![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
86 Cards in this Set
- Front
- Back
|
Trendelenburg's test
|
Put hands on patients hips, and ask them to lift one leg. If the hip on that side sags, then it is a positive sign that the abductor muscles on the other side are weak.
|
|
|
Schoberg's test
|
One finger 10 cm above level of posterior superior iliac spine, one finger 5 cm below.
Tell patient to bend forward. The space between your fingers should increase from 15 to about 22 cm. Diagnose ankylosing spondylitis and seronegative spondyloarthropathy. |
|
|
Tripod test
|
While patient is sitting, extend the knee passively.
If patient leans back onto their hands, this is a sign of nerve root impingement. |
|
|
Bulbocavernosus test
|
S2-4
|
|
|
Thomas test
|
Tests hip flexion contracture.
Flex the opposite hip fully to flatten the lumbar lordosis. The other leg should be able to lay down flat. If it doesn't, then there may be hip flexion contracture. |
|
|
Lasegue's test
|
A root tension sign test.
If the straight leg raise test was positive, then lower the leg and then dorsiflex the ankle to confirm the pain. |
|
|
Bowstring sign
|
A root tension sign test.
Use thumb to press in the popliteal fossa. |
|
|
Faber test
|
A test for SI joint pain.
Figure four position - bend one knee, cross the ankle over the straight leg's knee. Press down on the bent knee, while holding the ASIS on the other side. |
|
|
Femoral stretch test
|
In prone position.
Flex knee 90 degrees Lift thigh to extend the hip Pain if there is L3 or L4 nerve root impingement |
|
|
Patellar tracking, J-sign
|
While patient is sitting, tell patient to extend the leg and look for J-sign, which is the patella moving laterally.
J-sign: patellar instability, causes patella to flip over to the lateral side of the knee when the leg is extended. |
|
|
Fluid bulge sign
|
Test for knee effusion.
Patient supine. Milk fluid from medial side of knee Run hand from superior lateral area of patellar pouch down to lateral side of knee. Look for wave of fluid on medial side. |
|
|
Patellar tap
|
Test for knee effusion.
Squish fluid from suprapatellar pouch Tap patella against distal femur Look at patella to see if it bobs up and down |
|
|
Patellofemoral compression test
|
Patient supine.
Tests for anterior knee pain Put fingers on knee cap, and move it back and forth, pushing it against the femur. |
|
|
Patellofemoral grind test
|
Patient supine.
Use one hand to push the patella distally. Ask patient to contract quadriceps muscle. This also compresses the patella against the femur. Sometimes, this pinches the synovium under the patella, and hurts even in normal instances. Don't press too hard. |
|
|
Lachman's test
|
Checks ACL
Put one hand under thigh and lift it up so that knee is flexed about 20 degrees Use other hand and pull the tibia forward. There should be a firm endpoint. Compare the amount of translation to the other side |
|
|
McMurray's maneuver
|
Tests for meniscal tears.
Patient supine. Usually negative Hold foot in one hand, other hand on the knee's joint line. Bend knee slightly Gentle valgus force Flex knee fully Rotate tibia externally Apply varus force, and extend knee Feeling a clunk, and eliciting pain from patient = positive sign. Both must be present to be positive. Go the other way now - flex while varus load, internally rotate the tibia, extend while applying valgus load. |
|
|
Patellar apprehension
|
Knee flexed slightly, push patella laterally.
If there is patellofemoral instability, this will make them apprehensive. |
|
|
Anterior drawer test for ankle
|
Patient sitting.
People with recurrent ankle sprains. Grasp heel with one hand, tibia with other, and pull ankle forward. |
|
|
Windlass test
|
Press on medial side of plantar surface of foot (plantar fascia).
Extend great toe, which will tighten the fascia. Pain indicates plantar fasciitis. |
|
|
Thompson's test
|
Put patient in prone position.
Feet hanging over edge of bed. Palpate the Achilles tendons on both sides. May be dented on a side if ruptured. Squeeze gastrosoleus muscles simultaneously bilaterally, and watch for flexion in in both feet. If foot doesn't flex, indicates Achilles tendon rupture |
|
|
Spurling's test
|
Patient sitting.
Tests for cervical nerve root compression. Patient extends neck, and turns toward side of affected extremity. This should help reproduce pain that shoots down the patient's arm. If pain not reproduced, apply gentle axial load to the neck to look for pain reproduction. |
|
|
Adson's test
|
While palpating radial pulse, abduct, extend and externally rotate the shoulder.
