![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
38 Cards in this Set
- Front
- Back
|
What is the minimum dose of irradiation that must be delivered to any portion of a product for it to be considered adequately irradiated?
A. 5 Gy B. 25 Gy C. 100 Gy D. 50 Gy E. 15 Gy |
E. 15 Gy.
At least 15 Gy must be delivered to any point of the product while at least 25 Gy must be delivered to the middle of the product. After irradiation, it must be noted that the expiration date cannot exceed 28 days. |
|
|
Which of the following indications is an appropriate usage of irradiated products?
A. cellular products to immunocompromised hosts B. granulocyte concentrates for neutropenic sepsis C. prevention of alloimmunization in platelets D. red blood cells to prevent CMV transmission E. red blood cells to prevent recurrent febrile nonhemolytic transfusion reactions |
A. cellular products to immunocompromised hosts.
The only clear indication for irradiation is to prevent transfusion-associated graft v. host disease. By irradiating white blood cells, they are rendered incapable of engrafting in an immunocompromised host. Irradiated products do not prevent CMV transmission, alloimmunization, or recurrent febrile non-hemolytic transfusion reactions, like leukoreduction does. Furthermore, irradiating granulocytes would destroy your product. Don't do that. |
|
|
All of the following products would be useful in the treatment of symptomatic anemia in a patient that you wish to remain CMV negative, except:
A. red blood cells, CMV(-) by serology B. frozen, thawed, and deglycerolized red blood cells C. washed red blood cells D. red blood cells leukoreduced to <5 × 108 white blood cells E. all of the above are acceptable |
D. red blood cells leukoreduced to <5 × 10 8 white blood cells.
Red cell unit can contain up to 5 × 109 white blood cells/unit and should be reduced one order of magnitude in order to prevent febrile nonhemolytic transfusion reactions and three orders of magnitude to prevent CMV transmission or alloimmunization. Washed red blood cells are considered leukoreduced. Most experts believe that leukoreduced and CMV negative by serology units are equivalent in prevention of CMV transmission. |
|
|
Which is the first step in the workup of a suspected transfusion reaction?
A. call the blood bank B. stop the transfusion C. infuse a bolus of normal saline D. paperwork and bag check E. check urine for hemoglobin |
B. Stop the transfusion.
The first step in all transfusion reactions should be always be the same. STOP THE REACTION. Always, every time, always, always. The most important factor in determining the severity of reactions is the amount of product that is delivered to the patient. |
|
|
Which of the following is the most common cause of hemolytic transfusion reactions?
A. ABO incompatibility B. Rh incompatibility C. paperwork errors D. anti-Kidd alloantibodies E. mechanical hemolysis due to faulty packaging |
C. paperwork errors.
Unfortunately, clerical errors still account for a significant number of hemolytic transfusion reactions - patient ID, sample mislabeling, etc. |
|
|
Which of the following is the most common type of transfusion reaction?
A. febrile nonhemolytic transfusion reaction B. acute hemolytic transfusion reaction C. delayed hemolytic transfusion reaction D. transfusion-associated graft v. host disease E. transfusion-related acute lung injury |
A. febrile nonhemolytic transfusion reaction.
Luckily, the least severe reaction is the most common, reportedly seen in 0.5% of all transfusions. The most common cause of FNHTRs is cytokines elaborated from white blood cells while the unit is stored. A decreased incidence can be achieved with filtration of red blood cells at the time of collection as well as pretransfusion administration of acetaminophen to patients. |
|
|
What is the most common antibody associated with acute hemolytic transfusion reactions?
A. anti-D B. anti-Kidd C. anti-A/anti-B D. anti-Kell E. anti-Duffy |
C. anti-A/anti-B.
Intravascular acute hemolysis is most commonly due to anti-A or anti-B in cases of ABO incompatibility. The only other antibody of significance associated with acute intravascular hemolysis is anti-Kidd. All the other antibodies presented as choices are more commonly associated with extravascular hemolysis, either acute or delayed. |
|
|
All of the following are illness-causing bacteria most commonly associated with red blood cell transfusions, except:
A. Yersinia enterocolitica B. Serratia liquifaciens C. Citrobacter spp. D. Staphylococcus aureus E. Pseudomonas spp. |
D. S .
While platelet products are associated with contamination from gram-positive cocci, red blood cells are associated with gram-negative organisms, especially those listed in the choices (except Staph). Remember that red blood cells are refrigerated so organisms that grow in the cold will be favored. |
|
|
Why are most cases of transfusion-associated graft v. host disease seen in transfusions between related individuals?
