difficile infection, giardiasis, and amebiasis HOSPITALIZATION: severe dehydration severe or worsening bloody diarrhea severe or wrosening diarrhea in >70y/o or immunocompromised severe abdominal pain severe infection (high fever, rash, leukocytosis) or sepsis |
|
|
|
What are the physical exam findings of testicular torsion?
|
acute onset
nausea and vomiting scrotal erythema, swelling, and extreme tenderness absence of cremasteric flex on affected side lack of voiding symptoms (compared to epididymitis) |
Mosbys p663
|
|
|
What is bronchiectasis?
|
permanent abnormal dilation and destruction of bronchial walls
|
|
|
|
What patient population is most commonly affected by testicular torsion?
|
adolescents
10-20y/o |
Mosbys p663
|
|
|
What are the complications and prognosis of acute diarrhea?
|
severe dehydration → hypokalemia, metabolic acidosis
toxic colitis sepsis |
|
|
|
When palpating the testis, what should they feel like?
|
smooth
rubbery free of nodules sensitive but non-tender |
Mosbys p650
|
|
|
Define cryptorchordism.
|
undescended testicle(s)
|
|
|
|
If a scrotal mass is identified, how can you determine if it is cystic or solid?
|
perform transillumination
if light shines through → cystic if light doesn't shine through → solid |
|
|
|
What is the non-pharmacologic management of diarrhea?
|
1. adequate oral fluids with carbs and lytes (oral rehydration solution → 1L water, 1 tbsp sugar, 1 tsp salt)
2. drink tea or flat carbonated beverages 3. eat soft easily digested foods (bananas, applesauce, soup, crackers, toast, rice) 3. avoid fiber, fats, milk products, caffeine, alcohol |
|
|
|
Define orchitis.
|
inflammation of the testicle
|
|
|
|
Define epididymitis.
|
inflammation of the epididymis
|
|
|
|
What may currant jelly sputum indicate?
|
klebsiella pneumonia
|
|
|
|
Define varicocele.
|
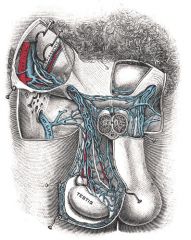
condition where the veins of the pampiniform plexus in the spermatic cord are abnormally dilated and tortuous
|
Mosbys p662
|
|
|
What is the clinical presentation of a varicocele?
|
commonly on LT side
often only visible while standing → usually dimish in size or disappear when supine "bag of worms" appearance may be painful |
Mosbys p662
|
|
|
What is the ddx of epidiymitis?
|
UTI
STI TB (if chronic epididymitis) |
Mosbys p663
|
|
|
What are the complications of a varicocele?
|
reduced fertility
|
Mosbys p662
|
|
|
What disorders of the spermatic cord, scrotum, and testes are emergencies?
|
orchitis
testicular torsion |
|
|

|
LT varicocele
|
|
|
|
What is the etiology of epididymitis?
|
if acute → usually infectious
may also follow heavy lifting or trauma STI: <40 y/o associated urethritis gonorrhea or chlamydia Non-STI: older men associated UTI or prostatitis gram-negative rods Route → via urethra to ejaculatory duct, then down vas deferens to epididymis |
|
|
|
What are the clinical features of typical vs atypical pneumonia?
|
TYPICAL:
acute onset prostration high fever cough with sputum lobar consolidation ATYPICAL: insidious onset little to no fever cough without sputum hazy diffuse infiltrates (no signs of consolidation) |
|
|
|
What is the diagnostic workup of epididymitis?
|
CBC → leukocytosis, shift to the left
if STI: URNC GCCHDNA → positive if non-STI: UA → puria, bacteriuria, +/- hematuria URNC → positive |
|
|
|
What is the management of epidiymitis?
|
1. best rest with scrotal elevation
2. if STI → antibiotics x 10-21 days; treat partner 3. if non-STI → antibiotics x 21-28 days |
|
|
|
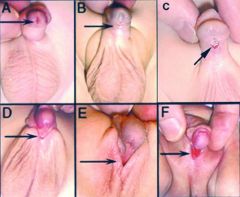
Define hypospadias.
|
congenital abnormality where urethral meatus is located on ventral surface of glans penis, shaft of penis, or base of penis
|
|
|
|
What is the prognosis for epididmyitis?
|
if prompt treatment → outcome favorable
if delayed treatment → possible orchitis, abscess formation, or decreased fertility |
|
|
|
What is the most common cause of bronchiectasis?
|
CF
|
|
|
|
What is the etiology of orchitis?
|
associated with mumps (viral)
associated with epididymitis (bacterial) |
|
|
|
hypospadias
|
|
|
|
What is the clinical presentation of orchitis?
|
mild or severe scrotal pain
MUMPS: fatigue, fever, HA, myalgias occurs 4-7 days following parotitis testicular pain and swelling (sparing epididymis) scrotal skin may be erythematous or edematous 70% unilateral EPIDIDYMITIS enlarged, tender epididymis boggy, tender prostate |
|
|
|
Which is more common, indirect or direct hernia?
|
indirect
|
Mosbys p650
|
|
|
What is the diagnostic workup of orchitis?
|
Doppler U.S. to differentiate between mumps orchitis and testicular torsion
|
|
|
|
List organisms that cause typical vs atypical pneumonia.
|
TYPICAL:
streptococcus pneumoniae staphyloccocus aureus haemophilus influenzae klebsiella pneumoniae ATYPICAL: mycoplasma pneumoniae chlamydia pneumoniae legionella species influenza viruses |
|
|
|
What is the management of orchitis?
|
MUMPS ORCHITIS:
1. symptomatic treatment only 2. analgesics 3. hot or cold packs 4. scrotal elevation EPIDIDYMO-ORCHITIS: 1. treat same as epididymitis |
|
|
|
Recurrent bleeding in children at multiple sites may indicate?
|
heritable hemostasis disorder
|
Current p481
|
|
|
What are examples of hemoglobinopathies?
|
sickle cell anemia
hemoglobin S-C disese sickle cell trait hemoglobin C, D, E, H, I or combination |
|
|
|
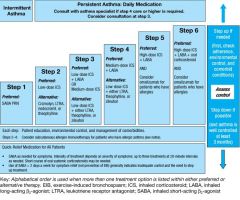
What 3 criteria are assessed to determine asthma severity?
|
FEV1/FVC ratio
asthma symptoms medication use |
Interpreting Laboratory Data p194
|
|
|
Where does a direct hernia occur?
|
through external inguinal ring
|
|
|
|
Where does an indirect hernia occur?
|
internal inguinal ring
|
|
|
|
What are examples of coagulopathies?
|
hemophilia A
hemophilia B Von Willebrand disease vitamin K deficiency liver disease Dengue Fever leukemia DIC |
|
|
|
Where does a femoral hernia occur?
|
fossa ovalis where femoral artery exits abdomen
|
Mosbys p656
|
|
|
Are femoral hernias more common in males or females?
|
females
|
Mosbys p656
|
|
|
Define exanthem?
|
generalized skin rash; caused by infectious disease, autoimmune disease, or drugs/toxins
|
|
|
|
Which type of inguinal hernia may descend into the scrotum, direct or indirect?
|
indirect
|
|
|
|
What is the etiology of asthma?
|
genetic predisposition
risk factors include obesity and atopy (dust mites, dander, pollen) other precipitating factors include cold weather, exercise, URTI, GERD, stress affects 5% of population more common in male children and female adults |
|
|
|
Define epispadias.
|
congenital abnormality where urethral meatus is located along dorsal shaft of penis
|
|
|

|
oral candadiasis
|
|
|
|
Hypospadias increases the risk of what disorder?
|
cryptochordism
|
Mosbys p657
|
|
|
What is the clinical presentation of asthma?
|
chronic or recurrent symptoms of airflow obstruction
airflow obstruction reversible → either sponatneously or with bronchodilator therapy dyspnea cough chest tightness prolonged expiration episodic wheezing symptoms often worse at night if allergic asthma → enalarged nasal mucosa, nasal secretions, nasal polyps, eczema, atopic dermatitis |
|
|
|
Discuss community acquired pneumonia vs hospital acquired pneumonia.
|
CAP:
occurs outside hospital or within 48 hours of admission in patient who is ambulatory and did not reside in long-term care facility HAP: occurs in hopsital after 48 hours of admission excludes infections at time of admission common in patients requiring mechanical ventilation |
|
|
|
What is the clinical presentation of a platelet disorder?
|
bleeding localized to skin and mucous membranes → petechiae, purpura, ecchymosis, epistaxis, gingival bleeding
small superficial nonpalpable ecchymosis bleeding after minor wounds immediate post-surgical bleeding |
hemostasis lecture
|
|
|
What is the treatment of CAP?
|
If not being admitted:
oral clarithromycin, azithromycin, or doxycycline x 5 days to 2 weeks and until patient afebrile x 2-3 days If admitting: order BC IV extended spectrum B-lactam (ceftriaxone or cefotaxime) + macrolide (clarythromycin or azithromycin) |
|
|

|
epispadias
|
|
|
|
List signs of upper airway obstruction.
|
nasal flaring
retraction at suprasternal notch inspiratory stridor hoarse cough or cry If severe: cyanosis retractions also involving intercostal and subcostal spaces barking cough inspiratory and expiratory stridor |
Current p377
|
|
|
What is the diagnostic workup of asthma?
|
PFTs → measure before and after use of bronchodilator
*significant reversibility of airflow obstruction = ≥12% and 200mL in FEV1 and ≥15% and 200mL in FVC after inhaling SABA bronchoprovacation challenge → if PFTs non-diagnostic exercise challenge → if exercise-induced asthma suspected allergy testing GERD workup |
|
|
|
te
|
mild stridor
|
|
|
|
Define enuresis.
|
bedwetting
|
|
|
|
Blank
|
severe stridor
|
|
|
|
What is the prevention of asthma attacks?
|
1. develop asthma action plan
2. identify aggravating factors and reduce exposure 3. stop smoking |
|
|
|
What is the ddx for stridor?
|
airway obstruction →
foreign body aspiration narrowing due to trauma, allergic reaction, infection or neoplasm inhalation of caustic agent |
|
|
|
What symptoms/signs characterize coagulation disorders?
|
bleeding localized to joints and muscles
no petechiae large palpable ecchymosis bleeding after minor wounds rare delayed post-surgical bleeding |
hemostasis lecture
|
|
|
What is an Asthma Action Plan?
|
plan develped between provider and patient to control asthma
-what medications to take daily -how to handle asthma long-term → what to avoid -how to handle asthma attacks → what additional medications to take, when to call provider or go to ER |
http://tiny.cc/AsthmaActionPlan
|
|
|
Does wheezing on forced expiration indicate airflow obstruction?
|
no, wheezing during normal breathing or prolonged expiration indicates obstruction
|
|
|
|
Does PT measure intrinsic or extrinsic coagulation pathway?
|
extrinsic
|
hemostasis lecture
|
|
|
A reduced FEV1/FVC ratio indicates?
|
airflow obstruction
|
|
|
|
Define enathem?
|
mucosal membrane rash; often accompanying an exanthem
|
|
|
|
Describe the stepwise management of asthma.
|
|
|
|
|
Describe the recommendations for the influenza vaccine.
|
1. includes H1N1
2. get if >6 m/o 3. get yearly during flu season 4. get especially if high risk for developing flu complications or spreading flu: -children <5y/o -pregant women -adults >50y/o -nursing home residents -chronic medical conditions -household contacts of at-risk persons -caregivers -healthcare workers |
CDC
|
|
|
Describe the classifications of asthma severity.
|

|
|
|
|
Describe the recommendations for the haemophilus influenzae type (hib) vaccine.
|
prevents epiglottitis, pneumonia, meningitis,etc.
get 4-dose series at 2, 4, 6, and 12 months |
CDC
|
|
|
Does PTT measure intrinsic or extrinsic coagulation pathway?
|
intrinsic
|
hemostasis lecture
|
|
|
Prolonged PTT indicates a possible deficiency in what factors?
|
XII, XI, IX, VIII, von willebrand, X, V, II, I
|
hemostasis lecture
|
|
|
What is the common name for oral candadiasis?
|
thrush
|
|
|
|
Prolonged PT indicates a possible deficiency in what factors?
|
VII, X, V, II, I
|
hemostasis lecture
|
|
|
What is frontal bossing?
|
unusually prominent forehead
|
|
|
|
What is the most common cause of elevated PTT?
|
von Willebrand disease
|
hemostasis lecture
|
|

|
frontal bossing
|
|
|
|
What is the etiology of viral gastroenteritis?
|
causes include rotavirus, norwalk virus, enteric adenoviruses, astrovirus, coronaviris; spread via ingestion of contaminated water or food; common among children, elderly, immunosuppressed
|
|
|
|
Bleeding time is a measure of?
|
platelet function
|
|
|

|
oral candidiasis
|
|
|
|
What is the diagnostic work-up of hemophila B?
|
PT → normal
PTT → prolonged bleeding time → normal factor IX → deficiency |
|
|
|
What is the common name for viral gastroenteritis?
|
stomach flu
|
|
|
|
What is the clinical presentation of viral gastroenteritis?
|
onset within 4-48hr of ingestion; nausea, vomiting, abdominal cramps, large-volume watery diarrhea
|
|
|

|
mumps
|
|
|
|
What is the most common hereditary bleeding disorder?
|
von Willebrand disease
|
|
|
|
What is the diagnostic work-up of viral gastroenteritis?
|
usually not indicated
rotavirus if severe illness in child |
|
|
|
What are the steps of the extrinsic pathway?
|
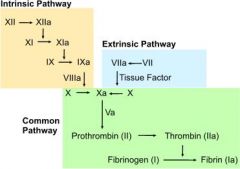
1. tissue injury → release of tissue factor (factor III)
2. tissue factor activates factor VII 3. factor VIIa activates factor X |
|
|
|
What is the etiology of nongonococcal (septic) arthrits)?
|
Staph aureus (50%)
MRSA group B strep gram-negatives (10%) → E. coli and pseudomonas aeruginosa associated with: loss of skin integrity → psoriasis, ulcers infection → endocarditis damaged or prosthetic joints → RA immunocompromise → DM, alcoholism, cirrhosis, kidney disease, immunosuppressant therapy) IV drug use |
Current p777
|
|

|
mumps
|
|
|
|
What are the steps of the intrinsic pathway?
|
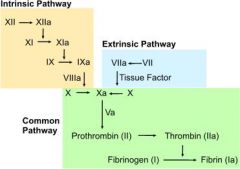
1. exposed collagen following tissue injury activates factor XII
2. factor XIIa activates factor XI 3. factor XIa activates factor IX 4. factor IXa + factor VIIIa activate factor X |
|
|
|
What is the clinical presentation of septic arthritis?
|
inflammatory monoarticular arthritis
commonly affects knee, hip, wrist, shoulder, or ankle acute pain, swelling, warmth worsens over hours joint effusion |
Current p777
|
|
|
What is the most common cause of severe diarrhea in children?
|
rotovirus
|
|
|
|
What are the steps of the common coagulation pathway?
|
1. Xa + Va catalyzes prothrombin (factor II) → thrombin
2. thrombin catalyzes fibrinogen (factor I) → fibrin 3. fibrin → clot |
|
|
|
What is the management of septic arthritis?
|
1. hospitalization
2. broad-spectrum antibiotics until culture results (vancomycin if suspected MRSA) 3. narrow-spectrum antibiotics x 6 weeks 4. early orthopedic consult for joint drainage |
Current p777
|
|
|
What is the management of viral gastroenteritis?
|
1. self-limiting
2. rehydration via oral solution or IV fluids |
|
|
|
What is the prevention of rotavirus?
|
vaccination
|
|
|
|
What are the complications of viral gastroenteritis?
|
dehydration → death, especially in young children
|
|
|
|
What is the common name for pertussis?
|
whooping cough
|
Current p1308
|
|
|
What is the etiology of pertussis?
|
caused by bordetella pertussis; spread via respiratory droplets; 50% before 2y/o
|
Current p1308
|
|
|
What is the prevention of pertussis?
|
TDAP vaccination
|
Current p1308
|
|
|
What is the management of pertussis?
|
1. erythromycin 500mg PO 4x daily x 7 days
2. offer erythromycin to contacts if exposed within 3 weeks of onset |
Current p1308
|
|
|
What is the clinical presentation of pertussis?
|
1. catarrhal stage → fatigue, lacrimation, sneezing, rhinorrhea, hacking night cough, anorexia
2. paroxysmal stage → whooping cough 3. convalescent stage → decrease in severity of whooping cough, 4 weeks after onset entire illness lasts 6 weeks |
Current p1308
|
|
|
What is the diagnostic work-up of pertussis?
|
collect nasopharyngeal dacron swab
pertussis PCR or pertussis culture with bordet-gengou agar |
Current p1308
|
|
|
What is the evaluation of a bleeding disorder?
|
1. onset
childhood → heritable disorder adult → mild heritable disorder or acquired 2. location mucocutenous → platelet disorder joints and muscles → clotting factor disorder 3. clinical context → pregnancy, underlying medical conditions, sepsis, medications, postsurgery 4. personal history → prior spotaneous bleeding, excessive bleeding with trauma, dental, menses, surgery 5. family history |
Current p481
|
|
|
Erythematous or cobblestoned conjunctiva may indicate?
|

allergic conjunctivitis
infectious conjunctivitis |
Mosbys p290
|
|

|
allergic conjunctivitis
|
|
|
|
What is pink eye?
|
conjunctivitis
|
|
|
|
If an eye moves rapidly to the right and then slowly drifts to the left, is this right or left nystagmus?
|
right nystagmus
|
Mosbys p293
|
|
|
How do you perform the cover-uncover test?
|
if asymmetric corneal light reflex:
1. ask patient to stare at a fixed object 2. ask patient to cover one eye 3. inspect uncovered eye for movement 4. ask patient to uncover eye and inspect for movement 5. repeat on other side *if non-paralytic strabismus → bad eye will move when good eye covered *if paralytic strabismus → bad will NOT move when good eye covered |
Mosbys p293
|
|
|
What is the management of amblyopia?
|
patch normal eye to force lazy eye to center
|
|
|

|
bacterial conjunctivitis
|
|
|
|
When would you perform the cover-uncover test?
|
if asymmetric corneal light reflex present
|
|
|
|
Define amblyopia.
|
lazy eye
|
|
|
|
What is the etiology of strabismus?
|
1. paralytic → impaired nerve or weakened EOM
2. non-paralytic → intraocular pathology → infantile cataract, retinoblastoma |
Mosbys p307
|
|
|
What is parotitis?
|
inflammation of the parotid gland(s)
|
|
|
|
What is the most common viral cause of parotitis?
|
mumps virus
|
|
|
|
How do you differentiate oral candidiasis from oral leukoplakia?
|
candidiasis will wipe off (and bleed when scraped) while leukoplakia will not
|
|
|
|
Hereditary anemias are more common in what ethnicities?
|
African Americans
Mediterranean Middle Eastern Indian Southeast Asian |
Interpreting Laboratory Data p9
|
|

|
pharyngitis
|
|
|
|
List examples of hereditary anemias.
|
sickle cell anemia
glucose-6-phosphate dehydrogenase (G6PD) deficiency thalassemias |
Interpreting Laboratory Data p9
|
|

|
palatal petichiae → GABHS pharyngitis
|
|
|
|
What is oral candidiasis?
|
yeast infection of the mouth
|
|
|
|
What is the etiology of oral candidiasis?
|
caused by yeast Candida albicans; commonly associated with dentures, dibilitation, anemia, DM, HIV, broad-spectrum antibiotics, corticosteroids, chemotherapy, radiation therapy
|
|
|
|
What is the clinical presentation of oral candidiasis?
|

white curd-like patches overlying erythematous mucosa; painful; removable
*angular cheilitis is another manifestation of candidiasis |
|
|
|
What is the diagnostic workup of oral candidiasis?
|

