![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
107 Cards in this Set
- Front
- Back
|
Human skeleton
|
-Initially just cartilage, replaced by bone, except areas of flexibility.
-Skeletal Cartilage- resilient, molded cartilage tissue, primarily made of water. No blood vessels /nerves |
|
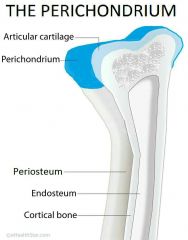
Perichondrium |
-Dense Irregular C.T around cartilage, like girdle -resists outward expansion - blood vessels nourish cartilage |
|
|
Bone tissue components (Cartilage) |
-All bones have the same basic components. -Cartilage made of chondrocytes, cells encased in small cavities -> lacunae, within extracellular matrix 3 Types: Hyaline, Elastic & Fibrocartilage |
|
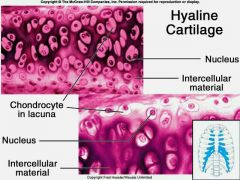
Hyaline |
- support/flexibility - Most abundant type; contains collagen fibers only. - joints, ribs, larynx, nose tip |
|
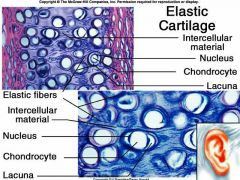
Elastic |
-Flexibility - contains elastic fibers -External ear, Epiglottis |
|

Fibrocartilage |
-compressible, high tensile strength -Intermediate between hyaline & elastic -rows of chondrocytes alternating w/ thick collagen fiber -Menisci of knee, intervertebral disc |
|

Growth of Cartilage 1. Appositional Growth |
-Growth from outside -Cartilage forming cells in perichondrium secrete matrix onto external face of existing cartilage |
|

2. Interstitial Growth |
-Growth from inside -Chondrocytes within lacunae divide and secrete new matrix, expanding from within |
|
|
Calcification of cartilage |
-Occurs in normal youth bone growth, also old age.
-Hardened cartilage is not the same as bone |
|
|
Functions of Bones
|
-Support & Protection -Movement -Mineral & Triglyceride (fat) storage -Blood Cell & Hormone production |
|
|
|
Axial- Skull & Torso bones Appendicular- Limb bones & girdles |
|

Long Bones |
-Longer than wide, shaft & 2 ends (Limb Bones) |
|

Short Bones |
-Cube shaped bones (Wrist & Ankle) |
|
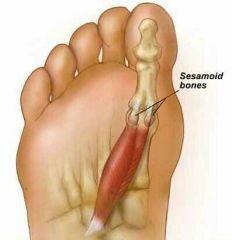
Sesamoid Bones |
-Form within tendons, shaped like seeds (vary in size & #) -Patella (Largest sesamoid bone) |
|
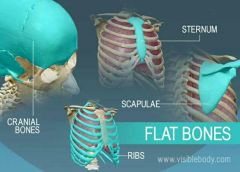
Flat Bones |
-Thin, flattened, usually curved (sternum, scapula, ribs, most skull bones) |
|
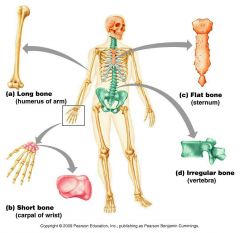
Irregular Bones |
-Complicated shapes (don't fit other classes) -Vertebrae & Hips |
|
|
Bones are Organs
|
-Mostly osseous tissue, also has nervous tissue, cartilage, fibrous C.T, muscle cells & epithelial cells in blood vessels 3 Levels of Bone Structure: Gross, Microscopic & Chemical
|
|
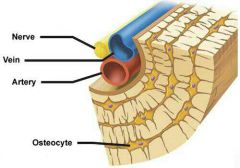
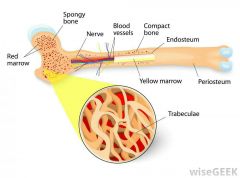
Gross Anatomy -Compact Bone |
Looks solid, but riddled w/ passageways for nerves, blood vessels & lymphatic vessels |
|
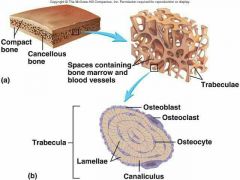
-Spongy Bone (Trabecular bone)
|
honeycomb of small, needle-like pieces of bone called Trabeculae (open spaces filled with red/yellow marrow)
|
|