A. common disease exposures B. HLA similarity, not identity C. shared non-genetic environmental exposures D. less compatibility E. less stringent donor requirements |
B. HLA similarity, not identity.
TAGVHD occurs most often when the recipient has an antigen that the donor does not, while all the donor's antigens are present in the recipient. This means that the recipient's white blood cells don't see the donor as foreign, however the donor's white blood cells react to the foreign antigen on the recipient's cells. |
|
|
All of the following are associated with transfusion-related acute lung injury, except:
A. patients on induction chemotherapy for lymphoma B. bypass patients C. blood stored for long periods of time D. multiparous female donors E. patients post-op from lung surgery |
E. patients post-op from lung surgery.
In addition, products containing plasma are more commonly associated with TRALI, perhaps due to anti-HLA antibodies from the donor unit. The diagnosis of TRALI is one of exclusion, after volume overload, sepsis, anaphylaxis, hemolysis, etc. have been ruled out. |
|
|
What feature of allergic transfusion reactions makes them unique?
A. the patient does not have to be treated; continue transfusion B. patient serum does not exhibit a positive DAT C. the reaction does not need to be reported D. the transfusion can be restarted after treating the patient E. they cause hemolysis |
D. the transfusion can be restarted after treating the patient.
Allergic transfusion reactions are unique because once it is determined that the patient is experiencing urticaria due to the transfusion, the patient can be treated with anti-histamines and the transfusion restarted. All of the other choices are either untrue or not unique. |
|
|
Which of the following factors involved with the degree of platelet refractoriness is the most important?
A. gender B. spleen status (present or absent) C. age D. height and weight E. active bleeding |
B. spleen status (present or absent).
The absence of a spleen is associated with the greatest platelet increments following transfusion. All of the other factors, with the exception of patient age, are associated with platelet refractoriness. To prevent the occurrence of refractoriness, one must try to prevent alloimmunization. |
|
|
Which of the following viruses is a patient at the highest risk of acquiring through a blood transfusion?
A. hepatitis B virus B. hepatitis C virus C. hepatitis A virus D. human immunodeficiency virus E. West Nile virus |
A. hepatitis B virus.
The viruses are presented in the order of risk of infection. HBV risk is at 1:100000, while HCV risk is 10 times lower and HAV mildly lower than HCV. HIV rates vary wildly but are in the same range as HCV and HAV. West Nile virus-associated infection has been reported in case reports. |
|
|
What is the purpose of rapid plasmin reagent testing on donated whole blood?
A. detection of N. gonorrheae infection B. detection of syphilis infection C. marker of Chagas disease D. detection of past CMV infection E. surrogate marker of high-risk behavior |
E. surrogate marker of high-risk behavior.
RPR is a confirmatory test for Treponema infections, but is a very poor screening test (low PPV). Instead, RPR positivity is used as a marker for other diseases associated with high-risk behavior (HIV, HCV). |
|
|
Which of the following red blood cell units would be the most difficult to find in donated blood?
A. type B B. c (-) C. Jk (a-b-) D. E (-) E. K (-) |
C. Jk (a-b-).
Of the major antigens associated with hemolysis, Kidd (Jk) is one of the more difficult to deal with. The Jk (a-b-) phenotype is rare. Jka is most commonly associated with hemolysis and luckily ~20% of the donor population is Jka-. |
|
|
What is the appropriate storage temperature for granulocyte concentrates?
A. 37°C B. 20-24°C C. 1-6°C D. -20°C E. -80°C |
B. 20-24°C.
Granulocyte concentrates must be collected and used within 24 hours. For that reason, the product is not routinely collected until it is needed. The optimal temperature at which to keep the product is 20-24°C (room temperature). |
|
|
After thawing, what is the time frame within which fresh frozen plasma must be used?
