![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
85 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
what are the major pathologic or structural changes associated with chronic bronchitis?
|
Chronic inflammation and swelling of the peripheral airways
Excessive mucus plugging and accumulation Partial or total mucus plugging Hyperinflation of alveoli (air trapping) Smooth muscle constriction of bronchial airways (bronchospasm) |
|
|
|
Anatomic Alterations of the Lungs with Chronic Bronchitis
|
Bronchial walls are narrowed by vasodilation, congestion and mucosal edema
Submucosal bronchial glands enlarge and goblet cells to increase resulting in excessive mucus The number and function of cilia lining in the tracheobronchial tree are diminished |
|
|
|
Definition of chronic bronchitis according to the American Thoracic Society
|
characterized by a daily, productive cough for at least 3 consecutive months each year for 2 years in a row.
|
|
|
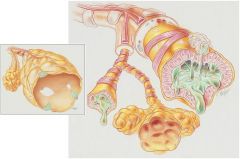
Anatomic Alterations of the Lungs associated with Chronic Bronchitis
|
Chronic inflammation and swelling of the peripheral airways
Excessive mucus production and accumulation Partial or total mucus plugging Hyperinflation of alveoli (air-trapping) Smooth muscle constriction of bronchial airways (bronchospasm) |
|
|
|
Clinical data obtained at the bedside - chronic bronchitis
|
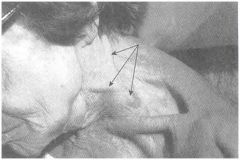
Use of Accessory Muscles during inspiration
|
|
|
|
Because polycythemia and cor pulmonale are associated with chronic bronchitis, what else might be seen?
|

pitting edema
distended neck veins enlarged and tender liver |
|
|
|
Main bronchodilators used in the treatment of COPD
|
Short Acting:
Ipratropium bromide Ipratropium bromide and alburterol sulfate (DuoNeb) Long Acting: Tiotropium bromide (Spiriva handihaler) |
|
|
What are the characteristics of Panacinar (Panlobular) emphysema
|
An abnormal weakening and enlargement of all air spaces distal to the terminal bronchioles, the respiratory bronchioles, alveolar ducts, alveolar sacs and alveoli.
|
The alveolar-capillary surface area is decreased.
Found in the lower parts of the lungs and associated with a1-antitrypsin |
|
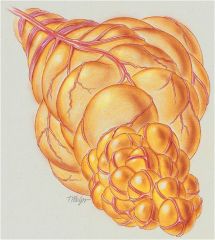
What does Centrilobular emphysema involve?
|
The respiratory bronchioles in the proximal portion of the acinus. The respiratory bronchial walls enlarge, become confluent and then are destroyed
|
Centalobular emphysema is the most common form of emphysema and is often associated with chronic bronchitis.
|
|

Radiologic Findings with Emphysema
|
Translucent (dark) lung fields
Depressed or flattened diaphragms Long and narrow heart Enlarged Heart Increased retrosternal air space (lateral radiograph) |
|
|
|
The immunologic Mechanism associated with Asthma
|
1) Lyphoid tissue cells form specific IgE antibodies which attach to mast cells in the bronchial walls
2) the mast cell degranulates and releases chemical mediators such as histamine 3) Chemical mediators stimulate parasympathetic nerve endings in the bronchial airways |
|
|
|
Typical meds/agents used in the treatment asthma
|
Sympathomimetics short and long acting
Parasympatholytics (anticholinergics) |
|
|
|
Aerosolized Medication Sympathomimetics - short to intermediate acting
|
Metaproterenol (Alupent, Metaprel)
Terbutaline (Brethine, Brethaire) Pirbuterol (Maxair) Albuterol (Ventoline, Proventil) Levalbuterol (Xopenex) |
|
|
|
Aerosolized Medication Sympathomimetics - long acting
|
Salmeterol (Serevent)
Formoterol (Foradil) |
|
|
|
Aerosolized Medication Parasympatholytics (anticholinergics)
|
Atropine sulfate (Dey-Dose Atropine Sulfate)
Ipratropium bromide (Atrovent) Tiotroprium (Spirva) Ipratropium bromide and Albuterol (Combivent) |
|
|
|
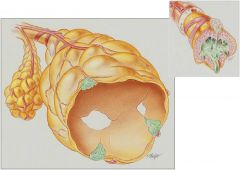
Three forms of bronchiectasis
|
Varicose (fusiform)
Cylindrical (tubular) Saccular (cystic) |
|
|
|
Cylindrical (tubular) bronchiectasis
|
The bronchi are dilated and constricted in an irrecgular fashion similar to varicose veins, ultimately resulting in a distorted, bulbous shape
|
|
|
|
Major pathologic or structural changes associated with bronchiectasis
|
Chronic dilation and distortion of bronchial airways
Excessive production of often foul-smelling sputum Smooth muscle constriction of bronchial airways Hyperinflation of alveoli (air trapping) Atelectasis, consolidation, and parenchymal fibrosis Hemorrhage secondary to bronchial arterial erosion |
|
|
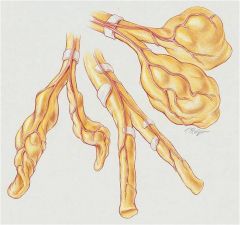
Bronchiectasis
|
A) Varicose bronchiectasis
B) Cylindrical bronchiectasis C) Saccular bronchiectasis |
|
|
|
What are the major structural changes associated with Pneumonia?