Structure of short, irregular and flat bones |
-Thin spongy bone plates (diploe) covered by compact bone -Compact bone covered w/ CT membranes -Bone marrow throughout spongy bone -Hyaline cartilage covers bone of movable joint |
|
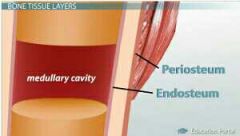
Endosteum |
Endosteum: Covers inside of compact bone |
|

Structure of Typical Long Bone |
Long Bones: shaft (diaphysis), bone ends (epiphyses), and membranes. |
|
|
Diaphysis |
Tubular shaft forms long axis of bone Compact bone surrounds Medullary Cavity (filled with yellow marrow-adults) |
|
|
Epiphyses |
End of long bones -> compact bone outside, spongy bone inside -articular cartilage covers joint surface |
|
|
Epiphyseal Line |
Between Diaphysis and Epiphyses -Remnant of childhood Epiphyseal Plate where bone growth occurs |
|

Membranes -Periosteum |
2 Layer Membrane covers external bone (except joints) -nerve fibers & blood vessels provide shaft w/ nutrients via foramen openings. -Anchoring points for tendons/ligaments. |
|
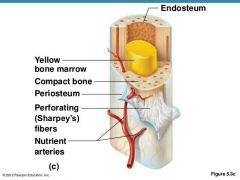
Fibrous layer |
Fibrous Layer: Outer layer of Dense Irregular tissue, consisting of Sharpey's fibers that secure to bone matrix. |
|
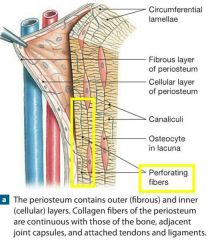
Osteogenic layer
|
Osteogenic Layer: Inner layer abutting bone, contains osteogenic stem cells, gives rise to almost all bone cells.
|
|

Endosteum |
Endosteum: -C.T membrane covering internal bone -Covers trabeculae -Line canals of compact bone. -Contains osteogenic cells , can change into other bone cells.
|
|
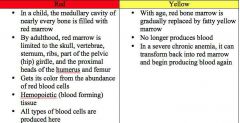
Hematopoietic Tissue in Bones -Red Marrow -Yellow Marrow |
In trabecular cavities of spongy bone -Newborns, medullary cavities & spongy bone contain red marrow Yellow marrow found in middle of long bones. - made of fat cells, body’s natural energy & blood reserve. -Adults, red in heads of femur/humerus, flat bone diploe, hips -Yellow can convert to red, in anemic people
|
|
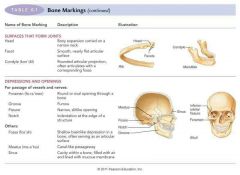
Bone Marking |
-Site of muscle, ligament & tendon attachment -involved in joint formation/conduits for blood vessels & nerves.
|
|

Three types of bone making: 1. Projection |
Outward bulge of bone -Due to increased stress from muscle pull or modification for joints. |
|

2. Depression |
Groove shaped cut-out that can serve as passageway for vessels & nerves, or joint attachment
|
|
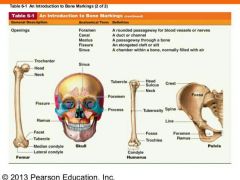
3. Opening
|
Hole / Canal, serves as passageway for blood vessels/nerves.
|
|
|
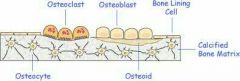
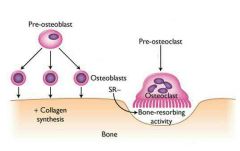
Bone Cell Types |
Five majors cell types 1. Osteogenic cells 2. Osteoblasts 3. Osteocytes 4. Bone-lining cells 5. Osteoclasts |
|
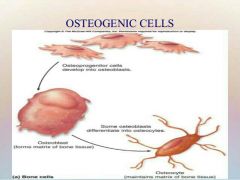
1. Osteogenic Cells |
Osteogenic: - Stem Cell (AKA Osteoprogenitor cell) -Mitotically active in periosteum & endosteum. -can differentiate into osteoblast/bone-lining cells |
|
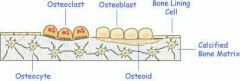
2. Osteoblasts |
Osteoblast: Secretes Matrix (Osteoid), bone growth cell (can divide) -Osteoid: collagen & calcium-binding proteins |
|
3. Osteocytes |
Osteocyte: Mature cell (in lacunae) no longer divide, maintains bone matrix (senses stress/strain)
|
|
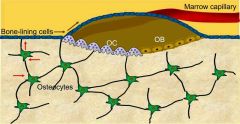
4. Bone-Lining Cell |
Bone-Lining Cell: -Flat cells on bone surface, help maintain matrix External-Periosteal, Internal-Endosteal |
|
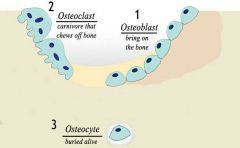
5. Osteoclast
|
Osteoclast: Bone breaking-down & reforming cell
|
|
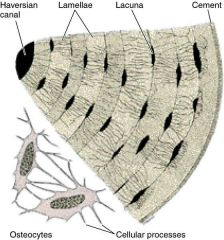
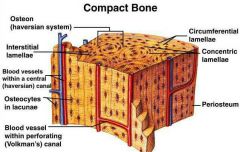
Compact Bone (lamellar bone) |
-Osteon -Canals & canaliculi. -Interstitial & circumferential lamellae. |
|

