![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
206 Cards in this Set
- Front
- Back
|
How do each of the following effect t4 and t3 resin uptake levels:
Hyperthyroidism, Hypothyroidism, High levels of TBG, Low levels of TBG |
Hyper-- both increased
Hypo- Both decreased High TBG- T4 incresed, t3r decreased Low TBG- T4 decreased, t3r increased |
|
|
How do each of the following effect t4 and t-uptake levels:
Hyperthyroidism, Hypothyroidism, High levels of TBG, Low levels of TBG |
Hyper- T4 incresed, t-up decreased
Hypo- T4 decreased, t-up increased High TBG- Both increased Low TBG- Both decreased |
|
|
What is t3 resin uptake a measure of?
|
Amount of left over radioactive T3 after adding a set amount of radioactive T3 to Thyroid binding globulin.
|
|
|
What is t-uptake a measure of?
|
Amount of free spaces left on Thyroid binding globulin (add set amount of measurable t3, remove excess)
|
|
|
What enzyme is affected in Hashimoto's thyroiditis?
|
Thyroid peroxidase (Breaks thyroglobulin in two; t4-t3 ---> t4 + t3
Also antibody seen in Graves 80% of time. |
|
|
What is the most important antibody seen in Graves' disease?
|
Anti TSH receptor (stimulates production)
|
|
|
How do we measure TSH stimulating antibodies in Graves' disease?
|
Grow thyroid cells in culture
Add pt. serum Measure cAMP production |
|
|
How is thyroid cancer followed post-thyroidectomy?
What if auto-antibodies are present? |
Measure thyroglobulin levels (t4-t4, t4-t3 form before peroxidase). These are elevated in most thyroid cancers (papillary and follicular)
Measure titers of anti-thyroglobulin antibodies. --Generally both are ordered in pts. |
|
|
What is the most likely cause of a normal t4 (bound and free), normal tsh, and low t3?
|
illness- illness causes decreased peripheral conversion of t4--->t3
|
|
|
Cause of Normal TSH, Normal free t4, High bound t4 and t3?
|
High thyroid binding globulin levels:
estrogens, phenothiazines, opiates |
|
|
When is ACTH production the highest? Lowest?
|
Upon waking
Early in sleep |
|
|
What molecule can be easily measured in saliva?
|
Cortisol - Free cortisol crosses into the saliva and is stable for up to 1 week.
|
|
|
What type of lactic acidosis will cause an anion gap but will not show increased levels of lactic acid on chemistry?
|
Bacterial overgrowth in gut with increased production of d-lactic acid (an isomer). Traditional assays do not pick up this chemical.
|
|
|
What is cortrosyn and what is it used for?
|
A synthetic ACTH (1000x normal potency) used to look for adrenal insufficiency.
|
|
|
How does our body compensate for a respiratory acidosis (mechanism)?
|
Urinary secretion of H+ and NH4+ (ammonium)
|
|
|
Metyrapone blocks the production of what subtrate? What is the measurable results?
|
11-deoxycortisol--\\-->cortisol
Normal patients can overcome this block(increased ACTH) while pts. with imparied pituitary function cannot. |
|
|
What tumors most commonly produce ACTH?
|
Adrenal adenoma/carcinoma
Small cell and carcinoid lung tumors |
|
|
What is the difference between Cushing's syndrome and Cushing's disease?
|
Syndrome= increased cortisol by any method
Disease= pituitary ACTH tumor (70% of Cushing's syndrome cases) |
|
|
How is urine anion gap calculated and how do you interpret the results?
|
(Na+) + (K+) - (Cl-) = UAG
UAG<0 in diarrhea, acetazolamide use and proximal tubular acidosis UAG>0 in distal tubular acidosis and CRF UAG=0 in normal |
|
|
What causes skin pigmentation with addison's disease?
|
Melanocyte stimulating factor (an ACTH derivative)
|
|
|
Decreased plasma cortisol
Increased ACTH |
Primary adrenal insufficiency (addison's disease)
|
|
|
What is the main intracellular anion?
What is the main extracellular anion? |
Phosphate
Chloride |
|
|
Congenital adrenal hyperplasia is caused by a deficiency of what enzyme?
