![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
114 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is MEN 1?
|
familial multiglandular endocrine tumor syndrome
affects 2-10 in 100,000 may present in childhood or adulthood presentation varies hyperparathyroidism may include pituitary, parathyroid, endopancreatic, and non-endocrine tumors gene testing hypercalcemia |
|
|
|
What is a giant cell tumor?
|
benign vascular lesion in bone but may transform into malignancy
|
Orthopedics p386
|
|
|
What are multiple endocrine neoplasias?
|
autosomal dominant genetic disorders causing a predisposition in the development of tumors, especially tumors involving endocrine glands
|
|
|
|
Define oncogene.
|
a gene that normally codes for proteins that up-regulate cell growth and differentiation; if mutated or over-expressed, can cause normal cells to become cancer cells
|
|
|
|
What characterizes MEN 2A?
|
medullary thyroid cancers, pheochromocytomas, Hirschsprung disease
|
|
|
|
What is the etiology of giant cell tumor?
|
spontaneous
associated with hyperparathyroidism rare usually occurs between 20-40y/o rare in children and elderly |
|
|
|
What characterizes MEN 2B?
|
medullary thyroid cancers, pheochromocytomas, Marfan-like habitus, mucosal neuromas, intestinal ganglioneuroma, delayed puberty
|
|
|
|
Define tumor suppressor gene.
|
a gene that normally codes for proteins that down-regulate cell growth or cause apoptosis; if mutated or under-expressed, can cause normal cells to become cancer cells
|
|
|
|
What characterizes MEN 1?
|
tumors of the parathyroid glands, endocrine pancreas and duodenum, pituitary, adrenal, thyroid; lipomas and facial angiofibromas
|
|
|
|
What is the clinical presentation of a giant cell tumor?
|
bone pain usually affecting distal metaphysis and epiphysis of femur
possible pathologic fracture |
|
|
|
Define hypertrophy.
|
enlargement due to an increase in the size of cells
|
|
|
|
What is the diagnostic workup of a giant cell tumor?
|
AP and lateral radiographs of femur → "soap bubble" appearance
|
Orthopedics p386
|
|
|
Define hyperplasia.
|
enlargement due to an increase in the number of cells
|
|
|
|
What is the management of a giant cell tumor?
|
surgical removal
|
|
|
|
Define dysplasia.
|
partially reversible change from a mature cell to cell with abnormalities in both differentiation and maturation
|
|
|
|
List types of bone tumors and their characteristic radiographic appearance.
|
osteosarcoma → sunburst appearance
ewing's sarcoma → onion skin appearance giant cell tumor → soap bubble appearance |
|
|
|
Define anaplasia.
|
regression of cells to an undifferentiated state
|
|
|
|
Benign and malignant lesions typically develop in which part of a long bone?
|
metaphysis
|
|
|
|
Define aplasia.
|
congenital absence or defective development of a tissue or organ
|
|
|
|
What percent of 2° bone tumors affect the spine?
|
40%
*spine = most common site for bone metastasis |
Orthopedics p356
|
|
|
Define metaplasia.
|
reversible change from one type of mature cell to another type of mature cell that is normally not found in the tissue involved
|
|
|
|
What is an enchondroma?
|
benign bone tumor originating from cartilage (i.e. cartilage cyst)
|
Orthopedics p446
|
|
|
Define neoplasm.
|
tissue that grows by cell proliferation more rapidly than normal and continues to grow after stimuli that initiated the new growth cease; usually forms a distinct mass; either benign or malignant
|
|
|
|
What is the clinical presentation of enchondroma?
|
usually occurs between 10-50 y/o
nonspecific symptoms no pain usually in small bones of hands and feet discovered incidentally or following pathologic fracture enlarged fingers deformities |
Orthopedics p446
|
|
|
Define neoplasia.
|
pathological process that results in a neoplasm
|
|
|
|
Where do enchondromas most commonly occur?
|
small bones of hands and feet
|
Orthopedics p446
|
|
|
Define carcinoma.
|
any malignant neoplasm derived from epithelial cells
|
|
|
|
What is the diagnostic workup of enchondroma?
|
radiograph
usually located centrally in bone |
|
|
|
What are examples of carcinoma?
|
squamous cell carcinoma
basal cell carcinoma melanoma adenocarcinoma |
|
|
|
What is the management of enchondroma?
|
1. observation → periodic radiographs
2. if diagnosis uncertain → surgery to R/O chondrosarcoma 3. if recurrent fracture → surgery |
Orthopedics p446
|
|
|
Define carcinoma in situ.
|
localized carcinoma; precursor of metastatic carcinoma
|
|
|
|
How do you distinguish between enchondroma and chondrosarcoma?