Ask patient to take a deep breath and look towards the ipsilateral side. If there is decrease in the radial pulse, could indicate thoracic outlet syndrome. This test is frequently positive in normal subjects. |
|
|
Painful arc test
|
Patient standing.
If they feel pain about 1/3 of the way through the arc, then the test is positive. Impingement syndrome - indicates that the rotator cuff and subacromial bursa are getting pinched under the acromion. |
|
|
Hawkin's test
|
Flex patient's arm forward 90 degrees.
Elbow belt to 90 degrees. Internally rotate arm. Tests for impingement syndrome. Subacromial bursa and rotator cuff will be pinched against coracoid and coracoacromial ligament. |
|
|
Neer's test
|
Patient sitting.
Stabilize patients scapula by placing one hand on the acromion. Flex the arm maximally forward. Tests for impingement syndrome. Subacromial bursa and rotator cuff will be pinched against the anterior acromion. |
|
|
Sulcus sign
|
Patient sitting.
Ask patient to relax. Passively pull down on arm. Look for sulcus under lateral edge of acromion. Indicates laxity of shoulder ligaments. Must be compared to other side. |
|
|
Yergason's test
|
Patient sitting.
Patient flexes elbow past 90 degrees, with forearms pronated. Actively resist the patient supinating the forearm as you externally rotate the shoulder. Tests for biceps tendon stability. If unstable, it will cause pain, and the tendon may dislocate from the bicipital groove. |
|
|
AC joint compression test
|
Patient sitting.
Passively flex their arm forward to 90 degrees Force arm into full adduction across the patient's body. Puts stress on the AC joint and will be painful if there is AC joint degeneration (eg. Osteoarthritis) |
|
|
Scapular winging
|
Wall push-up with hands together.
Tests long thoracic nerve injury, or impingement syndrome causing muscle weakness. |
|
|
Apprehension test
|
Patient is supine with shoulder hanging over edge of bed
Gently passively abduct and externally rotate the shoulder If anterior instability -> patient will be apprehensive. Pain only is not a positive test. |
|
|
What is the pivot-shift test?
|
• Important to confirm complete ACL test.
• Not reliable in acute setting. • Hold heel in one hand, tibia in other. • Apply axial load to limb with hand holding heel. • Apply valgus and internal rotation force with hand holding tibia. • Then gently flex the knee. • Feel for a clunk. |
|
|
What is Cullen's sign?
|
Periumbilical ecchymoses.
Retroperitoneal bleeding. Especially a sign of severe, acute pancreatitis. |
|
|
What is Grey Turner sign?
|
Ecchymoses on the abdomen and flanks that occur without trauma due to massive retroperitoneal bleeding (eg. pancreatitis, strangulated bowel, or bleeding from abscess).
|
|
|
What is Courvoisier's law?
|
If in the presence of jaundice the gall bladder is palpable, then the jaundice is unlikely due to stone. It is more likely due to obstruction due to cancer of the head of pancreas, or biliary malignancy. This is because stones don't cause gall bladder distension, but masses do.
|
|
|
Where does duodenum/pancreas pathology cause referred pain?
|
Mid-back.
|
|
|
Where does biliary tree or gall bladder pathology cause referred pain?
|
Right shoulder tip, and scapula.
|
|
|
What is tenesmus?
|
Painful, urgency to empty bowels, but ineffective (passes little or no matter)
|
|
|
When is neonatal jaundice considered pathological?
|
< 24 hours, or > 10 days of life is pathological.
Between, might still be pathological. |
|
|
What is the transpyloric plane used as a landmark for? 5 things.
|
• Pyloric portion of the stomach at the pyloric sphincter
• Duodeno-jejunal junction • Hilus of kidney • Neck of pancreas • Disk between L1 and L2 |
|
|
What is the intercristal plane?
|
This is the line that is across the PSIS. It is the level of the body of L4. Used to landmark for lumbar puncture between L3 and L4.
|
|
|
What level does the trachea bifurcate?
What level does the aorta bifurcate? |
Trachea: T4/5
Aorta: L4 |
|
|
What spinal level are the renal arteries at?
|
L2
|
|
|
What is diastasis recti?
|
Diastasis recti - occurs when the two abdominal rectus muscles lack their normal fibrous attachment in the midline. Looks normal with the abdomen relaxed. When patient raises head from pillow, the abdominal recti tense, revealing the separation.
|
|
|
What is Sister Mary Joseph's node?
|
Hard subcutaneous or dermal nodule at the umbilicus.