1. KOH → reveals pseudohyphae
2. HIV if no other explainable cause |
|
|
|
What is the management of oral candidiasis?
|
1. prescribe antifungal, either fluconazole 100mg/d x 7-14 days, ketoconazole 200-400mg/d x 7-14 days (take with breakfast), clotrimazole troches, nystatin vaginal troches, or mouth rinses
2. for local relief, half-strength hydrogen peroxide mouth rinses or 0.12% chlorhexidine 3. if dentures, prescribe nystatin powder applied to dentures 3-4x daily x several weeks 4. if HIV, prescribe longer course of antifungal 3. if refractory, prescribe itraconazole 200mg PO daily |
|
|
|
What is herpangina?
|
viral infection of the mouth
|
|
|
|
What is the etiology of herpangina?
|
caused by coxsackieviruses; spread via respiratory droplets or fecal-oral; usually affects infants and young children in summer
|
|
|
|
What is the management and patient eduction for herpangina?
|
1. self-limiting → usually resoves in 1 week
2. take acetominophen or ibuprofen for fever and discomfort (avoid aspirin) 3. increase fluids 4. eat cold non-irritating diet → milk, icecream, popsicles 5. avoid citrus, fried, spicy, and hot food |
|
|
|
What is the prevention for herpangina?
|
handwashing
|
|
|

|
herpangina
|
|
|
|
What is hand, foot, and mouth disease?
|
viral infection of the hands, feet, and mouth
|
|
|
|
What is the etiology of hand, foot, and mouth disease?
|
caused by coxsackievirus; transmitted via rhinorrhea, saliva, sputum, stool, blister fluid; commonly occurs in young children during summer and early fall
|
|
|
|
What is the clinical presentation of hand, foot, and mouth disease?
|

fatigue; fever; sore throat; non-pruritic blistering rash on hands, feet, and buttocks; ulcers in mouth
|
|
|
|
What is the management and patient education of hand, foot, and mouth disease?
|
1. self-limiting → resolves in 7-10 days
2. take acetominophen or ibuprofen for fever and pain 3. rinse with salt water → 1/2 tsp salt, 1 glass of warm water 4. increase fluids to prevent dehydration |
|
|
|
What is the prevention of hand, foot, and mouth disease?
|
avoid contact with infected people; handwashing; cleaning objects
|
|
|
|
List 4 types of pharyngitis/tonsillits.
|
1. viral pharyngitis
2. group A beta-hemolytic streptococcal pharyngitis (GABHS) 3. mononucleosis 4. diphtheria |
|
|
|
What is the etiology of GABHS pharyngitis?
|
group A beta-hemolytic streptococcus
|
|
|
|
What is the presentation of GABHS pharyngitis?
|
Centor Criteria:
sore throat + 1. fever >100.4°F 2. pharyngotonsillar exudates 3. anterior cervical lymphadenopathy 4. no cough *if 1 criteria present → unlikely *if 2 criteria present → possible *if 3 criteria present → likely *if 4 criteria present → treat regardless of rapid strep odynophagia, scarlatiniform rash; no rhinorrhea or hoarseness |
|
|
|
What is the diagnostic work-up of GABHS pharyngitis?
|
rapid strep; throat culture if negative
|
|
|
|
Where does hematopoiesis occur in adults?
|
red bone marrow of skull, ribs, vertebrae, pelvis, humerus, and femur
|
Pathology p72
|
|
|
What is the etiology of mononucleosis?
|
epstein barr virus (EBV); transmitted via saliva or genital secretions; common in young adults
|
Current p204
|
|
|
Where does hematopoiesis occur in children?
|
bone marrow of long bones (femur, tibia)
|
|
|
|
What is the presentation of mononucleosis?
|
fatigue, fever, sore throat, myalgia; cervical lymphadenopathy; hepatosplenomegaly; possible palatal petichiae, tonsillar exudates, or maculopapular rash
*1/3 of mono also presents with GABHS |
Current p204
|
|
|
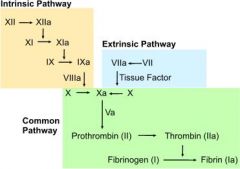
What is the diagnostic work-up of mononucleosis?
|
CBCDP → lymphocytosis (>35%)
blood smear → atypical large lymphocytes monospot EBV titers if monospot negative |
Current p204
|
|
|
What is the presentation of viral pharyngitis?
|
sore throat, rhinorrhea, no pharyngotonsillar exudate
|
Current p204
|
|
|
What is the treatment for GABHS pharyngitis?
|
1. prescribe antibiotics to prevent sequelae
|
|
|
|
What is the diagnostic work-up of viral pharyngitis?
|
rapid strep to R/O GABHS
|
|
|
|
What is the management of viral pharyngitis?
|
1. self-limiting → resolves within 7-10 days
2. acetominophen for fever 3. salt water gargle → 1tsp salt, 1 cup water several times per day 4. NO ANTIBIOTICS!!! |
|
|
|
What are the complications of viral pharyngitis?
|
complications rare
|
|
|
|
How long before a person infected with mononucleosis would test positive with a monospot?
|
4 weeks after onset
|
Current p1243
|
|
|
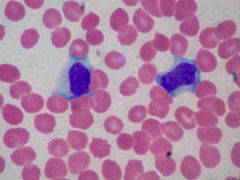
Interpret the results of an EBV titer for mononucleosis.
|
1. if VCA-IgM positive → current infection
2. if VCA-IgG positive → recent or past infection 3. if VCA-IgM negative but others positive → past infection 4. if VCA-IgG negative → susceptible to infection |
|
|
|
What is the management of mononucleosis?
|
1. acetominophen or ibuprofen for pain and fever
2. warm salt water gargle 3-4x daily for sore throat 3. increase fluids 4. rest 5. avoid contact sports >4 weeks 6. if GABHS → penicillin or erythromycin 7. if impending airway obstruction, hemolytic anemia, or severe thrombocytopenia → corticosteroids |
|
|
|
What is the prognosis of mononucleosis?
|
if non-complicated → fever disappears within 10 days, lymphadenopathy and splenomegaly within 4 weeks; fatigue may persist 2-3 months
|
|
|
|
What is the prevention of mononucleosis?
|
avoid sharing utensils or kissing person infected with mono
|
|
|
|
Are closed comedones, white heads or black heads?
|
white heads
|
Fitzpatrick p3
|
|
|
Are open comedones, white heads or black heads?
|
black heads
|
Fitzpatrick p3
|
|
|
What drugs can induce acne vulgaris?
|
androgens
glucocorticoids oral contraceptives lithium iodides bromides hydantoin isoniazid danazol |
Fitzpatrick p2
|
|
|
What topical antibiotics are used to treat mild acne?
|
clindamycin
erythromycin |
Fitzpatrick p6
|
|
|
What factors can exacerbate acne vulgaris?
|
occlusion/pressure on skin (leaning face in hands)
menstruation cosmetics (including mineral oils, pomade) drugs stress |
Fitzpatrick p2
|
|
|
What oral antibiotics are used to treat moderate acne?
|
minocycline 50-100mg twice daily
doxycycline 50-100mg twice daily |
Fitzpatrick p6
|
|
|
Acne vulgaris can be CAUSED by eating certain foods, true or false?
|
false
|
Fitzpatrick p2
|
|
|
What is a sebaceous gland?
|
small oil-producing gland in skin
usually attached to hair follicle in dermis secretes sebum into follicular duct and thence to surface of skin |
Stedman's
http://tiny.cc/sebaceous |
|
|
Where are sebaceous glands located?
|
entire body except palms of the hands and soles of the feet
|
http://tiny.cc/sebaceous
|
|
|
Where are sebaceous glands most abundant?
|
scalp
face |
http://tiny.cc/sebaceous
|
|
|
What does sebum consist of?
|
fats (cholesterol, triglycerides, wax esters, squalene)
cellular debris |
http://tiny.cc/sebaceous
|
|
|
What is the normal range for PT?
|
10-13 sec
|
Interpreting Laboratory Data p367
|
|
|
In managment of acne, does pyschological impact need to be addressed?
|
yes
assess psychological impact of acne in each patient and modify treatment accordingly |
Fitzpatrick p6
|
|
|
What is the ddx for prolonged PT?
|
factor VII, X, V, II, I deficiencies
vitamin K deficiency liver disease DIC warfarin |
Interpreting Laboratory Data p367
|
|
|
What are the goals for management of acne?
|
reduce ketatin plugging
reduce sebum production treat bacterial colonization |
Fitzpatrick p6
|
|
|
What is the ddx for prolonged PTT?
|
factor XII, XI, IX, VIII, X, V, II, I deficiencies
vitamin K deficiency lupus anticoagulant liver disease DIC heparin warfarin |
|
|
|
What is the managment for mild acne?
|
benzoyl peroxide gels (2%, 5%, or 10%)
topical retinoids (tretinoin or adapalene) TOPICAL antibiotics (clindamycin or erythromycin) taper as lesions lessen Fitzpatrick p.6 |
|
|
|
What is the patient education for acne?
|
not caused by dirt (wash face twice daily w/ mild cleanser and lukewarm water, excessive washing can exacerbate acne)
not caused by diet (though certain foods may exacerbate acne) use oil-free cosmetics (wash off nightly w/ mild cleanser and lukewarm water) use shampoo daily (if hair oily) picking/popping lesions can result in scarring tx prevents breakouts, it does not heal existing lesions tx must be continuous to be effective improvement may take 2-5 months (longer if non-inflamed comedones) |
Fitzpatrick p6
http://tiny.cc/acne598 |
|
|
In management of acne, combination therapy is best, true or false?
|
true
Fitzpatrick p.6 |
|
|
|
What is the management for moderate acne?
|
benzoyl peroxide gels (2%, 5%, or 10%)
topical retinoids (tretinoin or adapalene) ORAL antibiotics (minocycline or doxycycline) taper as lesions lessen Fitzpatrick p.6 |
|
|
|
What are the indications for isotretinoin?
|
moderate/severe acne -> nodular/cystic acne
acne conglobata acne refractory to tx Fitzpatrick p.6-7 |
|
|
|
What is the management for severe acne?
|
benzoyl peroxide gels (2%, 5%, or 10%)
topical retinoids (tretinoin or adapalene) ISOTRETINOIN Fitzpatrick p.6 |
|
|
|
What are the requirements for isotretinoin use?
|
monitor cholesterol, triglycerides, ALT, AST levels (isotretinoin may cause these to rise and increase cardiovascular risk or cause hepatotoxicity)
females must take oral contraceptives (isotretinoin is teratogenic) Fitzpatrick p.6-7 |
|
|
|
What should be avoided during isotretinoin use?
|
vitamin A supplements
tetracycline antibiotics |
|
|
|
What are the side effects of isotretinoin use?
|
commonly dry lips and cheilitis
night blindness (warn about driving at night) decreased tolerance to contact lenses during and after therapy (ask about contacts) eczema-like rash (tx w/ low potency topical glucocorticoids) hair thinning paronychia dryness of nasal mucosa nosebleeds headaches depression myalgia arthritis cardiovascular event hepatotoxicity Fitzpatrick p.8 |
|
|
|
What does AML stand for?
|
acute myeloid leukemia
|
|
|
|
How long does isotretinoin therapy take and how many courses are necessary?
|
most patients improve w/in 20 weeks
most patients only require one course to induce lasting remission but 3 courses may be necessary Fitzpatrick p.8 |
|
|
|
What is the function of linoleic acid?
|
regulation of keratinocyte proliferation
Fitzpatrick p.2 |
|
|
|
Is linoleic acid increased or decreased in acne?
|
decreased
Fitzpatrick p.2 |
|
|
|
What is the cause of inflammation and scarring in acne?
|
keratin plugging + interaction b/w androgens and propionibacterium acnes w/in plug
androgens stimulate sebaceous glands to produce sebum bacteria convert lipids to fatty acids via lipase bacteria also produce proinflammatory mediators if keratin plug forms, sebum cannot be released follicle distends follicular wall breaks keratin, sebum, bacteria, lipids, and fatty acids enter dermis fatty acids and proinflammatory mediators produce inflammatory/foreign-body response -> inflammation rupture + intense inflammation -> scarring Fitzpatrick p.2 |
|
|
|
The presence of what type of lesion is required for diagnosis of any type of acne?
|
comedones
Fitzpatrick p.6 |
|
|
|
Drug-induced acne (including steroids) presents w/ comedones, true or false?
|
false
Fitzpatrick p.6 |
|
|
|
When do acne flares often occur?
|
onset of menses
winter Fitzpatrick p.6 |
|
|
|
What additional management may be needed for acne conglobata?
|
systemic corticosteroids
Fitzpatrick p.8 |
|
|
|
List the types of acne lesions and their associated, depth, inflammation, and severity.
|
comedones -> blockage near surface, slight inflammation, least severe
papules pustules nodules cysts -> blockage very deep, intense inflammation, most severe http://tiny.cc/acne598 |
|
|
|
Patient's with acne should use oil-free cosmetics, true or false?
|
true
look for labels that say non-comedogenic (does not cause comedones) or non-acnegenic (does not cause pimples) remove nightly w/ mild cleanser and lukewarm water http://tiny.cc/acne598 |
|
|

|
mongolian spot
|
|
|

|
comedonal acne
|
|
|

|
papular acne
|
|
|

|
pustular acne
|
|
|

|
acne conglobata
|
|
|

|
acne conglobata
|
|
|

|
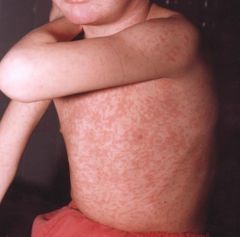
erythema infectiosum
|
|
|
|
What does CML stand for?
|
chronic myeloid leukemia
|
|
|
|
What is CML?
|
myeloproliferative disorder characterized by overproduction of myeloid cells with normal bone marrow function in early phase
|
Current p461
|
|
|
What is the etiology of CML?
|
philadelphia chromosome; presents during middle age
|
Current p461
|
|
|
What is the clinical presentation of CML?
|
fatigue, low fever, night sweats
splenomegaly sternal tenderness due to marrow overexpansion |
Current p461
|
|
|
What is the diagnostic work-up of CML?
|
CBC → high WBC count
blood smear → shift to the left, dominated by mature forms bone marrow biopsy → hypercelluar, shift to the left PCR for philadelphia chromosome → bcr/abl gene present |
Current p461
|
|
|
What is the management of CML?
|
1. refer to hematologist
If normal bone marrow function: 2. imatinib mesylate 400mg PO daily 3. if refractory to oral agents → bone marrow transplant If accelerated CML: 4. imatinib 600mg PO daily initially 5. bone marrow transplant 7. if leukostasis → emergent leukophoresis + myelosuppressive therapy |
Current p462
|
|
|
What are the complication sof CML?
|
1. leukostasis
2. progression to acute leukemia |
Current p462
|
|
|
What is the prognosis of CML?
|
80% survival rate at 7 years
|
Current p462
|
|

Abdominal mass seen in 7 year old with dyspnea.
|
Wilm's tumor
|
|
|
|
What is the common name for varicella?
|
chickenpox
|
|
|
|
What is etiology of varicella?
|
varicella zoster virus (VZV) AKA HHV-3
spread via respiratory droplets or lesion contact peak age 5-10 year round highly contagious |
Current p1239
|
|
|
What is the clinical presentation of varicella?
|

10-21 day incubation period
1-3 day prodrome with variable symptoms (mild fatigue, fever, HA, respiratory sxs) red maculopapules → clear vesicles on erythematous base ("dew drop on a rose petal") → pustules (superficial and elliptical with serrated borders) → crusts over 5-6 days affects scalp, face and trunk → extremities lesions can also occur in nose, mouth, conjunctiva, vagina pruritis |
Current p1239
|
|
|
What is the time frame for varicella lesions?
|
new lesions for 1-7 days
crusts slough in 7-10 days |
|
|
|
What is the diagnostic work-up for varicella or herpes zoster?
|
diagnosis usually made clinically; confirmation via DFA or PCR
|
Current p1241
|
|
|
What are the complications of varicella?
|
pitted scars
2° bacterial skin infections → staph, group A strep |
Current p1241
|
|
|
What is the management of varicella?
|
1. acetominphen for fever
2. antihistamines or cool soaks for pruritus 3. acyclovir if chronic disease or immunocompromised 3. keep fingernails short and skin clean to prevent 2° bacterial skin infections and scarring 4. bed rest until afebrile 5. isolation until crusts disappear |
Current p1242
|
|
|
What is the prevention for varicella?
|
vaccination via VARIVAX (varicella only) or MMRV at 12-15 months and 4-6 years
|
Current p1241
|
|
|
When should the MMR and varicella vaccinations be given?
|
12-15 months and 4-6 years
|
Current p1241
|
|
|
When is varicella no longer contagious?
|
when crusts begin to form
|
|
|
|
What is the common name for rubeola?
|
measles
|
|
|
|
What is the etiology of rubeola?
|
caused by a paramixovirus; spread via respiratory droplets; virtually eliminated in U.S.
|
Current 1247
|
|
|
What is the clinical presentation of rubeola?
|
9-14 day incubation period for onset of rash
prodrome of fatigue, fever, conjunctivitis, photophobia, rhinorrhea, cough Koplik spots 1-2 days prior to onset of rash and after onset of rash maculopapular rash, 3-4 days after onset of prodrome, brick-red, irregular, coalescent spreads downward from face and hairline to trunk and outward including palms and soles, lasting 6 days |
Current 1247
|
|
|
What is the diagnostic work-up of rubeola?
|
usually diagnosed clinically; supported by IgM measles Ab
leukopenia |
Current 1248
|
|
|
What disease are Koplik spots associated with?
|
rubeola
|
Current 1248
|
|
|
What are Koplik spots?
|

prodromic enanthem of rubeola; resemble grains of salt on wet background; found on buccal mucosa
|
|
|
|
"Grains of salt on a wet background" describe?
|