What substrate accumulates? |
21-hydroxylase
-low cortisol, low aldosterone 17-hydroxy-progesterone |
|
|
Why do females with 21-hydroxylase definciency have ambiguous genitalia?
|
Accumulation of 17-hydroxy-progesterone which acts as an androgen (also salt wasting)
-mild deficiency shows hirsutism and irregular periods after puberty |
|
|
Why with certain assays are sodium levels falsely lowered in hyperlipidemia
|
Fat does not contain sodium. When the device measures sodium/volume (vs. electrical current), you see falsely lowered values.
|
|
|
Hypertension, hypokalemia
Decreased renin Increased aldosterone |
Primary hyperaldosteronism
|
|
|
Since catecholamines change too much throughout the day, what test is used to indirectly measure catecholamines?
|
Urine or plasma metanephrines (fractionated)
VMA is a measure of total metanephrines (epi + nor) - may not be elevated in epi tumor. |
|
|
What genetic abnormality is associated with a worse prognosis in Neuroblastoma?
|
N-myc amplification
|
|
|
How is neuroblastoma followed?
|
Levels of VMA and HVA (dopamine derivative)
|
|
|
Prolactin production is inhibited by what feedback mechanism?
Causes? |
Dopamine
Pituitary adenoma (75%) Stalk compression (15%) Drugs, other |
|
|
When are growth hormone levels the highest?
|
During sleep or acute stress
|
|
|
What is the effect of Growth hormone on the liver?
|
Produces IGF-1 which promotes bone growth (IGF-1 can be used as a measure of GH levels).
|
|
|
With excess Growth hormone production, what can be used to potentially suppress levels to check for tumor?
|
Glucose- test 1 hour after oral glucose load, failure to suppress in tumors
|
|
|
What is best test to check for/follow growth hormone levels?
|
IGF-1 (produced by liver in response to GH)
|
|
|
What is the primary feedback on FSH?
What is the primary feedback on LH? |
Inhibin (seritoli cells)
Sex steroids (estrogen/progesterone) (leydig cells) |
|
|
What hormone stimulates spermatogenesis?
|
FSH
|
|
|
What hormone stimulates testosterone production?
|
LH
|
|
|
What enzyme converts testosterone in dihydrotestosterone in the periphery?
|
5 alpha reductase
(inhibitors used for cancer and BPH) |
|
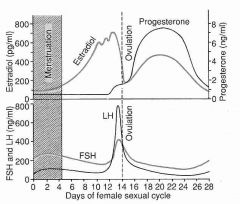
Know this!
|
Progesterone dominant after ovulation
Estrogen dominant before ovulation Fall in estrogen is the cause of LH surge |
|
|
What are the substrates measured in serum HCG vs. urine HCG
|
Serum assay uses antibody to the beta-subunit
Urine assay uses antibody to the beta-core fragment |
|
|
What is a good test for adrenal androgen overproduction?
Ovarian overproduction |
DHEA-S
Dehydroepiandrosterone bound to sulfate Testosterone |
|
|
21-hydroxylase deficiency with build up of 17-OH progesterone is the most common cause of congenital adrenal hyperplasia; what is the second most common cause?
|
11-hydroxylase deficiency with build up of 11-deoxycortisol (also causes hypertension)
|
|
|
When serum calcium levels are low, what happens to PTH levels?
|
Increased
|
|
|
What effect does PTH have on the kidney?
|
Blocks the reabsorbtion of phosphate and bicarbonate (HCO3)
----> less complexed/bound calcium ----> also by decreased pH |
|
|
What is the reaction of vitamin D in the liver?
|
Hydroxylated by 25-hydroxylase to 25-hydroxycholecalciferol
25(OH)D 25(OH)D is the most often measured vitamin D form |
|
|
What is the reaction of vitamin D in the proximal tubules?
|
1 alpha hydroxylase (activated by parathyroid hormone) converting 25-hydroxycholecalciferol to 1,25 dihydroxycholecalciferol (calcitriol, note the 3 -OH groups) 1,25 (OH)D
|
|
|
What is a major interference for measuring total calcium by colorimetric assay?
|
Gadolinium (MRI)
|
|
|
Most hypercalcemia due to tumor is caused by production of Parathyroid related protein (PTHrP); what tumors commonly produce PTHrP?
