![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
Paraneoplastic syndrome |
An unusual or unexpected consequence of a tumour usually caused by secretion of a hormone, cytokine or hormone-like substance |
|
|
PNS may occur as a result of |
Immune-mediated mechanisms Peptide, protein, ectopic or eutopic hormone secretion Protein hormone precursor or cytokine secretion Enzyme production or other biochemical mechanisms which interfere with normal metabolic pathways |
|
|
Diagnosis effects |
PNS may be detected incidentally -> indicates occult malignancy May suggest a particular tumour type |
|
|
Management effects |
Oncologic emergency Parallel approach to tumour and PNS May be difficult to differentiate from adverse therapy effects |
|
|
Prognosis effects |
Co-morbid disease - negative prognostic factor Reduced performance may preclude/prevent certain therapies with knock-on effects on survival |
|
|
Quality of life effects |
Increased morbidity and deleterious long term effects Longer recovery and hospitalisation times with increased complexity of interventions |
|
|
Tumour response parallel of PNS |
Marker of clinical remission or relapse |
|
|
Role of parathyroid hormone |
Increases calcium mobilisation from bone Increases renal calcium reabsorption Increases calcitriol production in kidneys -> increases GI calcium reabsorption |
|
|
Role of vitamin D/calcitriol |
Increases calcium and phosphorus reabsorption by small intestine Exerts negative feedback on PTH synthesis and secretion |
|
|
Role of calcitonin |
Inhibits bone resorption by osteoclasts |
|
|
Why can calcitonin not really be used to treat hypercalcaemia? |
Osteoclasts become resistant to its effects after a few days |
|
|
Role of calcitonin in day to day calcium homeostasis |
Much less than that of PTH and calcitriol Emergency hormone |
|
|
Which neoplasm is known to commonly cause hypercalcaemia? |
Anal gland carcinoma - PTH-related protein |
|
|
What does the total calcium value consist of? |
Protein-bound calcium - 45% Complexed calcium - 5-10% Ionised calcium - 50% - physiologically most important |
|
|
Changes in plasma protein concentration e.g. albumen |
Will directly affect total calcium concentration, does not affect ionised calcium |
|
|
Measure |
Serum ionised calcium |
|
|
Which physiological processes are calcium ions involved in? |
Neuromuscular activity Blood coagulation Complement activation Exocrine and endocrine secretory Structural integrity of bone |
|
|
Clinical signs of hypercalcaemia |
Polydipsia, polyuria, weakness and depression Neurological signs Cardiac dysrhythmias, hypotension, bradycardia Vomiting, constipation, anorexia |
|
|
Severity of clinical signs depends on |
Magnitude, rate, pH, underlying cause, metastatic disease, intercurrent disease |
|
|
Differential diagnoses |
Artefact Malignancies - lymphoma, multiple myeloma, carcinomas; anal sac adenocarcinoma; parathyroid gland primary tumour Primary hyperparathyroidism Renal failure Hypoadrenocorticism Toxin ingestion Vitamin D toxicity Hyperthyroidism Bone disease Granulomatous disease Idiopathic |
|
|
Physical examination |
Nodes and rectal examination |
|
|
Diagnosis approach - order |
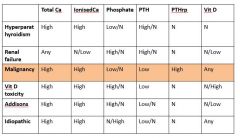
Clinical exam Measure serum ionised calcium Biopsy of tumour (if present), imaging for metastases, haemogram, serum biochemistry profile, urine analysis Body cavity and skeletal imaging and routine laboratory investigations BM aspirates - malignancy esp. lymphoid Blood assay of PTH, PTHrp and ionised calcium |
|
|
Does a normal PTH value rule out primary hyperparathyroidism? |
No, middle of range is still too high a value if animal has concurrent ionised hypercalcaemia -> confirms primary hpt Normal or low -> renal secondary hyperparathyroidism |
|
|
Diagnoses of hypercalcaemia |
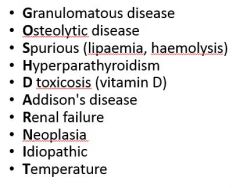
GOSHDARNIT |
|
|
Hypercalcaemia of malignancy pathophysiology |
Osteoclastic activating factors - IL-6, IL-1B, TGF-B,TNFa, RANKL Prostaglandin Calcitriol PTH PTHrp Osteolysis |
|
|
Hallmarks of malignancy |
gh |
|
|
treatment |
Severe hypocalcaemia - 1.5-2x maintenance intravenous sodium-replete isotonic fluid (e.g. 0.9% SODIUM CHLORIDE) and loop diuretic frusemide