|
In flammation of the alveoli
Alveolar consolidation Atelectasis (aspiration pneumonia) |
|
|
|
Radiographic findings associated with alveolar consolidation related to pneumonia
|
Increased density (from consolidation atelectasis)
Air bronchograms Pleural effusions |
|
|
|
Identify the organisms primarily responsible for causing pneumonia in the hospitalized patient.
|
P. aeruginosa, S. aureus, K. pneumoniae, E. coli, Serratia species and oral anaerobes (aspiration)
|
|
|
|
Treatment protocols for the management of postoperative atelectasis
|
Oxygen therapy protocol
Hyperinflation therapy protocol Mechanical Ventilation protocol |
|
|
|
This disorders that make up COPD
|
Chronic bronchitis
Emphysema Asthma |
|
|
|
Radiographic findings associated with chronic bronchitis
|
Translucent (dark) lung fields
Depressed diaphragms and long and narrow heart |
|
|
|
Is pneumonia a restrictive or obstructive disease.
|
Restrictive
|
|
|
|
Definition of lung abscess:
|
Necrosis of lung tissue that in severe cases, leads to a localized air and fluid-filled cavity
|
|
|
|
First line drug to treat TB
|
Isoniazid (INH) and rifampin (Rifadin) are first line agents prescribed for the entire 9 months.
|
|
|
|
Wheal size in a positive TB test
|
10 mm or greater is considered positive
|
|
|
|
Identifiy the area of the lung where TB spores flourish
|
Apex of the lung
|
|
|
|
Most common fungal infection in the US
|
Histoplasmosis
|
|
|
|
Medication of choice to treate Histoplasmosis
|
IV administration of amphotericin B
|
|
|
|
Causes of non-cardiogenic pulmonary edema
|
Increased capillary permeability
Lymphatic Insufficiency Decreased intrapleural pressure Decreased oncotic pressure |
|
|
|
Causes of cardiogenic pulmonary edema
|
Arrhythmias producing low cardiac output
Congenital heart defects Excessive fluid amin. Left ventricular failure Mitral or aortic valve disease Myocardial infarction Pulmonary embolus Renal failure Rheumatic heart disease Systemic hypertension |
|
|
|
Major pathologic or structural changes of the lungs associated with pulmonary edema
|
Interstitial edema
Alveolar flooding Increased surface tension of pulmonary surfactant |
|
|
|
The use of mask CPAP to treat pulmonary edema
|
Maski CPAP improves decreased lung compliance, decreases the work of breathing, enhances gas exchange, and decreases vascular congestion in patients with pulmonary edema
|
|
|
|
Define pulmonary embolism
|
pulmonary embolism occurs when a blood clot (thrombus) becomes disloged from veins elsewherein the body and moves (embolizes) into the pulmonary arterial circulation.
|
|
|
|
Methods of testing that are useful in the diagnosis of pulmonary embolism
|
XRay
Electrocardiogram (ECG) Ventilation/perfusion scan (V/Q scan) Fast computed tomography scan (CT) Pulmonary Angiogram |
|
|
|
Define flail chest
|
A flail chest is the result of double fractures of at least three or more adjacent ribs, which causes the thoracic cage to become unstable
|
|
|
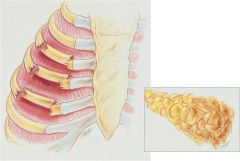
Different procedures, protocols and medications for managing the patient with flail chest
|
Medication for pain and routine bronchial hygiene in mild cases.
|
In more severe cases stabilization of the chest is required to allow bone healing and prevent atelectasis.
