![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
492 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is an atrial septal defect?
|
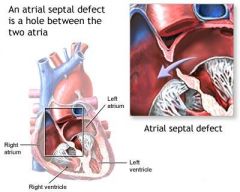
congenital heart defect characterized by persistence of foramen ovale or atrial-septal defect resulting in abnormal blood flow between atria
|
|
|
|
What is the cause of an ejection systolic murmur in anemia?
|
anemia -> O2 carrying capacity of blood reduced -> CO increases to meet metabolic demands -> heart pumps harder and faster -> creating ejection systolic murmur
constricted garden hose analogy: -slow water speed -> no sound -fast water speed -> sound |
|
|
|
What is the clinical presentation and diagnostic workup of patent ductus arteriosus?
|
CLINICAL PRESENTATION:
dependent on size of shunt and degree of pulmonary HTN diaphoresis with feeding failure to thrive tachypnea S2 narrowly split or paradoxically split (narrows on inspiration and widens on expiration) continuous machinery murmur begins shortly after S1, peaks at S2, passes through S2 into diastole, becomes a decrescendo murmur and fades before S1 maximal at 2nd left intercostal space radiates into anterior lung fields diastolic flow murmur at apex bounding peripheral pulses widened pulse pressure DIAGNOSTIC WORKUP: CXR EKG ECHO |
|
|
|
What is the ddx for ejection systolic murmur?
|
anemia
pregnancy excessive exercise |
|
|
|
What is patent ductus arteriosus?
|
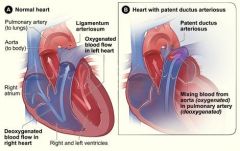
congenital heart defect characterized by persistence of ductus arteriosus resulting in abnormal blood flow between pulmonary artery and aorta
ductus arteriosus normally closes spontaneously at 3-5 days of age |
|
|
|
What is dextrocardia?
|
congenital defect where heart is situated on RT side of body
|
|
|
|
What is tetralogy of fellot?
|
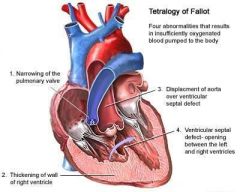
congenital heart defect characterized by:
1. narrowing of pulmonary valve 2. thickening of RT ventricular wall 3. displacement of aorta over ventricular-septal defect 4. ventricular-septal defect |
|
|
|
What is the clinical presentation and diagnostic workup of tetralogy of fellot?
|
CLINICAL PRESENTATION:
easy fatigability exertional dyspnea cyanotic spells characterized by: 1. sudden onset of cyanosis or deepening of cyanosis 2. dyspnea 3. altered consciousness ranging from irritability to syncope 4. decrease or disappearance of systolic ejection murmur d/t complete obstruction of right ventricular outflow tract squatting (though rare since often diagnosed at birth) cyanosis clubbing palpable RV lift rough systolic ejection murmur at left sternal border in 3rd ICS, radiates to back DIAGNOSTIC WORKUP: CBC → polycythemia 2° to chronic arterial desaturation CXR EKG ECHO |
|
|
|
What is rheumatic fever?
|
complication of strep throat or scarlet fever
|
|
|
|
What is the etiology of rheumatic fever?
|
strep throat
scarlet fever uncommon in United States |
|
|
|
What is the clinical presentation of rheumatic fever?
|

recent infection
fatigue fever erythema marginatum → erythematous rings mostly on trunk that disappear and reappear over weeks to months subcutaneous nodules → small painless nodules on extensor surfaces chorea → abrupt nonrhythmic involuntary movements and muscular weakness carditis polyarthritis |
|
|
|
What is the diagnostic workup of rheumatic fever?
|
↑ ESR
↑ CRP ↑ ASO → repeat in 10-14 days if normal ↑ PR interval on EKG → repeat in 2 weeks and 2 months if abnormal also order: CBC BC if febrile throat culture CXR echocardiogram → repeat in 1 month if negative |
Current
Harrisons |
|
|
What is the diagnostic (Jones) criteria of rheumatic fever?
|
recent strep throat + 2 major criteria or 1 major and 2 minor criteria
Major: erythema marginatum subcutaneous nodules pericarditis, myocarditis, or endocarditis polyarthritis chorea Minor: hx of rheumatic fever or rheumatic heart disease fever arthralgias ↑ ESR ↑ CRP ↑ ASO ↑ PR interval on EKG |
Current EMED ch19
|
|
|
What is the most common symptom of rheumatic fever?
|
arthritis
|
|
|
|
What is the management of rheumatic fever?
|
1. for strep throat → benzathine penicillin G 1.2 million units IM single dose
2. if penicillin allegy → erythromycin 40mg/kg daily 3. for fever and arthritis → aspirin 4. if refractory to aspirin → corticosteroids 4. bed rest until afebrile and resting HR, ESR, and EKG normal 5. to prevent recurrence → benzanthine penicillin G 1.2 million units IM every 4 weeks -if no carditis → continue until 21 y/p -if carditis + no valvular damage → continue for 10 years -if carditis + valvular damge → continue for 10 years or until 40y/o if high risk for reexsposure of strep throat (parent, teacher, medical professional, military personnel) If chorea: 1. provide calming environment 2. medications only control symptoms but do not alter duration or outcome 3. carbamazepine → may not see effect for 2 weeks, continue for 2 weeks after symptoms subside If HF: see HF management |
Current ch10
|
|
|
Who is most commonly affected by rheumatic fever?
|
children 5-15y/o
|
Current ch10
|
|
|
What are the complications of rheumatic fever?
|
1. CHF
2. rheumatic heart disease 3. myocardial involvement 4. arrhythmia 5. pericardial effusion 6. rheumatic pneumonitis |
Current ch10
|
|
|
True or false, increasing HR decreases cardiac output?
|
true
|
|
|
|
What are causes of increased HR?
|
stress, anxiety, body temperature, hormones (thyroxine, epinephrine, norepinephrine), medications
|
|
|
|
What is pulsus alternans?
|
pulse with alternating strong and weak beats
|
|
|
|
What is the ddx of pulsus alternans?
|
LT-sided HF
LT ventricular failure low ejection fraction pericardial effusion asthma |
|
|
|
*What is the etiology of endocarditis?
|
1. community acquired:
2. hospital acquired: UTI, catheter infection, or nosocomial wound → bacteremia → endocarditis 3. prosthetic valve infection 4. IV drug use |
|
|
|
*What is the clinical presentation of endocarditis?
|
fever
murmur osler's nodes subungual hemorrhages |
|
|
|
What is the diagnostic workup of endocarditis?
|
BC x 3
echocardiography |
Current ch118
|
|
|
*What is the management of endocarditis?
|
1. antibiotic therapy → dependent on BC results
|
|
|
|
What is the general ddx for chest pain?
|
cardiac
pulmonary musculoskeletal esophageal/GI anxiety |
|
|
|
What is another name for thromboangiitis obliterans?
|
Buerger's disease
|
Current ch12
|
|
|
What is thromboangiitis obliterans?
|

disease characterized by blood vessel inflammation and thrombosis
often resulting in blood vessel obstruction of the hands or feet |
|
|
|
Who is most commonly affected by thromboangiitis obliterans?
|
20-40 y/o male smokers
|
Current ch12
|
|
|
What is the etiology of thromboangiitis obliterans?
|
cause unknown
associated with smoking |
Current ch12
|
|
|
What are the complications of thromboangiitis obliterans?
|
necrosis → amputation
|
|
|
|
What is the management of thromboangiitis obliterans?
|
1. stop smoking to prevent amputation
2. avoid cold temperatures to prevent reduced circulation |
|
|
|
Define dyspnea.
|
SOB; subjective difficulty in breathing
|
|
|
|
Define orthopnea.
|
SOB lying down that is relieved when upright
|
|
|
|
Define paroxysmal nocturnal dyspnea.
|
sudden SOB upon waking
|
|
|
|
Define rubor.
|
red discoloration of skin
|
|
|
|
Define pallor.
|
pale skin
|
|
|
|
Define cyanosis.
|
bluish discoloration of skin
|
|
|
|
Define diaphoresis.
|
sweating
|
|
|
|
Define syncope.
|
fainting
|
|
|
|
What is the etiology of secondary HTN?
|
KIDNEY:
chronic kidney disease renal vascular HTN/disease ENDOCRINOPATHIES: thyroid disease parathyroid disease Cushing syndrome primary hyperaldosteronism pheochromocytoma DRUGS: alcohol NSAIDs decongestants corticosteroids cocaine methamphetamines sleep apnea aortic coarctation |
|
|
|
*What is the diagnostic workup of HTN?
|
Hct
BMP -glucose - diabetes screening -BUN/CREAT - kidney disease? -calcium - parathyroid disease LIPID - UA - glucose, protein? EKG - LVH? |
|
|
|
What is the etiology of occlusive disease of the lower extremeties?
|
atherosclerosis
associated with: smoking DM |
Current ch12
|
|
|
What is the clinical presentation of occlusive disease of the lower extremeties?
|
intermittent claudication of calf → exacerbated by exercise, relieved by rest
dependent rubor of foot with blanching upon elevation reduced skin temp atrophic changes → hair loss, thinning of skin, muscle atrophy, ulcerations (think toes!) decreased pulses |
Current ch12
|
|
|
Define natriuresis.
|
excretion of sodium in urine
|
|
|
|
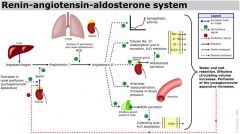
Describe the renin-angiotensin-aldosterone system.
|
|
|
|
|
What is the etiology of an aortic aneurysm?
|
result from abnormal production or degradation of structural components (elastin and collagen) of aorta
associated with: genetic or developmental diseases trauma → penetrating or non-penetrating chest trauma infection → syphilis, TB vasculitis → giant cell arteritis, Takayasu arteritis spondyloarthrapathies degenerative diseases → associated with atherosclerosis |
|
|
|
What is the clinical presentation of an aortic aneurysm?
|
Thoracic:
often asymptomatic chest pain SOB cough dysphagia hoarseness → due to stretching of recurrent laryngeal nerve Abdominal: often asymptomatic palpable, pulsatile, nontender mass if painful → impending rupture → surgical emergency!!! pain may refer to chest, back, or scrotum |
Harrisons ch242
|
|
|
What is the diagnostic workup of an aortic aneurysm?
|
Thoracic:
CXR → widening of mediatinal shadow, displacement or compression of trachea or left mainstem bronchus CT Abdominal: CT or abdominal ultrasound |
Hairrons ch242
|
|
|
What is the initial management of an aortic aneurysm?
|
Thoracic:
1. long-term B-blocker 2. if symptomatic, >5.5cm, or growing >1cm per year → surgery 3. if Marfan syndrome + >5cm → surgery 4. if asymptomatic → monitor with CT every 6-12 months Abdominal: 1. if symptomatic, expanding, or >5.5.cm → surgery |
Harrisons ch242
|
|
|
What is an aortic aneurysm?
|
pathological dilation of the aorta
|
|
|
|
90% of abdominal aortic aneurysms are related to?
|
atherosclerosis
|
Harrisons ch242
|
|

|
widening of aortic shadow → thoracic aortic aneurysm
|
|
|
|
What is aortic dissection?
|
spontaneous tear in intima (inner) layer of aorta
|
Current ch12
|
|
|
What is the etiology of aortic dissection?
|
spontaneous
associated with: HTN (most common) pregnancy bicuspid aortic valve coarcation abnormalities of smooth muscle, collagen, and elastin |
Current ch12
|
|
|
What is the clinical presentation of aortic dissection?
|
sudden severe persistent chest pain
radiation to back, neck, or abdomen HTN peripheral pulses diminished or unequal possible diastolic murmur due to aortic regurgitation |
Current ch12
|
|
|
What is the diagnostic workup of aortic dissection?
|
EKG → LVH from long-standing HTN common
CXR → widened superior mediastinum *CT → chest and abdomen |
Current ch12
|
|
|
What is the intial treatment of aortic dissection?
|
EMERGENCY!!!