|
Squamous cell carcinoma (anywhere)
Breast RCC (1/3rd of all cases) |
|
|
How can sarcoidosis causes hypercalemia?
|
Production of calcitriol (also some lymphomas)
|
|
|
What is the effect of low magnesium (hypomagnesemia) on calcium?
|
Hypocalcemia (needed for parathyroid hormone?)
|
|
|
What two antibodies are seen in Hashimoto thyroiditis?
|
anti-microsomal
anti-thyroglobulin |
|
|
What should be considered with a low TSH but normal T4?
|
Thyrotoxicosis- measure free t3 levels to see if high
|
|
|
What is the effect of amiodarone on the thyroid?
|
Depends. Contains lots of iodine so causes hyperthyroidism in iodine-poor areas. It is toxic to the thyroid so causes hypothyroidism in iodine-rich areas.
|
|
|
How does Vmax relate to substrate concentration
|
1/2 Vmax=[S]
|
|
|
Does a small Km mean fast or slow reactions?
|
The smaller the Km, the faster the reaction.
|
|
|
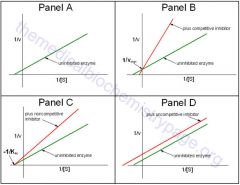
On a Lineweaver-Burk plot, an increased X-intercept (slope) without change in the Y intercept means what?
|
1/Vmax= Y-intercept, therefor no change
Slope and X-intercept are proportional to Km, so increase slope means increase Km ---> competitive inhibitor |
|
|
What does a non-competitive inhibitor look like on a Lineweaver-Burk plot?
|
Decreased V-max ---> increased Y-intercept
Km unchanged |
|
|
review
|
|
|
Which enzyme is more specific for liver damage, ALT or AST
|
ALT - Also found in kindey in lesser quantities in muscle
AST- Kindey, Muscle |
|
|
Why is AST more elevated in alcoholic liver
|
Pyrodoxine (B6) is co-enzyme for production of both but ALT is more dependent on it. Also there is mitochondrial AST which can be release with damage.
|
|
|
LD (lactate dehydrogenase) has five isoenzymes. Where are each found?
|
LD1- Heart, RBC's, Renal cortex
LD2- Heart, RBC's, Renal cortex LD3- Lung, Pancrease, plts, lymphs LD4- ------ LD5- Liver, Muscle, Prostate |
|
|
What LD marker is normally at the highest level?
|
LD2
|
|
|
What does an LD1/LD2 flip mean?
LD1>LD2 |
Heart attack, hemolysis or renal cortex necrosis
|
|
|
Elevated L1 and L5
|
Heart attack with centrilobular necrosis from congestion
|
|
|
Alkaline phosphatase comes from what 3 major sources?
1 minor |
Liver (biliary tract disease)
Bone (osteoblastic activity) Placenta/germ cell (pregnancy/germ cell tumor) Minor: intestinal disease of the ileum |
|
|
Why are alkaline phasphatase much higher in children?
|
Bone growth and repair, secreted by osteoblasts
-Also elevated in bone disease or fracture |
|
|
If alkaline phosphatase is elevated but the source is unclear, what other enzyme would indicate biliary tract origin?
|
GGT
|
|
|
Which hepatitis viruses are RNA viruses? DNA?
|
RNA= A, C and D
DNA- B |
|
|
Antimitochondrial autoantibodies are elevated in what disease?
|
Primary biliary cirrhosis
-destruction of intrahepatic bile ducts |
|
|
Smooth muscle autoantibody and anti-LKM are elevated in what disease?
|
Autoimmune hepatitis
|
|
|
What enzyme converts unconjugated bilirubin to conjugated bilirubin?
|
UDP-glucuronyl transferase
-deficient or absent in some newborns, congenitally in Crigler-Najjar syndrome and Gilberts |
|
|
UDP-glucuronyl transferase is absent in what disorder?
|
Crigler-Najjar syndrome
-it is decreased in gilbert's |
|
|
What is effected in Dubin-Johnson syndrome?
|
Inability to secrete conjugated bilirubin out of hepatocytes into the bile.
|
|
|
What is the rate-limiting step in bilirubin conjugation?