A. 8 hours B. 24 hours C. 2 days D. 7 days E. 30 days |
B. 24 hours.
There are a lot of numbers to remember with FFP preparation, storage, and use. The plasma separated from platelets by a hard spin must be frozen within 8 hours of collection to be considered “fresh frozen plasma.” The frozen product can be stored for up to 1 year as such, but then must be used within 24 hours of thawing. The product can be refrigerated and stored for 5 days, but it must be relabeled as thawed plasma with the expectation that it contains lower levels of coagulation factors, especially Factor V and VIII. |
|
|
All of the following are preferred uses of fresh frozen plasma, except:
A. multiple factor deficiencies in disseminated intravascular coagulation B. reversal of warfarin therapy C. massive transfusion D. replacement solution in plasmapheresis for thrombotic thrombocytopenic purpura E. hemophilia A |
E. hemophilia A.
FFP is best used in the situation of coagulopathy that results from the loss of multiple coagulation factors. Loss of single factors, such as Factor VIII in hemophilia A, is better treated with recombinant Factor VIII, or if needed, cryoprecipitate/FFP is also useful in TTP to return ADAMTS-13, in hereditary angioedema, to replace C1q, and in antithrombin deficiency. |
|
|
Cryoprecipitated plasma contains appreciable amounts of all of the following factors, except:
A. Factor VIII B. von Willebrand factor C. Factor XIII D. Factor V E. fibrinogen |
D. Factor V.
More numbers to remember. Each unit of cryo must contain at least 150 mg of fibrinogen and 80IU of Factor VIII. This is the same amount as in FFP (cryo is made from FFP), but instead of a volume of 200 mL, cryo has the factors in 15 mL. Cryo can be used to treat hemophilia, though for a number of reasons, recombinant Factor VIII is the preferred treatment. |
|
|
What is the minimum amount of platelets required in an apheresis platelet unit?
A. 3 × 1011 B. 3 × 1010 C. 1 × 1011 D. 1 × 1010 E. 1 × 108 |
A. 3 ×10 11.
An apheresis platelet unit is approximately equal to 6 single whole blood-collected units (the “6 pack”). Each individual platelet unit must contain at least 5.5 × 1010 platelets in at least 75% of the units tested. It makes sense that a “6 pack” would contain 6x more platelets than a single unit. |
|
|
ABO, Le, Lu, M, I, i, N, P.
|
Naturally-occurring antibodies
|
|
|
MNS, Kidd, C/c, E/e, Duffy.
|
Antigens that display dosage
|
|
|
Anti-M, N, P1, Lea, and Leb
|
Antibodies that react at room temperature:
|
|
|
anti-A, anti-Kell, anti-Jka, and anti-Fya
|
The 4 most common antibodies implicated in immediate HTR
|
|
|
I/i, P, Le, Rh, Kidd
|
Antigens that are enhanced by enzymes
|
|
|
MNSs, Fya, Fyb, Lutheran, Chido
|
Antigens that are destroyed by enzymes
|
|
|
anti-Jka, anti-E, anti-D, anti-C
|
4 most common antibodies implicated in delayed HTR
|
|
|
Lutheran, Sid, A3, and post-bone marrow transplant
|
Mixed field reactions are expected
|
|
|
ABO, Kidd, P (paroxysmal cold hemoglobinuria)
|
Antibodies that commonly produce intravascular hemolysis
|
|
|
anti-Jka, anti-E, anti-D, anti-C
|
4 most common antibodies implicated in delayed HTR
|
|
|
anti-AB, anti-D, anti-Kell, anti-c
|
4 most common antibodies implicated in HDN
|
|
|
Lutheran, Sid, A3, and post-bone marrow transplant
|
Mixed field reactions are expected
|
|
|
ABO, Kidd, P (paroxysmal cold hemoglobinuria)
|
Antibodies that commonly produce intravascular hemolysis
|
|
|
anti-AB, anti-D, anti-Kell, anti-c
|
4 most common antibodies implicated in HDN
|
|
|
((Platelet countpost – Platelet countpre) x BSAx 10^11)/
Number of platelets transfused |
corrected count increment(CCI)
|
|
|
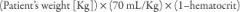
KB% x 5/3 = number of vials;
5=blood volume,if wt given x70ml/kg 3=#vials of RhIg needed don't forget to round up or down |
Kleihauer-Betke
Quantitative (maternal fetal hemorrhage) Acid-resistant Hgb F RBCs stain brightly |
|
|
(Total blood volume x (Platelet countpost – Platelet countpre) x 10^3)/
Number of platelets transfused ***use 10^11 in the denominator |
Post-transfusion Platelet Recovery (PPR)
|
|

|
|