1. if suspected aortic dissection → aggressively lower BP via B-blocker (start even before diagnostic complete) 2. if type A or complicated type B → emergency surgery |
Current ch12
|
|
|
What are 3 things you need to determine when talking about arrhythmias?
|
1. narrow or wide QRS complex
2. regular or irregular 3. normal, bradycardia, or tachycardia |
|
|
|
What is the etiology of sinus arrhythmia?
|
normal in children and young adults
enhancement of vagal tone → digoxin, morphine early sick sinus syndrome |
Current Cardiology ch20
|
|
|
What is the management of sinus arrhythmia?
|
benign → no treatment necessary
|
Current Cardiology ch20
|
|
|
What is the etiology of pulmonary HTN?
|
primary → idiopathic; associated with genetic factors
secondary → most common in younger women |
|
|
|
What is the clinical presentation of pulmonary HTN?
|
cyanosis
dyspnea right ventricle heave elevated JVP |
|
|
|
What is the diagnostic workup of pulmonary HTN?
|
CXR → enlarged pulmonary arteries
echocardiography → often diagnostic |
|
|
|
What is normal pulmonary arterial pressure?
|
~25/9 mmHg
|
http://tiny.cc/merckBP
|
|
|
*What is the etiology of cor pulmonale?
|
pulmonary disease → most commonly COPD
pulmonary HTN |
|
|
|
What is unstable angina?
|
angina pectoris with at least one of the following features:
1. occurs at rest or with minimal exertion, usually lasting >10 min 2. severe and of new onset (within last 4-6 weeks) 3. increasingly becomes more severe, prolonged, or frequent |
|
|
|
What is stable angina pectoris?
|
1. chest or arm discomfort
2. associated with physical exertion or stress 3. relieved by 5-10 min rest or sublingual nitroglycerin |
|
|
|
What is NSTEMI?
|
presentation of unstable angina + elevated cardiac biomarkers indicating myocardial necrosis
|
|
|
|
What are 3 sources of BP measurement error?
|
clinician
equipment technique http://tiny.cc/bp124 |
|
|
|
What are Korotkoff sounds?
|
sounds heard when measuring BP
|
|
|
|
Describe how to accurately measure BP.
|
ensure patient hasn't recently ingested caffeine, eaten food, or smoked cigarettes
ensure patient doesn't have full bladder explain procedure to reduce anxiety allow patient to quietly rest for 5 minutes position patient correctly: have patient sit with back supported, midpoint of arm at heart level, legs uncrossed, feet on floor use proper cuff size: bladder length should encircle 80% of adult's arm or 100% of child's arm; width should encircle 40% of adult’s arm position cuff correctly: do not measure over clothing, snug fit, 1in above antecubital space, middle of bladder over brachial artery take BP in warm, quiet room do not measure when patient talking palpate radial pulse and pump cuff to estimate systolic BP, pulse will disappear at systolic BP place bell of stethoscope over brachial artery rapidly inflate cuff 30mmHg above estimated systolic BP deflate cuff 2-3 mm/sec when sounds audible, deflate cuff 2 mmHg/pulse beat continue slow deflation for 10 mmHg after last Korotkoff sounds heard to detect auscultory gap rapidly and completely deflate cuff do not inflate/deflate too slowly or quickly record phase I (systolic BP) and phase V sounds (diastolic BP), do not round in children or when sounds are heard nearly to 0 in adults, record phase IV sounds (ex: 136/64/10) wait ≥30 sec to repeat or measure opposite arm average measurements if >1 BP taken http://tiny.cc/bp124 |
|
|
|
What are the phases of Korotkoff sounds?
|
phase I: when sounds appear = systolic BP
phase II: clinically insignificant phase III: clinically insignificant phase IV: muffled sounds phase V: when sounds disappear = diastolic BP http://tiny.cc/bp124 |
|
|
|
Is the stethoscope diaphragm more effective at transmitting low or high frequency sounds?
|
high frequency
|
|
|
|
What are examples of high frequency sounds?
|
splitting of sounds
opening snaps aortic diastolic murmurs |
|
|
|
Do you press lightly or firmly when using the stethoscope diaphragm?
|
firmly
|
|
|
|
Do you press lightly or firmly when using the stethoscope bell?
|
lightly
|
|
|
|
Is the stethoscope bell more effective at transmitting low or high frequency sounds?
|
low frequency
|
|
|
|
What are examples of low frequency sounds?
|
bruits
diastolic murmur of mitral stenosis 3rd and 4th heart sounds |
|
|
|
Define precordium.
|
chest area overlying heart
|
Mosbys p414
|
|
|
Define dextrocardia.
|
heart located on RT side of body in mirror image of normal LT-sided heart
|
Mosbys p414
|
|
|
Define situs inversus.
|
heart and stomach found on LT side of body and liver on RT side
|
Mosbys p414
|
|
|
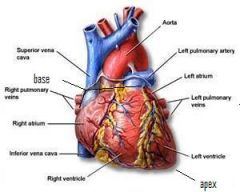
List the layers of the heart and their functions.
|
pericardium → outermost layer; fibrous double-walled sac encasing and protecting heart
myocardium → middle layer; muscular layer providing pumping action epicardium → innermost layer; lines heart chambers and valves |
Mosbys p414
|
|
|
What is the function of the atria?
|
collecting of blood
|
|
|
|
What is the function of the ventricles?
|
pumping of blood
|
|
|
|
|
|
|
|
List the pathway of blood starting from the body.
|
veins returning CO2 → superior/inferior vena cava → RT atrium → tricuspid valve → RT ventricle → pulmonic valve → pulmonary trunk → LT/RT pulmonary arteries → lungs → exchanges CO2 for O2 → LT/RT pulmonary veins → RT atrium → mitral valve → RT ventricle → aortic valve → ascending aorta → aortic arch → descending aorta → arteries supplying O2
|
|
|
|
Where is PMI normally seen?
|
LT mid-clavicular line in 5th ICS while sitting
*if in more than 1 ICP or seen while supine → suggest problem |
|
|
|
Define systole.
|
phase of cardiac cycle characterized by ventricular contraction and atrial filling
|
|
|
|
Define diastole.
|
phase of cardiac cycle characterized by atrial contraction and ventricular relaxation
|
|
|
|
What equipment is needed for the cardiac exam?
|
marking pen
cm ruler stethoscope |
|
|
|
Describe the cardiac exam.
|
1. inspect precordium
2. inspect PMI → use tangential light at level of chest 3. palpate PMI → assess for heaves/lifts 4. measure PMI to midsternal line 5. palpate for thrills 6. auscultate with diaphragm 7. auscultate with bell 8. ask patient to lean forward and exhale → auscultate with diaphragm over aortic valve 9. auscultate with bell over |
|
|
|
List signs of HF.
|
crackles
hepatomegaly peripheral edema |
Mosbys p428
|
|
|
Absent apical impulse + faint heart sounds may indicate?
|
pleural effusion
pericardial effusion |
Mosbys p429
|
|
|
Apical impulse that is more forceful and widely distributed, fills systole, or inferolaterally displaced may indicate?
|
increased cardiac output
LT ventricular hypertrophy |
Mosbys p430
|
|
|
A lift along the LT sternal border may indicate?
|
RT ventricular hypertrophy
|
Mosbys p430
|
|
|
Loss of apical impulse may indicate?
|
overlying air or fluid → pneumothorax, pleural effusion, pericardial effusion
displacement of heart beneath sternum |
Mosbys p430
|
|
|
Displacement of apical impulse to right + no loss of thrust may indicate?
|
dextrocardia
diaphragmatic hernia distended stomach pulmonary abnormality |
Mosbys p430
|
|
|
Define thrill.
|
palpable murmur
|
Mosbys p431
|
|
|
Thrill + systole + suprasternal notch and/or RT 2nd-3rd ICS suggests?
|
aortic stenosis
|
Mosbys p431
|
|
|
Thrill + systole + suprasternal notch and/or LT 2nd-3rd ICS suggests?
|
pulmonic stenosis
|
Mosbys p431
|
|
|
Janeway lesions indicate?
|
bacterial endocarditis
|
|
|
|
Define S1.
|
first heart sound characterized by "lubb" sound caused by closing of tricuspid and mitral valves
|
Mosbys p419
|
|
|
Which is normally silent, opening or closing of heart valves?
|
opening
|
Mosbys p419
|
|
|
Define S2.
|
second heart sound characterized by "dubb" sound caused by closing of pulmonic and aortic valves
|
Mosbys p419
|
|
|
What are the 2 parts of S2?
|
A2 → closing of aortic valve
P2 → closing of pulmonic valve |
Mosbys p419
|
|
|
Define S3.
|
occasional third heart sound caused by filling of ventricles during diastole
|
Mosbys p419
|
|
|
Define S4.
|
occasional fourth heart sound caused by atrial kick
|
Mosbys p419
|
|
|
What grade murmur is a thrill?
|
grade IV
|
Mosbys p431
|
|
|
Thrill + systole + LT 4th ICS may indicate?
|
ventricular septal defect
|
Mosbys p431
|
|
|
Thrill + systole + apex may indicate?
|
mitral regurgitation
|
Mosbys p431
|
|
|
Thrill + systole + LT lower sternal border may indicate?
|
tetralogy of fallot
|
Mosbys p431
|
|
|
Thrill + systole + LT upper sternal border +/- radiation may indicate?
|
patent ductus arteriosus
|
Mosbys p431
|
|
|
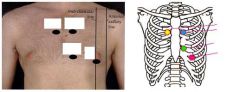
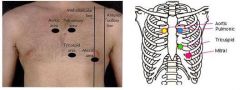
List the 5 locations for auscultating the heart.
|
RT 2nd ICS at sternal border → aortic valve
LT 2nd ICS at sternal border → pulmonic valve LT 3rd ICS at sternal border → Erb's point LT 4th ICS at sternal border → tricuspid valve LT 5th ICS at midclavicular line → mitral valve (PMI) |
Mosbys p433
|
|
|
What can you do to figure out if thrill corresponds with systole or diastole?
|
palpate carotid pulse which coincides with S1
|
|
|
|
What is the etiology of a thrill based on timing and location?
|

|
|
|
|
|
|
|
|
How can you differentiate S1 from S2?
|
period between S1 and S2 is twice as quick as period between S2 and S1
|
|
|
|
Define thrombosis.
|
formation of a blood clot
|
|
|
|
Define infarction.
|
vascular obstruction → tissue hypoxia → tissue necrosis
|
|
|
|
Define hypoxia.
|
inadequate O2 supply to body or tissue
|
|
|
|
Define anoxia.
|
complete O2 deprivation
|
|
|
|
Define hypoxemia.
|
abnormally low [blood O2]
|
|
|
|
Define stroke volume.
|
volume of blood pumped from one ventricle of the heart with each beat
|
|
|
|
How do you calculate cardiac output?
|
SV X HR = CO
|
|
|
|
The jugular veins help you evaluate?
|
RT side of heart
|
|
|
|
List risk factors of varicose veins.
|
women 4x > men
genetic predisposition → Irish or German descent, mother with varicosities age → veins become less elastic as age race → whites > blacks sedentary lifestyle → allows blood to pool and veins to be compromised |
Mosbys p467
|
|
|
Describe the peripheral vascular exam.
|
1. inspect for JVD
2. inspect upper extremity -skin color -hair distribution -varicosities -ulcerations -cyanosis -clubbing 3. palpate upper extremity -temperature -skin texture -edema -capillary refill 4. assess pulses bilaterally -carotid -brachial -radial -ulnar 5. assess pulses -abdominal aorta -femoral 6. inspect lower extremity -skin color -hair distribution -varicosities -ulcerations -cyanosis -clubbing 7. palpate lower extremity -temperature -skin texture -edema -capillary refill 8. assess pulses bilaterally -popliteal -dorsalis pedis -posterior tibialis |
|
|
|
What are you assessing when palpating pulses for the peripheral vascular exam?
|
rhythm
amplitude symmetry |
|
|
|
How is the amplitude of pulses documented?
