![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What does the primary survey consist of?
|
airway, breathing, circulation, neurologic deficits
|
|
|
|
What is the approach to the patient in the emergency room?
|
classify as critical, emergent, nonurgent
stabilize if necessary R/O most serious causes of presentation |
|
|
|
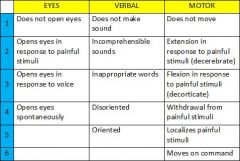
What is the range of the glascow coma scale?
|
3-15
where 3 = coma or death where 15 = normal |
|
|
|
Describe the glascow coma scale.
|
|
|
|
|
What is the clinical presentation and initial management of acetaminophen overdose?
|
1. clinical presentation → asymptomatic or nausea, vomiting, anorexia, RUQ pain
2. draw 4-hour post-ingestion acetaminophen level, LFTs 3. draw another acetaminophen level 4-6 hours later if sustained-release acetaminophen ingested 4. assess likelihood of hepatic toxicity based on clinical exam, acetaminophen level, LFTs 5. toxic dose of acetaminophen is >150mg/kg in children and 7g in adults 6. hepatic toxicity occurs 24-72 hours after ingestion and may be manifested by nausea, vomiting, anorexia, jaundice, RUQ pain, and ↑ LFTs 7. give activated charcoal 8. give N-acetylcysteine within 12-16 hours of ingestion if acetaminophen level >150 micrograms/mL 9. do not delay N-acetylcysteine if high suspicious and acetaminophen level not ready 10. obtain salicylate level since often ingested simultaneously 11. hospitalize if require N-acetylcysteine therapy or evidence of hepatic toxicity |
|
|
|
What is the clinical presentation and initial management of amphetamine overdose?
|
1. CNS stimulant
2. clinical presentation → sympathetic hyperactivity → euphoria, restlessness, psychosis, palpitations, HTN, hyperthermia, mydriasis, ↑ muscle tone, arrhythmias, seizures 3. hyperthermia and seizures may result in rhabdomyolysis and myoglobinuria 4. peak toxicity within 2-3 hours if oral and 30 minutes if IV or IM 5. serum drug levels are of little value and measures to enhance elimination do not alter outcome 6. treatment is supportive 7. monitor temp and start cooling blanket if hyperthermia 8. give diazepam if severe agitation, psychosis, or seizure 9. give nitroprusside if diastolic BP >120 10. may give propranolol if tachycardia or ventricular arrhythmias 11. get urine for myoglobin 12. get EKG, cardiac enzymes if chest pain 13. get CT if seizures 14. hospitalize if psychosis, HTN, hyperthermia, chest pain, arrhythmias, or prolonged symptoms |
|
|
|
What is the clinical presentation and intitial management of salicylate toxicity?
|
1. weak acid
2. clinical presentation → nausea, vomiting, tinnitus, listlessness, hyperventilation, hyperpnea, hyperthermia, respiratory alkalosis followed by severe metabolic acidosis, hypokalemia, hypoglycemia, seizures, hyperpyrexia, coma 3. presentation of sub acute toxicity often occurs in very young and very old and manifests as dehydration, obtundation, acidosis, cerebral and pulmonary edema, death 4. toxicity at >150 mg/kg 5. half life may increase from 2 to 20 hours at toxic levels 6. get salicylate level and repeat every 4-6 hours 7. give activated charcoal 8. additional activated charcoal and whole bowel irrigation if enteric-coated aspirin ingested 9. give IV crystalloid solution to correct dehydration 10. give sodium bicarbonate to correct acidosis 11. give glucose to correct hypoglycemia 12. give vitamin K IM if hypoprothombinemia 13. hemodialysis if persistent seizures, acidosis fails to respond to tx, cerebral or pulmonary edema 14. hospitalize all patients |
|
|
|
What is the clinical presentation and intitial management of TCA overdose?
|
1. anticholinergic
2. clinical presentation → agitation, hallucinations, dry mouth, hypotension, tachycardia, mydriasis, twitching, myoclonic jerk, seizures, coma 3. toxic dose is 5mg/kg 4. 10-30 hour half-life 5. give activated charcoal within 1 hour of ingestion 6. get serial EKG for 6 hours – possible QRS widening, AV block, ventricular arrhythmias, torsades 7. treat hypotension with colloid solutions and sodium bicarbonate 8. treat ventricular arrhythmias and AV block with sodium bicarbonate 9. treat seizures with diazepam 10. hospitalize all patients |
|
|
|
Define concussion.
|
trauma-induced alteration in mental status that may or may not include loss of consciousness
|
|
|
|
Describe concussion grading.
|
GRADE I:
transient confusion, no loss of consciousness, symptoms last <15 minutes stop activity may return after asymptomatic for 15 minutes GRADE 2: transient confusion, no loss of consciousness, symptoms last >15 minutes stop activity may return to activity if asymptomatic for 1 week GRADE 3: loss of consciousness stop activity and go to ER may return to activity if asymptomatic for 1 week + LOC only seconds long may return to activity if asymptomatic for 2 weeks + LOC 1 minutes long |
|
|
|
What is the management of a concussion?
|
post-concussion symptoms include HA, dizziness, and memory problems
concussion self-limiting with post-concussion symptoms resolving within weeks to months |
|
|
|
BASILAR SKULL FX:
|
ETIOLOGY:
skull fracture at base of skull, typically at petrous portion of temporal bone caused by trauma CLINICAL PRESENTATION: raccoon eyes → periorbital ecchymosis Battle sign → mastoid ecchymosis CSF leak from ear or nose hemotympanum hearing loss DIAGNOSTIC WORKUP: non-contrast CT EMERGENT MANAGEMENT: admit for observation neurosurgery consult if more serious intracranial abnormality present |
|
|