Represents metastatic cancer to the umbilicus (stomach, pancreas, colorectum, ovary). Usually indicative of peritoneal carcinomatosis. |
|
|
What is the normal span of the liver?
|
10-12 cm (according to the GI clinical skills guide)
|
|
|
Psoas sign
|
Psoas sign
Patient supine or on side. Put hip through full ROM in flexion and extension. Pain suggests inflammation of the psoas or overlying peritoneum. |
|
|
Obturator sign.
|
□ Patient supine
□ Flex knee and hip to 90 degrees. □ Put hip through full range of internal and external rotation. □ Deep pelvic pain can suggest inflammation of obturator muscle, or pelvic peritoneum |
|
|
How can an enlarged left kidney be distinguished from an enlarged spleen on palpation?
|
1. It extends more posteriorly, whereas spleen is more superficial.
2. Has rounded edge, and lacks sharp edge or notch of spleen. 3. Surface may be more irregular than spleen. 4. Kidney moves only slightly with respiration, due to its retroperitoneal position. Spleen moved more. 5. As it enlarges, it remains confined to left side of abdomen. Spleen enlarges obliquely. |
|
|
What is Blummer's shelf?
|
On DRE, palpable rectal shelf. It is due to intra-abdominal cancer. Deposits of cancer in retrovesical or retrouterine pouch, palpable through the anterior rectal wall.
|
|
|
What are the signs / tests for ascites?
|
1. Bulging flanks
2. Tympany at top of abdomen, due to gas-filled intestines floating. 3. Shifting dullness > 4 cm. 4. Fluid wave. |
|
|
What are the five main causes of ascites?
|
Heart failure
Renal failure Liver failure Carcinomatosis Chronic peritonitis |
|
|
Name three tests for testing peritoneal inflammation.
|
1. Blumberg sign - press fingers in and release quickly. If it hurts more after releasing, this is positive.
2. Light percussion 3. Markle sign - patient stands on toes, and drops quickly on his heels. |
|
|
Rovsing's sign.
|
Sign of appendicitis.
Press in LLQ. Quickly remove fingers. Pain in RLQ suggests appendicitis. |
|
|
What opening does a gluteal hernia traverse?
|
Greater sciatic notch.
|
|
|
What opening does a sciatic hernia traverse?
|
Lesser sciatic notch.
|
|
|
What position is best used to do DRE?
|
Sims position
* Left lateral prone position |
|
|
What is the VACTERL syndrome?
|
It is a group of congenital anomalies that often occur together. If any one of them is seen in a pediatric patient, then you should look for the other ones too.
Vertebral anomaly Anal atresia Cardiac defect Tracheo-Esophageal fistula Renal defects Limb defects |
|
|
In a pediatric patient, what is the cause of visible peristalsis of the stomach, going from left to right?
|
Infantile hypertrophic pyloric stenosis.
|
|
|
Where do you feel for pyloric tumors?
|
Epigastric region.
|
|
|
What are 6 differences between the GI tract of newborn and 1 year old?
|
1. Slower gastric emptying time in newborn.
2. Young infant intolerance of certain foodstuffs. 3. Differences in colonic bacterial count and species. 4. GI tract immunity differences. 5. Physiological GERD seen in early infancy. 6. Infantile colic. |
|
|
What are some non-abdominal signs of GI disease in a child?
|
• Dematoses (eg. Erythema nodosum)
• Failure to thrive • Asthma • Uveitis • Joint swelling • Hematuria |
|
|
Signs of volume depletion in an infant.
|
• Lethargy
• Depressed fontanelle • Sunken eyes • Dry mucous membranes • Altered skin turgour • Tachycardia • Decreased capillary refill • Cool extremities • Hypotension |
|
|
What do cafe au lait spots with irregular borders on the posterior back skin indicate?
|
McCune Albrights syndrome
|
|
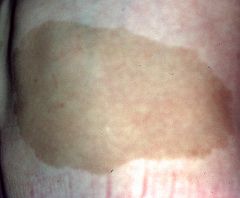
What do cafe au lait spots with regular borders on the posterior back skin indicate?
|
Neurofibromatosis.
|
|
|
How do you landmark for the hip joint?
|
Find the femoral pulse. Down 1 inch, lateral 1 inch is the hip joint.
|
|
|
Ortolani and Barlow maneuvers
|
• Tests for congenital hip dislocation
• Hold opposite hip maximally flexed • Adduct other hip and apply posterior directed force to try to sublux the hip joint. • Then abduct the hip to see if there is a clunk. |
|
|
Which metatarsal is most commonly fractured with a sudden increase in walking?
|
2nd metatarsal shaft.
|
|
|
If the third and fourth toes splay apart when the patient is standing, what is this a sign of?
|
Morton's neuroma.
|
|
|
How do you test for ankle joint passive ROM?
|
Must lock the subtalar joint by inverting the foot. This prevents compound movement of the subtalar and ankle joint.