Koplik spots
|
|
|
|
What are the complications of rubeola?
|
1. diarrhea and protein-losing enteropathy → especially significant in malnourished
2. bronchopneumonia or broncholitis 3. secondary bacterial infections 4. encephalitis |
Current p1248
|
|
|
What is the management of rubeola?
|
Supportive:
1. acetominophen for fever 2. vitamin A 200,000 units/d PO x 2 days 3. antibiotics for 2° bacterial infections 4. fluids as necessary 5. bed rest until afebrile 6. isolation for 1 week following onset of rash |
Current p1249
|
|

|
koplik spots → rubeola
|
|
|

|
rubeola
|
|
|
|
rubeola
|
|
|
|
What is the common name for rubella?
|
german measles
|
|
|
|
What is the etiology of rubella?
|
caused by a togavirus; spread via respiratory droplets; fetal rubella common in third world countries
|
Current p1254
|
|
|
What is the clinical presentation of rubella?
|
50% asymptomatic
fatigue, fever, rhinorrhea suboccipital, postauricular and posterior cervical lymphadenopathy rash → maculopapular, fine, pink; face → trunk → extremeties; fades quickly lasting 1 day each area if adult → 25% polyarticular arthritis of wrists, fingers, knees for 1 to several weeks |
Current p1254
|
|
|
What is the diagnostic work-up of rubella?
|
IgM Ab, 4-fold rise in IgG Ab, viral PCR, or viral culture
|
Current p1254
|
|
|
What is the procedure for serological testing of rubella on pregnant women?
|
1. rubella ordered to R/O possibility of prenatal infection
2. positive IgG suggests vaccination or past infection 3. positive IgM suggests POSSIBLE current infection but interpret with caution 4. negative IgM and IgG requires clinical observation and serological follow-up |
Current p1254
|
|
|
What are the complications of rubella?
|
congenital rubella → teratogenic → permanent congenital defects, high mortality rate
|
Current p1254
|
|
|
What is the management of rubella?
|
Supportive:
1. acetominophen If prenatal: 1. possible therapeutic abortion |
Current p1254
|
|
|
What are the differences between postnastal and congenital rubella?
|
postnatal → mild, usually lasts 3-4 days
congenital → teratogenic → congenital defects and high mortality rate |
|
|

|
rubella
|
|
|
|
What disease is characterized by rash starting on face and spreading downward and outward to palms and soles?
|
rubeola
|
|
|
|
What disease is characterized by rash starting on trunk and spreading to extremities?
|
varicella
|
|
|
|
What disease is characterized by rash starting on face, then spreading to trunk, then extremeties in quick sucession, lasting 1 day each?
|
rubella
|
|
|
|
What is the common name for torticollis?
|
wry neck
|
|
|
|
What is the etiology of torticollis?
|
usually d/t sternocleidomastoid muscle injury during delivery causing contracture of sternocleidomastoid muscle
other causes include congenital cervical spine deformity, mild trauma, URTI, RA, cerebellar or spinal cord tumor, syringomyelia |
Peds Current
|
|
|
What is the clinical presentation of torticollis?
|

head tilt toward affected side
+/- fibrous mass in midportion of SCM |
Peds Current
|
|
|
What is the diagnostic workup of torticollis?
|
radiograph of spine to R/O spine deformity
|
Peds Current
|
|
|
What is the management of torticollis?
|
1. if sternocleidomastoid → passive stretching, surgery if does not resolve within 1 year
|
Peds Current
|
|

|
scoliosis
|
|
|
|
What is the clinical presentation of Salter-Harris fractures?
|
history of trauma
acute pain localized swelling and maximal tenderness over growth plate |
EOMC p866
|
|
|
What is the management of Salter-Harris fractures?
|
1. reduction
2. maintain reduction during healing process 3. avoid growth arrest 4. fractures usually heal within 4-6 weeks 5. if type I-III → closed reduction + cast 6. if type IV-V → open reduction and internal fixation 7. follow-up in 1 year |
EOMC p866
|
|
|
What are the complications of Salter-Harris fractures?
|
growth arrest
|
EOMC p866
|
|
|
What is transient synovitis?
|
inflammation of the synovium of the hip joint that occurs in children
|
Orthopedics p200
|
|
|
What is the etiology of transient synovitis?
|
cause unknown
possibly caused by trauma or viral infection diagnosis of exclusion |
Orthopedics p200
|
|
|
Define synovium.
|
soft tissue that lines non-cartilaginous surfaces within joint cavities
|
|
|
|
What is the most common cause of hip pain in children?
|
transient synovitis
|
Orthopedics p200
|
|
|
What is the clinical presentation of transient synovitis?
|
acute onset
painful limp pain referred to inner aspect of thigh and knee joint hip → slight flexion, abduction, and external rotation restricted passive abduction and internal rotation possible fever |
Orthopedics p200
|
|
|
What is the diagnostic workup of transient synovitis?
|
radiographs usually normal
may reveal swelling of capsule and adjacent soft tissue, slight widening of joint space synovial fluid if suspected septic arthritis (i.e. fever, non-weight-bearing, WBC count >12,000, elevated ESR or CRP) |
Orthopedics p200
|
|
|
What is the management of transient synovitis?
|
1. elimination of weight bearing and bed rest
2. crutches x 2-4 weeks 3. monitor for 2 years for possible development of Legg-Calves-Perthes disease |
Orthopedics p201
|
|
|
What is a Salter I fracture?
|

fracture of physis
|
|
|
|
What is a Salter II fracture?
|

fracture of metaphysis and physis
|
|
|
|
What is a Salter III fracture?
|

fracture of physis and epiphysis
|
|
|
|
What is a Salter IV fracture?
|

fracture of metaphysis, physis, and epiphysis
|
|
|
|
What is a Salter V fracture?
|

compression fracture of physis
|
|
|

|
salter-harris II fracture (of distal femur)
|
|
|

|
salter-harris III fracture (of distal tibia)
|
|
|

|
salter-harris I fracture (of distal radius)
|
|
|

|
salter-harris IV fracture (of proximal phalanx of big toe)
|
|
|
|
What patient population are greenstick and torus fractures associated with and why?
|
pediatrics
pediatric bones are softer and thus able to bend and only partially break adult bones become harder and more brittle with age |
|
|

|
greenstick fracture (of radius and ulna)
|
|
|
|
What is the mnemonic for Salter-Harris fractures?
|
S - same - I
A - above - II L - below - III T - through - IV R - rammed - V |
|
|
|
What are the complications of a Salter-Harris type V fracture?
|
98% chance of growth arrest
|
Approach To The Orthopedic Patient handout
|
|
|
What is the etiology of juvenile rheumatoid arthritis?
|
usually occurs between 1-3y/o and 8-12y/o
2x more common in females |
|
|
|
What is juvenile rheumatoid arthritis?
|
inflammatory arthritic syndrome
types include: pauciarticular → affects <5 joints polyarticular systemic |
|
|
|
What is the clinical presentation of juvenile rheumatoid arthritis?
|
if systemic → high fever, rash, lymphadenopathy, carditis, splenomegaly, arthritis
if polyarticular → low fever, fewer systemic symptoms, ≥5 joints invovled if pauciarticular → iridocyclitis, affects <5 joints |
|
|
|
What are the complications of juvenile rheumatoid arthritis?
|
if pauciarticular → iridocyclitis may lead to blindness
|
|
|
|
What is the diagnostic workup of juvenile rheumatoid arthritis?
|
RF usually negative
if pauciarticular → opthalmic slit-lamp evaluation |
|
|
|
What is the clinical presentation of erb's palsy?
|

arm internally rotated and adducted ("waiter asking for tip")
|
Hoppenfeld p3
|
|
|
BABINSKI REFLEX
|
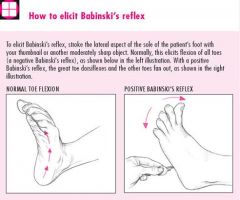
normal if positive when <2y/o
abnormal if positive when >2y/o → may indicate pyrimidal tract disease |
Mosbys p789
|
|
|
When is a positive Babinski reflex normal?
|
<2y/o
|
Mosbys p789
|
|
|
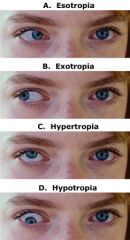
Define strabismus.
|
misalignment of the eyes
eyes that do not focus on an object simultaneously |
|
|
|
List the types of strabismus.
|
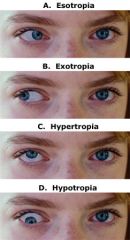
1. DIRECTION
esotropia → inward pointing eye(s) exotropia → outward pointing eye(s) hypertropia → upward pointing eye(s) hypotropia → downward pointing eye(s) 2. DURATION constant vs. intermittent |
|
|
|
How do you assess for strabismus?
|
corneal light reflex → if present, it will be asymmetrical
EOMs → possible restriction of eyes movements in certain directions of gaze cover uncover test |
|
|
|
Define craniosynostosis.
|
premature closure of cranial sutures
usually idiopathic may be associated with hereditary or metabolic disorders scaphocephaly → premature closure of sagittal suture → increase in cranial growth from anterior to posterior brachycephaly → premature closure of coronal suture → increase in cranial growth from left to right premature closure of ONE suture does not result in impaired brain growth or neurologic dysfunction |
|
|

|
sagittal craniosynostosis
|
|
|
|
Define hydrocephalus.
|
↑ volume of CSF with progressive ventricular dilation (brain swelling)
COMMUNICATING: CSF flow circulates through ventricular system into subarachnoid space without obstruction NON-COMMUNICATING: CSF flow blocked by obstruction |
|
|
|
What is the clinical presentation of hydrocephalus?
|

macrocephaly
excessive rate of head growth irritability vomiting anorexia impaired EOMs (upgaze) papilledema (if sutures closed) hypertonia of lower extremities hyperreflexia may result in optic atrophy if not treated |
|
|
|
When should WCC be scheduled?
|
newborn
1 month 2 month 4 month 6 month 9 month 12 month 15 month 18 month 2 years ... and yearly until 21 years |
|
|
|
Discuss the newborn exam.
|
PE:
VS → head circumference, length, weight GA → alertness, distress SKIN → jaundice, lesions HEENT → head → head shape/size, fontanelles, signs of birth trauma eyes → red reflex, opacification? ears → inspection nose → nasal patency, septal deviation mouth → cleft lip/palate, teeth, frenulum CV → auscultation, murmurs PV → femoral pulses GENITALIA → umbilical cord/vessels, descended testes, penile anomilies, patency M/S → back, spine, or foot deformities, ortolani, barlow NEURO → primitive reflexes BP vision hearing NBS |
|
|
|
Signs of dehydration in infants ...
|
depressed fontanelles
enopthalmos |
|
|
|
What is the leading cause of death in children and adolescents?
|
unintentional injuries (accidents)
|
|
|
|
What are the components of a sports physical?
|
sports physical is a screening for potential medical problems that could occur during athletic participation
screen 4-6 weeks before participation to allow time for any needed interventions by provider objectives: 1. establish baseline medical info 2. detect any medical condition that might limit participation 3. evaluate for preventable injuries 4. meet legal or insurance requirements 5. assess athlete’s maturity 6. make recommendations for protective equipment participation history: 1. cardiovascular history → investigate if <10y/o and BP >130/75 or ≥10y/o and BP >140/85; PMH of sudden fatigue, syncopal episodes, SOB, chest pain, recent illnesses with chest pain, cardiac murmur; FH of cardiac diseases (arrhythmias, prolonged QT syndrome, hypertrophic cardiomyopathy, Marfan syndrome, sudden death) 2. chronic disease history → reactive airway disease, exercise-induced asthma, liver disease, renal disease, neurologic disorders, hematologic disease, DM, chronic infections 3. M/S limitations → prior injuries, muscle weakness, limited ROM, overuse syndrome 4. menstruation → female athlete triad (eating disorder, amenorrhea, osteoporosis) 5. nutrition → attempts and methods to maintain, gain or lose weight 6. medications physical exam: 1. VS 2. HEENT → visual acuity, retinal problems 3. CV → auscultation for murmurs sitting and standing 4. ABD → hepatosplenomegaly 5. GENITALIA → testicular abnormalities, hernias, sexual maturity/tanner stage 6. PV → pulses 7. M/S → ROM, flexibility, strength, previous injuries 8. NEURO → mental processing, coordination, gait 9. SKIN → contagious lesions (herpes, impetigo) recommendations include unrestricted, limited or no participation |
|
|
|
Describe a preparticipation sports history.
|

|
|
|
|
Describe a preparticipation sports physical exam.
|

|
|
|
|
What are the components of the HEADDSS adolescent interview?
|
H → home
E → education/employment A → activities D → drugs and alcohol D → depression/suicide S → sleep S → sex |
|
|
|
*What are the recommendations for obtaining head circumference, length/height, weight, BP, HR and RR in infants, children, and adolescents?
|
head circumference → birth to 2 years
length height weight BP HR RR |
|
|
|
*What is the normal weight gain pattern in children?
|
weight drop following birth
return to birth weight by weight doubles by 6 months weight triples by 12 months |
|
|
|
What are the major milestones of pediatric development?
|
Gross motor skills:
lift head at 3 months sit at 6 months crawl at 9 months walk at 12 months run at 18 months Fine motor skills: raking motion involving ulnar aspect of hand at 3-4 months thumb added at 5 months picking up objects at 7 months pincer grasp at 9 months hand preference at 18-30 months Language: cooing with vowel sounds and reciprocal vocal play at 2 months babbling with consonants and repetition of sounds at 6-10 months increased comprehension at 9 months (understanding of 20-100 words by 13 months) 5-10 comprehensible words at 12-18 months 2-3 word phrases at 2 years use of verbs, “I”, “you” after 2 years Developmental and social skills: turn-taking games at 3-6 months separation anxiety and stranger anxiety at 8-9 months, peaks at 15 months, disappears at 2 years peek-a-boo at 9 months object permanence at 9-12 months single play from 1-2 years toileting at 18 months independence at 2 years parallel play at 2-3 years collaborative play at 3-4 years Accelerated separation-individuation at 5 years Achievement in school and acceptance by peers at 7 years |
|
|
|
What is the expected pattern of dental eruption?
|
Teeth generally begin to erupt at 6 months (but varies between 3-16 months)
Mandibular incisors usually erupt before maxillary incisors Associated fever, URTI, or systemic illness not related to teething |
|
|
|
What is the anticipatory guidance for each WCC?
|
newborn → family readiness, infant behavior, feeding, safety, routine baby care
1 week → maternal well-being, newborn transion, nutritional adequacy, safety, newborn care 1 month → marternal well-being, family adjustment, infant adjustment, feeding routines, safety 2 month → maternal well-being, infant behavior, infant-family synchrony, nutritional adequacy, safety 4 month → family functioning, infant development, nutritional adequacy and growth, oral health, safety 6 month → family functioning, infant development, nutritional adequacy and growth, oral health, safety 9 month → family adaptation, infant independence, feeding routine, safety 12 month → family support, establishing routines, feeding and appetite changes, dentist, safety 15 month → communication and social development, sleep routines and issues, temper tantrums and discipline, healthy teeth, safety 18 month → family support, child develpment and behavior, language and hearing, toilet training, safety 2 years → language, temperament and behavior, toilet training, tv, safety |
|
|
|
How do you assess the tonic neck reflex?
|
primitive reflex found in newborns
when turn head to one side, ipsilateral limbs will extend and contralateral limbs will flex sign of nervous system malfunction if occurs beyond 6 m/o |
|
|
|
When does the tonic neck reflex expire?
|

6 m/o
|
|
|
|
How do you assess for the moro (startle) reflex?
|

primitive reflex in newborns
startling newborn (by withdrawing head support, slapping bed, or creating a loud noise), causes arms to abduct, extend upward, and then arms to clasp together |
|
|
|
When does the moro (startle) reflex expire?
|
4-5 m/o
|
|
|
|
When do the anterior and posterior fontanelles normally close?
|
posterior fontanelle closed at 2 months
anterior fontanelle closure varies from about 3 months to 2 years average is 13.8 months tends to close earlier in boys than girls size not predictor of closure |
|
|
|
What are the benefitis and risks of circumcision?
|
BENEFITS:
prevention of phimosis, paraphimosis, balanoposthitis, UTI ↓ incidence of STIs, HIV, penile cancer ↓ incidence of cervical cancer in female sexual partners RISKS: bleeding infection urethral trauma removal of too much skin *incidence of complications <1% |
|
|
|
What are the indications and contraindications for circumcision?
|
INDICATIONS:
cultural or religious reasons hygeine required use of catheters hx of phimosis, paraphimosis, balanoposthitis, UTI CONTRAINDICATIONS: genital abnormalities (hypospadias, epispadias, curvature of penis, webbed penis, micropenis, concealed penis, ambiguous genitalia) RELATIVE CONTRAINDICATIONS: premature, ill, unstable, tendency to bleed (do coagulation screen if FH for bleeding disorders) |
|
|
|
What are the procedures used to to perform circumcision?
|
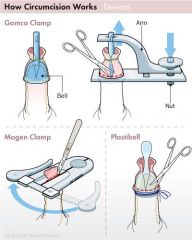
local anesthesia by either:
1. 1% lidocaine for dorsal penile nerve block or circumferential ring block 2. topical anesthetic cream TECHNIQUES: Plastibell (allows visualization of glans) Gomco clamp (allows visualization of glans) Mogen clamp (blind technique which may result in amputation of glans) |
|
|
|
When does strabismus usually occur in children?
|
2-5y/o
|
|
|
|
What are cleft lip and cleft palate?
|
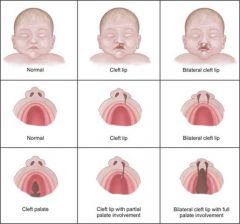
|
|
|
|
What are the recommendations regarding breast feeding?
|
breast feed solely until 6 months
|
|
|
|
What are the recommendations for introducing new foods into infant diet?
|
begin introducing solids at 6 months
introduce 1 new food per week |
|
|
|
What is the placing reflex and how is it assessed?
|
primitive newborn reflex
when infant's hand of foot brought into contanct with edge of table, it is automatically lifted and placed on surface |
|
|
|
When does the placing reflex expire?
|
6 months
|
|
|
|
What is the rooting reflex and how is it assessed?
|
primitive newborn reflex
when stroked cheek of infant, will turn toward side that was stroked and make sucking motions with mouth assists in breastfeeding |
|
|
|
When does the rooting reflex expire?
|
4 months
|
|
|
|
What is the palmar grasp and how is it assessed?
|
primitive newborn reflex
place finger in infant's hand, hand will close around finger and attempt to remove finger causes hand to tighten |
|
|
|
When does the palmar grasp reflex expire?
|
5-6 months
|
|
|
|
What is the sucking reflex and how is it assessed?
|
primitive newborn reflex
infant instinctively sucks at anything that touches the roof of the mouth linked with rooting reflex and breastfeeding |
|
|
|
When does the sucking reflex expire?
|
4 months
|
|
|
|
What is breast feeding associated jaundice?
|
ETIOLOGY:
exaggerated physiologic jaundice associated with inadequate intake of breast milk, infrequent stooling, and unsatisfactory weight gain may be caused by unidentified factor in breast milk that inhibits conjugation of bilirubin CLINICAL PRESENTATION: jaundice, inadequate milk intake, infrequent stooling, inadequate weight gain DIAGNOSTIC WORKUP: bilirubin MANAGEMENT: increase frequency of nursing if necessary augment infant’s sucking with regular breast pumping (to increase milk production) if suspected d/t impaired conjugation of bilirubin → stop breast feeding for 24-36 hours (use breast pump during this period) PREVENTION: use appropriate breast feeding techniques |
|
|
|
What are the recommendations for breast feeding?
|
BREAST FEEDING RECOMMENDATIONS:
1. start as soon as mother and baby stable 2. feed newborn every 2-3 hours during day and every 4-5 hours at night for total of 8-10 feedings per day 3. guideline for duration of feeding is 5 minutes per breast at each feeding the first day, 10 minutes on each side at each feeding the second day, and 10–15 minutes per side thereafter 4. alternate side on which feeding commences 5. place finger in infant’s mouth to break suction after nursing 6. loose stool passed with every feeding with newborns (failure indicates inadequate feeding) and every few days for 3-4 m/o 7. breast feed exclusively for first 6 months of life 8. begin to add solid foods at 6 months but continue to breast feed up to 2 years 9. if newborn <1750g → fortify breast milk to increase calories, protein, calcium, phosphorus, and micronutrients 10. contraindicated if maternal HIV, maternal TB, mother taking certain drugs, infant galactosemia BREAST FEEDING BENEFITS: 1. nutrition → (1) relatively low but highly bioavailable protein content (2) generous but not excessive quantity of essential fatty acids (3) long-chain polyunsaturated fatty acids, of which DHA is thought to be especially important; (4) relatively low sodium and solute load (5) lower concentration of highly bioavailable minerals 2. immunologic factors (IgA, lysozyme, lactoferrin, bifidus factor, macrophages) → provide protection against URTI and GI infections 3. encourages maternal-baby interaction 4. provides source of security and comfort to infant 5. free! BREAST FEEDING BARRIERS: 1. educate on correct infant positioning and latch – stomach to stomach, mouthful of breast 2. do not schedule feedings 3. do not allow breast to become engorged (reduces milk production) → pump if necessary 4. if nipple tenderness → correct positioning and latch, use less sore side, nurse for shorter periods, temporarily pump, use lanolin cream, analgesics and antibiotics for mastitis (but continue breast feeding) RECOMMENDATIONS FOR INTRODUCING SOLID FOOD: 1. start introducing solid foods at 6 months 2. introduce single component foods, one at a time, at 3-4 day intervals before another new food is given (to be able to detect allergies) 3. fortified cereals, fruits, vegetables, and meats 4. fruit juice not essential, only give after 6 months, only offer in cup, only give 4oz 5. avoid cow’s milk until 12 months 6. avoid honey, strawberries, peanuts, peanut butter, shellfish, chocolate |
|
|
|
Describe the APGAR Score.
|
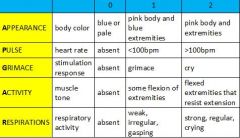
1. evaluation of infant at 1 minute and 5 minutes following birth
2. add scores of five individual observations for score between 0-10 3. continue at 5-minute intervals for ≤ 20 minutes until score ≥7 4. score reflects cardiopulmonary and neurological status 5. score does not determine need for resuscitation 6. 5 minute score of 0-3 associated with increased mortality |
|
|
|
Describe the care of an infant immediately following delivery.
|
dry infant with pre-warmed towels
suction nose and mouth to clear airway resuscitation? (bradycardia, central cyanosis, grunting) determine APGAR score perform bried exam skin color chest auscultation musculoskeletal birth-related trauma? congenital defects? umbilical cord vessels (should be 2 arteries and 1 vein) placenta (for size, number of vessels, clots or infarcts) |
|
|
|
Define caput succedaneum.
|
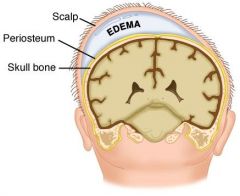
subcutaneous edema over presenting part of head
d/t force on scalp and skull during labor maximal at birth rapidly grows smaller disappears within hours to days |
|
|
|
Define cephalohematoma.
|