|
Battle sign indicating basilar skull fx
|
|
|
|
Any alteration of consciousness or amnesia to an event of injury requires?
|
CT
|
|
|
|
EPIDURAL HEMATOMA:
|

ETIOLOGY:
collection of blood and clot between dura mater and bones of skull bleeding source may be meningeal arteries (often middle meningeal artery) or occasionally dural venous sinuses usually d/t head trauma CLINICAL PRESENTATION: brief loss of consciousness followed by transient lucid interval followed by rapid deterioration DIAGNOSTIC WORKUP: CT reveals biconvex (lens-shaped) hematoma EMERGENT MANAGEMENT: decompression to prevent brain herniation ASAP |
|
|

|
epidural hematoma of right frontal lobe
|
|
|
|
SUBDURAL HEMATOMA:
|
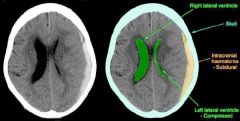
ETIOLOGY:
collection of blood between dura mater and arachnoid mater bleeding source is often bridging veins may be acute, chronic, or acute on chronic usually d/t brain atrophy risk factors include elderly, alcoholism, anticoagulants, repeated head injuries CLINICAL PRESENTATION: HA, confusion, LOC minimal neurologic deficit with chronic hematomas neurologic deficits with acute hematomas DIAGNOSTIC WORKUP: CT reveals concave (crescent-shaped, conforms to underlying cerebral cortex) hematoma EMERGENT MANAGEMENT: neurosurgery consult |
|
|