|
on scale of 0 to 4:
0 = absent, not palpable 1 = diminished, barely palpable 2 = expected 3 = full, increased 4 = bounding |
Mosbys p470
|
|
|
Define tachycardia.
|
HR > 100
|
Mosbys p470
|
|
|
Define bradycardia.
|
HR < 60
|
Mosbys p470
|
|
|
Define pulsus paradoxus.
|
arterial pulse amplitude decreases on inspiration
|
Mosbys p470
|
|
|
What is the ddx for pulsus paradoxus?
|
COPD
pericardial effusion constrictive pericarditis |
Mosbys p470
|
|
|
Define pulsus alternans.
|
arterial pulse amplitude that alternates from beat to beat with weak and strong beats
|
Mosbys p470
|
|
|
Pulsus alternans is associated with?
|
LT ventricular HF
|
Mosbys p470
|
|
|
What is the ddx for bounding pulse?
|
exercise
atherosclerosis aortic rigidity patent ductus arteriosus anemia hyperthyroidism fever anxiety |
Mosbys p470
|
|
|
An irregular regular HR may indicate?
|
sinus arrhythmia → increased HR on inspiration and decreased rate on expiration
|
Mosbys p470
|
|
|
Asymmetrical pulses suggests?
|
impaired circulation
|
Mosbys p470
|
|
|
Diminished femoral pulse may indicate?
|
aortic coarctation
|
Mosbys p470
|
|
|
What is aortic coarctation?
|
congenital condition characterized by narrowing of aorta where ductus arteriosus inserts
|
|
|
|
When auscultating for bruits, what should you ask the patient to do?
|
hold breath
|
Mosbys p472
|
|
|
What are the 5 Ps of arterial occlusion?
|
pain
paresthesias → if major artery occluded pallor pulselessness paralysis → rarely |
Mosbys p473
|
|
|
Compartment syndrome is characterized by?
|
pain
paresthesias pallor pulselessness paralysis |
Mosbys p473
|
|
|
What is the ddx for carotid bruit?
|
obstructive disease in carotid artery → athersclerosis, arteritis, fibromuscular hyperplasia
transmitted murmurs → aortic stenosis, severe aortic regurgitation, ruptured chordae tendinae of mitral valve vigorous LT ventricular ejection → more common in children |
Mosbys p472
|
|
|
Define claudication.
|
pain caused by muscle ischemia
|
|
|
|
How do you differentiate pain due to vascular insufficiency and pain due to musculoskeletal disorders?
|
Arterial:
onset during exercise quickly relieved by rest intensity increases with intensity and duration of exercise Venous and Musculoskeletal: onset during or several hours after exercise relieved by rest but sometimes only after hours or days greater variability than arterial pain in response to intensity and duration of exercise |
Mosbys p473
|
|
|
What is the range for normal BP?
|
<120/80 mmHg
|
http://tiny.cc/jncvii
|
|
|
What is the management for normal BP?
|
encourage lifestyle modification:
1. ↑ fruit, vegetables, and low-fat dairy 2. ↓ sodium, fat, and alcohol → <2 drinks/day for men and <1 drink/day for women 3. get 30 minutes of aerobic exercise daily → brisk walking 4. obtain normal BMI → 18.5-24.9 |
http://tiny.cc/jncvii
|
|
|
What is the BP range for pre-HTN?
|
120/80-139/89 mmHg
|
http://tiny.cc/jncvii
|
|
|
What is the managment for pre-HTN?
|
1. encourage lifestyle modification
2. no drug therapy unless compelling indication → DM, increased risk of coronary disease, post-MI, HF, chronic kidney disease |
http://tiny.cc/jncvii
|
|
|
What is the BP range for stage I HTN?
|
140/90-159/99 mmHg
|
http://tiny.cc/jncvii
|
|
|
What is the management for stage I HTN?
|
1. encourage lifestyle modification
2. prescribe thiazide diuretic |
http://tiny.cc/jncvii
|
|
|
What is the BP range for stage II HTN?
|
>160/100 mmHg
|
http://tiny.cc/jncvii
|
|
|
What is the management for stage II HTN?
|
1. encourage lifestyle modification
2. prescribe thiazide diuretic + either B-blocker, ACE inhibitor, ARB or CCB |
http://tiny.cc/jncvii
|
|
|
For BP management, what does "lifestyle modification" consist of?
|
1. ↑ fruit, vegetables, and low-fat dairy
2. ↓ sodium, fat, and alcohol → <2 drinks/day for men and <1 drink/day for women 3. get 30 minutes of aerobic exercise daily → brisk walking 4. obtain normal BMI → 18.5-24.9 |
http://tiny.cc/jncvii
|
|
|
For pre-HTN management, what qualifies as a "compelling indication" for drug therapy?
|
DM
increased risk of coronary disease post-MI HF chronic kidney disease |
http://tiny.cc/jncvii
|
|
|
Which is more common, essential HTN or secondary HTN?
|
essential (95%)
|
Current
|
|
|
What patient population is most commonly affected by isolated systolic HTN?
|
elderly
|
Primary Care Medicine p130
|
|
|
What is hypertensive urgency?
|
severely elevated BP with NO signs of end-organ damage
|
EMED Current
|
|
|
What is hypertensive emergency?
|
severely elevated BP with signs of end-organ damage → mental status changes, cardiac ischemia, CHF, or acute renal failure
|
EMED Current
|
|
|
What are the most important complications of HTN?
|
coronary heart disease
stroke HF end-stage kidney disease |
Current ch11
|
|
|
What is the etiology of essential HTN?
|
complex combination of genetic and environmental factors:
-sympathetic nervous system hyperactivity → young? -abnormal cardiac or renal development → low birth weight? -abnormal renin-angiotensin-aldosterone system -abnormal natriuresis -increased intracellular sodium and calcium -polycythemia -high salt intake -low potassium intake -high alcohol intake -cigarette smoking -obesity -sleep apnea -NSAIDs |
Current ch11
|
|
|
When should secondary HTN be suspected?
|
1. presents at early age
2. presents >50y/o 3. HTN previously controlled but now refractory to treatment |
Current ch11
|
|
|
When does essential HTN usually present?
|
25-55 y/o
|
Current ch11
|
|
|
What are the risk factors of essential HTN?
|
1. poor diet → low potassium, high sodium
2. sedentary lifestyle 3. alcohol 4. smoking 5. drugs → NSAIDs, decongestants, corticosteroids, oral contraceptives, cocaine, methamphetamines 6. obesity |
Current ch11
|
|
|
What is the full name for B-blockers?
|
beta-adrenergic blocking agents
|
|
|
|
List types of B-blockers.
|
propranolol
atenolol metoprolol |
|
|
|
What is the MOA of B-blockers?
|
decrease activation of B1-adrenergic receptors on heart → decreasing cardiac output → decreasing BP
decrease renin → decreasing angiotensin II → decreasing aldosterone → decreasing Na+ and water retention → decreasing blood volume → decreasing cardiac output → decreasing BP |
Pharmacology p220
|
|
|
What B-receptors do propranolol, atenolol, and metoprolol effect?
|
propranolol → decrease activation of B1 and B2
atenolol → decrease activation of B1 metoprolol → decrease activation of B1 |
Pharmacology p220
|
|
|
What are the contraindications for propranolol?
|
asthma → due to blockade of B2-mediated brochodilation
|
Pharmacology p220
|
|
|
What are the indications for B-blockers?
|
HTN in young white patients
HTN + concomitant diseases such as migraine HA, angina pectoris, previous MI, chronic HF, supraventricular tachyarrhythmia |
Pharmacology p221
|
|
|
What does ACE inhibitors stand for?
|
angiotensin converting ezyme inhibitors
|
|
|
|
List types of ACE inhibitors.
|
lisinopril
captopril benazepril enalapril quinapril |
|
|
|
What class of drugs end in -olol?
|
B-blockers
|
|
|
|
What class of drugs end in -pril?
|
ACE inhibitors
|
|
|
|
What is the MOA of ACE inhibitors?
|
inhibit ACE → leading to decreased angiotenin II (and subsequent decreased vasoconstriciton) and increased bradykinin (and subsequent vasodilation)
ACE normally converts angiotensin I into angiotensin II leading to vasoconstriction ACE also normally breaksdown bradykinin bradykinin is a vasodilator |
Pharmacology p222
|
|
|
What are the indications for ACE inhibitors?
|
HTN in young white patients
if used with diuretic → effect in black patients similar to white patients post-MI HF diabetic neuropathy albuminuria |
Pharmacology p222
|
|
|
What are the adverse effects of ACE inhibitors?
|
dry cough
fever rash hyperkalemia hypotension angioedema or first-dose syncope → administer first dose under close observation of patient |
Pharmacology p222
|
|
|
What are the contraindications of ACE inhibitors?
|
pregnancy
K supplementation K-sparing diuretics |
Pharmacology p222
|
|
|
What class of drug ends in -artan?
|
ARBs
|
|
|
|
What does ARB stand for?
|
angiotensin II receptor blockers
|
|
|
|
List types of ARBs.
|
losartan
valsartan |
|
|
|
What are the adverse effects of ARBs?
|
similar to ACE inhibitors → fever, hypotension, skin rash, hyperkalemia
but compared to ACE inhibitors, risk of cough and angioedema significantly decreased |
Pharmacology p223
|
|
|
What are the indications for ARBs?
|
alternative to ACE inhibitors
(i.e. if chronic cough) HTN + diabetes → reduce nephrotoxicity of diabetes |
Pharmacology p223
|
|
|
What are the contraindications for ARBs?
|
pregnancy
|
Pharmacology p223
|
|
|
What is the treatment for ischemic heart disease?
|
B-blocker
anti-platelet smoking cessation exercise weight loss treatment of diabetes and hyperlipidemias if not well-controlled by B-blocker alone or B-blocker contraindicated → add or substitute CCB if still not-well controlled → add nitrates |
JNCVII
|
|
|
What should be prescribed for HTN + HF?
|
ACE inhibitor, B-blocker, and diuretic
if intolerant to ACE inhibitor → substitute ARB if severe LT ventricular dysfunction → aldosterone anatagonist → spironolactone |
JNCVII
|
|
|
What is the BP goal for hypertensive diabetics?
|
130/80 mmHg
|
JNCVII
|
|
|
What should be prescribed for HTN + DM?
|
thiazide diuretic, ACE inhibitor
B-blockers useful in combination CCB useful in combination |
JNCVII
|
|
|
What is the BP goal for patients with HTN and chronic kidney disease?
|
130/80 mmHg
|
JNCVII
|
|
|
What should be prescribed for HTN + chronic kidney disease?
|
ACE inhibitor or ARB + loop diuretic
|
JNCVII
|
|
|
How do the effectiveness of B-blockers, ACE inhibitors, and ARBs compare in blacks and whites?
|
monotherapy of B-blocker, ACE inhibitor or ARB less effective in blacks than whites
if combined with diuretic, these differences are abolished ACE inhibitor less effective than either thiazide diuretic or CCB in blacks |
|
|
|
How do the adverse effects of ACE inhibitors compare in blacks and whites?
|
risk of angioedema 3-4 times higher in blacks than whites
risk of cough higher in blacks than whites |
|
|
|
What are the adverse effects of B-blockers?
|
CNS → fatigue, lethargy, insomnia, hallucinations
hypotension bradycardia sexual dysfunction → decreased libido or impotence |
Pharmacology p221
|
|
|
Discuss the approach to modifying treatment when antihypertensive agents adversely affect sexual function?
|
to decrease risk of erectile dysfunction → encourage smoking cessasation, exercise, and weight loss
if erectile dysfunction occurs as a result of therapy → discontinue offending agent and prescribe a different one |
JNCVII
|
|
|
List types of CCBs.
|
verapamil
diltiazem nifedipine amlodipine |
|
|
|
What are the indications for CCBs?
|
verapamil → migraine HA, HTN, angina, supraventricular tachyarrhythmias
diltiazem → HTN, angina, supraventricular tachyarrhythmia nifedipine and amlodipine → HTN, angina overall useful in HTN with asthma, diabetes, angina or PVD blacks respond well |
Pharmacology p223
|
|
|
What is the MOA of CCBs?