subperiosteal hematoma over presenting part of head
d/t force on scalp and skull during labor may not be apparent until hours after delivery grows larger disappears after weeks to months |
|
|
|
What is the normal range for total bilirubin?
|
0.3-1.0 mg/dL
|
|
|
|
What is the normal range for indirect (unconjugated) bilirubin?
|
0.2-0.7 mg/dL
|
|
|
|
What is the normal range for direct (conjugated) bilirubin?
|
0.1-0.3 mg/dL
|
|
|
|
Describe bilirubin metabolism.
|
RBC breakdown in spleen and bone marrow → heme broken down into iron, carbon monoxide, and biliverdin by heme oxygenase → iron is conserved, carbon monoxide is exhaled, and bilivirdin is converted to unconjugated biliruin by bilirubin reductase → unconjugated bilirubin is bound to albumin and transported to liver → unconjugated bilirubin converted to conjugated bilirubin by UDPGT → conjugated bilirubin secreted through bile into intestines → conjugated bilirubin converted to stercobilins and excreted in feces
|
|
|
|
At what total bilirubin concentration does jaundice develop?
|
2-4 mg/dL
|
|
|
|
PHYSIOLOGIC JAUNDICE:
|
ETIOLOGY:
65% of newborns develop jaundice during 1st week of life factors contributing to physiologic jaundice include: 1. ↑ RBC count 2. ↓UDPGT activity 3. ↓ intestinal motility (causing stasis of bilirubin in intestines) 4. ↓ intestinal flora (causing stasis of bilirubin in intestines) 5. ↑enterohepatic circulation of bilirubin (following stasis of bilirubin) CLINICAL PRESENTATION: jaundice manifests at 24 hours old resolves by 1 week if full-term and 2 weeks if pre-term DIAGNOSTIC WORKUP: total bilirubin rises <5 mg/dL/day peaks at <15 mg/dL at 3-5 days old MANAGEMENT: monitor total serum bilirubin no treatment → physiologic jaundice is normal PREVENTION: none → physiologic jaundice is normal |
|
|
|
What are the diagnostic criteria for physiologic jaundice?
|
TOTAL SERUM BILIRUBIN:
rises <5 mg/dL/day peaks at <15 mg/dL at 3-5 days old |
|
|
|
How long may maternal antibodies be present in newborns?
|
2-3 months
|
|
|
|
ANTIBODY-MEDIATED HEMOLYSIS:
|
ETIOLOGY:
hemolysis → increased bilirubin production → hyperbilirubinemia → jaundice ABO incompatibility: type O mother has maternal anti-A and anti-B IgG antibodies that attack fetal RBCs (maternal antibodies may persist several months after birth) hemolysis usually mild but severity varies (20% of pregnancies can result in ABO incompatibility but only 33% of those 20% have positive direct coombs tests and only 20% of those 33% develop jaundice requiring therapy) Rh-isoimmunization: Rh-negative mother produces antibodies against Rh-positive fetus (usually affects fetus of subsequent pregnancy) less common, more severe, and more predictable than ABO incompatibility severity increases with each immunized pregnancy CLINICAL PRESENTATION: signs of anemia (fatigue, weakness, pallor) jaundice splenomegaly dark urine erythroblastosis fetalis → most severe form of Rh-isoimmunization, characterized by life-threatening anemia, HF, and edema DIAGNOSTIC WORKUP: anemia reticulocytosis hyperbilirubinemia → total serum bilirubin >5 mg/dL before 24 hours positive direct coombs MANAGEMENT: 1. transfuse Rh-negative cells into umbilical vein or into fetal abdominal cavity 2. IV immune globulin (IVIG 0.5-1 g/kg) upon delivery 3. phototherapy upon delivery 4. transfuse packed RBCs as needed 5. monitor for 2-3 months (until maternal antibodies no longer present) for recurrent anemia requiring transfusion PREVENTION: Rh-isoimmunization → give RhoGam to Rh-negative women during pregnancy |
|
|
|
NON-IMMUNE HEMOLYSIS:
|
instrinsic:
genetic disease (sickle cell, G6PD, thalassemia?) extrinsic: mechanical damage (artificial heart valve) infection (HUS) hepatic disease? renal disease? |
|
|
|
FETAL ALCOHOL SYNDROME:
|
ETIOLOGY:
• excessive exposure to alcohol during gestation affects 30-40% of mothers whose daily alcohol intake exceeds 3 ounces CLINICAL PRESENTATION: • growth deficiencies – low birth weight, poor head growth, short stature • facial abnormalities – midface hypoplasia, narrow palpebral fissures, short nose with anteverted nares, long poorly developed philtrum • developmental delay – difficulty in complex cognitive tasks (speech, planning, attention) and lack of appropriate social interaction and judgment • IQ usually in 60’s • associated with neural tube, cardiac, and GU malformations diagnosis requires presence of growth deficiency, facial abnormalities, and neurodevelopmental problems MANAGEMENT: • evaluation by a multidisciplinary team – examination of growth, facial features, cognitive abilities, behavioral function, and documentation of prenatal alcohol exposure • emphasize structure in child’s life – types of structure may include visual structure (color code each content area), environmental structure (keep work area uncluttered, avoid decorations), and task structure (clear beginning, middle, and end) medications may be needed for attention and mood disorders |
|
|
|
What is Turner syndrome?
|

sex-linked genetic disorder characterized by partial or complete absence of an X chromosome in female
|
|
|
|
What is the etiology of Turner syndrome?
|
sex-linked genetic disorder characterized by partial or complete absence of an X chromosome in female
|
|
|
|
What is the clinical presentation of Turner syndrome?
|

• short stature, triangular facies, epicanthal folds, high-arched palate, webbed neck, shield chest, wide-set nipples, short 4th metacarpals, edema of hands and feet
• hypogonadism, absence of 2° sex characteristics (small breasts, sparse pubic hair), primary amenorrhea • streak ovaries, infertility • associated with coarctation of the aorta and GU malformations • IQ normal but learning disabilities common (2° to difficulties in perceptual motor integration) |
|
|
|
What is the diagnostic workup of Turner syndrome?
|
blood karyotype → 45,XO or X chromosome abnormalities or mosaicism
elevated FSH and LH normal GH and IGF-1 |
|
|
|
What is the management of Turner syndrome?
|
1. growth hormone therapy to increase height
2. estrogen replacement therapy to induce development of 2° sex characteristics and menstruation and to prevent osteoporosis 3. begin estrogen therapy at 12y/o and add progestin when growth stops 4. monitor for cardiac problems (100-fold increased risk for aortic dissection), renal problems, DM |
|
|

|
Turner syndrome
|
|
|
|
KLINEFELTER SYNDROME:
|

ETIOLOGY:
• extra X chromosome(s) in males (usually XXY but may be XXXY or XXXXY) CLINICAL PRESENTATION: • males appear normal until puberty • tall, disproportionately long arms and legs, eunuchoid build • minimal facial hair, gynecomastia • small, firm, fibrotic, nontender testes • lack of libido • infertility d/t azoospermia • IQ varies from normal to borderline MANAGEMENT: • testosterone replacement therapy • high risk for DM and breast cancer so consider appropriate screening |
|
|

|
klinefelter syndrome
|
|
|
|
DOWN SYNDROME:
|
ETIOLOGY:
• 3 copies of chromosome 21 or a chromosome rearrangement that results in 3 copies of a region of the long arm of chromosome 21 • high risk if mother >35y/o CLINICAL PRESENTATION: • flat occiput, midface hypoplasia, small dysplastic pinnae, upslanting palpebral fissures, epicanthal folds, large tongue • generalized hypotonia • mental retardation • associated with congenital heart disease in 50% • associated with GI malformations (esophageal and duodenal atresias) • may see feeding problems, prolonged jaundice, polycythemia, and a transient leukemoid reaction in newborns • may see hearing loss, hypothyroidism, celiac disease, atlanto-occipital instability during childhood • risk of leukemia 12-20 times higher than in general population MANAGEMENT: • goal of treatment is to help affected children develop to their full potential • infant stimulation programs • special education • physical, occupational, and speech therapies • support groups for families • appropriate management of congenital heart disease and GI malformations • monitor for common complications (hearing loss, hypothyroidism, celiac disease, atlanto-occipital instability, leukemia) |
|
|
|
What is spina bifida?
|

congenital defect characterized by incomplete neural tube closure
|
|
|
|
SPINA BIFIDA:
|
ETIOLOGY:
caused by genetic syndrome or teratogens (alcohol, valproic acid) CLINICAL PRESENTATION: detectable by ↑ AFP and US open or skin-covered lesion protruding from back associated with hydrocephalus, Arnold-Chiari II malformation, neurogenic bladder and bowel, congenital paralysis of lower extremities neurologic deficit depends on location of lesion MANAGEMENT: MRI place in prone position keep lesion moist with sterile dressing monitor for hydrocephalus surgery for closure within 24-48 hours to reduce risk of infection correct additional abnormalities if suspected genetic syndrome → evaluation by geneticist and chromosome analysis if future pregnancies → genetic counseling, folic acid supplementation d/t risk of recurrence support groups |
|
|
|
What are mongolian spots?
|
blue macules
|
Fitzpatrick pxxvii
|
|
|
How should lesions be described?
|
distribution, configuration, color, secondary changes, primary changes
for example → generalized, discrete, red, scaly papules |
|
|
|
What are milia?
|
tiny keratin-filled epidermal cysts
|
|
|
|
MILIA:
|

ETIOLOGY:
dead skin trapped in pockets at surface of skin or mouth CLINICAL PRESENTATION: tiny white bumps (1-2 mm keratin-filled epidermal cysts) found on face, typically nose, cheeks, and chin (in 40% of newborns) found in mouth and called Epstein pearls, typically roof and gums (in 60-85% of newborns) MANAGEMENT: self-limiting → resolves within first few weeks of life |
|
|

|
milia in newborn
|
|
|
|
What is acne neonatorium?
|
neonatal acne vulgaris characterized by inflammatory papules and pustules + occasional comedones on face
|
|
|
|
ACNE NEONATORIUM:
|

ETIOLOGY:
cause unknown may be associated with increased sensitivity of fetal sebaceous glands to maternal hormones during pregnancy CLINICAL PRESENTATION: may present at birth but usually develops between 2-4 weeks inflammatory papules and pustules occasionally comedones usually occur on face (in 20% of newborns) MANAGEMENT: self-limiting → resolves within 6-12 months without scarring |
|
|

|
acne neonatorum (AKA neonatal acne vulgaris)
|
|
|
|
What is the common name for miliaria?
|
heat rash
|
|
|
|
MILIARIA:
|
ETIOLOGY:
heat and high humidity → pore closure of eccrine sweat ducts → obstruction of eccrine sweat ducts superficial obstruction in stratum corneum causes miliaria crystallina deep obstruction in epidermis causes miliaria rubra CLINICAL PRESENTATION: miliaria crystalline → grouped, 1-2 mm, superficial clear vesicles miliaria rubra → grouped, deep erythematous papules; may progress to pustules; pruritic both found in intertriginous areas and adjacent skin (neck, upper chest) MANAGEMENT: cool environment to prevent sweating |
|
|
|
List transient newborn skin disorders.
|
milia
acne neonatorum miliaria |
|
|
|
ERYTHEMA TOXICUM:
|

ETIOLOGY:
cause unknown associated with eosinophilia more common if full-term CLINICAL PRESENTATION: usually manifests at 24-48 hours but occasionally present at birth 2-3 cm blotchy erythematous macules may progress to wheals in center of macules may progress to pustules range from few to 100 usually occur on chest but also face, back, and extremities MANAGEMENT: self-limiting → resolve within 5-7 days |
|
|

|
erythema toxicum
|
|
|
|
MONGOLIAN SPOTS:
|

ETIOLOGY:
spindle-shaped pigment cells deep in dermis occur in Native American, African American, or Asian descent normal variant CLINICAL PRESENTATION: blue-black macule found in lumbosacral area (and sometimes shoulder, back, or buttocks) MANAGEMENT: none → normal variant, may fade with time |
|
|

|
mongolian spot
|
|
|
|
CAFE AU LAIT MACULES:
|

ETIOLOGY:
increase in melanin content normal variant also consider neurofibromatosis type 1 (if ≥6 lesions >1.5 cm), McCune-Albright syndrome (if large and unilateral), tuberous sclerosis, Fanconi anemia CLINICAL PRESENTATION: light brown oval macule on light skin dark brown oval macule on dark skin found anywhere on body MANAGEMENT: typically none → normal variant, persist throughout life consider NF-1 if multiple present or increase in number |
|
|

|
cafe au lait macules
|
|
|

|
cafe-au-lait spot
|
|
|
|
PORT WINE STAINS:
|

ETIOLOGY:
vascular birthmark d/t permanent vascular abnormalities (dilation) consider Sturge-Weber syndrome (if bilateral facial lesion or covering entire half of face) or Klippel-Trenaunay syndrome (if over extremity) CLINICAL PRESENTATION: dark red macules found anywhere on body MANAGEMENT: laser treatment with pulsed dye laser |
|
|

|
port-wine stain
|
|
|
|
What are port-wine stains?
|
dark red macules d/t permanent vascular abnormalies
|
|
|
|
HEMANGIOMAS:
|

ETIOLOGY:
benign tumor of capillary endothelial cells CLINICAL PRESENTATION: permanent blanched area of skin at birth evolves into hemangioma at 2-4 weeks red rubbery nodule superficial, deep or mixed MANAGEMENT: 50% reach maximal regression by 5y/o, 70% by 7y/o and 90% by 9y/o redundant skin, hypopigmentation and telangiectasia remain laser therapy with pulsed dye laser may be helpful if ulcerated or bleeding complications requiring immediate treatment with prednisone: 1. visual obstruction 2. airway obstruction 3. cardiac decompensation |
|
|

|
hemangioma
|
|
|

|
tinea capitis
|
|
|

|
tinea corporis
|
|
|
|
TINEA CAPITIS:
|

ETIOLOGY:
fungal infection of hair and/or scalp caused by Trichophyton tonsurans (90%) or Microsporum canis (10%) CLINICAL PRESENTATION: thickened, broken-off hairs 2-3 mm from follicle leaving “black dot” appearance erythema and scaling of underlying scalp +/- diffuse pustules on scalp +/- boggy fluctuant mass (kerion) on scalp suggesting exaggerated host response MANAGEMENT: 1. wood lamp → Trichophyton tonsurans doesn’t fluoresce, Microsporum canis fluoresces yellow-green 2. KOH 3. fungal culture 4. oral griseofulvin (take with fatty meal to increase absorption) 5. continue fungal cultures every 4 weeks 6. continue medication 4 weeks following negative fungal culture |
|
|
|
TINEA CORPORIS, CRURIS, PEDIS & UNGUIUM
|

ETIOLOGY:
fungal infection usually caused by Trichophyton mentagrophytes, Trichophyton rubrum, Microsporum canis, Epidermophyton floccosum CLINICAL PRESENTATION: tinea corporis → annular marginated plaques with a thin scale and clear center or annular confluent dermatitis tinea cruris → symmetrical, sharply marginated lesions in inquinal areas tinea pedis → red scaly lesions on soles of feet or fissuring between toes tinea unguium (onychomycosis) → yellowed, thickened, crumbling nails MANAGEMENT: 1. KOH → scrape thin scales from border of lesion, positive for hyphae 2. fungal culture 3. treat tinea corporis, tinea cruris, and tinea pedis with topical → imidazoles, allylamines, benzylamines, or ciclopirox applied twice daily x 3-4 weeks 4. treat tinea unguium with griseofulvin (if refractory, try itraconazole or terbinafine) |
|
|

|
tinea pedis
|
|
|

|
tinea cruris
|
|
|

|
tinea corporis
|
|
|

|
tinea unguium
|
|
|
|
What is an atrial septal defect?
|
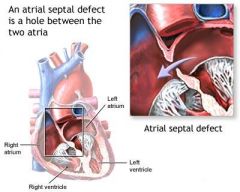
congenital heart defect characterized by persistence of foramen ovale or atrial-septal defect resulting in abnormal blood flow between atria
|
|
|
|
What is the clinical presentation and diagnostic workup of patent ductus arteriosus?
|
CLINICAL PRESENTATION:
dependent on size of shunt and degree of pulmonary HTN diaphoresis with feeding failure to thrive tachypnea S2 narrowly split or paradoxically split (narrows on inspiration and widens on expiration) continuous machinery murmur begins shortly after S1, peaks at S2, passes through S2 into diastole, becomes a decrescendo murmur and fades before S1 maximal at 2nd left intercostal space radiates into anterior lung fields diastolic flow murmur at apex bounding peripheral pulses widened pulse pressure DIAGNOSTIC WORKUP: CXR EKG ECHO |
|
|
|
What is patent ductus arteriosus?
|

congenital heart defect characterized by persistence of ductus arteriosus resulting in abnormal blood flow between pulmonary artery and aorta
ductus arteriosus normally closes spontaneously at 3-5 days of age |
|
|
|
What is tetralogy of fellot?
|

congenital heart defect characterized by:
1. narrowing of pulmonary valve 2. thickening of RT ventricular wall 3. displacement of aorta over ventricular-septal defect 4. ventricular-septal defect |
|
|
|
What is the clinical presentation and diagnostic workup of tetralogy of fellot?
|
CLINICAL PRESENTATION:
easy fatigability exertional dyspnea cyanotic spells characterized by: 1. sudden onset of cyanosis or deepening of cyanosis 2. dyspnea 3. altered consciousness ranging from irritability to syncope 4. decrease or disappearance of systolic ejection murmur d/t complete obstruction of right ventricular outflow tract squatting (though rare since often diagnosed at birth) cyanosis clubbing palpable RV lift rough systolic ejection murmur at left sternal border in 3rd ICS, radiates to back DIAGNOSTIC WORKUP: CBC → polycythemia 2° to chronic arterial desaturation CXR EKG ECHO |
|
|
|
What is rheumatic fever?
|
complication of strep throat or scarlet fever
|
|
|
|
What is the etiology of rheumatic fever?
|
strep throat
scarlet fever uncommon in United States |
|
|
|
What is the clinical presentation of rheumatic fever?
|