Then you can flex or extend the ankle joint. |
|
|
How do you test subtalar joint passive ROM?
|
Dorsiflex the foot to lock the ankle joint. This prevents compound movement of the ankle joint with the subtalar joint.
Then you can invert/evert the foot to test the subtalar joint. |
|
|
If the little finger rests abducted, what is this a sign of?
|
Waternburg's sign.
An early sign of ulnar nerve injury. |
|
|
Finkelstein's test
|
Tests DeQuervain's tenosynovitis
Patient makes fist with thumb tucked inside. Passively ulnar deviate the wrist. Pain in first extensor compartment is positive sign. |
|
|
What is the normal range for intraocular pressure?
|
10-21 mmHg
|
|
|
Components of a full patient-centred history.
|
1. Identifying information.
2. Chief complaint. 3. HPI 4. Past medical history. 5. Medications. 6. Allergies 7. Family history. 8. Social history. 9. Lifestyle issues, preventions, immunizations. 10. Functional evaluation. 11. Review of systems. |
|
|
What is the chest wall excursion observation in patients with severe COPD called?
|
Modified Hoovers sign
- Normally the lateral ribs flare, and the costal margin widens with a deep inspiration. - If the lungs are over-inflated with a low flat diaphragm, the lateral chest wall may be drawn inwards with inspiration. |
|
|
What are the percussion notes that you can possibly elicit?
|
i. Normal resonance
ii. Dull • Consolidation. Similar note as over liver. iii. Flat • Over large pleural effusion. Similar to note over thigh. iv. Hyperresonant • Over large pneumothorax. v. Tympanic • A hollow sound. As over stomach bubble. |
|
|
Name the different breath sounds that you can hear, and where/when you would hear them.
|
Normal or vesicular breathing
• Abnormal if not present Bronchial breath sounds • Heard over consolidation, as in pneumonia. Bronchovesicular sounds • Heard over right upper lobe anteriorly, or between the scapulae Tubular breath sounds • Normally heard over the trachea, or sometimes over consolidation |
|
|
Name the causes of hearing early, late, or continuous crackles when auscultating the lungs.
|
◊ Early - bronchiectasis, occasionally with asthma
◊ Late - pulmonary fibrosis, CHF ◊ Continuous - pneumonia |
|
|
Chest signs that you would expect for consolidation, pleural effusion, pneumothorax, atelectasis, asthma, emphysema.
|

|
|
|
What is pulsus paradoxus?
|
A decrease in systolic pressure during inspiration, and/or an increase in systolic pressure during expiration
Normal if < 10 If > 10, this is called pulsus paradoxus Caused by: □ Cardiac tamponade □ Severe volume depletion □ Severe asthma |
|
|
For psychiatric interviews, when doing the mental status exam, what are the headings?
|
ASEPTIC
1. Appearance and general behaviour 2. Speech 3. Emotions • Both the examiners assessment through observation, and also by asking patient about • What their mood is like • Hopelessness? • Suicide? • Homicide? 4. Perception • Hallucinations, illusions 5. Thought form and content • Delusions • Obsessions • Phobias • Bradyphrenia 6. Insight (really a part of cognition) • Do they know that they are ill? 7. Cognition |
|
|
What are good prognostic features of schizophreniform disorder?
|
- acute onset of psychosis
- confusion at the peak of psychosis - good premorbid social and occupational functioning - lack of flattened affect |
|
|
What is the mnemonic for remembering what the components of an APGAR score are?
|
• Appearance
• Pulse (HR) • Grimace (reflex irritability) • Activity (muscle tone) • Respiratory rate |
|
|
When does the posterior fontanelle close?
|
3 months of less
|
|
|
What questions must you ask during an adolescent interview?
|
HEEADSSS questions
Home Education/employment Eating Activities Drugs Sexuality Suicide Safety |
|
|
What are the questions that you must as an adolescent regarding drugs?
Note: there is a mnemonic for this. |
CRAFFT questions
car, relax, alone, forget, friends, trouble Have you ever ridden in a car driven by someone who was high, or had been using drugs or alcohol Do you ever use alcohol or drugs to relax, feel better about yourself, or fit in? Do you ever use drugs or alcohol when you are alone? Do you forget things you did while using drugs or alcohol? Do your family or friends ever tell you that you should cut down your drinking or drug use? Have you ever gotten into trouble while using drugs or alcohol? |