-Osteon (Harversian System) |
-Structural unit of bone, weight-bearing pillars -Osteon cylinder -> rings of bone matrix called Lamellae (like tree rings)
|
|
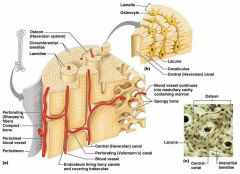
-Lamellae |
Lamellae: -Contain collagen fibers (bone salts between) that run in different directions in adjacent rings -Resists stress/twists |
|

-Interstitial Lamellae |
Interstitial Lamellae: -Lamellae not part of Osteon -Fills gaps between forming Osteons, remnant of bone remodeling |
|
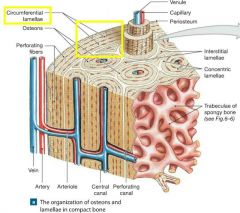
-Circumferential Lamellae |
Circumferential Lamellae: -Between Periosteum & Endosteum -Lamellae layer around surface of diaphysis (resist twisting) |
|
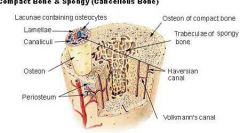
-Cental (Haversian) Canal |
Central (Haversian) Canal: -Runs through core of Osteon (holds blood vessels & nerves) |
|

-Perforating (Volkmann's) Canals |
Volkmann's Canals: -Endosteum-lined canals running horizontally -Connects blood vessels & nerves of periosteum, medullary cavity, and cental canal |
|
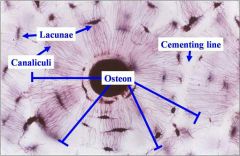
Lacunae (Osteocytes) |
Lacunae: Small cavities that contain Osteocytes |
|
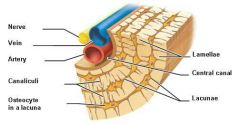
Canaliculi |
Canaliculi: Hairlike canals connect lacunae to each other & central canal |
|
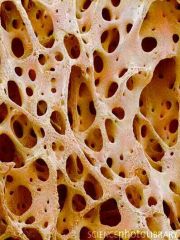
Spongy Bone |
Spongy Bone: -Appears poorly organized, but actually organized along lines of stress to resist stresses |
|
Trabeculae |
Trabeculae: -Suspension-like cables give bone strength -No osteons, contain irregularly arranged lamellae & osteocytes interconnected by canaliculi. -Capillaries in endosteum supply nutrients |
|
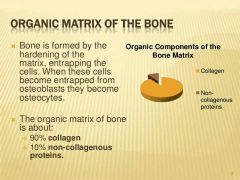
Organic Bone Components |
-Bone Tissue Cells & Osteoid. -Resilience from sacrificial cells -> stretch/break to dissipate energy & prevent fractures (bonds reform) |
|
Osteoid |
Osteoid: -1/3 of organic bone matrix -ground substances and collagen fibers = high tensile strength /flexibility 1. Proteoglycans 2. Glycoproteins
|
|

Inorganic Bone Components: Hydroxylapatities(Minerals salts) |
Hydroxylapatites: - 65% of bone tissue -calcium phosphate crystals in/around collagen fibers, decompose slowly (hardness & compression resistance) |
|
Ossification (osteogenesis) |
Ossification (osteogenesis): -Bone tissue formation (2nd month of fetus) -Postnatal growth until early adulthood. -Bone remodeling/repair = lifelong |
|