recent infection
fatigue fever erythema marginatum → erythematous rings mostly on trunk that disappear and reappear over weeks to months subcutaneous nodules → small painless nodules on extensor surfaces chorea → abrupt nonrhythmic involuntary movements and muscular weakness carditis polyarthritis |
|
|
|
What is the diagnostic workup of rheumatic fever?
|
↑ ESR
↑ CRP ↑ ASO → repeat in 10-14 days if normal ↑ PR interval on EKG → repeat in 2 weeks and 2 months if abnormal also order: CBC BC if febrile throat culture CXR echocardiogram → repeat in 1 month if negative |
Current
Harrisons |
|
|
What is the diagnostic (Jones) criteria of rheumatic fever?
|
recent strep throat + 2 major criteria or 1 major and 2 minor criteria
Major: erythema marginatum subcutaneous nodules pericarditis, myocarditis, or endocarditis polyarthritis chorea Minor: hx of rheumatic fever or rheumatic heart disease fever arthralgias ↑ ESR ↑ CRP ↑ ASO ↑ PR interval on EKG |
Current EMED ch19
|
|
|
What is the most common symptom of rheumatic fever?
|
arthritis
|
|
|
|
What is the management of rheumatic fever?
|
1. for strep throat → benzathine penicillin G 1.2 million units IM single dose
2. if penicillin allegy → erythromycin 40mg/kg daily 3. for fever and arthritis → aspirin 4. if refractory to aspirin → corticosteroids 4. bed rest until afebrile and resting HR, ESR, and EKG normal 5. to prevent recurrence → benzanthine penicillin G 1.2 million units IM every 4 weeks -if no carditis → continue until 21 y/p -if carditis + no valvular damage → continue for 10 years -if carditis + valvular damge → continue for 10 years or until 40y/o if high risk for reexsposure of strep throat (parent, teacher, medical professional, military personnel) If chorea: 1. provide calming environment 2. medications only control symptoms but do not alter duration or outcome 3. carbamazepine → may not see effect for 2 weeks, continue for 2 weeks after symptoms subside If HF: see HF management |
Current ch10
|
|
|
Who is most commonly affected by rheumatic fever?
|
children 5-15y/o
|
Current ch10
|
|
|
What are the complications of rheumatic fever?
|
1. CHF
2. rheumatic heart disease 3. myocardial involvement 4. arrhythmia 5. pericardial effusion 6. rheumatic pneumonitis |
Current ch10
|
|
|
What is bronchiolitis?
|
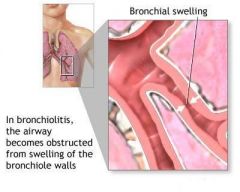
lower respiratory tract infection
inflammation of the bronchioles usually d/t viral infection |
|
|
|
BRONCHIOLITIS:
|
ETIOLOGY:
lower respiratory tract infection characterized by inflammation of the bronchioles usually caused by RSV other causes include Parainfluenza, human metapneumovirus, influenza, adenovirus, Mycoplasma, Chlamydia, Ureaplasma, Bocavirus, and Pneumocystis usually affects children <2y/o most common serious acute respiratory illness in young children CLINICAL PRESENTATION: irritability, poor feeding, coughing, vomiting labored breathing, tachypnea, hypoxia prolonged expiration, wheezing, crackles usual course → 1-2 days fever, rhinorrhea, and cough followed by respiratory distress (nasal flaring, retractions, cyanosis), tachypnea (shallow and rapid), and wheezing DIAGNOSTIC WORKUP: CBC → may be normal or mild lymphocytosis CXR not indicated in children if temperature not elevated, no significant respiratory distress, or bilateral symmetrical findings on exam MANAGEMENT: 1. supportive care → fluids, humidifier, rest, no smoking near child 2. hospitalization indicated if: a. history of apnea b. marked respiratory distress with retractions c. moderate tachypnea with feeding difficulties d. hypoxemia on room air 3. hospital supportive care → frequent suctioning, fluids to maintain hydration, supplemental O2 if hypoxemia present 4. do not prescribe antibiotics unless evidence of associated bacterial pneumonia 5. do not prescribe bronchodilators or corticosteroids (have not been shown to change severity or duration of illness) 6. PREVENTION: proper handwashing reduce exposure to potential environmental risk factors → cigarette smoke, crowded conditions PATIENT EDUCATION: cigarette smoke makes a child more susceptible to infection |
|
|
|
ASPIRATION OF FOREIGN BODY:
|
ETIOLOGY:
aspiration of foreign body into any part of respiratory tract history of running with food in mouth (seeds, peanuts, popcorn, hot dogs, hard candy) or playing with small coins or toys highest risk at 6 months to 4 years CLINICAL PRESENTATION: aspiration rarely observed abrupt onset of coughing, choking, or wheezing symptoms depend on location of obstruction (laryngospasm if above glottis) foreign body in upper respiratory tract: partial upper respiratory tract obstruction → ability to vocalize, drooling, stridor complete upper respiratory tract obstruction → acute onset of choking, inability to vocalize or cough, cyanosis with marked distress lower respiratory tract aspiration → abrupt onset of coughing, wheezing, or respiratory distress, asymmetrical decreased breath sounds, localized wheezing, chronic cough, persistent wheezing or recurrent pneumonia DIAGNOSTIC WORKUP: CXR → inspiratory and forced expiratory views, asymmetrical findings, 25% normal in setting of aspiration MANAGEMENT: if partial upper airway obstruction → initially allow child to use cough reflex to remove foreign body, intervene if does not resolved as brief observation if complete upper airway obstruction → intervene immediately 1. open airway, if foreign body is visualized carefully remove object, do not perform blind sweeps of mouth 2. if <1 y/o → place infant face down over rescuer’s arm with head positioned below trunk, deliver 5 rapid blows between scapulae with heel of hand, if obstruction persists roll child over and deliver 5 rapid chest compressions, repeat sequence until obstruction relieved 3. if >1 y/o → perform Heimlich maneuver with special care to prevent abdominal organ injury 4. if persistent inadequate ventilation → tracheotomy, cricothyrotomy, or intubation depending on skill and setting if lower airway aspiration → hosptitalization, bronchoscopy for removal of foreign body, nebulizer treatments and chest physiotherapy to treat bronchospasm and clear mucus PREVENTION: teach children not to run with food in mouth or swallow small objects teach older children not to give certain foods to younger children PATIENT EDUCATION: |
|
|
|
RESPIRATORY SYNCYTIAL VIRUS:
|
ETIOLOGY:
RSV causes 70% of bronchiolitis and 40% of pneumonia in young children CLINICAL PRESENTATION: epidemics in late fall to early spring (January–February peak) upper respiratory symptoms (low-grade fever for 2-4 days, cough, difficulty feeding) followed by tachypnea and diffuse wheezing for 3-7 days hyperinflation, retractions, prolonged expiration, wheezing, crackles may manifest with apnea complicated by otitis media, bacterial pneumonia DIAGNOSTIC WORKUP: RSV antigen in nasal or pulmonary secretions (fluorescent antibody or ELISA) CXR → diffuse hyperinflation, peribronchiolar thickening, +/- patchy infiltrates and atelectasis MANAGEMENT: outpatient: self-limiting hospitalization: 1. hospitalize if respiratory distress prevents feeding, hypoxia 2. tube or IV feedings 3. supplemental O2 4. trial of bronchodilator therapy, d/c if no improvement 5. corticosteroids and ribavirin controversial PREVENTION: proper handwashing respiratory isolation during peak season RSV monoclonal antibody IM monthly during peak season in high-risk children PATIENT EDUCATION: 90% of children infected by age 2 years reinfection common but generally only causes upper respiratory symptoms may increase risk of asthma later in life |
|
|
|
What is Sudden Infant Death Syndrome (SIDS)?
|
sudden death of an infant <1y/o without explanation despite a thorough case investigation (autospy, examination of death scene, review of clinical history)
|
|
|
|
SUDDEN INFANT DEATH SYNDROME:
|
ETIOLOGY:
sudden death of infant <1y/o without explanation diagnosis of exclusion after thorough case investigation (autopsy, examination of death scene, review of clinical history) affects <1:1000 infants, affects male:female 3:2, usually occurs between few weeks and 6 m/o, peak at 2-4 m/o risk factors include mothers who are racial minorities, teenagers, drug-addicted, low SES, smokers; FH of SIDS; low birth weight; prone sleeping position CLINICAL PRESENTATION: history of mild upper respiratory infection symptoms before death death usually occurs between midnight and 8am while sleeping DIAGNOSTIC WORKUP: autopsy examination of death scene MANAGEMENT: counseling and support groups → The National SIDS Resource Center (http://www.sidscenter.org) PREVENTION & PATIENT EDUCATION: do not smoke when pregnant place infant on back to sleep firm sleep surface pacifier use during nap or bedtime avoid overheating quit smoking educate family members, friends, and childcare providers on proper sleep position recent immunizations do not increase risk |
|
|
|
What is the etiology of CF?
|
autosomal recessive genetic disorder → abnormalities in cell membrane chloride channels → causing exocrine glands to produce abnormal mucus → causing obstruction of glands and ducts → causing glandular dilation and tissue damage
abnormalities occur in respiratory, GI, and male reproductive systems affects 1:3200 (1:25 is carrier) most common cause of severe lung disease in young adults most common fatal hereditary disorder in whites in U.S. |
|
|
|
What is the clinical presentation of CF?
|
meconium ileus at birth virtually diagnostic of CF
failure to thrive chronic or recurrent productive cough chronic or recurrent respiratory infections (sinusitis, bronchitis, pneumonia) purulent rhinorrhea, nasal polyps dyspnea, exercise intolerance hemoptysis bulky greasy malodorous stools and steatorrhea (d/t pancreatic insufficiency) increased AP diameter hyperresonance wheezing apical crackles clubbing also consider CF if severe dehydration + hypochloremic alkalosis, unexplained bronchiectasis, cirrhosis, or pancreatitis, rectal prolapse |
|
|
|
What is the diagnostic workup of CF?
|
nutritional deficiencies → hypoproteinemia, anemia, fat-soluble vitamin deficiencies
CXR → hyperinflation, mucus plugging, bronchiectasis, focal atelectasis, pnuemothorax PFTs → mixed obstruction and restriction; reduced FVC, airflow rates, TLC, air trapping, reduced diffusing capacity chloride sweat test → >60 mEg/L on two occasions genotyping → CF gene mutation positive NBS should be confirmed with chloride sweat test or genotyping false-negative NBS can occur |
|
|
|
What is the management of CF?
|
1. refer to CF center
2. high calorie, protein, fat, and salt diet 3. daily multivitamin 4. pancreatic enzyme supplement prior to eating 5. clear lower airway secretions via manual chest compressions etc. 6. treat active airway infections via antibiotics 7. inhaled bronchodilators 8. influenza and pneumococcal immunizations 9. lung transplant if end-stage lung disease 10. screen family members 11. genetic counseling and support groups |
|
|
|
What is the prevention of CF?
|
none → genetic disorder
|
|
|
|
What is the prognosis for CF?
|
median survival age is >35y/o
death occurs from pulmonary complications (pneumonia, pneumothorax, hemoptysis), chronic respiratory failure, or cor pulmonale |
|
|
|
APNEA:
|
ETIOLOGY:
unexplained breathing cessation for ≥20 seconds or shorter period of breathing cessation associated with bradycardia, pallor, cyanosis, or hypotonia central apnea: characterized by respiratory cessation 2° to diminished muscular activation occurs in newborns (especially preterm infants) d/t infection, metabolic abnormalities, anemia, hypoxia, CNS injury obstructive apnea: characterized by cessation of airflow despite respiratory effort (movement of chest wall and abdomen present) occurs in later infancy and childhood d/t obstructive upper airway conditions (tonsillitis, laryngitis, laryngomalacia, masses) CLINICAL PRESENTATION: breathing cessation DIAGNOSTIC WORKUP: central apnea → CBCDP, BMP, ionized calcium, magnesium, BC, UAC, URNC, toxicology studies; CT if abnormal mental status, bulging fontanelle, focal neurological sxs; LP if lethargic or toxic-appearing obstructive apnea → CXR, laternal neck radiograph, sleep study MANAGEMENT: hospitalization for observation and full workup pulse oximeter and apnea monitor supplemental O2 IV fluids if dehydrated |
|
|
|
What disorders comprise croup syndrome?
|
laryngotracheal bronchitis
epiglottitis bacterial tracheitis |
|
|
|
What is the ddx for acute stridor?
|
laryngeal or esophageal foreign body
croup → laryngotracheobronchitis, epiglottitis, bacterial tracheitis spasmodic croup retropharyngeal abscess angioedema |
|
|
|
What is croup?
|
group of disorders characterized by acute inflammation of the larynx
|
|
|
|
Laryngotracheal Bronchitis (AKA viral croup)
|
usually caused by parainfluenza viruses
also caused by RSV, human metapneumovirus, influenza virus, rubeola virus, adenovirus, and Mycoplasma pneumoniae usually affects younger children in fall and early winter edema in subglottic space results in signs of upper airway obstruction, though inflammation of entire airway is usually present prodrome of upper respiratory tract symptoms barking cough stridor usually no fever no drooling lateral neck radiograph treatment based on symptoms mild croup = barking cough, no stridor at rest → supportive therapy with oral hydration severe croup = barking cough, stridor at rest → supplemental O2, nebulized racemic epinephrine, dexamethasone (corticosteroid), recurrent nebulized racemic epinephrine if respiratory distress persists, intubation if impending respiratory failure most children improve within few days |
|
|
|
EPIGLOTTITIS:
|
usually d/t Haemophilus influenzae in unimmunized children, nontypeable Haemophilus influenza, Neisseria meningitides, or Streptococcus
sudden onset of high fever, dysphagia, drooling, muffled voice cyanosis, inspiratory retractions, soft stridor sitting-dog position (provides best airway) lateral neck radiographs reveal “thumbprint” sign swollen cherry red epiglottis and swollen arytenoids management: 1. immediate intubation in children once diagnosis established 2. BC 3. epiglottis culture 4. IV antibiotics covering Haemophilus influenza and Streptococcus → cefriaxone x 2-3 days 5. oral antibiotics x 7 days 6. extubation within 24-48 hours if reduction in swelling |
|
|
|
Define hydrocele.
|

cyst due to fluid accumulation in tunica vaginalis of scrotum
|
|
|
|
What is the clinical presentation of a hydrocele?
|
smooth, firm, nontender scrotal mass that transilluminates
10% of testicular tumors associated with hydrocele |
|
|
|
What is the diagnostic workup of hydrocele?
|
positive transillumination
|
|
|
|
What is the treatment for a hydrocele?
|
usually resolves spontaneously
|
|
|
|
In what patient population does a hydrocele most commonly occur?
|
infants
|
|
|

|
hydrocele
|
|
|
|
What is the ddx for testicular swelling?
|
testicular trauma
testicular torsion orchitis epididymitis hydrocele spermatocele varicocele testicular tumor hernia |
|
|

|
RT hydrocele
|
|
|
|
What is scoliosis?
|
lateral curvature of the spine associated with rotation of involved vertebrae (usually thoracic or lumbar, rarely cervical)
|
Orthopedics p158
Current Pediatrics |
|
|
What is the etiology of scoliosis?
|
if structural (i.e.fixed, fail to correct with lateral flexion) → usually idiopathic, but also congenital abnormalities, neurofibromatosis, neurologic or myopathic conditions
if non-structural (i.e. flexible, correct with lateral flexion) → compensatory mechanism secondary to leg length discrepancy, acute lumbar disc disease, or local inflammation 6x more common in females than males usually occurs between 8-13y/o infantile scoliosis may occur between 2-4y/o |
Orthopedics p158
Current Pediatrics |
|
|
What is the clinical presentation of scoliosis?
|

asymptomatic
lateral curvature of the spine assymmetry of the heights of the ribs or paravertebral muscles right thoracic curves most common |
Orthopedics p158
|
|
|
What is the diagnostic workup of scoliosis?
|

standing radiograph of the spine
|
Orthopedics p158
|
|
|
What is the management of scoliosis?
|
if nonstructural:
1. treat primary cause if structural: 1. refer to specialist 2. if <20 degrees → frequent observation 3. if >20 degrees → spinal bracing via Miwaukee brace or thoracolumbosacral orthotic 4. brace worn 23 hours per day 5. exercises performed in brace 6. if >45 degrees → surgery |
Orthopedics p158
|
|
|
What are the complications of scoliosis?
|
pain, deformity, disability, cardiopulmonary compromise
|
Orthopedics p160
|
|
|
What is the patient education for scoliosis?
|
1. spinal brace may have to be worn for >2 years
2. bracing does not eliminate curve but prevents progression 3. surgery may cause loss of spine motion 4. if >25 degree curve + pregnant → curve may increase |
Orthopedics p161
|
|
|
What is the etiology of genu varum and genu valgum in children?
|
normal variant
genu varum → normal from infancy to 2 years genu valgum → normal from 2-8 years |
|
|
|
When are genu varum and genu valgum normal?
|
genu varum → normal from infancy to 2 years
genu valgum → normal from 2-8 years |
Peds Current
|
|
|
What is the clinical presentation of genu varum and genu valgum?
|
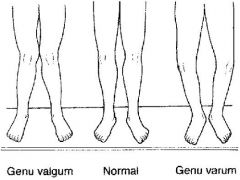
genu varum → bow-legged
genu valgum → knock-kneed |
Peds Current
|
|
|
When is the management for genu varum and genu valgum?
|
refer to orthopedist if:
bowing persists beyond 2/yo bowing increases rather than decreases bowing is unilateral knock-knees associated with short stature |
Peds Current
|
|
|
What are the complications of genu varum and genu valgum?
|
failure to straighten in appropriate time frame
genu varum → normal from infancy to 2 years genu valgum → normal from 2-8 years |
|
|

|
genu varum
|
|
|

|
genu valgum
|
|
|
|
What is the common name for talipes equinovarus?
|
clubfoot
|
|
|
|
What is the etiology of talipes equinovarus?
|
1. idiopathic (hereditary)
2. neurogenic 3. associated with a disorder (arthrogryposis, Larsen syndrome) occurs in 1:1000 live births |
Peds Current
|
|
|
What is the clinical presentation of talipes equinovarus?
|

1. plantar flexion of foot at ankle joint (equinus)
2. inversion of heel (varus) 3. medial deviation of forefoot (varus) |
Peds Current
|
|

|
talipes equinovarus
|
|
|
|
What is the management of talipes equinovarus?
|
1. immediate manipulation of foot following birth
2. splint to hold foot in correct position 3. once full correction obtained, long-term night brace 4. if resistant to manipulation and casting → surgery |
Peds Current
|
|
|
What is the etiology of metatarsus varus?
|
congenital
usually 2° to positioning in uterus |
Peds Current
|
|
|
What is the clinical presentation of metatarsus varus?
|

medial deviation of the forefoot
angulation at base of 5th metatarsal vertical crease in arch if rigid form |
Peds Current
|
|
|
What is the management of metatarsus varus?
|
if flexible → resolve spontaneously
if rigid → cast changed at intervals of 2 weeks |
Peds Current
|
|
|
What conditions are commonly associated with congenital hip dysplasia?
|
torticollis
metatarsus varus |
Peds Current
|
|
|
Define dysplasia.
|
abnormal growth or development
|
|
|
|
How do you perform the Ortolani and Barlow maneuvers?
|
place infant on back
obtain complete relaxation of infant ORTOLANI: place long finger over greater trochanter and thumb over inner side of thigh flex hips to 90° slowly abduct from midline one hip at a time attempt to lift greater trochanter forward feeling of slipping as head relocates is sign of instability BARLOW: apply pressure with thumb over inner side of thigh adduct thigh attempt to slip hip posteriorly eliciting a jerk as hip dislocates is sign of instability |
|
|
|
CONGENITAL DYSPLASIA OF THE HIP:
|