|
block calcium channels → vasodilation of coronary vessels
|
Pharmacology p223
|
|
|
What are the adverse effects of CCBs?
|
verapamil → constipation
nifedipine and amlodipine → fatigue, dizziness, HA, hypotension |
Pharmacology p223
|
|
|
What are the contraindications for verapamil?
|
CHF
AV block |
Pharmacology p223
|
|
|
What class of drugs ends in -zosin?
|
alpha-blockers
|
|
|
|
Lists types of alpha blockers.
|
doxazosin
prazosin terazosin |
|
|
|
What is the MOA of alpha blockers?
|
block alpha 1 adrenergic receptors → decreasing peripheral vascular resistance and lowering BP by relaxation of arterial and venous smooth muscle
|
|
|
|
What are the indications for prazosin?
|
mild-to-moderate HTN
prescribed in combination with propranolol or a diuretic |
Pharmacology p225
|
|
|
What are the adverse effects of prazosin?
|
reflex tachycardia
first-dose syncope |
Pharmacology p225
|
|
|
What are the indications for alpha-blockers?
|
seldom used to treat HTN
|
Pharmacology p225
|
|
|
List central alpha agonists.
|
clonidine
guanabenz methyldopa |
|
|
|
What are the indications for clonidine?
|
HTN refractory to treatment with 2 or more drugs
useful in HTN + renal disease → does not decrease renal blood flow or glomerular filtration |
Pharmacology p225
|
|
|
What are the adverse effects of clonidine?
|
sedation
drying of nasal mucosa rebound HTN if withdrawn → so withdraw slowly |
Pharmacology p226
|
|
|
What are the indications for methyldopa?
|
HTN + renal insufficiency
|
Pharmacology p226
|
|
|
What type of drug is hydralazine?
|
vasodilator → acting primarily on arteries and arterioles → decreasing peripheral resistance → reflex increase in HR and cardiac output
|
Pharmacology p226
|
|
|
What are the indications for hydralazine?
|
moderately severe HTN → prescribe with B-blocker (to balance reflex tachycardia) and loop diuretic (to decrease sodium retention)
pregnancy-induced HTN |
Pharmacology p226
|
|
|
What are the adverse effects of hydralazine?
|
HA, nausea, sweating, tachycarida, arrhythmia, angina
|
Pharmacology p226
|
|
|
What are the indications for minoxidil?
|
severe to malignant HTN refractory to other drugs → prescribe with B-blocker (to balance reflex tachycardia) and loop diuretic (to decrease sodium retention)
|
Pharmacology p226
|
|
|
What are the adverse effects of minoxidil?
|
sodium and water retention volume overload, edema, and CHF
|
Pharmacology p226
|
|
|
What does NCEP stand for?
|
National Cholesterol Education Program
|
http://tiny.cc/ncep
|
|
|
What is the goal of NCEP?
|
"The goal of the NCEP is to contribute to reducing illness and death from coronary heart disease (CHD) in the United States by reducing the percent of Americans with high blood cholesterol."
|
http://tiny.cc/ncep
|
|
|
What are the NCEP guidelines for 1° prevention screening in adults?
|
fasting lipid profile (total cholesterol, LDL, HDL, triglycerides) for all adults >20 y/o every 5 years
|
http://tiny.cc/ncep1
|
|
|
What are the ranges for optimal, borderline, and high total cholesterol?
|
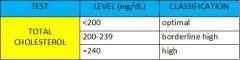
|
National Heart, Lung & Blood Institute - http://tiny.cc/ncep
NCEP Guidelines - http://tiny.cc/ncep1 Lab Tests Online - http://tiny.cc/lipid |
|
|
What are the ranges for optimal, near optimal, borderline high, high, and very high LDL cholesterol?
|
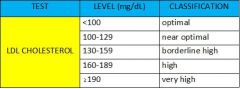
|
National Heart, Lung & Blood Institute - http://tiny.cc/ncep
NCEP Guidelines - http://tiny.cc/ncep1 Lab Tests Online - http://tiny.cc/lipid |
|
|
If a patient does not fast for a lipid profile, which tests are valid and what are the indications for ordering a follow-up lipid profile?
|
only total cholesterol and HDL are valid
order a follow-up lipid profile if total cholesterol >200 mg/dL or HDL <40 mg/dL |
http://tiny.cc/ncep1
|
|
|
List risk factors for atherosclerosis.
|
1. >45y/o for men and >55y/o for women
2. FH of early heart disease 3. poor diet → high in saturated fat, trans fat, sodium, and sugar 4. lack of exercise 5. smoking 6. overweight or obesity 7. HTN 8. hyperlipidemia 9. DM |
http://tiny.cc/nhlbi-atherosclerosis
|
|
|
What is familial hypercholesterolemia?
|
lipid disorder characterized by defective or absent cell-surface receptors for LDL resulting in unregulated synthesis of LDL
if heterozygous for this disorder → LDL concentrations are 2x normal; presents in 3rd-4th decade if homozygous for this disorder → LDL concentrations 8x normal; presents in childhood HMG CoA reductase inhibitors and bile-acid sequestrants not effective in treating this disorder |
Current p1123
|
|
|
What is familial hyperchylomicronemia?
|
lipid disorder characterized by an abnormality in lipoprotein lipase
lipoprotein lipase normally enables peripheral tissues to take up triglyceride from VLDL particles and chylomicrons |
Current p1123
|
|
|
What is the clinical presentation and diagnostic workup of familial hyperchylomicronemia?
|
presents in childhood with recurrent hepatosplenomegaly and pancreatitis
LIPID panel → hypertriglyceridemia |
Current p1123
|
|
|
Do modest amounts of alcohol (1-2 ounces) increase or decrease HDL cholesterol?
|
increase
|
Current p1130
|
|
|
What is the normal range for triglycerides?
|
<150 mg/dL
|
Current p1133
|
|
|
High triglycerides increases the risk for what condition?
|
pancreatitis
|
Current p1133
|
|
|
What is the management of hypertriglyceridemia?
|
1. goal → TRIG <150 mg/dL; reduce risk of cardiovascular disease and pancreatitis
2. secondary causes → ask about alcohol, oral contraceptives, diuretics; BMP for chronic kidney disease; A1C for DM; obesity 2. dietary modification → restrict total calories; avoid alcohol, simple sugars, refined starches, and saturated/trans fats 3. exercise 4. if TRIG >500 mg/dL + refractory to dietary modification → prescribe triglyceride-lowering drug → fibric acid derivative, niacin, or HMG CoA reductase inhibitor |
Current p1133
|
|
|
What are the ranges for borderline high, high, and very high triglycerides?
|
borderline high: 150-199 mg/dL
high: 200-499 mg/dL very high: ≥500 mg/dL |
http://tiny.cc/lipid
|
|
|
True or false, in a LIPID profile, if TRIG is too high, LDL cannot be calculated?
|
true
LDL cannot be calculated if TRIG >400 |
|
|
|
What should you order to determine LDL, if LDL cannot be calculated because TRIG is >400?
|
LDL direct
|
|
|
|
What is the management for elevated LDL?
|
1. goal → LDL <100; reduce risk of cardiovascular disease
2. secondary causes of total cholesterol → ask about alcohol/meds; order CMP, A1C, TSH obstructive liver disease chronic liver disease nephrotic syndrome DM hypothyroidism Cushing's syndrome alcohol oral contraceptives corticosteroids diuretics (short-term effects) B-blockers (short-term effects) 2. diet therapy → reduce total fat to 25-30% of calories, reduce saturated fat to <7% of calories, reduce cholestrol to <200mg/d, eat more fruits, vegetables, and fiber, could try mediterranean diet 3. prevention/risk factor modification -exercise 30 minutes per day -lose weight -reduce alcohol -stop smoking -control HTN -control DM |
|
|
|
List 2° causes of hypercholesterolemia.
|
obstructive liver disease
chronic liver disease nephrotic syndrome DM hypothyroidism Cushing's syndrome alcohol oral contraceptives corticosteroids diuretics (short-term effects) B-blockers (short-term effects) |
Current ch28
|
|
|
List 2° causes of decreased HDL.
|
sedentary lifestyle
obesity B-blockers (short-term effects) |
Current ch28
|
|
|
List 2° causes of hypertriglyceridemia.
|
obesity
chronic kidney disease DM alcohol oral contraceptives diuretics (short-term effects) |
Current ch28
|
|
|
List possible systolic murmurs.
|
aortic or pulmonic stenosis
mitral or tricuspid regurgitation |
|
|
|
Describe systole and diastole.
|
mitral and tricuspid valves close (S1)
aortic and pulmonic valves open ventricles eject blood aortic and pulmonic valves close (S2) mitral and triscuspid valves open ventricles fill with flood |
|
|
|
List possible diastolic murmurs.
|
mitral or tricuspid stenosis
aortic or pulmonic regurgitation |
|
|
|
What is another name for aortic stenosis?
|
systolic ejection murmur
|
|
|
|
Describe the murmur of aortic stenosis.
|
occurs between S1 and S2 → crescendo-decrescendo
S2 → paradoxically split, soft, or absent (since only pulmonic valve slamming shut) |
|
|
|
What is the clinical presentation of aortic stenosis?
|
syncope, angina, LT ventricular HF → all present on exertion
harsh murmur between S1 and S2 crescendo-decrescendo S2 paradoxically split, soft, or absent best heard at RT 2nd ICS radiation to carotid arteries parvus et tardus → weakened and delayed carotid pulse |
|
|
|
What is the etiology of aortic stenosis?
|
congenital biscuspid aortic valve → presents in middle/old age
degenerative aortic stenosis |
|
|
|
What are the HDL CHOLESTEROL ranges for increased risk, average risk, and less than average risk for coronary heart disease?
|
increased: <40 mg/dL for men or <50 mg/dL for women
average: 40-50 mg/dL for men and 50-59 mg/dL for women less than average: ≥60 for both men and women |
http://tiny.cc/lipid
|
|
|
What is the management of aortic stenosis?
|
surgery for all symptomatic patients with aortic stenosis
|
|
|
|
When is a lipid profile ordered?
|
to determine risk of coronary artery disease
|
http://tiny.cc/lipid
|
|
|
What is the prevention of aortic stenosis?
|
risk factors same as atherosclerosis
|
|
|
|
When is HS-CRP ordered?
|
cardiac risk assessment
|
http://tiny.cc/hscrp
|
|
|
What is the etiology of aortic regurgitation?
|
congential biscupsid valve
HTN endocarditis aortic root dilation → syphilis, Marfan's syndrome, aortic dissection ankylosing spondylitis reactive arthritis |
|
|
|
Where is CRP synthesized and then secreted?
|
liver then secreted into bloodstream
|
http://tiny.cc/hscrp
|
|
|
What is the clinical presentation of aortic regurgitation?
|
fatigue, exertional dyspnea, chest pain or LT ventricular HF
diastolic murmur occurs between S2 and S1 best heard along LT sternal border wide pulse pressure (i.e. distance between systolic and diastolic pressure widened since diastolic pressure cannot be maintained) bounding pulse -Corrigan's pulse → carotids -Musset sign → head bobs with pulse -Quinke pulse → nailbed capillary pulsations |
|
|
|
Which is more sensitive, CRP or HS-CRP?
|
HS-CRP
more accurately detects lower concentrations of CRP |
http://tiny.cc/hscrp
|
|
|
Describe the murmur of aortic regurgitation.
|
occurs between S2 and S1 during diastole
descrescendo best heard along left sternal border |
|
|
|
What does an elevated CRP indicate?
|
non-specific inflammation
|
http://tiny.cc/hscrp
|
|
|
What is the management of aortic regurgitation?
|
surgery
|
|
|
|
What is the difference b/w CRP and HS-CRP?
|
CRP detects elevated levels of CRP in patients w/ inflammation or infection
HS-CRP distinguishes b/w low normal and high normal levels of CRP in patients who are otherwise healthy |
http://tiny.cc/hscrp
|
|
|
What is the prevention of aortic regurgitation?