O2 therapy protocol Hyperinflation therapy protocol Mechanical Ventilator protocol |
|
|
Define pneumothorax
|
A pneumothrorx exists when gas (sometimes called free air) accumulates in the pleural space
|
|
|
|
Major pathologic and structural
changes associated with a pneumothorax |
Lung collapse
Ateletasis Chest wall expansion Compression of the great veins and decreased cardiac venous return |
|
|
|
When to employ the use a chest tube to treat a
pneumothorax |
When the pneumothorax is larger than 20%, it should be evacuated. In more serious cases, a chest tube is inserted into the patients pleural cavity
|
|
|
|
The most common cause of pleural effusion (2) The major causes of an exudative effusion
|
Malignant pleural effusions
Malignant mesotheliomas Pneumonias Tuberculosis Fungal diseases |
|
|
|
Describe the type fluid that makes up a
transudative pleural effusion |
thin watery containing a few blood cells and little protein
|
|
|
|
Define the terms empyema and hemothorax
|
Empyema is the accumulation of pus in the pleural cavity
Hemothorax is the presence of blood in in the pleural space |
|
|
|
Type of mediastinal shift associated with a pleural
effusion. |
Mediastinal shift to the unaffected side
|
|
|
|
Structural / pathologic changes associated with
pleural effusion |
Lung compression
Atelectasis Compression of the great veins and decreased cardiac venous return |
|
|
|
Radiographic technique used for identifying a
pleural effusion |
Chest X-Ray
|
|
|
|
Type of breath sounds, fremitus, and percussion
note associated with kyphoscoliosis |
Bronchial breath sounds
Increased tactile and vocal fremitus Dull percussion note |
|
|
|
Define “pneumoconiosis”
|
general term used to describe diseases of the lungs that are caused by the chonic inhalation of inorganic dusts and particulate matter usually of occupational or environmental origin
|
|
|
|
Structural / pathologic changes associated with
pneumoconiosis |
Destruction of the alveoli and adjacent pulmonary capillaries
Fibrotic thickening of the respiratory bronchioles, alveolar ducts, and alveoli Cystlike structures (honeycomb appearance) fibrocalcific pleural plaques Airway obstruction caused by inflammation and excessive bronchial secretions Bronchospasm Bronchogenic carinoma Mesothelioma |
|
|
|
Describe the chest radiograph for the patient
suffering from asbestosis |
Small round opacities scattered throughout the lung
Irregularly shaped opacities Irregular cardiac and diaphragmatic borders Pleural plaques Honeycomb appearance |
|
|
|
Identify the type of hypoxemia associated with
capillary shunting in “pneumoconiosis” |
The hypoxemia that develops in pneumoconiosis is most commonly caused by alveolar thickening, fibrosis, and capillary shunting. Hypoxemia caused by capillary shunting is often refractory to oxygen therapy.
|
|
|
|
Define cancer
|
Cancer is a general term that refers to abnormal new tissue growth characterized by the progressive, uncontrolled multiplication of cells.
|
|
|
|
Identify those types of cancers that are considered
non-small cell lung cancer. |
Squamous (Epidermoid) Cell Carcinoma
Adenocarcinoma (Including bronchioalveolar cell carcinoma) |
|
|
|
Type of lung cancer most associated with smoking
|
Small-cell lung cancer
|
|
|
|
Describe the origin of squamous cell carcinoma
|
The tumor originates from the basal cells of the bronchial epithelium and grows through the epithelium before invading the surrounding tissues.
|
|
|
|
Lettering and numeric elements of the TNM
classification system for staging lung cancer |
Stage 0: the cancer is limited to the lining of the bronchial airways (TisNOMO)
Stage I: the tumor is less than 3 cm and located in lobar or distal airways (T1NOMO) Stage II: The cancer has invaded neighboring lymph nodes (T1N1MO) Stage III A: the tumor is any size - local invasion involves chest wall, diaphragm, mediastinal, pleural or parietal pericardium (T3N1MO) Stage III B: the cancer has spread locally to areas such as mediastinum, heart, blood vessels, trachea, esophagus, vertebral body (T4 and N, MO) |
|
|
|
Best treatment option for the patient with small cell
carcinoma of the lung |
Chemotherapy - either alone or in combination with radiation therapy
|
|
|
|
Is ARDS an obstructive or restrictive disease?
|
Restrictive
|
|
|
|
Major structural / pathologic changes associated
with ARDS |
Interstitial and intra-alveolar edema and hemorrhage
Alveolar consolidation Intra-alveolar hyaline membrane Pulmonary surfactant deficiency or abnormality Atelectasis |
|
|
|
Ventilation strategy for managing the patient with
ARDS in terms of setting the tidal volume and respiratory rate |
low tidal volumes and high respiratory rate
initial tidal volume set at 4 to 8 ml/kg and ventilatory rate as high as 35 breaths/min |
|
|
|
Refractory hypoxemia associated with ARDS
|
the hypoxemia that develops in ARDS most commonly is caused by widespread alveolar consolidation, atelectasis, and capillary shunting. Hypoxemia caused by capillary shunting often is refractory to oxygen therapy.