|
enchondroma → painless
chondrosarcoma → painful, bone erosion |
|
|
|
Define metastatic/invasive carcinoma.
|
carcinoma that has spread beyond epithelium into adjacent structures
|
|
|

|
enchondroma (of 5th metacarpal)
L: radiograph R: MRI |
|
|
|
What are the most common sites of metastasis for lung cancer?
|
brain, bones
|
http://www.cancer.gov/cancertopics/factsheet/Sites-Types/metastatic
|
|
|
What is an osteochondroma?
|
classified as benign bone tumor but thought to be a developmental abnormility where part of physis forms outgrowth on bone surface
|
Orthopedics p446
|
|
|
What are the most common sites of metastasis for colon cancer?
|
liver
|
http://www.cancer.gov/cancertopics/factsheet/Sites-Types/metastatic
|
|
|
What is the clinical presentation of osteochondroma?
|
painless mass
usually occurs at distal metaphysis of femur or proximal metaphysis of tibia growth ceases with skeletal maturity |
Orthopedics p446
|
|
|
What are the most common sites of metastasis for breast cancer?
|
brain, lungs, liver, bones
|
http://www.cancer.gov/cancertopics/factsheet/Sites-Types/metastatic
|
|
|
What is the management of osteochondroma?
|
1. observation → periodic radiographs → often regresses once reach skeletal maturity
2. if symptoms (pain, blood vessel or nerve compromise, large cartilage cap) → surgical removal once reach skeletal maturity |
Orthopedics p446
|
|
|
What are the most common sites of metastasis for prostate cancer?
|
bones
|
http://www.cancer.gov/cancertopics/factsheet/Sites-Types/metastatic
|
|
|
What is the diagnostic workup of osteochondroma?
|
radiograph →
sessile or pedunculated lesion continuous with cortex and marrow cavity small cartilage cap |
|
|
|
List the 5 most common sites of metastasis and their associated symptoms.
|
brain → HA, vertigo, seizures
lungs → dyspnea, cough, hemoptysis liver → hepatomegaly, jaundice bones → pain, fracture lymph nodes → lymphadenopathy |
|
|

|
pedunculated osteochondroma of distal femur + associated fracture
|
|
|
|
Define sarcoma.
|
any malignant neoplasm derived from connective tissue cells
|
|
|
|
What is chondrosarcoma?
|
malignant cartilage tumor
primary or secondary from enchondroma |
Orthopedics p448
|
|
|
Define leukemia.
|
malignancy derived from hematopoietic cells
|
|
|
|
What is the clinical presentation of chondrosarcoma?
|
occurs >40 y/o
shoulder girdle, pelvis, proximal femur painful swelling |
Orthopedics p448
|
|
|
What does ALL stand for?
|
acute lymphocytic leukemia
|
|
|
|
What bone tumor presents at the diaphysis?
|
Ewing's sarcoma
|
Orthopedics p448
|
|
|
What does AML stand for?
|
acute myeloid leukemia
|
|
|
|
What is the diagnostic workup of chondrosarcoma?
|
radiograph → speckled calcifications in destructive radiolucent lesion
|
Orthopedics p449
|
|
|
What is the difference between acute and chronic leukemias?
|
acute → predominance of immature WBCs
chronic → bone marrow functional → differentiation → predominance of mature WBCs |
Pathology p84
|
|

|
bone destruction + sunburst pattern → osteosarcoma (of proximal fibula)
|
|
|
|
Who is most commonly affected by chronic leukemia, children or adults?
|
adults
|
Pathology p84
|
|

|
chondrosarcoma of inferior ramus of pubis
|
|
|
|
Who is most commonly affected by acute leukemia, children or adults?
|
children
|
Pathology p84
|
|

|
Ewing's sarcoma (of femur)
|
|
|
|
What is the etiology of AML?
|
malignant proliferation of myeloid precursor cells; commonly occurs in young adults 15-39y/o
|
|
|
|
What is the management for chondrosarcoma?
|
1. refer to orthopedic specialist
2. surgical resection 3. NOT sensitive to chemotherapy or radiation |
Orthopedics p449
|
|
|
What is the clinical presentation of acute leukemia?
|
acute onset
pallor bleeding → petechiae, purpura, gingival bleeding, epistaxis, menorrhagia infection → pneumonia, cellulits, perirectal fissures gingival hypertrophy hepatosplenomegaly variable lymphadenopathy variable bone tenderness → sternum, femur, tibia joint pain hyperleukocytosis → headache, confusion, blurred vision, dyspnea, priapism |
Current p464
|
|
|
What is the most common tumor of the hand?