ETIOLOGY:
congenital → both acetabulum and femur underdeveloped occurs in 1:1000 live births CLINICAL PRESENTATION: abnormal relationship between proximal femur and acetabulum (dysplasia, subluxable hip, dislocatable hip, dislocated hip) Ortolani and Barlow reveal instability (signs of instability less evident after 1 m/o) if abduction limited to <90° → contracture around hip joint if knees unequal heights when hips and knees flexed → dislocated hip on side of lower knee if walking → painless limp, lurch to affected side, standing on affected leg results in dip in pelvis of opposite side d/t weakness of gluteus medius muscle (Trendelenburg sign) if bilateral dysplasia → waddling gait, widened perineum, lumbar lordosis MANAGEMENT: 1. completely reversible if corrected within first few weeks of life 2. if <4 m/o → manual reduction by flexion and abduction of hip, then pavlik harness to maintain reduction 3. if > 4m/o → traction x 2-3 weeks, then reduction under general anesthesia, then hip spica x 6 months 4. if unstable after closed reduction → open reduction 5. if older age → open reduction + correction of deformity COMPLICATIONS: if not corrected → dysplasia will be become progressive and irreversible and deformity will worsen, especially after walking age |
|
|
|
What is the etiology of tibial torsion?
|
if <16-18 months → normal variant
if persists beyond 16-18 months → sleeping with feet turned in |
Peds Current
|
|
|
What is the management of tibial torsion?
|
self-limiting → resolves by 16-18 months
if persists beyond 16-18 months → external rotation splint worn nightly |
Peds Current
|
|
|
What is the clinical presentation of tibial torsion?
|

internally rotated tibia
usually 20° sometimes accentuated by laxity of knee ligaments |
Peds Current
|
|
|
What is the clinical presentation of femoral anteversion?
|

internally rotated femur
|
Peds Current
|
|
|
What is the management of femoral anteversion?
|
returns to neutral by 6-8y/o
encourage external rotation exercises → bike riding, skating refer to orthopedist if no external rotation of hip in extension |
Peds Current
|
|
|
What are the disorders associated with "in-toeing"?
|
metatarus varus
tibial torsion femoral anteversion |
|
|
|
What does SCFE stand for?
|
slipped capital femoral epiphysis
|
|
|
|
Where does SCFE often refer?
|
knee
|
|
|
|
What is a SCFE?
|
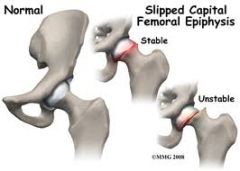
displacement of proximal femoral epiphysis
usually displaced medially and posteriorly relative to femoral neck |
PEDs Current
|
|
|
What is the etiology of a SCFE?
|
displacement of proximal femoral epiphysis d/t disruption of growth plate
cause unknown may be d/t weakness associated with hormonal changes associated with: obesity trauma hypothyroidism most common in obese adolescent males |
PEDs Current
|
|
|
What is the clinical presentation of a SCFE?
|
pain and limp
referred pain to thigh and medial knee (knee pain may be only complaint) limited internal rotation of hip stable if able to bear weight unstable if unable to bear weight |
PEDs Current
|
|
|
What is the diagnostic workup of a SCFE?
|
AP and lateral radiographs of the hip
|
PEDs Current
|
|
|
What is the management of a SCFE?
|
crutches for non-weight bearing
immediate referral to orthopedics for surgical fixation |
PEDs Current
|
|
|
What are the complications of a SCFE?
|
AVN
premature degenerative arthritis |
|
|
|
What is another name for Legg-Calves-Perthes disease?
|
avascular necrosis of proximal femur
|
|
|
|
LEGG-CALVES-PERTHES DISEASE:
|
ETIOLOGY:
idiopathic osteonecrosis of capital femoral epiphysis usually occurs between 4-8 y/o CLINICAL PRESENTATION: persistent pain in hip or groin referred mild or intermittent pain in thigh or knee atrophy of thigh 2° to disuse ↓ internal rotation and abduction limping gait MANAGEMENT: 1. radiograph of hip 2. protect hip joint and maintain normal joint motion to prevent degenerative arthritis 3. little benefit from bracing and surgery controversial COMPLICATIONS: poorer prognosis if metaphysical defects, complete involvement of femoral head, or late childhood onset |
|
|
|
What is nursemaid's elbow?
|
subluxation of radial head from annular ligament
|
PEDS Current
|
|
|
What is the etiology of nursemaid's elbow?
|
being lifted or pulled by the hand
consider abuse! |
PEDs Current
|
|
|
What is the clinical presentation of nursemaid's elbow?
|
painful fully pronated elbow
complaint that elbow will not bend radial head tenderness |
PEDs Current
|
|
|
What is the diagnostic workup of nursemaid's elbow?
|
radiographs normal
|
PEDs Current
|
|
|
What is the management of nursemaid's elbow?
|
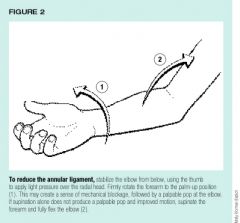
1. reduction → fully supinate arm and move from full extension to full flexion, will often hear click, and child will immediately feel better
2. sling x few days |
PEDs Current
|
|
|
What is the most common cause of septic arthritis?
|
staph aureus
|
Current p777
|
|
|
What is the diagnostic workup of septic arthritis?
|
synovial fluid:
cell count >50,000 cells/mcL differentail >90% PMNs gram stain culture BC positive in 50% of cases |
Current p777
|
|
|
SEPTIC ARTHRITIS:
|

ETIOLOGY:
source varies according to age: infant → usually d/t adjacent osteomylelitis child → usually isolated infection without bone involvement teenager → usually organism with affinity for joints (gonococcus) or underlying systemic infection organism varies with age: <4 m/o → group B strep, staph aureus 4 m/o to 4 y/o → staph aureus, h. flu (less common d/t immunizations) >4 y/o → staph aureus, staph pyogenes CLINICAL PRESENTATION: inflammatory monoarticular arthritis commonly affects knee, hip, wrist, shoulder, or ankle acute pain, swelling, warmth worsens over hours joint effusion infant → suspect if irritable, poor feeding, decreased abduction; paralysis of limb d/t inflammatory neuritis child → fever, malaise, vomiting, restriction of motion MANAGEMENT: 1. joint aspiration → WBC count >50,000 2. hospitalization and surgical drainage 3. empiric antibiotic therapy → nafcillin or oxacillin + 3rd generation cephalosporin 4. narrow-spectrum antibiotic therapy → selected based on age, gram stain, culture; 3 weeks for staph infection, 2 weeks for other infections COMPLICATIONS: if not detected before 24 hours, destruction of joint cartilage occurs, followed by arthrosis and fibrosis damage to growth plate may also occur |
|
|
|
Define torticollis.
|
stiff neck
|
|
|
|
What is the etiology of hemophilia A?
|
x-linked recessive disorder → factor VIII deficiency/inactivity; only symptomatic in males
|
|
|
|
What is the etiology of hemophilia B?
|
x-linked recessive disorder → factor IX deficiency/inactivity; only symptomatic in males
|
|
|
|
What is hemophilia A?
|
coagulation disorder characterized by factor VIII deficiency/inactivity
|
|
|
|
What is hemophilia B?
|
coagulation disorder characterized by factor IX deficiency/inactivity
|
|
|
|
What is the diagnostic work-up of hemophilia A and B?
|
PT → normal
PTT → prolonged (corrects upon mixing with normal plasma) bleeding time → normal factor VIII → deficiency if hemophilia A factor IX → deficiency if hemophilia B |
|
|
|
What is the clinical presentation of hemophilia A and B?
|
male
bruising soft-tissue bleeding hemarthrosis spontaneous bleeding involving mucous membranes, skin, joints, muscles, and viscera (if severe) trauma/surgery-associated bleeding (if mild) |
|
|
|
What are the complications of hemophilia A and B?
|
recurrent hemarthorses → arthropathy and arthritis
large intramuscular hematomas → compartment syndrome intercranial hemorrhage |
|
|
|
What is the management of hemophilia A and B?
|
1. refer to hematologist
2. if mild → intranasal or IV DDAVP 2. if severe + child → factor transfusions 2-3 x week 3. if severe + adult → factor transfusions prior to high-risk activities or during bleeding episodes 4. antifibrinolytics for mucosal bleeding 5. celecoxib for arthritis |
Current p491
|
|
|
Which is more common, hemophilia A or B?
|
hemophilia A
|
|
|
|
What is the function of von Willebrand factor?
|
1. forms complex with factor VIII to activate factor X
2. mediates platelet adhesion to extracellular matrix during clot formation |
|
|
|
What is the diagnostic work-up of von Willebrand disease?
|
PT → normal
PTT → prolonged bleeding time → prolonged von willebrand factor → deficiency (though type 2N resembles hemophilia A) |
|
|
|
What is the etiology of von Willebrand disease?
|
autosomal dominant disorder → von Willebrand factor deficiency
|
|
|
|
What is von Willebrand disease?
|
coagulation disorder characterized by von Willebrand factor deficiency
|
|
|
|
What is the clinical presentation of von Willebrand disease?
|
easy bruising and epistaxis from early childhood
menorrhagia prolonged bleeding following trauma/surgery |
|
|
|
What is the management of von Willebrand disease?
|
1. if mild → desmopressin acetate
2. if severe → vWF-containing factor VIII transfusions 3. antifibrinolytics for mucosal bleeding 4. estrogen-containing contraceptives for menorrhagia 5. avoid aspirin and NSAIDs |
|
|
|
What is aplastic anemia?
|
failure of bone marrow to produce RBCs, WBCs, or platelets
|
|
|
|
What is the etiology of aplastic anemia?
|
either direct stem cell injury or autoimmune disease mediated by T-cells or IgG Ab against stem cells; usually autoimmune
|
|
|
|
What is the ddx for aplastic anemia?
|
idiopathic → probably autoimmune
congenital → rare pregnancy posthepatitis paroxysmal nocturnal hemoglobinuria SLE toxins → benzene, toluene, insecticides medications → phenytoin, carbamazepine, sulfonamides, chloramphenicol, pehnylbutazone, gold salts, quinacrine, tolbutamide chemotherapy radiation |
Current p454
|
|
|
What is the clinical presentation of aplastic anemia?
|
anemia → fatigue, weakness, pallor
neutropenia → bacterial infection thrombocytopenia → skin and mucosal bleeding, petechiae, purpura *hepatosplenomegaly, lymphadenopathy, and bone tenderness should NOT be present |
Current p454
|
|
|
What is the diagnostic work-up of aplastic anemia?
|
CBC → pancytopenia
RETIC → low blood smear → normal morphology bone marrow biopsy → hypocellular, normal morphology |
Current p454
|
|
|
What is the management of aplastic anemia?
|
1. if mild, supportive care as necessary → RBC and platelet transfusions, antibiotics
2. if severe + <50y/o → bone marrow transplant from HLA-matched sibling donor 3. if severe + >50y/o or no HLA-matched sibling donor → ATG + cyclosporine |
Current p455
|
|
|
What is the prognosis for aplastic anemia?
|
1. if severe and untreated → 3 months to live
2. if bone marrow transplant → 80% success rate 3. if ATG → 60% success rate; improvement within 4-12 weeks; usually only partial response |
Current p455
|
|
|
What bone tumor presents at the diaphysis?
|
Ewing's sarcoma
|
Orthopedics p448
|
|
|
Sickle cell anemia imparts resistance to what disease?
|
malaria
|
|
|
|
SICKLE CELL ANEMIA:
|
ETIOLOGY:
homozygous genetic disorder characterized by hemoglobin S (instead of hemoglobin A) common in African, Mediterranean, Middle Eastern, Indian, or Caribbean CLINICAL PRESENTATION: fatigue, pallor, jaundice dactylitis, recurrent abdominal or musculoskeletal pain gallstones, splenomegaly in early childhood with later disappearance DIAGNOSTIC WORKUP: NBS CBC → normocytic or macrocytic anemia peripheral blood smear → sickle cells, target cells (hemolytic anemia) ↑ RETIC hemoglobin electrophoresis MANAGEMENT: education program prophylactic penicillin started at 2m/o and continued until at least 5y/o immunizations if illness with fever >38.5°C → BC, IV broad-spectrum antibiotics, observation if vaso-occlusive episode → maintain adequate analgesia, hydration, and oxygen saturation; correct acidosis; treat infections if acute severe exacerbation of anemia (splenic sequestration, aplastic crisis), acute severe vaso-occlusive episode (acute severe chest syndrome, stroke, organ failure), high-risk procedures, surgery → packed RBCs *acute chest syndrome = fever, pleuritic chest pain, pulmonary infiltrates with hypoxemia caused by pulmonary infection, infarction, or fat embolism from ischemic bone marrow hydroxyurea PROGNOSIS: early identification and prophylactic penicillin allow children to live into adulthood but end-organ damage d/t vaso-occlusion invariably occurs |
|
|

|
bone destruction + sunburst pattern → osteosarcoma (of proximal fibula)
|
|
|
|
What is immune thrombocytopenic purpura (ITP)?
|
autoimmune disorder characterized by low platelet count
|
Current p482
|
|
|
What is the etiology of ITP?
|
autoimmune disease → antibodies bind platelets → accelerated platelet clearance; usually primary and idiopathic
often follows infection with viruses, such as rubella, varicella, measles, parvovirus, influenza, or EBV usually occurs in children 2-5y/o |
Current p482
|
|

|
Ewing's sarcoma (of femur)
|
|
|
|
What is the clinical presentation of ITP?
|
petechiae, ecchymosis
epistaxis |
Current p482
|
|
|
What is the diagnostic work-up of ITP?
|
CBC → anemia if bleeding, thrombocytopenia (marked reduced, usually <50,000)
PT → normal PTT → normal bleeding time → prolonged HepC HIV |
Current p482
|
|
|
What is the management of ITP?
|
1. refer to specialist
2. d/c offending medications (aspirin) 3. if mild → observe, wear helmet, avoid contact sports 5. if platelet count <10,000/mcL or significant bleeding → corticosteroids + IV immunoglobulin 6. if hemorrhage → platelet transfusion 7. splenectomy after 5y/o |
Current p483
|
|
|
What are the complicatons of ITP?
|
intercranial hemorrhage
|
Pathology p83
|
|
|
What is the prognosis of ITP?
|
90% of children have spontaneous remission
relapse common for adults |
Current p483
Current Peds |
|
|
What is the ddx for ITP?
|
primary:
idiopathic secondary: hepatitis C HIV lupus lymphoma medications |
Current p482
|
|
|
What does ITP stand for?
|
immune thrombocytopenic purpura
|
|
|
|
What patient population is most commonly affected by osteosarcoma and Ewing's sarcoma?
|
boys during puperty
affects boys > girls rarely affects adults |
Orthopedics p357
|
|
|
What is osteosarcoma?
|
1° malignant bone tumor characterized by malignant tumor cells that produce osteoid or bone
|
Orthopedics p386, 448
|
|
|
What is Ewing's sarcoma?
|
malignant tumor of unknown histogenesis
|
Orthopedics p448
|
|
|
What is the clinical presentation of Ewing's sarcoma?
|
10-15 y/o
diaphysis of long bone bone pain sometimes painful soft tissue mass with increased warmth lethargy, fever, weight loss |
Orthopedics p448
|
|
|
What is the diagnostic workup of Ewing's sarcoma?
|
radiograph → mottled irregular destructive changes with periosteal new bone formation → "onion skin" appearance
|
Orthopedics p449
|
|
|
What is the diagnostic workup of osteosarcoma?
|
radiograph →
1. blastic (dense), lytic (lucent) or mixed 2. sunburst pattern due to periosteal reaction 3. poorly defined margins |
Orthopedics p449
|
|
|
What is the management for Ewing's sarcoma?
|
1. refer to orthopedic specialist
2. local resection, radiation, chemotherapy |
Orthopedics p449
|
|
|
Where do osteosarcomas most commonly occur?
|
75% occur in distal metaphysis of femur
|
Orthopedics p386
|
|
|
What is the management of osteosarcoma?
|
wide resection, local radiation, chemotherapy
|
|
|
|
What is the clinical presentation of osteosarcoma?
|
pain or swelling in a bone or joint, especially around knee
may mimic sports injury |
|
|
|
What is the prognosis of osteosarcoma and Ewing's sarcoma?
|
osteosarcoma = 60% 5-year survival rate
Ewing's sarcoma = 50% mortality rate |
|
|
|
What are the risk factors for Wilm's tumor (nephroblastoma)?
|
<10y/o
|
|
|
|
What is the clinical presentation of Wilm's tumor?
|

abdominal swelling or mass
|
|
|
|
What is the diagnostic workup of Wilm's tumor?
|
CBC, CMP, PT/PTT, UA
US or CT CXR |
|
|
|
What is the management of Wilm's tumor?
|
nephrectomy
chemotherapy |
|
|
|
What is the pattern of metastasis for Wilm's tumor?
|
lung (80-85%)
liver (15%) |
|
|
|
WILM'S TUMOR:
|
ETIOLOGY:
usually idiopathic sometimes associated with malformations or syndromes most common between 2-5y/o, unusual after 6y/o CLINICAL PRESENTATION: asymptomatic abdominal swelling or mass (smooth, firm, well demarcated, rarely crosses midline, may extend to pelvis) fever, HTN DIAGNOSTIC WORKUP: UA → +/- hematuria, leukocytes US for abdominal mass CXR for metastasis MANAGEMENT: surgery for biopsy and resection radiation and chemotherapy depending on stage PROGNOSIS: 90% cure rate |
|
|
|
ACUTE LYMPHOBLASTIC LEUKEMIA
|
ETIOLOGY:
uncontrolled proliferation of immature lymphocytes cause unknown most common childhood malignancy, peak 4y/o 14-fold increased risk if Down’s syndrome CLINICAL PRESENTATION: intermittent fever, pallor, petechiae, purpura, bone pain (vertebra, pelvis, legs) hepatosplenomegaly lymphadenopathy DIAGNOSTIC WORKUP: anemia, neutropenia, leukopenia or leukocytosis, thrombocytopenia peripheral blood smear → teardrop RBCs, lymphoblasts bone marrow aspirate or biopsy → >25% lymphoblasts MANAGEMENT: 1st phase = induction during 1st month of therapy with predinisone 2nd phase = consolidation for several months with chemotherapy + continued prednisone 3rd phase = maintenance therapy bone-marrow transplant if refractory to chemotherapy PROGNOSIS: dependent on features at diagnosis and response to therapy |
|
|
|
ACUTE MYELOID LEUKEMIA:
|
ETIOLOGY:
CLINICAL PRESENTATION: fatigue, bleeding, infection hepatosplenomegaly, adenopathy, skin nodules leukocytosis may cause venous stasis and occlusion leading to hypoxia, hemorrhage and infarction DIAGNOSTIC WORKUP: anemia, neutropenia, hyperleukocytosis, thrombocytopenia bone marrow aspirate or biopsy → >20% leukemic blasts MANAGEMENT: induction, chemotherapy, stem cell transplant less responsive than ALL PROGNOSIS: 75-85% complete remission rate 50-60% 5-year survival rate without stem cell transplant, otherwise 60-70% |
|
|
|
What type of disease is mumps?
|
parotitis
|
|
|
|
What is the etiology of mumps?
|
caused by a paramyxovirus; spread via respiratory droplets; usually affects unimmunized children
|
Current p1250
|
|
|
What is the clinical presentation of mumps?
|

incubation 2-3 weeks before onset
fatigue and fever → variable parotid gland enlargement → unilateral or bilateral, usually one enlarges before the other stenson's duct → erythematous, edematous with yellow secretions parotid tenderness facial edema +/- trismus +/- submaxillary and sublingual gland involvement |
Current p1250
|
|
|
What is the diagnostic work-up of mumps?
|
usually diagnosed clinically; swab parotid duct for confirmation via NAAT (more sensitive), viral culture or serum IgM
|
Current p1250
|
|
|
What are the complications of mumps?
|
pancreatitis →affects children; upper abdominal pain, nausea, vomiting
orchitis → affects 25-40% postpubertal men, high fever, testicular swelling and tenderness oophoritis → affects 5% of postpubertal women, lower abdominal pain, ovarian enlargement meningitis → high fever, headache, stiff neck, lethargy rarely nerve deafness, myocarditis, facial paralysis, transvere myelitis, hydrocephalus, aquaductal stenosis |
Current p1250
Current Peds |
|
|
Mumps is the most common cause of what disease in children?
|
pancreatitis
|
Current p1250
|
|
|
What is the management of mumps?
|
Symptomatic:
1. analgesics 2. fluids 3. topical compresses 4. bed rest until afebrile 5. isolation until swelling subsides infectious 1-2 days prior to onset of symptoms and 5 days afterward |
Current p1250
|
|
|
What is the prevention of rubeola, mumps, rubella, and varicella?
|
MMRV vaccine at 12-15 months and 4-6 years
|
Current 1249
|
|
|
What is the prevention of rubeola, mumps, rubella, and varicella?
|
MMRV vaccine at 12-15 months and 4-6 years
|
Current 1249
|
|
|
What is herpangina?
|
viral infection of the mouth
|
|
|
|
What is the etiology of herpangina?
|
caused by coxsackieviruses; spread via respiratory droplets or fecal-oral; usually affects infants and young children in summer
|
|
|
|
What is the clinical presentation of herpangina?
|

high fever; sore throat, dysphagia, and loss of appetite; red macules → vesicles → ulcerations with white-grey base and red border, located on soft palate or tonsillar pillars
|
|
|
|
What is the management and patient eduction for herpangina?
|
1. self-limiting → usually resoves in 1 week
2. take acetominophen or ibuprofen for fever and discomfort (avoid aspirin) 3. increase fluids 4. eat cold non-irritating diet → milk, icecream, popsicles 5. avoid citrus, fried, spicy, and hot food |
|
|
|
What is the prevention for herpangina?
|
handwashing
|
|
|
|
How do you differentiate oral candidiasis from oral leukoplakia?
|
candidiasis will wipe off (and bleed when scraped) while leukoplakia will not
|
|
|
|
What is oral candidiasis?
|
yeast infection of the mouth
|
|
|
|
What is the etiology of oral candidiasis?
|
caused by yeast Candida albicans; commonly associated with dentures, dibilitation, anemia, DM, HIV, broad-spectrum antibiotics, corticosteroids, chemotherapy, radiation therapy
|
|
|
|
What is the clinical presentation of oral candidiasis?
|

white curd-like patches overlying erythematous mucosa; painful; removable
*angular cheilitis is another manifestation of candidiasis |
|
|
|
What is the diagnostic workup of oral candidiasis?
|