|
reduce risk factors for HTN
|
|
|
|
Should HS-CRP be ordered to determine cardiac risk in a patient w/ chronic inflammation?
|
no
HS-CRP only meaningful in patients who are otherwise healthy |
http://tiny.cc/hscrp1
|
|
|
What is the etiology of mitral stenosis?
|
pregnancy
congenital rheumatic fever endocarditis |
|
|
|
What is the clinical presentation of mitral stenosis?
|
exertional dyspnea, orthpnea, and PND
pulmonary HTN RT HF Afib |
|
|
|
Describe the murmur of mitral stenosis.
|
diastolic murmur
occurs between S2 and S1 opening snap (more severe the earlier the snap) apical rumble best heard at apex in LT lateral ducubitus position |
|
|
|
What is the management of mitral stenosis?
|
if Afib → warfarin
if mild-to-moderate + planning on pregnancy → surgery othewise surgery depends on symptoms and severity |
|
|
|
When do initial elevation, peak elevation, and normalization occur for MYGB, CK, CKMB, and TROP?
|

|
|
|
|
What is the etiology of mitral regurgitation?
|
ventricular dilation
mitral valve prolapse rheumatic fever endocarditis ischemic heart disease |
|
|
|
List procedures used in diagnosis of cardiac disorders.
|
CXR
CT of heart MRI with gadolinium contrast resting EKG stress EKG ambulatory EKG (Holter/event monitoring transthoracic ECHO transesophageal ECHO stress ECHO doppler US of extremities MUGA scan scintigraphy with thallium scan angiography cardiac catheterization |
|
|
|
What is the clinical presentation of mitral regurgitation?
|
if acute → no LT atrial dilation, but pulmonary congestion
if chronic → LT atrial dilation, fatigue, dyspnea systolic murmur occurs between S1 and S2 pansystolic possible S3 best heard at apex radiating into axilla can lead to Afib |
|
|
|
Describe the murmur of mitral regurgitation.
|
systolic murmur
occurs between S1 and S2 pansystolic associated with S3 if large regurgant volume best heard at apex radiating into axilla |
|
|
|
What is the management of mitral regurgitation?
|
surgery
|
|
|
|
Describe the murmur of mitral valve prolapse.
|
systolic murmur
pansystolic or late-systolic single or multiple mid-systolic clicks |
|
|
|
What is the clinical presentation of mitral valve prolapse?
|
usually asymptomatic
fatigue, dyspnea, palpitations, chest pain systolic murmur pansystolic or late-systolic single or multiple mid-systolic clicks skeletal changes → straight back, pectus, scoliosis hyperreflexes |
|
|
|
What is the etiology of mitral valve prolaspe?
|
common in thin females
dilated aortic root Marfan's syndrome |
|
|
|
What is the management of mitral vavle prolapse?
|
mitral valve repair
B-blocker if arrhythmia |
|
|
|
Describe the murmur of tricuspid stenosis.
|
diastolic murmur
rumble mimicking mitral stenosis louder with inspiration best heard at LT lower sternal border |
Current ch10
|
|
|
What is the etiology of tricuspid stenosis?
|
rheumatic fever (less common in U.S.)
carcinoid disease iatrogenic → tricuspid valve repair or replacement more common in women |
Current ch10
|
|
|
What is the clinical presentation of tricuspid stenosis?
|
diastolic murmur
rumble mimicking mitral stenosis louder with inspiration best heard at LT lower sternal border may lead to RT HF → elevated JVP (giant a wave), hepatomegaly, ascities, dependent edema |
Current ch10
|
|
|
What is the management of tricuspid stenosis?
|
1. diuretic for edema → torsemide if gut edema → better abosorbed than furosemide
2. aldosterone inhibitor if hepatomegaly or ascites 3. surgery → bioprosthetic valve replacement |
Current ch10
|
|
|
Describe the murmur of tricuspid regurgitation.
|
systolic murmur
pansystolic increases with inspiration possible S3 best heard at LT parasternal border |
|
|
|
What is the etiology of tricuspid regurgitation?
|
pulmonary or cardiac disease, especially if pulmonary HTN present
|
|
|
|
What is the clinical presentation of tricuspid regurgitation?
|
systolic murmur
pansystolic increases with inspiration possible S3 best heard at LT parasternal border systolic c-v wave in JVP symptoms of RT HF → hepatomegaly, ascites, peripheral edema cyanosis |
|
|
|
What is the management of tricuspid regurgitation?
|
1. treat edema → torsemide, aldosterone inhibitor
2. treat underlying problem → LT heart disease, pulmonary HTN etc. 3. surgery → bioprosthetic valve replacement if also need to replace mitral valve |
|
|
|
What is dilated cardiomyopathy?
|
condition characterized by LV dilation + systolic dysfunction (EF <50%)
|
Current ch10
|
|
|
What is the etiology of dilated cardiomyopathy?
|
often idiopathic
genetic diseases postpartum myocarditis endocrinopathies alcoholism doxirubicin major catecholamine discharge most common in black men |
Current ch10
|
|
|
What is the clinical presentation of dilated cardiomyopathy?
|
gradual signs of left ventricular HF or bi-ventricular HF: dyspnea
crackles cardiomegaly S3 gallop rhythm ↑ JVP peripheral edema ascites |
Current ch10
|
|
|
What is the diagnostic workup of dilated cardiomyopathy?
|
EKG → ST-T changes, conduction abnormalities, ventricular ectopy
CXR → cardiomegaly, pulmonary edema echocardiogram → LV dilation and dysfunction |
Current ch10
|
|
|
What is the initial management of dilated cardiomyopathy?
|
1. refer to cardiologist
2. standard CHF therapy 2. restrict sodium 3. no alcohol |
Current ch10
|
|
|
What is the most common cardiomyopathy?
|
dilated cardiomyopathy (25%)
|
Current ch10
|
|
|
List 4 common types of cardiomyopathy.
|
dilated
hypertrophic restrictive Tako-Tsubo |
Current ch10
|
|
|
What is hypertrophic cardiomyopathy?
|
condition characterized by LVH + diastolic dysfunction
|
|
|
|
What is the etiology of hypertrophic cardiomyopathy?
|
hereditary
|
Current ch10
|
|
|
What is the clinical presentation of hypertrophic cardiomyopathy?
|
dyspnea
chest pain postexertional syncope ↑ diastolic pressure pulsus bisferiens sustained PMI S4 |
Current ch10
|
|
|
What is the diagnostic workup of hypertrophic cardiomyopathy?
|
EKG → LVH, exaggerated Q waves
CXR → mild cardiomegaly echocardiogram → LVH, diastolic dysfunction |
Current ch10
|
|
|
What is the initial management of hypertrophic cardiomyopathy?
|
1. B-blockers → slows HR → assisting in diastolic filling of stiff LV
2. refer to cardiologist if syncope, difficulty controlling symptoms, or high risk (FH of sudden death, marked hypertrophy, BP fails to increase with exercise) |
Current ch10
|
|
|
Compare dilated, hypertrophic, and restrictive cardiomyopathies.
|
dilated → ventricles dilated
hypertrophic → ventricles thickened restrictive → ventricles stiffened |
Current ch10
|
|
|
Define pulsus bisferiens.
|
when palpating pulse, double peak can be appreciated (striking twice)
|
|
|
|
What is the ddx for pulsus bisferiens?
|
aortic stenosis + aortic insufficiency
aortic insufficiency hypertrophic cardiomyopathy |
|
|
|
What are the complications of hypertrophic cardiomyopathy?
|
sudden death
often due to post-exertional arrhythmia often in young athletes |
|
|
|
What is the etiology of angina pectoris?
|
usually atherosclerotic heart disease
congenital anomolies arteritis dissection emboli severe myocardial hypertrophy severe aortic stenosis or regurgitation hyperthyroidism anemia paroxysmal tachycardias |
|
|
|
What is the clinical presentation of angina pectoris?
|
precordial chest pain
precipitated by exertion or stress relieved by rest or nitrates usually <3 minutes; possibly 15-20 minutes if caused by meal or anger if >30 min → think ustable angina, MI, etc!! |
|
|
|
What is the diagnostic workup of angina pectoris?
|
CPP
EKG scintigraphy |
|
|
|
What is the most common cause of angina pectoris?
|
atherosclerotic heart disease
|
|
|
|
Symptomatic aortic stenosis is a contraindication for EKG stress testing, true or false?
|
true
|
|
|
|
Which is more common, left HF or right HF?
|
left HF
|
|
|
|
What is the Functional Classification of Heart Disease?
|
classification system used for patients with heart disease to quantify and monitor symptoms associated with rest/activity
|
|
|
|
Describe the components of the Functional Classification of Heart Disease.
|

|
|
|
|
What is class I of the Functional Classification of Heart Disease?
|
no limitation of physical activity → ordinary physical activity does not cause undue fatigue, dyspnea, or anginal pain
|
Current
|
|
|
What is class II of the Functional Classification of Heart Disease?
|
slight limitation of physical activity → ordinary physical activity causes symptoms
|
Current
|
|
|
What is class III of the Functional Classification of Heart Disease?
|
marked limitation of physical activity → ordinary physical activity causes symptoms
|
Current
|
|
|
What is class IV of the Functional Classification of Heart Disease?
|
unable to engage in physical activity w/out discomfort → symptoms may be present at rest
|
Current
|
|
|
When monitoring patients with heart disease, it is best to document SPECIFIC activities that cause symptoms, true or false?
|
true → grocery shopping, vacuuming, climbing stairs, etc.
|
Current
|
|
|
What is the clinical presentation of left HF vs. right HF?
|
Left HF: think lungs!!!
fatigue exertional dyspnea orthopnea PND cough crackles pulmonary edema gallop cardiomegaly Right HF: think body!!! elevated JVD and JVP dependent peripheral edema hepatomegaly ascites |
Current ch10
|
|
|
Why do orthopnea and PND occur in heart failure?
|
when lying down, blood reaches the heart more easily than when standing which increases the heart's workload → if heart failure present, the heart can't compensate appropriately → blood backs up into lungs → SOB
|
Clinical Pathology p3
|
|
|
Define preload.
|
pressure that fills ventricles during diastole
|
Clinical Pathology p3
|
|
|
Define afterload.
|
resistance that heart faces during systole
|
Clinical Pathology p3
|
|
|
What are the 2 goals for treatment of HF?
|
HF causes ↓ forward flow and ↑ backup of flow, so goals are:
1. ↑ forward flow by increasing cardiac output ↑ force of ventricular contraction → inotropes ↓ rate of ventricular contraction → B-blockers 2. ↓ backup of flow by decreasing heart's workload ↓ intravascular volume → decrease preload → diuretics dilate arteries → decrease afterload → vasodilators |
Clinical Pathology p3
|
|
|
What is the clinical use of inotropes in HF?
|
↑ force of ventricular contraction → increasing cardiac output → increasing foward flow and decreasing backup of flow
|
Clinical Pathology p4
|
|
|
What is the clinical use of beta-blockers in HF?
|
↓ rate of ventricular contraction → allowing for more filling time → increasing cardiac output → increasing foward flow and decreasing backup of flow
|
Clinical Pathology p4
|
|
|
What is the clinical use of diuretics in HF?
|
↓ intravascular volume → decrease preload → decrease heart's workload → decrease backup of flow
|
Clinical Pathology p4
|
|
|
What is the clinical use of vasodilators in HF?
|
dilate arteries → decrease afterload → decrease heart's workload → decrease backup of flow
|
Clinical Pathology p4
|
|
|
Describe the renin-angiotensin-aldosterone system in relation to HF.
|
HF → decreased blood flow to kidneys → kidney releases renin → renin converts angiotensinogen to angiotensin I → ACE converts angiotensin I to angiotensin II → angiotensin II causes vasoconstriction + release of aldosterone from adrenals → aldosterone causes ↑ sodium (and water) reabsorption → increased BP
|
Clinical Pathology p5
|
|
|
What is the MOA of ACE inhibitors?
|
decrease conversion of angiotensin I to angiotensin II → preventing vasoconstriction and aldosterone release → preventing sodium/water retention → preventing ↑ BP → preventing back up of fluid
|
Clinical Pathology p5
|
|
|
What is the MOA of ARBs?