|
subdural hematoma of left hemisphere
|
|
|
|
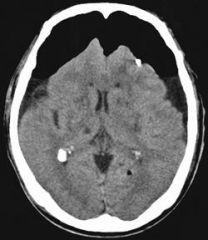
SUBARACHNOID HEMATOMA:
|
ETIOLOGY:
collection of blood between subarchnoid mater and pia mater causes include head trauma, AVM leading to an aneurysm, bleeding disorders, anticoagulants CLINICAL PRESENTATION: sudden severe HA - “worst HA of your life” DIAGNOSTIC WORKUP: CT → peripheral if traumatic; circle of willis if AVM If CT negative, do LP LP positive if blood present EMERGENT MANAGEMENT: may obstruct CSF and cause increased ICP if asymptomatic → admit for observation if altered consciousness or other neurological deficits → admit to critical care for ICP monitoring |
|
|
|
DIFFUSE AXONAL INJURY:
|
ETIOLOGY:
blunt trauma → sudden acceleration/deceleration → diffuse neuronal shearing blunt trauma may be d/t MVA, child abuse (shaken baby syndrome), fall, assault, etc CLINICAL PRESENTATION: post-traumatic coma possible autonomic dysfunction → HTN, fever, sweating DIAGNOSTIC WORKUP: difficult to see on CT CT may reveal blurring of the margin between gray and white matter, punctate cerebral hemorrhages or cerebral edema EMERGENT MANAGEMENT: lacks specific treatment stabilize patient and prevent increasing ICP |
|
|
|
pneumocephalus
AKA mount Fugi sign presence of air or gas within cranial cavity |
|
|
|
SKULL FX:
|
ETIOLOGY:
trauma CLINICAL PRESENTATION: closed skull fracture open skull fracture → underlies scalp lacerations, palpable depressed skull fracture → visible on inspection, palpable DIAGNOSTIC WORKUP: noncontrast CT open skull fx likely if pneumocephalus present EMERGENT MANAGEMENT: R/O intracranial injuries closed skull fx → observation for developing epidural hematoma open skull fx → admit, surgical referral, consider antibiotics d/t high risk of infection depressed skull fx → admit, surgical referral, consider antibiotics d/t high risk of infection if open fx |
|
|
|
Describe first-degree burn.
|
involves epidermis
characterized by erythema, skin texture normal, pain resolves in 5-10 days no scarring |
|
|
|
Describe second-degree burn.
|
SUPERFICIAL PARTIAL-THICKNESS:
extends into superficial (papillary) dermis characterized by erythema, +/- blistering, skin edematous, pain resolves in 10-21 days minimal or no scarring DEEP PARTIAL THICKNESS: extends into deep (reticular) dermis characterized by pink to white discoloration, skin thick, possible pain resolves in 25-60 days dense scarring |
|
|
|
Describe third-degree burn.
|
extends through entire dermis
characterized by white, brown or black discoloration, skin leathery, no pain no spontaneous healing |
|
|
|
Describe fourth-degree burn.
|
extends through subcutaneous tissue, tendon, or bone
characterized by black or charred discoloration, dry skin, no pain no spontaneous healing |
|
|
|
SUNBURN:
|
1st-degree or 2nd-degree (superficial partial-thickness)
characterized by erythema +/- blistering hx of sun or tanning booth exposure no diagnostic workup saline-soaked dressings, calamine lotion, and NSAIDs (ibuprofen) for pain relief no scarring RTC in 2-3 days if large blisters to monitor for secondary infection admit if IV fluids and analgesics required avoid prolonged sun exposure and wear sunscreen |
|
|
|
CHEMICAL BURNS:
|
CLINICAL PRESENTATION:
usually d/t acids or alkalis, sometimes phosphorus or phenol ascertain type of chemical, concentration acid burns → partial-thickness, erythema, erosion, HCL stains skin black, nitric acid stains skin yellow, sulfuric acid stains skin brown alkali burns → full-thickness, pale, leathery, slippery DIAGNOSTIC WORKUP: none MANAGEMENT: remove contaminated clothing copious irrigation with large amounts of tap water ASAP alkali burns may require emergency excision PROGNOSIS: size usually underestimated d/t slow development so reevaluate after 24-48 hours |
|
|
|
What are the 5 P's of compartment syndrome?
|
pain, paresthesias, pallor, pulselessness, poikilothermia
|
|
|
|
CHILBLAINS:
|
Chilblains (Pernio)
d/t cold exposure but less severe that frostbite (no actual freezing of tissues) most common in women, children, PVD pruritic, red, violaceous lesions that usually form on face or extremities +/- blistering, edema, lymphocytic vasculitis elevate and allow to warm gradually at room temp do not massage or apply heat |
|
|
|
DECOMPRESSION SICKNESS:
|
RISK FACTORS:
scuba diving inadequately pressurized airplane CLINICAL PRESENTATION: Type 1 = deep aching pain in large joints and extremities AKA “the bends”, cutaneous marmorata Type 2 = cardiorespiratory (chest pain, SOB) or neurologic (ataxia, spinal paralysis, vertigo, visual or speech disturbance, cognitive deficits) symptoms INITIAL MANAGEMENT: 100% O2 x 2 hours mild analgesics crystalloid IV fluids recompression in hyperbaric chamber ASAP |
|
|
|
What is the most common infecting organism from cat scratches?
|
pasteurella multocida
|
|
|
|
What is the cause of cat scratch disease?
|
bartonella henselae
|
|
|
|
What do acid burns do?
|
produce a coagulation necrosis
denature proteins → forming coagulum (AKA eschar) → limiting penetration |
|
|
|
What do alkali burns do?
|
produce a liquefaction necrosis
denaturation of proteins saponification of lipids which does not limit penetration |
|
|
|
Which are worse, acid or alkali burns?
|
alkali
penetration not limited like in acid burns |
|
|

|
allergic angioedema
|
|
|
|
Why is angioedema a medical emergency?
|
rapid swelling → airway obstruction
|
|
|
|
What is treatment for allergic angioedema?
|
epinephrine
|
|
|
|
What are the indications for a drug screen?
|
suspected substance abuse, overdose, or poisoning
|
Interpreting Laboratory Data p47
|
|
|
What is a drug screen (AKA tox screen)?
|
a qualitative test used to determine the presence of a specific substance or group of substances
|
Interpreting Laboratory Data p47
|
|
|
How are drug screens categorized?
|
1. tests included
2. preliminary vs. confirmatory |
Interpreting Laboratory Data p48
|
|
|
What factors should be considered when ordering a drug screen confirmation?
|
1. Will result affect patient's care?
2. Will result be reported before patient discharge? 3. Is cost justified? 4. Are legal actions anticipated? |
Interpreting Laboratory Data p48
|
|
|
What should you order for drug screen confirmatory testing?
|
GC-MS confirmation
(gas chromatography-mass spectrometry) |
Interpreting Laboratory Data p49
|
|
|
If a drug screen is negative, it means the drug was not present, true or false?
|
false
it means the drug was not detected |
Interpreting Laboratory Data p51
|
|
|
What are possible reasons for negative drug screen?
|
drug not taken
drug not part of drug screen panel urine too dilute |
Interpreting Laboratory Data p51
|
|
|
What tests are in UDAS for Swedish?
|
Amphetamines
Barbiturates Benzodiazepines Cannabinoids Cocaine Metab. Methadone Opiates Phencyclidine THC Metabolite Creatinine |
Antrim
|
|
|
What factors should be considered when ordering a drug screen in ER setting?
|
1. Substances that exhibit delayed toxic symptoms (e.g. sustaine release agents)?
2. Multiple agents ingested? 3. Multiple agents found at scene? If yes to any of the above, order drug screen |
Interpreting Laboratory Data p49
|
|
|
How does transfusion of one unit of RBCs affect HCT?
|
raises HCT 4%
|
Current p518
|