|
|
|
|
Commonly prescribed medications used in the
treatment of ARDS |
Antibiotics
Diuretic Agents Corticosteroids |
|
|
|
Define “extrinsic allergic alveolitis”
|
also called hypersensitivity pneumonitis - is an immunologically medicated inflammation of the lungs caused by the inhalation of a variety of offending agents such as pollen, animal dander, organic dusts and spores.
|
|
|
|
Clinical findings associated with chronic interstitial
lung disease (ABGs, PFTs, Shunting and DO2) |
pH increased, PaCO2 decreased, HCO3- (slightly) decreased PaO2 decreased
|
|
|
|
Goal of plasmapheresis in treating chronic
interstitial lung disease |
Reduces the circulating anti-GBM antibodies that attack the patient's flomerular basement membrane.
|
|
|
|
Define Guillain- Barre Syndrome (GBS)
|
Relatively rare disorder of the peripheral nervous system in which flaccid paralysis of the the skeletal muscle and loss of reflexes develop in a previously healthy patient
|
|
|
|
What is the usual onset of GBS?
|
The onset of Guillain-Barre syndrome frequently occurs 1 to 4 weeks after a febrile episode such as an upper respiratory or gastrointestinal illness.
|
|
|
|
Etiology of GBS
|
The precise cause of Guillain-Barre syndrome is not known.It is probably an immune disorder that causes inflammation and deterioration of the patient's peripheral nervous system.
|
|
|
|
Structural / pathologic changes associated with
GBS |
Mucus accumulation
Airway obstruction Alveolar consolidation Atelectasis |
|
|
|
The goal of plasmapheresis in GBS
|
Remove the antibodies from the plasma that contribute to the immune system attack on the peripheral nerves.
|
|
|
|
Identify treatment modalities beneficial in the
management of the GBS patient |
Plasmapheresis
Infustion of immunoglobulin Corticosteroids |
|
|
|
Identify non-cardiopulmonary manifestations
associated with myasthenia gravis. |
Weakness of striated muscles:
Eye muscles - drooping of the upper eyelids Extraocular muscles - double vision Muscles of the lower protion of the face - speech impairment Chewing and swallowing muscles Skeletal muscles of the arms and legs |
|
|
|
Useful techniques used in diagnosing myasthenia
gravis |
Clinical history
Neurologic examination Electromyography Blood analysis Edrophonium test CT or MRI |
|
|
|
Beneficial treatment modalities in managing the
severely ill patient with myasthenia gravis. |
Adrenocorticotropic hormone (ACTH)
|
|
|
|
Identify the probable cause of myasthenia gravis
|
The cause appears to be related to circulating antibodies of the autoimmune sytem (anti-ACh receptor antibodies)
|
|
|
|
Clinical findings associated with myasthenia gravis
(PFTs, ABGs, DO2, and Shunting) |
FVC, FEVt, FEF 20%-75%, FEF 200-1200, PEFR, MVV, FEF 50%, FEV1% all decreased
|
ABG's
pH decreased PaCO2 increased HCO3- increased (slightly) PaO2 decreased DO2 -decreased Shunting - increased |
|
|
Describe the role of the thymus gland in
myasthenia gravis |
The thymus gland in the myasthenic patient frequently appears to be the source of anti-ACh receptor antibodies
|
|
|
|
Recognize the treatment options for managing the
patient with myasthenia gravis |
Cholinesterase inhibitors
Immunosuppressants Adrenocorticotropic hormone therapy Thymectomy Plasmapheresis |
O2 therapy protocol
Bronchopulmonary hygiene therapy protocol Hyperinflation therapy protocol Mechanical ventilation protocol |
|
|
Cite the most common sleep disorder seen in the
clinical setting |
Obstructive sleep apnea
|
|
|
|
Recognize the general clinical manifestations
associated with obstructive sleep apnea (OSA) |
Chronic loud snoring
Hypertension Morning headaches Systemic hypertension Congestive heart failure Nausea Dry mouth upon awakening Intellectual and personality changes |
Memory loss
Depression Sexual impotence Nocturnal enuresis Excessive daytime sleepiness Auto accidents Pulmonary hypertension and/or cor pulmonale |
|
|
Recognize that polysomnography as a means of diagnosing OSA
|
Include an EEG and electro-oculogram (EOG) to identify sleep stages. Use a monitoring device for airflow, and ECG to identify cardiac arrhythmias, impedance pneumography, intercostal elctromyography
|
Esophageal manometry to monitor the patient's ventilatory rate and effort, ear oximetry or transcutaneous O2 monitoring
|
|
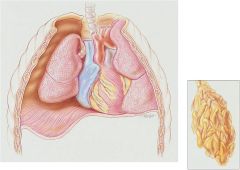
Pneumothorax
|
Right-side pneumothorax. GA, Gas accumulation; DD, depressed diaphragm; CL, collapsed lung. Inset, Atelectasis, a common secondary anatomic alteration of the lungs
|
|