|
Transfer of the conjugated bilirubin into bile duct, thus hepatitis gives you conjugated bilirubinemia
|
|
|
Indirect and direct bilirubin refer to what?
|
Reflection of the methodologies used to measure the bilirubin
Indirect = Unconjugated Direct= Conjuaged Total can be measured |
|
|
How is bilirubin converted to urobilinogen?
|
By the intestinal flora
|
|
|
How does the diazo-colorimetric method work?
|
Formation of a colored dye when bilirubin reacts with a diazo compound. Alcohol (an accelerator) is added to allow the unconjugated to react. Thus direct and total are measured.
|
|
|
Other then diazo-colorimetric rxn, what other method can be used to measure bilirubin?
|
Direct spectrophotometry
absorbance at 455 nm -only measures total bilirubin |
|
|
What can be used as a longer term indicator of elevated conjugated hyperbilirubinemia?
|
delta-bilirubin, conjugated bilirubin covalently bound to albumin (not excreted)
|
|
|
what is the absorbtion spectrum of NADH?
|
340 nm
|
|
|
what is the difference between a noncompetitive and uncompetitive inhibitor
|
Noncom. binds enzyme away from the binding site, thus only decreasing Vmax. uncom. binds the enzyme with the substrate, thus decreasing Vmax and Km
|
|
|
What is the effect of renal failure on AST and ALT levels?
|
Both are decreased
|
|
|
What is the effect of heat/urea inhibition on bone and placental Alk phosphatase isoenzymes?
|
Bone isoenzymes are inactivated (burns), placental isoenzymes (persist)
|
|
|
Why is phototherapy not helpful in hyperbilirubinemia due to Dubin-Johnson syndrome?
|
Dubin-Johnson syndrome is a conjugated hyperbilirubinemia; phototherapy only converts unconjugated bilirubin
|
|
|
Breast milk jaundice generally occurs how long after birth?
|
>1 week
|
|
|
Congenital enzyme definiciencies generally present themselves with jaundice how long after birth?
|
>1 week
|
|
|
True or False
PT levels correlate with degree of hepatic injury? AST? ALT? Bilirubin? |
PT is the best indicator of prognosis with hepatic injury(>4.0 = bad) bilirubin of >15 is bad; AST and ALT are poor markers and do not correlate well with degree of injury
|
|
|
Electrophoresis for salivary and pancreatic enzymes show what pattern?
|
There are 6 isoenzymes. Salivary move the farthest, while pancreatic are the slowest.
|
|
|
What inhibition test/substance can be used to differentiate salivary and pancreatic amylase?
|
Salivary amylase is inhibited by "triticum vulgaris" a wheat germ lectin.
Pancreatic amylase is not. |
|
|
Why are amylase levels not elevated in 10% of patients with pancreatitis?
|
This is due to pts. with hypertriglyceridemia associated pancreatitis. Triglycerides interfere with the amylase assay.
|
|
|
True or False
Serum amylase levels correlate with severity of pancreatitis? Lipase? |
False
False |
|
|
What is the result of Macroamylasemia (Ig-amylase complexes) on serum and urine amylase levels respectively?
|
Serum- markedly elevated
Urine- Normal |
|
|
What are the advantages of lipase over amylase to measure pancreatitis?
|
They both rise within hours, but amylase drops within 2 days while lipase drops within 2 weeks. Lipase is more specific. Lipase is less effected by renal clearance.
|
|
|
What is the defect in Rotor syndrome?
|
Decreased hepatic glutathione-S-transferase levels
|
|
|
What enzyme is elevated in Sarcoidosis?
|
ACE (angiotensin converting enzyme)
|
|
|
What isoenzymes of Creatine kinase travel the furthest on electrophoresis?
Which hump is elevated with MI? |
BB followed by MB followed by MM
MB is elevated with MI (middle peak) |
|
|
The MB isoenzyme of CK can be separated (by electrophoresis) into two peaks, M-lys-B and M-B. Which is elevated in MI?
|
The M-lys-B is elevated in MI. It travels further on electrophoresis making a distinct double peak when present.
|
|
|
3 types of troponin are are found on actin; which two forms are elevated in MI?
|
C - I - T are the 3 forms
I and T are elevated in MI |
|
|
How long does it take for troponins (I and T) to elevate after MI?