|
block angiotensin II receptors → preventing vasoconstriction and aldosterone release → preventing sodium/water retention → preventing ↑ BP → preventing back up of fluid
|
Clinical Pathology p5
|
|
|
What does the ACE in ACE inhibitors stand for?
|
angiotensin converting enzyme inhibitors
|
|
|
|
What drugs should be avoided in HF?
|
alcohol, NSAIDs, CCB, some anti-arrhythmic drugs
|
Pharmacology 187
|
|
|
List 5 ACE inhibitors.
|
lisinopril
captopril benazepril enalapril quinapril |
|
|
|
What are the indications for ACE inhibitors?
|
all stages of left HF
post-MI |
Pharmacology p189
|
|
|
What is the patient education for ACE inhibitors?
|
1. take on empty stomach → otherwise food may decrease absorption
|
Pharmacology p189
|
|
|
What are the adverse effects of ACE inhibitors?
|
postural hypotension, renal insufficiency, hyperkalemia, angioedema, peristent dry COUGH
|
Pharmacology p189
|
|
|
What type of medication may cause an adverse effect of a persistent dry cough?
|
ACE inhibitors
|
Pharmacology p189
|
|
|
What is the MOA of digoxin?
|
1. inhibits Na+/K+ exchange by Na+/K+ ATPase
2. intracellular [Na+] increases 3. Na+ concentration gradient decreases disrupting the Na+/Ca2+ exchanger 4. less Ca2+ is pumped into the extracellular space 5. more Ca2+ remains intracellularly causing ↑ force of ventricular contraction |
Pharmacology p191
|
|
|
What are the indications for digoxin?
|
severe LT ventricular systolic dysfunction after initiation of ACE inhibitor and diuretic therapy
HF with atrial fibrillation *not indicated for diastolic dysfunction or RT venticular HF |
Pharmacology p192
|
|
|
What are the adverse effects of digoxin?
|
digoxin toxicity
→ digoxin has narrow therapeutic window and long half-life (36 hours) → mainly eliminated by kidneys so renal failure can lead to toxicity → hypokalemia enhances toxicity so give K+ supplementation or K-sparing diuretic → arrhythmia → usually due to hypokalemia → nausea and vomiting → fatigue, HA, confusion, vision changes |
Pharmacology p193
|
|
|
What are the drug interactions for digoxin?
|
quinidine
verapamil amiodarone cause digoxin intoxication by displacing digoxin from protein-binding sites and by competing with digoxin for renal excretion |
Pharmacology p193
|
|
|
What is the patient education for digoxin?
|
requires periodic blood draw to monitor digoxin and potassium levels
|
|
|
|
What are the contraindications for digoxin?
|
hypersensitivity to digoxin
history of toxicity ventricular tachycardia ventricular fibrillation constrictive pericarditis amyloid disease Wolff-Parkinson-White syndrome + Afib |
Drug Handbook p444
|
|
|
List 4 inotropes.
|
digoxin
dobutamine dopamine epinephrine |
|
|
|
What are the indications for dobutamine?
|
acute HF
|
|
|
|
What are the contraindications for dobutamine?
|
hypersensitivity to dobutamine
idiopathic hypertrophic subarotic stenosis |
Drug Handbook p470
|
|
|
What is the MOA for dobutamine?
|
stimulates B1 adrenergic receptors → increase intracellular [cAMP] → activation of protein kinase → phosphorylation of slow Ca2+ channels → increase in intracellular [Ca2+] → increase in force of ventricular contraction
|
Pharmacology p194
|
|
|
What are the adverse effects of doputamine?
|
↑ HR and BP (but occasionally hypotension)
increased ventricular ectopy premature ventricular beats |
|
|
|
What is class of drug is spironolactone?
|
potassium-sparing diuretic
|
|
|
|
What is the MOA of spironolactone?
|
anatgonist of aldosterone → preventing sodium (and water retention), myocardial hypertrophy, and hypokalemia
|
Pharmacology p195
|
|
|
What is the patient education for spironolactone?
|
do not take K+ supplements
|
Pharmacology p195
|
|
|
What are the adverse effects of spironolactone?
|
GI → gastritis, peptic ulcer
endocrine → gynecomastia, menstrual irregularities, ↓ lidibo CNS → fatigue, confusion |
Pharmacology p195
|
|
|
S3 heard in context of HF suggests?
|
dilated heart/systolic dysfunction
|
Pathophysiology p8
|
|
|
S4 heard in context of HF suggests?
|
hypertrophic heart/diastolic dysfuction
|
Pathophysiology p8
|
|
|
What are the MOA, indications, contraindications, adverse effects, and drug interactions of dopamine?
|
MOA → stimulate dopaminergic and beta-adrenergic receptors
indications → adjunctive therapy in treatment of shock (including cardiac decompensation) that persists after adequate fluid replacement contraindications → hypersensitivity, pheochromocytoma, ventricular fibrillation adverse effects → palpitations, angina, hypotension, tachycardia, vasoconstriction, ectopic beats, dyspnea, nausea, vomiting, HA drug interactions → |
Drug Handbook p480
|
|
|
What are the MOA, indications, contraindications, adverse effects, and drug interactions of epinephrine?
|
think EPI PEN!!!
MOA → stimulates alpha and beta receptors → vasoconstriction → increase in force of ventricular contraction indications → cardiac arrest, bronchospasm (asthma, anaphylaxis), nasal congestion, viral croup, decrease superficial hemorrhage contraindications → none to epi pen in life threatening situation adverse effects → drug interactions → |
Drug Handbook p526
|
|
|
What is the clinical presentation of rheumatic fever?
|

recent infection
fatigue fever erythema marginatum → erythematous rings mostly on trunk that disappear and reappear over weeks to months subcutaneous nodules → small painless nodules on extensor surfaces chorea → abrupt nonrhythmic involuntary movements and muscular weakness carditis polyarthritis |
|
|
|
What is the most common symptom of rheumatic fever?
|
arthritis
|
|
|
|
What is pericarditis?
|
inflammation of the pericardium
|
|
|
|
What is the etiology of pericarditis?
|
infection → cocksackieviruses, echoviruses
inflammation in lung or myocardium post MI post cardiac surgery hemopericardium uremia autoimmune disease → RA, SLE neoplasm → lung, breast, renal cell carcinoma, Hodgkin disease, lymphoma drug toxicity → penicillins, clozapine, minoxidil radiation |
Current ch10
|
|
|
What is the diagnostic workup of pericarditis?
|
↑ elevated ESR
EKG → diffuse ST segment elevation, often PR depression, sometimes T wave inversion CXR → often normal, possible cardiac enlargement if fluid present, R/O extracardiac disease |
Current ch10
|
|
|
What is the most common cause of pericarditis?
|
viral infection
usually cocksackieviruses and echoviruses sometimes influenza, varicella, mumps, EBV, hepatitis, or HIV rarely TB or bacterial → pneumococci from lung infection or borrelia burgdorferi from lyme disease |
Current ch10
|
|
|
Describe the EKG often found in pericarditis.
|
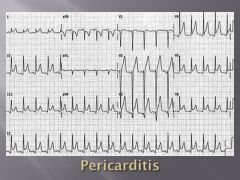
diffuse ST segment elevation
possible PR segment depression |
Current ch10
|
|

|
pericardial effusion
|
Current ch10
|
|
|
What are the characteristics of a pericardial friction rub?
|
high frequency → use diaphragm
scratching, grating, squeaking sound 3 components → 1 systolic sound between S1 and S2 + 1 diastolic sound during early diastole + 1 diastolic sound during late diastole loudest at lower left sternal border, during inspiration sometimes better detected during forced expiration while leaning forward |
|
|
|
|
pericardial friction rub
|
|
|
|
What is the management for pericarditis?
|
1. if viral → symptomatic treatment
-aspirin 650mg every 3-4 hours or indomethacin -if unresponsive → corticosteroids x 2 weeks -may recur or be complicated by cardiac tamponade 2. if post-MI or cardiac surgery → symptomatic treatment -aspirin 650mg every 3-4 hours x 2-4 weeks -if severe → corticosteroids -to prevent recurrences → colchicine x few months |
Current ch10
|
|
|
What is rheumatic heart disease?
|
condition characterized by damaged heart valves due to rheumatic fever
|
|
|
|
What is the management of rheumatic fever?
|
1. for strep throat → benzathine penicillin G 1.2 million units IM single dose
2. if penicillin allegy → erythromycin 40mg/kg daily 3. for fever and arthritis → aspirin 4. if refractory to aspirin → corticosteroids 4. bed rest until afebrile and resting HR, ESR, and EKG normal 5. to prevent recurrence → benzanthine penicillin G 1.2 million units IM every 4 weeks -if no carditis → continue until 21 y/p -if carditis + no valvular damage → continue for 10 years -if carditis + valvular damge → continue for 10 years or until 40y/o if high risk for reexsposure of strep throat (parent, teacher, medical professional, military personnel) If chorea: 1. provide calming environment 2. medications only control symptoms but do not alter duration or outcome 3. carbamazepine → may not see effect for 2 weeks, continue for 2 weeks after symptoms subside If HF: see HF management |
Current ch10
|
|
|
Who is most commonly affected by rheumatic fever?
|
children 5-15y/o
|
Current ch10
|
|
|
What is the clinical presentation of rheumatic heart disease?
|
history of rheumatic fever → may be single attack or repeated attacks
damage to valve cusps, commissures, and chordae tendineae → stenosis and/or insufficiency 50-60% → mitral valve 20% → mitral and aortic valves 10% → mitral and/or aortic + tricupsid valves |
Current ch10
|
|
|
What valve is most commonly affected in rheumatic heart disease?
|
mitral valve
|
Current ch10
|
|
|
What are the complications of rheumatic heart disease?
|
endocarditis
|
|
|
|
What is the clinical presentation of pericarditis?
|
fever
dyspnea anterior pleuritic chest pain → worse when supine, relieved when upright may radiate to neck, shoulders, back, or epigastrium pericardial friction rub |
|
|
|
What is superficial thrombophlebitis?
|
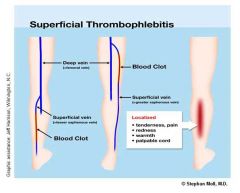
inflammation of a superficial vein due to a blood clot
|
Current ch12
|
|
|
What is the etiology of superficial thrombophlebitis?
|
spontaneous → pregnancy, postpartum, varicose veins, thromboangitis obliterans
trauma → blow, irritating solution from IV hypercoaguable states → factor V leiden, protein S deficiency, protein C deficiency, antithrombin III deficiency abdominal cancer → pancreatic carcinoma → systemic hypercoaguability oral contraceptives iatrogenic → IV, PICC 20% associated with occult DVT |
Current ch12
|
|
|
What is the most common cause of superficial thrombophlebitis?
|
IV or PICC lines
|
Current ch12
|
|
|
What is the clinical presentation of superficial thrombophlebitis?
|

localized dull pain
redness, warmth, induration, and tenderness along a superficial vein (usually great saphenous vein) or at recent IV site inflammation clears in 1-2 weeks but firm cord may persist |
Current ch12
|
|
|
What is the most common site of superficial thrombophlebitis?
|
great saphenous vein
|
Current ch12
|
|

|
superficial thrombophlebitis
|
|
|
|
What is the management of superficial thrombophlebitis?
|
1. if localized → NSAIDs, local heat
2. if extensive or near superficial-deep vein junction → ligation and division of vein 3. broad-spectrum antibiotics to prevent septic phlebitis If septic phlebitis develops: 1. may be indicated by fever/chills or positive culture 2. continue antibiotics x 7-10 days 3. heparin 4. possible excision of vein |
Current ch12
|
|
|
What is the patient education for superficial thrombophlebitis caused by varicose veins?
|
often recurrent
|
Current ch12
|
|
|
What is the prognosis of superficial thrombophlebitis and septic phlebitis?