|
enchondroma
|
|
|
|
What is the diagnostic work-up of acute leukemia?
|
CBCDP → pancytopenia
blood smear → blasts bone marrow biopsy → hypercellular, >20% blasts flow cytometry to determine type of leukemia |
Current p464
|
|
|
What is multiple myeloma?
|
neoplastic proliferation of plasma cells of bone marrow
|
Orthopedics p168
|
|
|
Which is more difficult to treat, AML or ALL?
|
AML
|
Pathology p85
|
|
|
What is the etiology of ALL?
|
leukemia characterized by malignant proliferation of lymphoid precursor cells; commonly occurs in young adults
|
|
|
|
What is the ddx for leukemia?
|
idiopathic
chromosomal abnormalities myeloproliferative diseases myelodysplasia toxins → benzene chemotherapy radiation |
Current p464
|
|
|
ALL comprises _% of childhood leukemias and _% of adult leukemias?
|
80% of childhood leukemias
20% of adult leukemias |
Current p464
|
|
|
What are auer rods?
|
needle-like clumps in cytoplasm of myeloid blasts
|
|
|
|
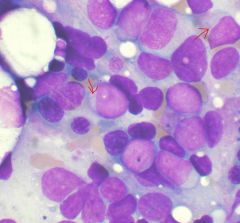
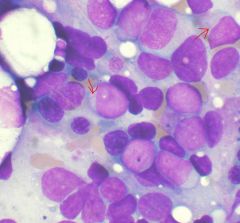
auer rods → AML
|
|
|
|
What is the management for acute leukemia?
|
1. refer to hematologist
2. initial chemotherapy → dependent on leukemia type 3. postremission therapy → chemotherapy, transplantation → dependent on age, risk-factors, status |
Current p467
|
|
|
What is the prognosis for AML?
|
if <60y/o, complete remission for 70-80%; 35-60% cure rate dependent on postremission therapy
if >60y/o, complete remission for 50% but only 10-15% cure rate |
Current p467
|
|
|
What does CLL stand for?
|
chronic lymphocytic leukemia
|
|
|
|
What is CLL?
|
leukemia characterized by malignant proliferation of B lymphocytes
|
|
|
|
What is the etiology of CLL?
|
malignant proliferation of B lymphocytes; commonly occurs >50y/o
|
Current p467
|
|
|
What is the clinical presentation of CLL?
|
fatigue
lymphadenopathy hepatosplenomegaly |
Current p467
|
|
|
What is the diagnostic work-up of CLL?
|
CBCDP → lymphocytosis
FISH |
Current p467
|
|
|
What is the management of CLL?
|
1. refer to hematologist
2. if early → observation 3. if progressive fatigue, symptomatic lymphadenopathy, anemia, or thrombocytopenia → treatment 4. chemotherapery → fludarabine 5. antibody → rituximab 6. if refractory → allogenic transplantation |
Current p467
|
|
|
What are the complications of CLL?
|
autoimmune hemolytic anemia
immune thrombocytopenia |
Current p467
|
|
|
What is the prognosis of CLL?
|
if early, 10-15 years
if late, 2 years |
Current p467
|
|
|
What are the USPSTF screening recommendations for bladder cancer?
|
do not screen (grade D)
*encourage smoking cessation since 50% of all bladder cancer occurs in current or former smokers |
USPSTF Handbook 2009
|
|
|
What are the USPSTF screening recommendations for prostate cancer?
|
1. men <75y/o → current evidence insufficient to recommend screening (grade I)
2. >75y/o → do not screen (grade D) *discuss benefits and harms of prostate cancer screening and treatment with patients |
USPSTF Handbook 2009
|
|
|
What are the USPSTF screening recommendations for testicular cancer?
|
do not screen in asymptomatic adolescent and adult males (grade D)
|
USPSTF Handbook 2009
|
|
|
What are the USPSTF screening recommendations for renal cell carcinoma?
|
no recommendations
|
USPSTF Handbook 2009
|
|
|
What are the USPSTF screening recommendations for penile cancer?
|
no recommendations
|
USPSTF Handbook 2009
|
|
|
What are the USPSTF screening recommendations for Wilms' tumor?
|
no recommendations
|
USPSTF Handbook 2009
|
|
|
What do the USPSTF screening grades mean?
|
A = recommend screening (high benefit)
B = recommend screening (moderate benefit) C = recommend against screening (but may be useful in certain patients) D = recommend against screening (no benefit or potential harm) I = insufficient evidence to recommend for or against screening |
|
|
|
What is the controvery of PSA screening?
|
prostate cancer is slow-growing
may be lethal or cause no harm controvery over overdiagnosis and overtreatment controvery over whether PSA screening save lives or just subjects patients to unecessary radiation, surgery, and side effects |
|
|
|
What are the risk factors of prostate cancer?