Myoglobin? CK-MB? |
4-6 hours
1.5, 1.5 |
|
|
How long does myoglobin stay elevated after MI?
CK-MB isoforms? Troponin T? Tropoinin I? |
12 hours
2 days 2 weeks 5 days |
|
|
You have a suspicion of a repeat MI but don't have a previous troponin, what test would be helpful?
|
CK-MB isoform will only be elevated for 2 days so measuring this could demonstrate a repeat MI
|
|
|
Are troponins elevated with skeletal muscle damage/trauma?
CK-MB? |
No
Yes |
|
|
Can troponins be used to detect unstable angina?
|
Yes, a borderline elevated troponin indicates angina however the sensitivity and specificity aren't great. Troponins can also be elevated in renal disease and infer a worse prognosis.
|
|
|
ProBNP gets cleaved into NT-proBNP and BNP; how is this useful?
|
NT-proBNP rises more with heart failure, has a longer half-life and is not interfered with when synthetic BNP is administered
|
|
|
Where is Lipoprotein lipase located and what is its function?
|
Produced by adipocytes and muscle cells. Sits at luminal side of capillary. Releases Triglycerides from Chylomicrons -->remnant and VLDL--> IDL. The resulting monoglycerides and free fatty acids are used by the cells
|
|
|
Where does VLDL come from and what is its function.
|
Produced in Liver. Is composed of much triglycerides which can be released with Lipoprotein lipase to cells and thus forming IDL.
|
|
|
What happens to IDL after it is made (VLDL ---LPL---> IDL)?
|
Rapidly metabolized by liver OR converted to LDL via hepatic lipase
|
|
|
After LDL is made from IDL via hepatic lipase, what happens to it.
|
It is either metabolized by the liver or its cholesterol component is used by cells (esp. gonads and adrenals).
OR scavenger receptors in subendothelial spaces ---> athrosclerosis |
|
|
What is the function of HDL?
|
Transport of cholesterol from tissues to the liver
|
|
|
LDL, ILD and to a lesser extent VLDL are associated with atherosclerosis; which is associated with hypertriglyceridemia?
|
VLDL, this makes sense because VLDL is the main carrier of triglycerides from the liver to tissues.
|
|
|
Which Fredrickson phenotypes show high triglycerides?
|
1, 4 and 5
1- elevated chylomicrons 4- elevated VLDL 5- elevated chylomicrons and VLDL (1+4=5) |
|
|
Which Fredrickson phenotypes show elevated LDLs?
|
2a (common)
|
|
|
Which Fredrickson phenotypes show elevated "calculated" LDL and elevated triglycerides?
|
2b and 3, the triglyceride component of 2b is from elevated VLDL while the triglyceride component of 3 if from IDL
|
|
|
What does type 1 hypercholesterolemia look like in a test tube?
|
Elevated triglycerides (chylomicrons) so you get a water/oil layer with the chylos on top. (Very rare)
|
|
|
What does type 2a hypercholesterolemia look like in a test tube?
|
Clear
|
|
|
What does type 2b hypercholesterolemia look like in a test tube?
|
Has elevated LDL (calculated) and triglycerides(VLDL) thus ----> clear or cloudy
|
|
|
What does type 4 hypercholesterolemia look like in a test tube?
|
Elevated triglycerides (VLDL) so you get a turbid vile. (common)
|
|
|
What does type 5 hypercholesterolemia look like in a test tube?
|
Elevated triglycerides (chylomicrons and VLDL) so you get a turbid vile + an oil/water layer. (uncommon)
|
|
|
What does type 3 hypercholesterolemia look like in a test tube?
|
The elevated triglycerides are due to the presence of increased IDL --->Usually cloudy
|
|
|
What are the causes (3) for type 1 hyperlipidemia?
|
Increased chylomicrons---> LPL deficiency, LPL antibody (lupus), apo CII deficiency
-Both deficiencies are AR and rare |
|
|
What are the causes for type 2 (a and b) hyperlipidemia?
|
Familial -defective LDL receptor
Familial combined- too much apo B hypothyroidism --> regulator of LDL expression |
|
|
What should be the LDL levels in someone with hypothyroidism?