1. KOH → reveals pseudohyphae
2. HIV if no other explainable cause |
|
|
|
What is the management of oral candidiasis?
|
1. prescribe antifungal, either fluconazole 100mg/d x 7-14 days, ketoconazole 200-400mg/d x 7-14 days (take with breakfast), clotrimazole troches, nystatin vaginal troches, or mouth rinses
2. for local relief, half-strength hydrogen peroxide mouth rinses or 0.12% chlorhexidine 3. if dentures, prescribe nystatin powder applied to dentures 3-4x daily x several weeks 4. if HIV, prescribe longer course of antifungal 3. if refractory, prescribe itraconazole 200mg PO daily |
|
|
|
What are the criteria for a febrile seizure?
|
1. age 3 m/o to 6 y/o (most common between 6-18 months)
2. fever > 38.8°C 3. non-CNS infection |
|
|
|
What are the most common causes of febrile seizures?
|
usually acute respiratory illness
sometimes gastroenteritis (Shigella, Campylobacter), UTI rarely roseola infantum, immunizations |
|
|
|
FEBRILE SEIZURES:
|
ETIOLOGY:
Criteria: 1. age 3 m/o to 6 y/o (most common between 6-18 months) 2. fever > 38.8°C 3. non-CNS infection Causes: usually d/t acute respiratory illnesses sometimes d/t gastroenteritis (Shigella, Campylobacter), UTI rarely d/t Roseola infantum (classic cause), immunizations occur in 2-3% of children CLINICAL PRESENTATION: 90% generalized, last <5 min, occur early in illness causing fever DIAGNOSTIC WORKUP: evaluate for source of fever and R/O CNS infection (meningitis, encephalitis) CBCDP and BC LP → if child < 18 months (since signs unreliable), cause of fever not found, close F/U not possible, or recovery slow (negative finding does not R/O emerging CNS infection) MANAGEMENT: 1. find source of fever and treat appropriately 2. measures to control fever (tepid baths, antipyretics, antibiotics) are reasonable but unproven to prevent recurrent febrile seizures 3. if complicated seizure or medical reassurance fails to relieve family anxiety → anticonvulsant prophylaxis (phenobarbital, valproic acid) PATIENT EDUCATION: 1. recurrent febrile seizures occur in 30-50% of cases → expect more seizures 2. simple febrile seizures do not have any long-term adverse outcomes 3. complex febrile seizures may rarely lead to epilepsy (occur in 1-3%; risk increased 2-5 times; risk higher if complex features such as longer than 15 minutes, more than 1 seizure daily, focal features; risk higher if abnormal neurologic status preceding seizure, onset before age 1, FH of epilepsy) |
|
|
|
PKU is highly sensitive when testing infants at least _ hours old?
|
24
|
Interpreting Laboratory Data p.4
|
|
|
At what age should repeat PKU testing be performed?
|
10-14 days
|
|
|
|
What tests are in PKU for Washington state?
|
Congenital Adrenal Hyperplasia (CAH)
Hemoglobinopathy Biotinidase Galactosemia CH(Thyroid) Cystic Fibrosis Amino Acid Organic Acid Fatty Acid |
Antrim
|
|
|
What is phenylketonuria?
|
autosomal recessive genetic disorder of amino acid metabolism
characterized by an inability to breakdown the amino acid phenylalanine into tyrosine d/t absence/deficiency of phenylalanine hydroxylase phenylalaline and related substances accumulate and result in mental retardation treated with diet low in phenylalanine |
|
|
|
What is galactosemia?
|
autosomal recessive genetic disorder characterized by an inability to breakdown galactose d/t a deficiency in either:
1. galactose-1 phosphate uridyl transferase (classic) 2. galactose kinase 3. galactose-6-phosphate epimerase galactose builds up and may result in eye, liver, kidney and brain damage treatment is to avoid milk and other foods containing galactose + calcium supplementation |
|
|
|
What is the clinical presentation of PKU?
|
hyperactivity
light complexion, eczema seizures, mental retardation |
|
|
|
What is the clinical presentatio of galactosemia?
|
if given lactose → vomiting, jaundice (indirect and direct), hepatomegaly, liver insufficiency
if untreated → cataracts (reversible if treated), hepatic cirrhosis, renal Fanconi syndrome, death within a month (usually d/t sepsis with E. coli) even if treated → often delayed apraxic speech (can’t say what want to say), ovarian failure; less often developmental delay, tremor, ataxia (gross lack of motor coordination), mental retardation |
|
|
|
What is the clinical presentation of congenital hypothyroidism?
|
usually appear normal at birth, gain weight normally during first few months of life
may have jaundice, dry skin, large fontanels, thick tongue, hoarseness, umbilical hernia, hypotonia, mental retardation |
|
|
|
What is the clinical presentation of congenital hypoglycemia?
|
may be asymptomatic or symptoms may be difficult to detect
lethargy, apathy, limpness, high-pitched crying, refusal to eat, hypothermia, cyanosis, irregular breathing or apnea, tremors, seizures |
|
|
|
How do you convert lbs to kg?
|
lbs/2.2 = kg
|
|
|
|
How do you calculate a pediatric dosage of a given medication based on weight (lbs or kg)?
|
pediatric doses usually available as mg/kg/dose or mg/kg/day
if no pediatric dosing available: 1. Clark's Rule for 2-17y/o: pediatric dose = adult dose x [weight (kg)/70] pediatric dose = adult dose x [weight (lb)/150] 2. Fried's Rule for <2y/o: pediatric dose = adult dose x [age (months)/150] |
|
|
|
Define pharmacokinetics.
|
what the body does to a drug
A = absorption D = distribution M = metabolism E = elimination |
|
|
|
Define pharmacodynamics.
|
what a drug does to the body
|
|
|
|
List medications that are contraindicated in children.
|
aspirin/salicylates (d/t potential Reye's syndrome)
tetracyclines (d/t potential discoloration of teeth enamel) sulfonamides (d/t potential kernicterus) ceftriaxone (3rd generation cephalosporin; d/t potential kernicterus) ciprofloxacin (2nd generation fluoroquinolone; d/t potential tendon and ligament rupture) chloramphenicol (d/t potential grey baby syndrome) benzoalcohol (d/t potential gasping syndrome) use caution with SSRIs (d/t increased risk of suicide) |
|
|
|
What is scoliosis?
|
lateral curvature of the spine associated with rotation of involved vertebrae (usually thoracic or lumbar, rarely cervical)
|
Orthopedics p158
Current Pediatrics |
|
|
What is scoliosis?
|
lateral curvature of the spine associated with rotation of involved vertebrae (usually thoracic or lumbar, rarely cervical)
|
Orthopedics p158
Current Pediatrics |
|
|
Define subluxation.
|
partial dislocation
|
|
|
|
Define subluxation.
|
partial dislocation
|
|
|
|
What is the etiology of scoliosis?
|
if structural (i.e.fixed, fail to correct with lateral flexion) → usually idiopathic, but also congenital abnormalities, neurofibromatosis, neurologic or myopathic conditions
if non-structural (i.e. flexible, correct with lateral flexion) → compensatory mechanism secondary to leg length discrepancy, acute lumbar disc disease, or local inflammation 6x more common in females than males usually occurs between 8-13y/o infantile scoliosis may occur between 2-4y/o |
Orthopedics p158
Current Pediatrics |
|
|
What is the etiology of scoliosis?
|
if structural (i.e.fixed, fail to correct with lateral flexion) → usually idiopathic, but also congenital abnormalities, neurofibromatosis, neurologic or myopathic conditions
if non-structural (i.e. flexible, correct with lateral flexion) → compensatory mechanism secondary to leg length discrepancy, acute lumbar disc disease, or local inflammation 6x more common in females than males usually occurs between 8-13y/o infantile scoliosis may occur between 2-4y/o |
Orthopedics p158
Current Pediatrics |
|
|
Define paresthesia.
|
abnormal sensation such as tingling, prickling, burning
|
|
|
|
Define paresthesia.
|
abnormal sensation such as tingling, prickling, burning
|
|
|
|
What is the clinical presentation of scoliosis?
|

asymptomatic
lateral curvature of the spine assymmetry of the heights of the ribs or paravertebral muscles right thoracic curves most common |
Orthopedics p158
|
|
|
What is the clinical presentation of scoliosis?
|

asymptomatic
lateral curvature of the spine assymmetry of the heights of the ribs or paravertebral muscles right thoracic curves most common |
Orthopedics p158
|
|
|
Define dislocation.
|
complete separation of the surfaces of a joint
|
|
|
|
Define dislocation.
|
complete separation of the surfaces of a joint
|
|
|
|
What is the diagnostic workup of scoliosis?
|

standing radiograph of the spine
|
Orthopedics p158
|
|
|
What is the diagnostic workup of scoliosis?
|

standing radiograph of the spine
|
Orthopedics p158
|
|
|
Define strain.
|
injury to muscle or tendon
|
|
|
|
Define strain.
|
injury to muscle or tendon
|
|
|
|
What is the management of scoliosis?
|
if nonstructural:
1. treat primary cause if structural: 1. refer to specialist 2. if <20 degrees → frequent observation 3. if >20 degrees → spinal bracing via Miwaukee brace or thoracolumbosacral orthotic 4. brace worn 23 hours per day 5. exercises performed in brace 6. if >45 degrees → surgery |
Orthopedics p158
|
|
|
What is the management of scoliosis?
|
if nonstructural:
1. treat primary cause if structural: 1. refer to specialist 2. if <20 degrees → frequent observation 3. if >20 degrees → spinal bracing via Miwaukee brace or thoracolumbosacral orthotic 4. brace worn 23 hours per day 5. exercises performed in brace 6. if >45 degrees → surgery |
Orthopedics p158
|
|
|
Define sprain.
|
injury to ligament
|
|
|
|
Define sprain.
|
injury to ligament
|
|
|
|
What are the complications of scoliosis?
|
pain, deformity, disability, cardiopulmonary compromise
|
Orthopedics p160
|
|
|
What are the complications of scoliosis?
|
pain, deformity, disability, cardiopulmonary compromise
|
Orthopedics p160
|
|
|
Define gibbus deformity.
|
extreme kyphosis, hump, or hunch
posterior spinal deformity in which there is a sharply angulated segment |
Stedmans
|
|
|
Define gibbus deformity.
|
extreme kyphosis, hump, or hunch
posterior spinal deformity in which there is a sharply angulated segment |
Stedmans
|
|
|
What is the patient education for scoliosis?
|
1. spinal brace may have to be worn for >2 years
2. bracing does not eliminate curve but prevents progression 3. surgery may cause loss of spine motion 4. if >25 degree curve + pregnant → curve may increase |
Orthopedics p161
|
|
|
What is the patient education for scoliosis?
|
1. spinal brace may have to be worn for >2 years
2. bracing does not eliminate curve but prevents progression 3. surgery may cause loss of spine motion 4. if >25 degree curve + pregnant → curve may increase |
Orthopedics p161
|
|
|
Define arthroplasty.
|
surgery to restore integrity and function of a joint or to create an artificial joint
|
Stedmans
|
|
|
Define arthroplasty.
|
surgery to restore integrity and function of a joint or to create an artificial joint
|
Stedmans
|
|
|
What is the etiology of genu varum and genu valgum in children?
|
normal variant
genu varum → normal from infancy to 2 years genu valgum → normal from 2-8 years |
|
|
|
What is the etiology of genu varum and genu valgum in children?
|
normal variant
genu varum → normal from infancy to 2 years genu valgum → normal from 2-8 years |
|
|
|
Define arthrodesis.
|
surgical stiffening of a joint to reduce pain that cannot be managed by other means; pain often caused by fracture or arthritis
|
Stedmans
Wikipedia |
|
|
Define arthrodesis.
|
surgical stiffening of a joint to reduce pain that cannot be managed by other means; pain often caused by fracture or arthritis
|
Stedmans
Wikipedia |
|
|
When are genu varum and genu valgum normal?
|
genu varum → normal from infancy to 2 years
genu valgum → normal from 2-8 years |
Peds Current
|
|
|
When are genu varum and genu valgum normal?
|
genu varum → normal from infancy to 2 years
genu valgum → normal from 2-8 years |
Peds Current
|
|
|
Define radiculopathy.
|
disorder of spinal nerve roots
|
Stedmans
|
|
|
Define radiculopathy.
|
disorder of spinal nerve roots
|
Stedmans
|
|
|
What is the clinical presentation of genu varum and genu valgum?
|

genu varum → bow-legged
genu valgum → knock-kneed |
Peds Current
|
|
|
What is the clinical presentation of genu varum and genu valgum?
|

genu varum → bow-legged
genu valgum → knock-kneed |
Peds Current
|
|
|
What are other names for physis?
|
epiphyseal plate
growth plate |
|
|
|
What are other names for physis?
|
epiphyseal plate
growth plate |
|
|
|
When is the management for genu varum and genu valgum?
|
refer to orthopedist if:
bowing persists beyond 2/yo bowing increases rather than decreases bowing is unilateral knock-knees associated with short stature |
Peds Current
|
|
|
When is the management for genu varum and genu valgum?
|
refer to orthopedist if:
bowing persists beyond 2/yo bowing increases rather than decreases bowing is unilateral knock-knees associated with short stature |
Peds Current
|
|
|
What is the function of the epiphysis.
|
primary growth center of a bone
|
|
|
|
What is the function of the epiphysis.
|
primary growth center of a bone
|
|
|
|
What are the complications of genu varum and genu valgum?
|
failure to straighten in appropriate time frame
genu varum → normal from infancy to 2 years genu valgum → normal from 2-8 years |
|
|
|
What are the complications of genu varum and genu valgum?
|
failure to straighten in appropriate time frame
genu varum → normal from infancy to 2 years genu valgum → normal from 2-8 years |
|
|
|

|
|
|
|
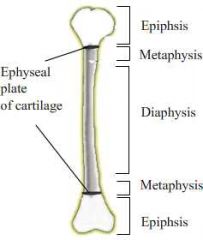
|
|
|

|
genu varum
|
|
|

|
genu varum
|
|
|

|

|
|
|

|

|
|
|

|
genu valgum
|
|
|

|
genu valgum
|
|
|
|
What should you consider when ordering radiographs?
|
1. always order orthagonal view → diagnosis should be never be made based on one view
2. comparison view of opposite side helpful, especially in pediatrics 3. if radiograph normal, but high clinical suspicion, have patient return in 7-10 days for repeated films |
Orthopedics p343
|
|
|
What should you consider when ordering radiographs?
|
1. always order orthagonal view → diagnosis should be never be made based on one view
2. comparison view of opposite side helpful, especially in pediatrics 3. if radiograph normal, but high clinical suspicion, have patient return in 7-10 days for repeated films |
Orthopedics p343
|
|
|
What is the common name for talipes equinovarus?
|
clubfoot
|
|
|
|
What is the common name for talipes equinovarus?
|
clubfoot
|
|
|
|
Define open fracture.
|
fracture where skin pierced
|
|
|
|
Define open fracture.
|
fracture where skin pierced
|
|
|
|
What is the etiology of talipes equinovarus?
|
1. idiopathic (hereditary)
2. neurogenic 3. associated with a disorder (arthrogryposis, Larsen syndrome) occurs in 1:1000 live births |
Peds Current
|
|
|
What is the etiology of talipes equinovarus?
|
1. idiopathic (hereditary)
2. neurogenic 3. associated with a disorder (arthrogryposis, Larsen syndrome) occurs in 1:1000 live births |
Peds Current
|
|
|
Define closed fracture.
|
fracture where skin intact
|
|
|
|
Define closed fracture.
|
fracture where skin intact
|
|
|
|
What is the clinical presentation of talipes equinovarus?
|

1. plantar flexion of foot at ankle joint (equinus)
2. inversion of heel (varus) 3. medial deviation of forefoot (varus) |
Peds Current
|
|
|
What is the clinical presentation of talipes equinovarus?
|

1. plantar flexion of foot at ankle joint (equinus)
2. inversion of heel (varus) 3. medial deviation of forefoot (varus) |
Peds Current
|
|
|
What is another name for open fracture?
|
compound fracture
|
|
|
|
What is another name for open fracture?
|
compound fracture
|
|
|

|
talipes equinovarus
|
|
|

|
talipes equinovarus
|
|
|
|
Define comminuted fracture.
|
fracture characterized by multiple breaks
|
|
|
|
Define comminuted fracture.
|
fracture characterized by multiple breaks
|
|
|
|
What is the management of talipes equinovarus?
|
1. immediate manipulation of foot following birth
2. splint to hold foot in correct position 3. once full correction obtained, long-term night brace 4. if resistant to manipulation and casting → surgery |
Peds Current
|
|
|
What is the management of talipes equinovarus?
|
1. immediate manipulation of foot following birth
2. splint to hold foot in correct position 3. once full correction obtained, long-term night brace 4. if resistant to manipulation and casting → surgery |
Peds Current
|
|
|
What should you consider when assessing a fracture?
|
open vs closed
incomplete (stress, greenstick, torus) vs complete (transverse, oblique, spiral, avulsion) simple vs comminuted angulation rotation displacement |
|
|
|
What should you consider when assessing a fracture?
|
open vs closed
incomplete (stress, greenstick, torus) vs complete (transverse, oblique, spiral, avulsion) simple vs comminuted angulation rotation displacement |
|
|
|
What is the etiology of metatarsus varus?
|
congenital
usually 2° to positioning in uterus |
Peds Current
|
|
|
What is the etiology of metatarsus varus?
|
congenital
usually 2° to positioning in uterus |
Peds Current
|
|
|
Define occult fracture.
|
clinical signs of fracture but no radiographic evidence → new bone growth evident on radiographs within 2-4 weeks
|
|
|
|
Define occult fracture.
|
clinical signs of fracture but no radiographic evidence → new bone growth evident on radiographs within 2-4 weeks
|
|
|
|
What is the clinical presentation of metatarsus varus?
|
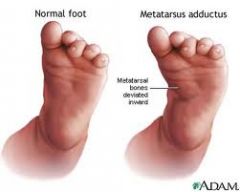
medial deviation of the forefoot
angulation at base of 5th metatarsal vertical crease in arch if rigid form |
Peds Current
|
|
|
What is the clinical presentation of metatarsus varus?
|

medial deviation of the forefoot
angulation at base of 5th metatarsal vertical crease in arch if rigid form |
Peds Current
|
|

|

|
|
|

|
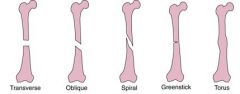
|
|
|
|
What is the management of metatarsus varus?
|
if flexible → resolve spontaneously
if rigid → cast changed at intervals of 2 weeks |
Peds Current
|
|
|
What is the management of metatarsus varus?
|
if flexible → resolve spontaneously
if rigid → cast changed at intervals of 2 weeks |
Peds Current
|
|
|
What is another name for stress fracture?
|
hairline fracture
|
|
|
|
What is another name for stress fracture?
|
hairline fracture
|
|
|
|
What conditions are commonly associated with congenital hip dysplasia?
|
torticollis
metatarsus varus |
Peds Current
|
|
|
What conditions are commonly associated with congenital hip dysplasia?
|
torticollis
metatarsus varus |
Peds Current
|
|
|
Define stress fracture.
|
type of incomplete fracture characterized by small crack in bone
|
|
|
|
Define stress fracture.
|
type of incomplete fracture characterized by small crack in bone
|
|
|
|
Define dysplasia.
|
abnormal growth or development
|
|
|
|
Define dysplasia.
|
abnormal growth or development
|
|
|
|
What is the most common cause of stress fracture?
|
sports injury
|
|
|
|
What is the most common cause of stress fracture?
|
sports injury
|
|
|
|
How do you perform the Ortolani and Barlow maneuvers?
|
place infant on back
obtain complete relaxation of infant ORTOLANI: place long finger over greater trochanter and thumb over inner side of thigh flex hips to 90° slowly abduct from midline one hip at a time attempt to lift greater trochanter forward feeling of slipping as head relocates is sign of instability BARLOW: apply pressure with thumb over inner side of thigh adduct thigh attempt to slip hip posteriorly eliciting a jerk as hip dislocates is sign of instability |
|
|
|
How do you perform the Ortolani and Barlow maneuvers?
|
place infant on back
obtain complete relaxation of infant ORTOLANI: place long finger over greater trochanter and thumb over inner side of thigh flex hips to 90° slowly abduct from midline one hip at a time attempt to lift greater trochanter forward feeling of slipping as head relocates is sign of instability BARLOW: apply pressure with thumb over inner side of thigh adduct thigh attempt to slip hip posteriorly eliciting a jerk as hip dislocates is sign of instability |
|
|

|
comminuted fracture (of tibia and fibula)
|
|
|

|
comminuted fracture (of tibia and fibula)
|
|
|
|
CONGENITAL DYSPLASIA OF THE HIP:
|