Salmon calcitonin - powerful but transient, few days + osteoclast poisoning biphosphonate drug
Anti-neoplastic chemotherapeutic agents - diagnostic and therapeutic
Glucocorticoids - can reduce calcitriol GI calcium absorption - can confound diagnostic efforts with unconfirmed lymphoma |
|
|
Which diuretics should be avoided and why? |
Thiazide - can cause hypercalcaemia |
|
|
Frusemide role |
Diuretic - decreases tubular Ca resorption at Loop of Henle |
|
|
Biphosphonates role |
Bind Ca to hydroxyappetite crystals, decrease bone resorption, analgesic, anti-tumour effects |
|
|
Sodium bicarbonate |
Promotes alkalosis, increases protein-bound Ca fraction |
|
|
Dopamine role |
Inotrope, restore urine output, treat oliguric renal failure |
|
|
Which tumours are associated with paraneoplastic extreme leukocytosis? |
Certain carcinomas - little or no inflammation present |
|
|
Mechanism |
Tumour cells inappropriately secrete colony stimulating factors |
|
|
Which tumours are occasionally associated with polycythaemia? |
Renal umours |
|
|
Possible mechanisms |
Tumour compresses normal renal tissues -> renal tissue hypoxia -> erythropoietin expression by normal cells
Erythropoietin expression by tumour cells |
|
|
Paraneoplastic hypoglycaemia |
Insulin-secreting islet cell tumours Large liver tumours - hepatic carcinomas Leukaemias |
|
|
Clinical signs |
Seen in first two, not leukaemias |
|
|
Clinical signs |
Seizures Hind limb weakness Collapse |
|
|
Diagnostic tests |
Routine blood work Abdominal palpation X-rays Ultrasound (rules out large liver tumours, insulinomas too small to see this way usually) |
|
|
Mechanism |
Insulin-like growth factors produced by liver tumours |
|
|
Low glucose, medium insulin |
May be fine but probably inappropriately high for glucose concentration |
|
|
Causes |
Exercise Fasting After feeding - insulin Neuroglycopenic Compensatory adrenergic due to catecholamine release |
|
|
Severity of clinical signs depends on |
Absolute level Rate of fall Underlying cause Metastatic disease Duration |
|
|
Treatment |
Supportive therapy irrespective of aetiology Surgery - partial pancreatectomy for insulinoma with metastectomy as required, radical resection for other tumours |
|
|
Prognosis |
Good for benign tumours and where neurological damage is reversible |
|
|
Mast cell tumour PNS |
Hyperhistaminaemia Binds to H2 receptors on gastric parietal cells -> HCl release -> ulceration Binds to H1 receptors on areriole walls -> hypotension and vasodilation Increases capillary porosity -> oedema and shock Excessive haemorrhage and/or wound healing |
|
|
Treatment |
Diphenhydramine - blocks H1 receptors Ranitidine, cimetidine, famotidine - block H2 receptors |
|
|
Thymoma PNS |
Immune-mediated diseases Myasthenia gravis, blood dyscrasias, polymyopathies |
|
|
Acquired myasthenia gravis clinical signs |
Muscle weakness and regurgitation Muscles recover after brief period of cage rest, rapidly and progressively weaken with subsequent exercise |
|
|
Treatment |
Thymectomy Thymomectomy Immunosuppressant drugs - palliative |
|
|
Cancer cachexia |
Weight loss in the face of adequate calorific intake |
|
|
Mechanism |
Alterations in carbohydrate, lipid and protein metabolism; mediated by cytokines IL-1, TNF, IL-6 |
|
|
Treatment |
Poor prognosis Make sure patient receives adequate quantity of highly bioavailable nutrients present in palatable form |
|
|
Tumour metabolism |
Anaerobic -> lactic acidosis -> net energy deficit |
|
|
Tumour associated fever causes |
Rapid metabolism of cells e.g. leukaemia Leukopaenia and subsequent infection Release of tumour pyrogens -> hypothalamus |
|
|
Cancer-associated neurological disorders |
Cerebellar degeneration Optic neuritis Peripheral neuropathy Myesthenia gravis |
|
|
Cancers associated with hypertrophic osteopathy |
Thoracic neoplasia |
|
|
Mechanism |
Periosteal proliferation and subsequent osteophyte development (bony projections) -> palisades from cortical bone at 90 degrees |
|
|
Treatment |
Lameness resolves upon tumour removal Radiological changes may persist for months or years |