Graves? |
Increased LDL levels because the thyroid regulates production of the LDL receptor in the liver.
Graves= decreased |
|
|
What is the genetic defect in type 3 hyperlipidemia?
|
Homozygous Apo E2/E2
|
|
|
Which apo E is associated with alzheimer's disease?
|
Apo E4
|
|
|
What are some causes of type 4 hyperlipidemia?
|
Any disease with decreased insulin action such as... obesity, diabetes, beta blockers
|
|
|
What are some causes of type 5 hyperlipidemia?
|
Anybody with a combination of causes of type 1 + type 4 can progress to type 5
|
|
|
What is abetalipoproteinemia?
|
AR, deficient production of apo B. Everything except HDL have apo B, so all but HDL are markedly lowered. ---> fat malabsorption, acanthocytosis and neurologic abnormalities (b/c fat malabsorption).
|
|
|
How do you estimate VLDL?
|
Triglycerides/5, formula is valid up to 400
|
|
|
How do you calculate LDL?
|
=Total chosesterol - (HDL +VLDL)
or =Total cholesterol - (HDL + Triglyerides/5) |
|
|
Name an acute phase reactant that causes hypercoagulability?
|
Factor 8 and fibrinogen (also due to activation of platelets)
|
|
|
Manose binding lectin is an acute phase reactant; what is its function?
|
Part of immune system; binds/recognizes foreign bacterial particles and activates complement
|
|
|
Chronic inflammatory disease with cardiomyopathy, enlarged liver and tongue.
|
Serum amyloid A is an acute phase reactant that can cause amyloidosis in inflammatory diseases.
|
|
|
Name 4 proteins that decrease with stress (negative acute phase reactants)?
|
Retinol binding protein
Transthyretin (carrier of T4)(called pre-albumin due to its place on electrophoresis) Albumin Transferrin |
|
|
Why is electrophoresis done on serum and not plasma?
|
Fibrinogen (between beta and gamma) - can also show up in "serum" if line is anticoagulated -->fibrinogen present
|
|
|
How does immunoelectrophoresis work?
|
Antigen and antibody are place opposite each other and migrate toward each other forming a band
|
|
|
How do you interpret IEP (immunoelectrophoresis)?
|
Each antibody has a control (normal human serum, NHS) and the pt. sample. Look for symmetry. Peplaced by immunofixation electrophoresis (IFE)
|
|
|
What is found in the pre-albumin region on serum protein electrophoresis (SPE)?
|
Retinol-binding protein
Transthyretin - T4 transport -Both are negative acute phase reactants |
|
|
What is found in the alpha-1 region on serum protein electrophoresis (SPE)?
|
alpha-1 anti trypsin - protease inhibitor
HDL, Thyroxin binding globulin- T4/T3 transcortin- AKA cortisol binding glob. prothrombin- clotting (plasma only) |
|
|
What is found in the alpha-2 region on SPE?
|
Alpha-2 macro globulin- protease inhibitor
haptoglobin- hgb transport after hemolysis ceruloplasmin- redox, contains CU ion |
|
|
What is found in the beta region on SPE?
|
transferrin- Fe3+ transport
hemopexin- hgb transport after haptoglobin is used up LDL, C3, IgA, fibrinogen (plasma) |
|
|
Name 2 major causes of hyperproteinemia on SPE that are non-pathologic.
|
Dehydration
Prolonged tourniquet time |
|
|
Which is normally higher, hydrostatic or oncotic pressure?
|
Hydrostatic- thus our lymphatic work
|
|
|
What is the result of A-1-antitrypsin disease on the lung? Liver?
|
Emphasema
Cirrhosis |
|
|
What proteins go down in nephrosis?
what ones go up? |
gamma globulin (Ig gamma) and albumin
Alpha-2 macroglobulin |
|
|
Nephrosis will predispose to what type of infections, viral or bacterial?
|
Bacterial due to loss of gamma globulins
|
|
|
What is the effect in increased IgA levels on SPE?
|
Can cause beta-gamma bridging
|
|
|
What is the effect of lupus on an SPE?
|
Elevated beta region due to elevated C3 levels (also elevated in hep c)
|
|
|
What causes hyper-IgM syndrome?
|
Defect in CD40 ligand, B cells can't class switch
---> low IgG than also |
|
|
What is the function of alpha-1 antitrypsin?