|
superficial thrombophlebitis → generally benign and brief
septic phlebitis → 20% mortality rate |
Current ch12
|
|
|
What are the complications of superficial thrombophlebitis?
|
cellulitis
gangrene septic phlebitis DVT PE |
|
|
|
What is the prevention of superficial thrombophlebitis?
|
1. monitor IV lines daily
2. remove IV if inflammation develops to prevent septic phlebitis and thrombotic complications 3. avoid remaining still for long periods of time |
Current ch12
|
|
|
What does PICC line stand for?
|
peripherally inserted central catheter
|
Current ch12
|
|
|
What is chronic venous insufficiency?
|
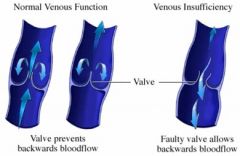
disorder characterized by limited venous return to heart caused by malfunctioning valves → scarred valves or dilated vein prevents valve closure → blood pools → pressure increases → causing edema and skin changes
|
Current ch12
|
|
|
What is the etiology of chronic venous insufficiency?
|
leg trauma
DVT varicose veins arteriovenous fistula neoplastic obstruction |
Current ch12
|
|
|
What is the clinical presentation of chronic venous insufficiency?
|
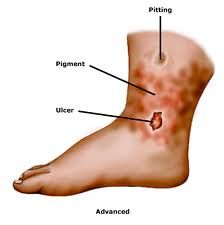
lower extremities:
dull aching itching pitting edema liposclerosis brown skin discoloration around ankles ulcers around ankles secondary varicosities |
Current ch12
|
|
|
What causes the brown skin discoloration seen in chronic venous insufficiency?
|
blood leaks out of blood vessels → hemoglobin broken down into hemosiderin → hemosiderin permanently deposited in dermal macrophages
|
Current ch12
|
|

|
chronic venous insufficiency
|
|
|

|
chronic venous insufficiency
|
|
|
|
What is the management of chronic venous insufficiency?
|
1. compression stockings worn from mid foot to just below knee
2. elevate legs intermittently during day 3. elevate legs above heart with pillows at night 4. avoid long periods of sitting/standing 5. if refractory to above → pneumatic compression of leg If ulceration: 1. control edema 2. apply compression or semi-rigid gauze boot and change every 2-3 days |
Current ch12
|
|
|
What is the prevention of chronic venous insufficiency?
|
aggressive management of DVT
compressive stockings for varicose veins |
Current ch12
|
|
|
What is the etiology of varicose veins?
|
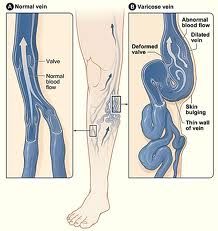
usually hereditary
pregnancy prolonged standing heavy lifting superficial thrombophlebitis with deep vein complications arteriovenous fistula → diagnose by presence of bruit obstruction due to neoplasm vein dilation causes malfunctioning of valves → blood pools |
Current ch12
|
|
|
What is the clinical presentation of varicose veins?
|

asymptomatic or aching pain exacerbated by standing
dilated tortuous superficial veins in lower extremities often great saphenous vein, sometimes small saphenous vein secondary varicosities |
Current ch12
|
|
|
What is the management of varicose veins?
|
1. compression stockings
2. intermittent elevation of legs 3. sclerotherapy 4. surgery |
Current ch12
|
|
|
Who is most commonly affected by varicose veins?
|
women following pregnancy
|
Current ch12
|
|
|
What is the prevention of varicose veins?
|
wear compression stockings during pregnancy
|
Current ch12
|
|

|
varicose veins
|
|
|
|
Why is surgical removal of varicose veins often not helpful?
|
removal of one vein just puts more pressure on adjacent veins creating more varicose veins
|
|
|
|
What are diuretics?
|
medications that increase urine flow
|
Pharmacology p261
|
|
|
What are the classes of diuretics?
|
carbonic anhydrase inhibitors
osmotic diuretics loop diuretics thiazide diuretics potassium-sparing diuretics |
|
|
|
List classes of diuretics in order of most effective to least effective.
|
loop diuretics < thiazide diuretics < potassium sparing diuretics
|
Pharmacology p261
|
|
|
List types of carbonic anhydrase inhibitors.
|
acetazolamide
|
|
|
|
What is the MOA for carbonic anhydrase inhibitors (acetazolamide)?
|
inhibition of HCO3- reabsorption in proximal convoluted tubule
|
Pharmacology p261
|
|
|
What are the indications for acetazolamide?
|
prophylaxis for mountain sickness
↓ intraocular pressure of open-angle glaucoma |
Pharmacology p272
|
|
|
What are the contraindications for acetazolamide?
|
hepatic cirrhosis
|
Pharmacology p272
|
|
|
What are the adverse effects of acetazolamide?
|
hypokalemia
metabolic acidosis renal stone formation drowsiness paresthesia |
Pharmacology p272
|
|
|
List types of osmotic diuretics.
|
mannitol
|
|
|
|
What is the MOA for osmotic diuretics?
|
cause increased water secretion (not increased Na+ excretion like other diuretics)
|
Pharmacology p272
|
|
|
What are the indications for mannitol?
|
maintain urine flow following:
increased ICP due to shock acute renal failure due to shock drug toxicity trauma prevents kidneys from failing |
Pharmacology p272
|
|
|
What are the adverse effects of mannitol?
|
extracellular water expansion and dehydration
hypo and hypernatremia |
Pharmacology p272
|
|
|
List types of loop diuretics.
|
furosemide
torsemide bumetanide ethacrynic acid |
|
|
|
What is the MOA for loop diuretics?
|
inhibition of Na+/K+/2Cl- cotransport in ascending loop of Henle → retention of Na+, Cl-, and water in tubule
|
Pharmacology p261
|
|
|
What are the indications for loop diuretics?
|
acute pulmonary edema due to HF
hypercalcemia hyperkalemia |
Pharmacology p269
|
|
|
What are the adverse effects of loop diuretics?
|
ototoxicity → especially ethacrynic acid
hypokalemia hypomagnesemia hyperuricemia → furosemide and ethacrynic acid hypotension |
Pharmacology p269
|
|
|
List types of thiazide diuretics.
|
hydrochlorathiazide
chlorothiazide metolazone |
|
|
|
Describe chlorothiazide.
|
thiazide diuretic
MOA → inhibits Na+/Cl cotransporter in ascending loop of Henle indications → mild-to-moderate HTN; adjunctive therapy for edema contraindications → renal failure |
Drug Handbook p308
|
|
|
What is the MOA for thiazide diuretics?
|
inhibition of Na+/Cl- cotransporter in distal convoluted tubule → retention of water in tubule
|
Pharmacology p261
|
|
|
What are the indications for thiazide diuretics?
|
HTN
mild-to-moderate HF (if thiazide fails → prescribe loop diuretic) hypercalciuria diabetes insipidus |
Pharmacology p267
|
|
|
What are the adverse effects of thiazide diuretics?
|
hypokalemia
hyperuricemia hyponatremia hypomagnesemia hypercalcemia hyperglycemia volume depletion → hypotension hyperlipidemia hypersensitivity |
Pharmacology p267
|
|
|
List the thiazide diuretics from most effective to least effective?
|
metolazone < hydrochlorothiazide < chlorothiazide
|
Pharmacology p265
|
|
|
How does the strength of metolazone compare to the other thiazide diuretics?
|
more potent
causes Na+ excretion even in advanced renal failure |
Pharmacology p268
|
|
|
List types of potassium sparing diuretics.
|
spironolactone
triamterene amiloride hydrochloride |
|
|
|
What is the MOA for potassium-sparing diuretics?
|
occurs in collecting duct and tubule
spironolactone → aldosterone agonist → inhibits aldosterone-mediated Na+ resorption/K+ secretion triamterene and amiloride → block Na+ channels |
Pharmacology p261
|
|
|
What are the indications for spironolactone?
|
adjunctive therapy to prevent hypokalemia
severe HF hepatic cirrhosis secondary hyperaldosteronism |
Pharmacology p270
|
|
|
What are the adverse effects of spironolactone?
|
GI upset → nausea, peptic ulcer
gynecomastia menstrual irregularities hyperkalemia → lethargy, mental confusion |
Pharmacology p270
|
|
|
What are the indications for triamterene and amiloride hydrochloride?
|
adjunctive therapy to prevent hypokalemia
|
Pharmacology p271
|
|
|
What are the adverse effects of triamterene?
|
leg cramps
hyperkalemia hyperuricemia ↑ BUN |
Pharmacology p271
|
|
|
What is the effect of adrenergic stimulation on heart, lungs, and blood vessels?
|
heart → increase HR, contractility, and conduction velocity
lungs → bronchiole dilation (relaxing smooth muscle) blood vessels → vasoconstriction in skin and mucous membranes; dilation to liver and skeletal muscle |
|
|
|
What is the effect of cholinergic stimulation on heart, lungs, and blood vessels?
|
heart → decreases HR, contractility, and conduction velocity
lungs → bronchiolar constriction, increase in mucus secretion blood vessels → vasodilation |
|
|
|
What class of drug is epinephrine?
|
catecholamine → adrenergic receptor agonist
|
Pharmacology p71
|
|
|
What are the indications for epinephrine?
|
1. cardiac arrest
2. brochoconstriction → acute asthma, anaphylactic shock 3. glaucoma 4. anesthetics 3. |
Pharmacology p71
|
|
|
*What are the adverse effects of epinephrine, norepinephrine, and isoproterenol?
|
adverse effects → CNS disturbances (HA, tremor, tension, anxiety, fear), cardiac arrhythmia, pulmonary edema, cerebral hemorrhage
NE also causes blanching and skin sloughing at site of injection due to extreme vasoconstriction |
Pharmacology p71
|
|
|
What are the clinical uses of norepinephrine?
|
shock → NE causes vasoconstriction → increase in vascular resistance → increase BP
*though metaraminol preferred b/c it does not reduce blood flow to kidneys |
Pharmacology p74
|
|
|
What class of drug is norepinephrine?
|
catecholamine → adrenergic agonist
|
|
|
|
What are the adverse effects, contraindications, and toxicities of norepinephrine?
|
same as epinephrine + blanching and skin sloughing along injected vein (due to extreme vasoconstriction)
|
Pharmacology p75
|
|
|
What class of drug is isoproterenol?
|
synthetic catecholamine → B1- and B2-adrenergic receptor agonist
|
Pharmacology p75
|
|
|
What are the clinical use of isoproterenol?
|
1. stimulation of heart in emergency situations
2. rarely used as brochodilator in asthma |
Pharmacology p75
|
|
|
What class of drug is phenylephrine?
|
synthetic noncatecholamine → primarily binds alpha1 receptors
causes vasoconstriciton → raising BP no effect on heart |
Pharmacology p77
|
|
|
What is the clinical use of phenylephrine?
|
nasal decogestant
increase BP terminate supraventricular tachycardia |
Pharmacology p77
|
|
|
What are the adverse effects of phenylephrine?
|
hypertensive HA
cardiac irregularities |
Pharmacology p77
|
|
|
What class of drug is ephedrine?
|
noncatecholamine → mixed action adrenergic agonist
|
Pharmacology p79
|
|
|
What are the clinical uses of ephedrine?
|
raise BP
treat asthma via bronchodilation nasal decongestant |
Pharmacology p79
|
|
|
What class of drug is ephedrine?
|
noncatecholamine → mixed action adrenergic agonist
|
Pharmacology p79
|
|
|
What are the clinical uses of ephedrine?
|
raise BP
treat asthma via bronchodilation nasal decongestant |
Pharmacology p79
|
|
|
What is the MOA and clinical use of B-blockers?
|
MOA → B-adrenergic agonists → diminsh phase 4 depolarization → depressing automaticity, prolonging AV conduction, and decreasing HR and contractility
clinical use → atrial flutter, atrial fibrillation, AV-nodal reentrant tachycardia, prevention of ventricular arrhythmia following MI |
|
|
|
What is the MOA and clinical use of digoxin?