ETIOLOGY:
congenital → both acetabulum and femur underdeveloped occurs in 1:1000 live births CLINICAL PRESENTATION: abnormal relationship between proximal femur and acetabulum (dysplasia, subluxable hip, dislocatable hip, dislocated hip) Ortolani and Barlow reveal instability (signs of instability less evident after 1 m/o) if abduction limited to <90° → contracture around hip joint if knees unequal heights when hips and knees flexed → dislocated hip on side of lower knee if walking → painless limp, lurch to affected side, standing on affected leg results in dip in pelvis of opposite side d/t weakness of gluteus medius muscle (Trendelenburg sign) if bilateral dysplasia → waddling gait, widened perineum, lumbar lordosis MANAGEMENT: 1. completely reversible if corrected within first few weeks of life 2. if <4 m/o → manual reduction by flexion and abduction of hip, then pavlik harness to maintain reduction 3. if > 4m/o → traction x 2-3 weeks, then reduction under general anesthesia, then hip spica x 6 months 4. if unstable after closed reduction → open reduction 5. if older age → open reduction + correction of deformity COMPLICATIONS: if not corrected → dysplasia will be become progressive and irreversible and deformity will worsen, especially after walking age |
|
|
|
CONGENITAL DYSPLASIA OF THE HIP:
|

ETIOLOGY:
congenital → both acetabulum and femur underdeveloped occurs in 1:1000 live births CLINICAL PRESENTATION: abnormal relationship between proximal femur and acetabulum (dysplasia, subluxable hip, dislocatable hip, dislocated hip) Ortolani and Barlow reveal instability (signs of instability less evident after 1 m/o) if abduction limited to <90° → contracture around hip joint if knees unequal heights when hips and knees flexed → dislocated hip on side of lower knee if walking → painless limp, lurch to affected side, standing on affected leg results in dip in pelvis of opposite side d/t weakness of gluteus medius muscle (Trendelenburg sign) if bilateral dysplasia → waddling gait, widened perineum, lumbar lordosis MANAGEMENT: 1. completely reversible if corrected within first few weeks of life 2. if <4 m/o → manual reduction by flexion and abduction of hip, then pavlik harness to maintain reduction 3. if > 4m/o → traction x 2-3 weeks, then reduction under general anesthesia, then hip spica x 6 months 4. if unstable after closed reduction → open reduction 5. if older age → open reduction + correction of deformity COMPLICATIONS: if not corrected → dysplasia will be become progressive and irreversible and deformity will worsen, especially after walking age |
|
|
|
Define simple fracture.
|
fracture characterized by single break
|
|
|
|
Define simple fracture.
|
fracture characterized by single break
|
|
|
|
What is the etiology of tibial torsion?
|
if <16-18 months → normal variant
if persists beyond 16-18 months → sleeping with feet turned in |
Peds Current
|
|
|
What is the etiology of tibial torsion?
|
if <16-18 months → normal variant
if persists beyond 16-18 months → sleeping with feet turned in |
Peds Current
|
|
|
What is another name for torus fracture?
|
buckle fracture
|
|
|
|
What is another name for torus fracture?
|
buckle fracture
|
|
|
|
What is the management of tibial torsion?
|
self-limiting → resolves by 16-18 months
if persists beyond 16-18 months → external rotation splint worn nightly |
Peds Current
|
|
|
What is the management of tibial torsion?
|
self-limiting → resolves by 16-18 months
if persists beyond 16-18 months → external rotation splint worn nightly |
Peds Current
|
|
|
Define pathologic fracture.
|
fracture due to weakened bone caused by underlying condition
|
|
|
|
Define pathologic fracture.
|
fracture due to weakened bone caused by underlying condition
|
|
|
|
What is the clinical presentation of tibial torsion?
|

internally rotated tibia
usually 20° sometimes accentuated by laxity of knee ligaments |
Peds Current
|
|
|
What is the clinical presentation of tibial torsion?
|

internally rotated tibia
usually 20° sometimes accentuated by laxity of knee ligaments |
Peds Current
|
|
|
What is the ddx for pathologic fracture?
|
osteogenesis imperfecta
osteomalacia osteoporosis paget's disease of the bone benign bone tumor → osteochondroma, enchondroma primary bone malignancy → osteosarcoma, chondrosarcoma secondary bone malignancy |
|
|
|
What is the ddx for pathologic fracture?
|
osteogenesis imperfecta
osteomalacia osteoporosis paget's disease of the bone benign bone tumor → osteochondroma, enchondroma primary bone malignancy → osteosarcoma, chondrosarcoma secondary bone malignancy |
|
|
|
What is the clinical presentation of femoral anteversion?
|

internally rotated femur
|
Peds Current
|
|
|
What is the clinical presentation of femoral anteversion?
|

internally rotated femur
|
Peds Current
|
|
|
Define avulsion fracture.
|
fracture characterized by tearing away of a small bone fragment from the larger bone due to trauma to a ligament or tendon
|
|
|
|
Define avulsion fracture.
|
fracture characterized by tearing away of a small bone fragment from the larger bone due to trauma to a ligament or tendon
|
|
|
|
What is the management of femoral anteversion?
|
returns to neutral by 6-8y/o
encourage external rotation exercises → bike riding, skating refer to orthopedist if no external rotation of hip in extension |
Peds Current
|
|
|
What is the management of femoral anteversion?
|
returns to neutral by 6-8y/o
encourage external rotation exercises → bike riding, skating refer to orthopedist if no external rotation of hip in extension |
Peds Current
|
|
|
What are the complications of open (AKA compound) fracture?
|
blood loss
infection |
|
|
|
What are the complications of open (AKA compound) fracture?
|
blood loss
infection |
|
|
|
What are the disorders associated with "in-toeing"?
|
metatarus varus
tibial torsion femoral anteversion |
|
|
|
What are the disorders associated with "in-toeing"?
|
metatarus varus
tibial torsion femoral anteversion |
|
|
|
Define impacted fracture.
|
fracture characterized by one bone fragment being driven into another
|
|
|
|
Define impacted fracture.
|
fracture characterized by one bone fragment being driven into another
|
|
|
|
What does SCFE stand for?
|
slipped capital femoral epiphysis
|
|
|
|
What does SCFE stand for?
|
slipped capital femoral epiphysis
|
|
|
|
Define complicated fracture.
|
fracture + damage to surrounding structures (ligaments, tendons, arteries, nerves)
|
|
|
|
Define complicated fracture.
|
fracture + damage to surrounding structures (ligaments, tendons, arteries, nerves)
|
|
|
|
Where does SCFE often refer?
|
knee
|
|
|
|
Where does SCFE often refer?
|
knee
|
|
|
|
Positive Babinski indicates?
|
upper motor neuron lesion
*response may be absent if damage to reflex arc at nerve or root level |
Orthopedics p145
|
|
|
Positive Babinski indicates?
|
upper motor neuron lesion
*response may be absent if damage to reflex arc at nerve or root level |
Orthopedics p145
|
|
|
What is a SCFE?
|
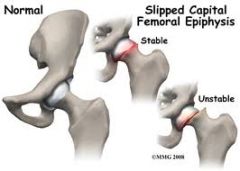
displacement of proximal femoral epiphysis
usually displaced medially and posteriorly relative to femoral neck |
PEDs Current
|
|
|
What is a SCFE?
|
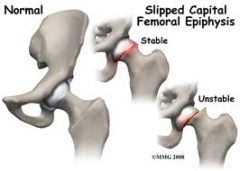
displacement of proximal femoral epiphysis
usually displaced medially and posteriorly relative to femoral neck |
PEDs Current
|
|
|
*double check for accuracy!!!
How do you differentiate articular from non-articular disorders? |
Articular:
pain in joint or in reference area of joint swelling and tenderness of entire joint line pain in passive and action ROM in all directions Nonarticular: diffuse pain |
|
|
|
*double check for accuracy!!!
How do you differentiate articular from non-articular disorders? |
Articular:
pain in joint or in reference area of joint swelling and tenderness of entire joint line pain in passive and action ROM in all directions Nonarticular: diffuse pain |
|
|
|
What is the etiology of a SCFE?
|
displacement of proximal femoral epiphysis d/t disruption of growth plate
cause unknown may be d/t weakness associated with hormonal changes associated with: obesity trauma hypothyroidism most common in obese adolescent males |
PEDs Current
|
|
|
What is the etiology of a SCFE?
|
displacement of proximal femoral epiphysis d/t disruption of growth plate
cause unknown may be d/t weakness associated with hormonal changes associated with: obesity trauma hypothyroidism most common in obese adolescent males |
PEDs Current
|
|
|
Define monoarticular, oligoarticular, and polyarticular.
|
monoarticular → 1 joint affected
oligoarticular → 2-5 joints affected polyarticular → >5 joints affected |
|
|
|
Define monoarticular, oligoarticular, and polyarticular.
|
monoarticular → 1 joint affected
oligoarticular → 2-5 joints affected polyarticular → >5 joints affected |
|
|
|
What is the clinical presentation of a SCFE?
|
pain and limp
referred pain to thigh and medial knee (knee pain may be only complaint) limited internal rotation of hip stable if able to bear weight unstable if unable to bear weight |
PEDs Current
|
|
|
What is the clinical presentation of a SCFE?
|
pain and limp
referred pain to thigh and medial knee (knee pain may be only complaint) limited internal rotation of hip stable if able to bear weight unstable if unable to bear weight |
PEDs Current
|
|
|
What is osteogenic imperfecta?
|
autosomal dominant genetic disorder characterized by brittle bones that are extremely susceptible to fracture
|
|
|
|
What is osteogenic imperfecta?
|
autosomal dominant genetic disorder characterized by brittle bones that are extremely susceptible to fracture
|
|
|
|
What is the diagnostic workup of a SCFE?
|
AP and lateral radiographs of the hip
|
PEDs Current
|
|
|
What is the diagnostic workup of a SCFE?
|
AP and lateral radiographs of the hip
|
PEDs Current
|
|
|
What is avascular necrosis?
|
poor blood supply → bone necrosis
|
|
|
|
What is avascular necrosis?
|
poor blood supply → bone necrosis
|
|
|
|
What is the management of a SCFE?
|
crutches for non-weight bearing
immediate referral to orthopedics for surgical fixation |
PEDs Current
|
|
|
What is the management of a SCFE?
|
crutches for non-weight bearing
immediate referral to orthopedics for surgical fixation |
PEDs Current
|
|
|
What is the ddx for avascular necrosis?
|
idiopathic in most cases
trauma → dislocation, fracture disease → chronic renal disease, sickle cell disease medications → prolonged oral steroid use, radiation therapy alcohol decompression sickness |
|
|
|
What is the ddx for avascular necrosis?
|
idiopathic in most cases
trauma → dislocation, fracture disease → chronic renal disease, sickle cell disease medications → prolonged oral steroid use, radiation therapy alcohol decompression sickness |
|
|
|
What are the complications of a SCFE?
|
AVN
premature degenerative arthritis |
|
|
|
What are the complications of a SCFE?
|
AVN
premature degenerative arthritis |
|
|
|
What is Charcot's joint?
|
progressive degeneration of a weight-bearing joint due to impaired sensation to the joint
impaired sensation to joint → decrease in protective mechanisms about the joint → destruction → deformity usually caused by DM |
Orthopedics p298
|
|
|
What is Charcot's joint?
|
progressive degeneration of a weight-bearing joint due to impaired sensation to the joint
impaired sensation to joint → decrease in protective mechanisms about the joint → destruction → deformity usually caused by DM |
Orthopedics p298
|
|
|
What is another name for Legg-Calves-Perthes disease?
|
avascular necrosis of proximal femur
|
|
|
|
What is another name for Legg-Calves-Perthes disease?
|
avascular necrosis of proximal femur
|
|
|
|
Where does avascular necrosis most commonly occur?
|
head of femur
head of humerus |
Orthopedics p77
|
|
|
Where does avascular necrosis most commonly occur?
|
head of femur
head of humerus |
Orthopedics p77
|
|
|
LEGG-CALVES-PERTHES DISEASE:
|
ETIOLOGY:
idiopathic osteonecrosis of capital femoral epiphysis usually occurs between 4-8 y/o CLINICAL PRESENTATION: persistent pain in hip or groin referred mild or intermittent pain in thigh or knee atrophy of thigh 2° to disuse ↓ internal rotation and abduction limping gait MANAGEMENT: 1. radiograph of hip 2. protect hip joint and maintain normal joint motion to prevent degenerative arthritis 3. little benefit from bracing and surgery controversial COMPLICATIONS: poorer prognosis if metaphysical defects, complete involvement of femoral head, or late childhood onset |
|
|
|
LEGG-CALVES-PERTHES DISEASE:
|
ETIOLOGY:
idiopathic osteonecrosis of capital femoral epiphysis usually occurs between 4-8 y/o CLINICAL PRESENTATION: persistent pain in hip or groin referred mild or intermittent pain in thigh or knee atrophy of thigh 2° to disuse ↓ internal rotation and abduction limping gait MANAGEMENT: 1. radiograph of hip 2. protect hip joint and maintain normal joint motion to prevent degenerative arthritis 3. little benefit from bracing and surgery controversial COMPLICATIONS: poorer prognosis if metaphysical defects, complete involvement of femoral head, or late childhood onset |
|
|
|
Define malunion and nonunion.
|
malunion → fracture that heals incorrectly
nonunion → fracture that fails to heals |
|
|
|
Define malunion and nonunion.
|
malunion → fracture that heals incorrectly
nonunion → fracture that fails to heals |
|
|
|
What is nursemaid's elbow?
|
subluxation of radial head from annular ligament
|
PEDS Current
|
|
|
What is nursemaid's elbow?
|
subluxation of radial head from annular ligament
|
PEDS Current
|
|
|
What is the etiology of nursemaid's elbow?
|
being lifted or pulled by the hand
consider abuse! |
PEDs Current
|
|
|
What is the etiology of nursemaid's elbow?
|
being lifted or pulled by the hand
consider abuse! |
PEDs Current
|
|
|
What is the clinical presentation of nursemaid's elbow?
|
painful fully pronated elbow
complaint that elbow will not bend radial head tenderness |
PEDs Current
|
|
|
What is the clinical presentation of nursemaid's elbow?
|
painful fully pronated elbow
complaint that elbow will not bend radial head tenderness |
PEDs Current
|
|
|
What is the diagnostic workup of nursemaid's elbow?
|
radiographs normal
|
PEDs Current
|
|
|
What is the diagnostic workup of nursemaid's elbow?
|
radiographs normal
|
PEDs Current
|
|
|
What is the management of nursemaid's elbow?
|

1. reduction → fully supinate arm and move from full extension to full flexion, will often hear click, and child will immediately feel better
2. sling x few days |
PEDs Current
|
|
|
What is the management of nursemaid's elbow?
|
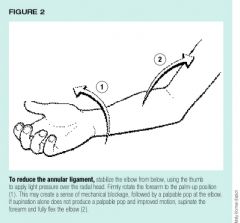
1. reduction → fully supinate arm and move from full extension to full flexion, will often hear click, and child will immediately feel better
2. sling x few days |
PEDs Current
|
|
|
What is the most common cause of septic arthritis?
|
staph aureus
|
Current p777
|
|
|
What is the most common cause of septic arthritis?
|
staph aureus
|
Current p777
|
|
|
What is the diagnostic workup of septic arthritis?
|
synovial fluid:
cell count >50,000 cells/mcL differentail >90% PMNs gram stain culture BC positive in 50% of cases |
Current p777
|
|
|
What is the diagnostic workup of septic arthritis?
|
synovial fluid:
cell count >50,000 cells/mcL differentail >90% PMNs gram stain culture BC positive in 50% of cases |
Current p777
|
|
|
SEPTIC ARTHRITIS:
|

ETIOLOGY:
source varies according to age: infant → usually d/t adjacent osteomylelitis child → usually isolated infection without bone involvement teenager → usually organism with affinity for joints (gonococcus) or underlying systemic infection organism varies with age: <4 m/o → group B strep, staph aureus 4 m/o to 4 y/o → staph aureus, h. flu (less common d/t immunizations) >4 y/o → staph aureus, staph pyogenes CLINICAL PRESENTATION: inflammatory monoarticular arthritis commonly affects knee, hip, wrist, shoulder, or ankle acute pain, swelling, warmth worsens over hours joint effusion infant → suspect if irritable, poor feeding, decreased abduction; paralysis of limb d/t inflammatory neuritis child → fever, malaise, vomiting, restriction of motion MANAGEMENT: 1. joint aspiration → WBC count >50,000 2. hospitalization and surgical drainage 3. empiric antibiotic therapy → nafcillin or oxacillin + 3rd generation cephalosporin 4. narrow-spectrum antibiotic therapy → selected based on age, gram stain, culture; 3 weeks for staph infection, 2 weeks for other infections COMPLICATIONS: if not detected before 24 hours, destruction of joint cartilage occurs, followed by arthrosis and fibrosis damage to growth plate may also occur |
|
|
|
SEPTIC ARTHRITIS:
|

ETIOLOGY:
source varies according to age: infant → usually d/t adjacent osteomylelitis child → usually isolated infection without bone involvement teenager → usually organism with affinity for joints (gonococcus) or underlying systemic infection organism varies with age: <4 m/o → group B strep, staph aureus 4 m/o to 4 y/o → staph aureus, h. flu (less common d/t immunizations) >4 y/o → staph aureus, staph pyogenes CLINICAL PRESENTATION: inflammatory monoarticular arthritis commonly affects knee, hip, wrist, shoulder, or ankle acute pain, swelling, warmth worsens over hours joint effusion infant → suspect if irritable, poor feeding, decreased abduction; paralysis of limb d/t inflammatory neuritis child → fever, malaise, vomiting, restriction of motion MANAGEMENT: 1. joint aspiration → WBC count >50,000 2. hospitalization and surgical drainage 3. empiric antibiotic therapy → nafcillin or oxacillin + 3rd generation cephalosporin 4. narrow-spectrum antibiotic therapy → selected based on age, gram stain, culture; 3 weeks for staph infection, 2 weeks for other infections COMPLICATIONS: if not detected before 24 hours, destruction of joint cartilage occurs, followed by arthrosis and fibrosis damage to growth plate may also occur |
|
|
|
Define torticollis.
|
stiff neck
|
|
|
|
Define torticollis.
|
stiff neck
|
|