Why does it cause emphysema? |
Anti protease
Lung lacks protection from the bodies own enzymes |
|
|
What are the normal and defective alleles in alpha-1 antitrypsin disease?
|
M: Normal
Z: Defective MZ= asymptomatic, a-1-at ~60% of nomral ZZ= severe |
|
|
What does nephrotic syndrome classically look like on SPE?
|
A2 increase, Decreased albumin, decreased gamma
|
|
|
What does cirrhosis classically look like on SPE?
|
Increased beta, gamma or both
Decreased Alb, A1, A2 |
|
|
What does acute inflammation classically look like on SPE?
|
A1 or A1 and A2 increased, decreased alb
Protein synthesis shifted from albumin to acute phase reactants |
|
|
What does Chronic inflammation classically look like on SPE?
|
A1, A2, B, and Gamma increased
Decreased albumin |
|
|
What does parametric distribution mean?
|
Distributed in a bell curve/Gaussian distribution
|
|
|
What is coefficient of variation?
|
CV = SD/mean --> expressed as a percent
|
|
|
What is the equation for standard deviation?
|
Difference in all values from the mean squared and added together divided by N-1
Square root of that. |
|
|
What is the advantage of CV vs. SD?
|
CV is unitless, thus you can compare different assay regardless of units.
|
|
|
What N is generally considered adequate to establish a reference interval?
|
100-120
|
|
|
What is partitioning?
|
A reference interval for a specific population. Still need 100-120 people for each of these populations to be acceptable. Eg. TSH in 1st trimester
|
|
|
How do you establish the "abnormal" cutoffs in a non-parametric population?
|
Take the highest and lowest 2.5% of participants in your study and establish that as the cutoff.
|
|
|
How do you compare 2 populations, taking the same test, to see if the groups are different? eg.
100 people with disease ---> 80+ 100 people w/o diesease ---> 10+ |
Chi-square --> do not have to calculate on boards, just know concept
Result--> P value |
|
|
Define P value
|
Probability that the null hypothesis is true. 0.05 = 5% chance that the null hypothesis is true
|
|
|
What is a Fischer test?
|
When the False positives or false negative groups are < 5. This data would not be eligible to be compared with a chi-square test
|
|
|
What is the difference between a paired vs. unpaired t-test
|
Paired uses the same subjects for both tests.
Unpaired uses experimental vs. control group. |
|
|
The same analyte is run on 2 different analyzers; what statistical test is run to determine which is more precise?
|
F-test
|
|
|
What is sensitivity?
|
True positives/ disease
likelihood that a test will be positive a a diseased individual |
|
|
What is specificity
|
True negatives/No disease
Likelihood that a test will be negative in a healthy population |
|
|
What is accuracy?
AKA? |
AKA efficiency
True positive + True negatives/all results |
|
|
What is a receiver-operator characteristic curve?
|
Sen plotted with 1-Sp. The greater the area under the curve, the better the test.
|
|
|
Other than paired-t-test, what is another way to compare two analyzers with the same specimen?
|
Correlation analysis --> correlation coefficient
|
|
|
What is the difference between standard regression analysis and Deming regression analysis when assessing correlation?
|
Standard assuming that only the result has variation. Deming regression assumes that error is found in the X and the Y.
|
|
|
What does each contain?
Red top tube, Green, Gray, Purple, Blue? |
Red- Serum
Green - Plasma with heparin Gray- Plasma with k+ oxalate Purple- EDTA (heme) Blue- 3.2% Na+ citrate (coag) |
|
|
What is the difference between trough and peak.
|
Trough- measure right before administration
Peak- measure shortly after administration (gentimicin) |
|
|
What is Bias?
proportional bias? constant bias? |
The difference between the result and the "true" concentration.