|
black
high fat diet FH of prostate cancer |
Current ch39
|
|
|
What is the clinical presentation of prostate cancer?
|
prostate → focal nodules or areas of induration
(prostate may feel normal but PSA elevated) if large → obstructive voiding symptoms |
Current ch39
|
|
|
What is the diagnostic workup of prostate cancer?
|
elevated PSA
prostate biopsy transrectal ultrasonanography for staging bone scan for bone metastasis MRI for lymph metastasis |
Current ch39
|
|
|
What is the management of prostate cancer?
|
controversial
management based on age, comorbidities, staging observation → serial rectal exams, PSAs, and biopsies if >10 year life expectancy → consider treatment with prostatectomy or radiation therapy |
Current ch39
|
|
|
What is the pattern of metastasis for prostate cancer?
|
axial skeleton → back pain, pathologic fractures
lymph nodes → LE lymphedema |
Current ch39
|
|
|
What are the risk factors for bladder cancer?
|
smoking
environmental exposure to solvents or dyes |
Current ch39
|
|
|
What is the clinical presentation of bladder cancer?
|
hematuria
irritative voiding symptoms → frequency, urgency |
Current ch39
|
|
|
What is the diagnostic workup of bladder cancer?
|
UA → hematuria
cytology US, CT, or MRI → filling defects biopsy → staging |
Current ch39
|
|
|
What is the pattern of metastasis for bladder cancer?
|
liver → hepatomegaly
lymph → LE lymphedema |
Current ch39
|
|
|
What is the management of bladder cancer?
|
1. if superficial → resection +/-local chemotherapy
2. if invasive but localized → cystectomy, irradiation, chemotherapy 3. if invasive → systemic chemotherapy followed by cystectomy |
Current ch39
|
|
|
What are the risk factors for renal cell carcinoma?
|
smoking
familial and genetic factors dialysis |
|
|
|
What is the clinical presentation of renal cell carcinoma?
|
fever, weight loss
hematuria flank pain palpable mass in abdomen |
|
|
|
What is the diagnosic workup of renal cell carcinoma?
|
erythrocytosis 5% though anemia more common
hypercalcemia 10% UA → hematuria 60% KUB or CT → renal masses |
|
|
|
What is the management of renal cell carcinoma?
|
1. if localized → partial or complete nephrectomy
2. no effective chemotherapy |
|
|
|
What is the pattern of metastasis for renal cell carcinoma?
|
◦Lung (75%)
◦Soft tissues (36%) ◦Bone (20%) ◦Liver (18%) ◦Cutaneous sites (8%) ◦Central nervous system (8%) |
|
|
|
What are the risk factors for testicular cancer?
|
most common 20-35y/o and >60y/o
cryptochorism *trauma and infertility DO NOT increase risk |
|
|
|
What is the clinical presentation of testicular cancer?
|
usually asymptomatic
painless swelling or nodule of testicle sensation of heaviness nodule cannot be separated from testicle secondary hydrocele if advanced, |
|
|
|
What is the diagnostic workup of testicular cancer?
|
HCG
AFP (alpha-fetoprotein) LD (lactate dehydrogenase) scrotal ultrasound → to distinguish between testicular vs non-testicular inguinal orchiectomy → establishes diagnosis chest, abdominal, and pelvic CT → staging |
|
|
|
What is the management of testicular cancer?
|
1. inguinal exploration
2. if testicular cancer cannot be excluded → orchiectomy 3. avoid testicular biospy 4. further therapy dependent on histology and staging → irradiation, chemotherapy 5. FUV monthly x 2 years, then bimonthly x 1 year, obtaining tumor markers at each visit and CXR/CT every 3 months |
|
|
|
What is the pattern of metastasis of testicular cancer?
|
lymph
retroperitoneal lung brain |
|
|
|
What are the risk factors of penile cancer?
|
5th or 6th decade
uncircumsized smoking balanitis |
|
|
|
What is the clinical presentation of penile cancer?
|
non-tender ulcer or warty growth under foreskin
itchy or burning sensation beneath foreskin hidden behind erythematous phimosis |
|
|
|
What is the diagnostic workup of penile cancer?
|
ultrasonagraphy or MRI
biospy |
|
|
|
What is the management of penile cancer?
|
1. circumcision
2. resection 3. radiation if young male + noninvasive cancer, resection refused, metastasis 4. chemotherapy if metastasis |
|
|
|
What is the pattern of metastasis of penile cancer?
|
lymph
|
|
|
|
What is the best treatment for metastatic prostate cancer?
|
decreasing testosterone
|
|