|
MOA → cardiac glycoside → shortens refractory period in atrial and ventricular myocardial cells while prolonging refractory period and decreasing conduction velocity in AV node
clinical use → atrial flutter, atrial fibrillation, paroxysmal supraventricular tachycardia, HF *digoxin toxicity → can lead to ventricular fibrillation |
|
|
|
What is the MOA and clinical use of CCBs?
|
MOA →
clinical use → atrial flutter, atrial fibrillation, supraventricular tachycardia, HTN, angina |
|
|
|
What is the MOA and clinical use of quinidine?
|
MOA → Na+ channel blocker → binds to Na+ channels → prevents Na+ influx → slows phase 0 depolarization in ventricular muscle fibers
clinical use → atrial, junctional, and ventricular tachyarrhythmias; maintain sinus rhythm following cardioversion of atrial flutter or a-fib; prevent frequent ventricular tachycardia |
|
|
|
What is the MOA and clinical use of lidocaine?
|
MOA → Na+ channel blocker → shortens phase 3 repolarization and decreases duration of AP
clinical use → ventricular arrhythmias arising during myocardial ischemia |
|
|
|
What should be prescribed for atrial fibrillation?
|
first line → B-blocker
second line → CCBs, digoxin if ≥1 risk factor for stroke → long-term warfarin with INR 2.0-3.0 |
|
|
|
List 2 Na+ channel blockers.
|
lidocaine
quinidine |
|
|
|
What is lidocaine?
|
Na+ channel blocker used to treat ventricular arrhythmias often associated with MI
|
|
|
|
What is quinidine?
|
Na+ channel blocker used to treat atrial, junctional, or ventricular arrhythmias
|
|
|
|
List arrhytmias treated by B-blockers, CCBs, digoxin, quinidine, and lidocaine.
|
BBs:
-atrial flutter -atrial fibrillation -supraventricular tachycardia -ventricular tachycardia CCBs: -atrial flutter -atrial fibrillation -paroxysmal supraventricular tachycardia DIGOXIN: -atrial flutter -atrial fibrillation -paroxysmal supraventricular tachycardia QUINIDINE: prevention of atrial, junctional, and ventricular arrhythmias -atrial fibrillation -paroxysmal supraventricular tachycardia -premature atrial contraction -ventricular tachycardia -premature ventricular contraction -following cardioversion for atrial flutter or fibrillation LIDOCAINE: -ventricular arrhythmias (often due to MI) |
|
|
|
What is the clinical use of nitroglycerin and isosorbide dinitrate for angina and how does it effect myocardial O2 demand?
|
clinical use → stable angina, prinzmetals
MOA → vasodilator 1. dilation of large veins → decreased venous return → decreased preload → decreased work of heart → decreased myocaridal O2 demand 2. dilation of coronary arteries → increased blood supply to myocardium |
|
|
|
What is nitroglycerin?
|
vasodilator
|
|
|
|
List nitrates.
|
nitroglycerin
isosorbide dinitrate |
|
|
|
What is isosorbide dinitrate?
|
vasodilator
|
|
|
|
What is the clinical use of ranozaline and how does it effect myocardial O2 demand?
|
clinical use → chronic angina
*does not relieve acute angina MOA → |
|
|
|
What type of nitrate should be given for prompt relief of ongoing stable angina attack?
|
sublingual nitroglycerin
|
Pharmacology p210
|
|
|
What are the routes of administration, onset, and duration of nitroglycerine and isosorbide dinitrate?
|
NITROGLYCERIN:
1. sublingual tablet or spray -onset → 2 min -duration → 25 min 2. transdermal patch -onset → 30 min -duration → 8-14 hrs 3. oral sustained release tablet -onset → 35 min -duration → 4-8 hrs ISOSORBIDE DINITRATE: 1. sublingual -onset → 5 min -duration → 1 hr 2. oral slow-release tablet -onset → 30 min -duration → 8 hrs |
Pharmacology p211
|
|
|
What should you prescribe for newly diagnosed stable angina?
|
nitroglycerin or isosorbide dinitrate sublingual tablet or spray
take if angina attack can also take before activities that may precipitate angina attack |
Current ch10
|
|
|
What are the adverse effects of nitrates?
|
HA!!!
facial flushing postural hypotension tachycardia |
Pharmacology p211
|
|
|
Discuss tolerance to nitrates.
|
tolerance develops rapidly where blood vessels become desensitized to vasodilation
TO AVOID TOLERANCE: -schedule daily 8-12 hr nitrate-free interval to restore sensitivity -remove transdermal patch at night -if prinzmetal's angina → remove transdermal patch in afternoon since angina worsens early in morning |
Pharmacology p211
|
|
|
Nitrates are contraindicated if taking what drug?
|
sildenafil (Viagra) → potentiates action of nitrates → may cause extreme hypotension
*can prescribe ranolazine instead |
Pharmacology p211
|
|
|
List drugs for treatment of angina.
|
acute → nitrates
chronic → -first line → B-blockers, ranozaline -third line → CCBs |
|
|
|
What is the clinical use of pentoxifylline (Trental)?
|
MOA → reduces blood viscosity
clinical use → symptomatic treatment of intermittent claudication due to chronic occlusive arterial disease of limbs |
Drug Handbook p1173
|
|
|
What is the pharmological treatment following MI?
|
1. immediate chewable aspirin → 162mg or 325mg
2. if aspirin allergy → clopridogrel 300mg or 600mg 3. if STEMI → aspirin + clopridogrel 4. if STEMI (not NSTEMI) → thrombolytic therapy or coronary angioplasty 5. thrombolytic therapy → streptokinase or tissue plasminogen activator 6. continued aspirin 81mg and heparin 7. long term → aspirin 81mg, clopridogrel or both |
|
|
|
What does HMG COA reductase inhibitors stand for?
|
3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors
|
Pharmacology p253
|
|
|
What is the common name for HMG COA reductase inhibitors?
|
statins
|
Pharmacology p253
|
|
|
What are the indications for prescribing HMG COA reductase inhibitors?
|
1. elevated LDL
2. hyperlipidemias *not familial hypercholesterolemia |
Pharmacology p253
|
|
|
What are the first-line agents for elevated LDL?
|
HMG COA reductase inhibitors
|
Pharmacology p253
|
|
|
HMG COA reductase inhibitors are effective in patients who are homozygous for familial hypercholesterolemia, true or false?
|
false → since these patients lack LDL receptors
|
Pharmacology p253
|
|
|
What is the MOA for HMG COA reductase inhibitors?
|
inhibition of HMG COA reductase → decreased cholesterol synthesis → decreased [intracellular cholesterol] →
1. increased LDL receptor synthesis→ increased number of LDL receptors → increased internalization of LDL → decreased plasma cholesterol 2. decreased VLDL secretion → decreased plasma cholesterol |
Pharmacology p253
|
|
|
What are the contraindications of HMG COA reducatse inhibitors?
|
adolescents
pregnancy breast-feeding renal insufficiency |
Pharmacology p255
|
|
|
What are the adverse effects of HMG COA reductase inhibitors?
|
1. liver failure → monitor LFTs
2. myopathy and rhabdomyolysis → usually associated with renal insufficiency or drug interaction → monitor CK |
Pharmacology p255
|
|
|
What is rhabdomyolysis?
|
disintegration of muscle
|
Pharmacology p255
|
|
|
What are the drug interactions for HMG COA reductase inhibitors?
|
increase in warfarin → monitor INR
|
Pharmacology p255
|
|
|
What is the patient education for HMG COA reductase inhibitors?
|
1. do not take if pregnant or breast-feeding
2. must periodically get blood drawn to monitor LFTs and CK 3. if taking warfarin → must periodically get blood drawn to monitor INR |
Pharmacology p255
|
|
|
What are other names for niacin?
|
nicotinic acid
vitamin B3 |
Pharmacology p255
|
|
|
What are the indications for niacin?
|
1. decreased HDL
2. increased LDL 3. hypercholesterolemias 4. familial hyperlipidemias |
Pharmacology p255
|
|
|
What is the most effective agent for increasing HDL levels?
|
niacin
|
Pharmacology p255
|
|
|
What is the MOA of niacin?
|
inhibition of lipolysis in adipose tissue → decreased plasma levels of cholesterol and triglycerides
|
Pharmacology p255
|
|
|
What are the adverse effects of niacin?
|
*cutaneous flush
*pruritus nausea and abdominal pain hyperuricemia and gout → niacin inhibits uric acid secretion impaired glucose tolerance hepatotoxicity |
Pharmacology p255
|
|
|
What are the drug interactions of niacin?
|
alcohol → may increase cutaneous flushing
gout meds → allopurinol, probenecid, sulfinpyrazone DM meds |
|
|
|
What is the patient education for niacin?
|
if experience cutaneous flushing:
1. usually lasts 15-30min 2. may be accompanied by pruritus, especially in clothing-covered areas 3. take 300mg aspirin 30min before niacin to reduce flushing 4. flushing is usually self-limited after several weeks of a consistent dose |
Pharmacology p256
|
|
|
Which HMG COA reductase inhibitors are most effective at decreasing LDL, increasing HDL, and decreasing triglycerides?
|
decreasing LDL → atorvastatin, rosuvastatin
increasing HDL → pravastatin, simvastatin decreasing triglycerides → atorvastatin |
Pharmacology p255
|
|
|
List HMG COA reductase inhibitors in order of most effective to least effective at reducing LDL.
|
atorvastatin = rosuvastatin > pravastatin = simvastatin > lovastatin = fluvastatin
|
Pharmacology p255
|
|
|
Name 5 HMG COA reductase inhibitors.
|
atorvastatin
simvastatin pravastatin lovastatin fluvastatin |
|
|
|
Name 2 bile-acid sequestering agents
|
cholestyramine
colestipol |
|
|
|
What are the indications for prescribing bile-acid sequestering agents?
|
1. elevated LDL
*though not as effective as statins |
Pharmacology p257
|
|
|
What is the MOA of bile-acid sequestering agents?
|
bind negatively charged bile acids and bile salts in small intestine → complex secreted in feces → preventing bile acids from returning to liver → lowering [bile acid] → causing hepatocytes to increase conversion of cholesterol to bile acids → decreasing[intracellular cholesterol] → increasing LDL uptake into cell → decreasing plasma LDL
|
Pharmacology p257
|
|
|
List the categories of drugs used to treat elevated LDL, decreased HDL, and elevated TRIG in order of most effective to least effective.
|
elevated LDL → HMG CoA reductase inhibitors > bile acid sequestrants > niacin > fibrates
decreased HDL → niacin > fibrates > HMG CoA reductase inhibitors > bile acid sequestrants elevated TRIG → fibrates > niacin > HMG CoA reductase inhibitors > bile acid sequestrants |
Pharmacology p259
|
|
|
List statins and how they effect LDL, HDL, and TRIG.
|
lovastatin → decreases LDL, increases HDL
pravastatin → decreases LDL and TRIG fluvastatin, simvastatin, and atorvastatin → decreases LDL and TRIG, increases HDL |
|
|
|
Which is the cheapest statin?
|
lovastatin (but also least potent)
|
|
|
|
MI:
|
-sudden prolonged (>30 min) anterior chest discomfort; often describe as “gas” or pressure
-worsening -occurs at rest or with minimal exertion -diaphoresis -anxiety -SOB -soft heart sounds may indicate LV dysfunction -S4 is common -S3 is less common and indicates significant LV dysfunction -mitral regurgitation murmur may indicate papillary muscle dysfunction or rupture -cyanosis, cold temp, weak peripheral pulses, abnormal cap refill indicate low cardiac output -ST segment elevation with MI, Q waves, mean axis deviation, poor R wave progression -ST segment depression with angina or subendocardial MI -inverted T waves with ischemia -give aspirin 162 or 325mg -if present <12 hours with STEMI, reperfusion therapy either via percutaneous coronary intervention or via thrombolytic therapy |
|
|
|
AORTIC DISSECTION:
|
-sudden searing chest pain
-radiation to neck, back, or abdomen -HTN -diminished or unequal pulse in extremities -LVH common -mediastinal widening on CXR -lower BP to 100-120 with B-blocker -CT -surgical intervention if involving arch of aorta |
|