-Y changes by a % with X (m) -Y is a fixed amount different than X (b) |
|
|
What is the difference between a waived and moderate complexity test in the setting of a place that provides both?
|
Moderate complexity tests require proficiency testing.
|
|
|
What are the Westgard rules?
|
1 >3SD
2 sequential >2SD Range of sequential > 4SD 4 sequential > 1SD 10 sequential on one side of mean |
|
|
What are the 2 phases of aspirin toxicity?
|
Respiratory alkylosis
Metabolic acidosis |
|
|
What are the 3 current criteria for identifying type 2 diabetes?
|
Fasting glucose >126
Random or 2h glucose >200 Hb A1c >6.5 |
|
|
What are the criteria to identify pre-diabetes?
|
Fasting glucose >100
2h glucose > 140 Hb A1c > 5.7 |
|
|
What HLA markers are associated with type 1 diabetes?
|
HLA DR3 and DR4
DQB1 |
|
|
What DQ allele is associated with type 1 diabetes?
Protective? |
B1- 0201 and B1-0302
B1-0602 |
|
|
Fasting plasma glucose of 110, oral glucose tolerance test or >200.
How is this classified? |
Hyperglycemia.
In the absence of DKA, diabetes is only diagnosed if these symptoms are present on two occasions. One is pre |
|
|
What is the fructosamine assay?
|
Measure of glycosylated albumin. Better in pregnancy because changes faster so can be measured every few weeks.
|
|
|
How does glomerular disease manifest itself on Urine protein electrophoresis?
|
Albumin and transferrin (Beta peak) in urine
With increased damage --> A1 and gamma globulins |
|
|
How does tubular damage manifest itself on urine protein electrophoresis?
|
Albumin and A2 x2
|
|
|
If the urine sodium to plasma sodium ratio is greater than the urine creatinine to serum creatinine ratio, what does this mean?
|
likely acute tubular necrosis
|
|
|
What method is used to measure protein on urine analysis?
Glucose? |
Tetrabromphenol blue
Glucose oxidase -- Falsely low with ascorbic acid |
|
|
What method is used to measure blood on urine analysis?
Ketones? |
Peroxidase
Nitroprusside |
|
|
Ascorbic acid interferes with detection of what 2 measurements on urine analysis?
|
Glucose (glucose oxidase)
Blood (peroxidase) |
|
|
What are 2 drugs that cause red urine?
|
Pyridium and phenolphthalein
|
|
|
What are 3 things that can cause orange colored urine?
|
Rifampin
bilirubin pyridinium |
|
|
What disease causes black urine?
|
Alkaptonuria -tyrosine and phenylalanine
|
|
|
How is specific gravity calculated?
|
Weight of urine/ equal volume of water
N= 1.002-1.030 0.2% -- 3% heavier than water |
|
|
At what glucose level do you start seeing glucosuria?
|
>150
|
|
|
According to CLIA/CAP, generally how long must documentation of individual tests be storred (QC, reports, proficiency testing)?
|
2 years
|
|
|
How long must a specimen be saved, according to CAP, after it is analyzed?
|
24 hours
|
|
|
NADPH is the final product in many chemistry reactions; what is its wavelength?
|
340 nm
-likely the most important wavelength to know |
|
|
Does a slight increase in troponin levels have clinical significance in unstable angina or renal disease?
|
Both can cause elevations of troponins. In both diseases, the elevations are associated with worse outcomes.
|
|
|
Beyond as a marker of acute phase inflammation, what is the value of CRP as a risk factor?
|
Slight elevations are associated with increase risk for CAD
|
|
|
What is the formula for estimating true calcium levels with a low albumin?
|
Ca + (4.5 - albumin)*.8 = corrected
(Add 0.8 * grams/dL under 4.5) |
|
|
What two ions are mainly affected by hyperglycemia?
|
Causes hyponatremia (1.6 per 100 increased) and Hyperkalemia.
|
|
|
How is fractional excretion of sodium calculated?
|
FE= (Urinary Na+/ plasma sodium)/ urinary creatinine/plasma creatinine
|
|
|
How can fractional excreation of sodium be used to distinguish prerenal azotemia from acute tubular necrosis?
|
Prerenal azotemia FE= <1%
ATN FE>2% |
|
|
What is the value of Fractional excretion of urea vs. FE sodium?
|
FE urea < 35 is a better test for prerenal azotemia when the patient has been on diuretics
|
|
|
What is the effect of decreased magnesium levels on serum potassium?
|
Decreased levels due to increased loss in kidney
Calcium is also decreased. |