Formation of the Bony Skeleton |
Week 8 -> fibrous membranes/hyaline cartilage of fetal skeleton replaced with bone tissue
|
|
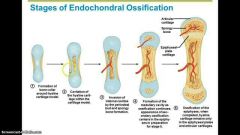
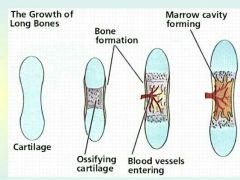
Endochondral Ossification |
Endochondral Ossification: -Forms all bones below skull (not clavicle) -Developed by replacing hyaline cartilage (2nd month of development) |
|
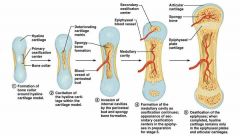
Primary Ossification Center |
Primary Ossification Center: -Center of hyaline cartilage shaft -> endochondral ossification occurs -Blood vessels infiltrate perichondrium, converting it to periosteum -Mesenchymal cells become osteoblasts |
|
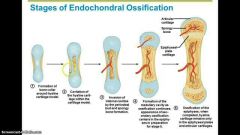
5 Stage process for Endochondral Ossification |
1. Bone collar forms around Diaphysis 2. Central cartilage calcifies, develops cavities 3. Periosteal Bud (vessels, nerves, red marrow, osteogenic & osteoblast cells) invades cavities, forms spongy bone. 4.Diaphysis elongates, Medullary cavity forms. ((Secondary Ossification Centers appear in epiphyses)) 5.Epiphyses ossify-Hyaline cartilage remains only in epiphyseal plates/articular cartilages |
|

Intramembranous Ossification |
Intramembranous Ossification: -Fibrous C.T membrane formed by mesenchymal cells -Forms skull bones ( frontal, parietal, occipital, temporal) & clavicles |
|
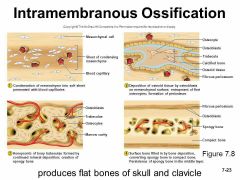
4 Major Steps for Intramembranous Ossification |
1.Ossification Center appears in fibrous C.T 2.Bone matrix (Osteoid) secreted in fibrous membrane -> calcifies 3.Woven bone & Periosteum form 4.Lamellar bone replaces woven bone beneath Periosteum. Red marrow appears. |
|

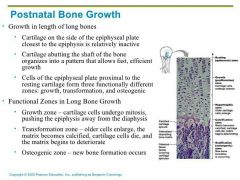
Postnatal Bone Growth |
Postnatal Bone Growth: -Long bones grow lengthwise by interstitial/longitudinal growth of epiphyseal plate -Bones increase thickness through appositional growth. -Bones stop growing during adolescence -Some facial bones continue to grow |
|

Growth in Length of Long Bones
|
-Interstitial growth requires epiphyseal cartilage in the epiphyseal plate -Epypheseal plate maintains constant thickness -Rate of cartillage growth on one side balanced by bone replacement on other
|
|
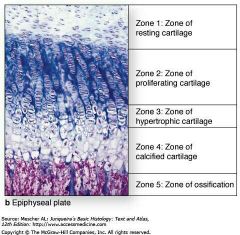
Epiphyseal Plate Consist of Five Zones |
1. Resting (quiescent) zone-Inactive Cartilage on epiphyseal side of epiphyseal plate 2. Proliferation (growth) zone- Rapidly dividing cartilage on diaphysis side of epiphyseal plate - New cells move upward, pushing epiphysis away from diaphysis = lengthening 3. Hypertrophic zone- Old chondrocytes closer to diaphysis have lacunae enlarge/ erode, interconnecting spaces form 4. Calcification zone-Cartilage matrix calcifies; chondrocytes die/deteriorate. 5. Ossification (osteogenic) zone- new bone forms |
|

End of Adolescence |
End of Adolescence: -Chondroblast divide less -Epiphyseal plate thins, replaced w/ bone, closes -> epiphysis & diaphysis fuse -Bone lengthening stops (females18, males21) |
|
Growth in Width (Thickness) |
-Bones widen through appositional growth (response to increase stress/weight/activity) -more build than break, forming thicker bones |
|
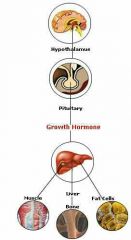
Hormonal Regulation of Bone Growth: |
-Stimulates epiphyseal plate activity in infancy/childhood (anterior pituitary gland) -Thyroid Hormone: Modulates activity/proportions of growth hormones -Testoterone/Estrogen at Puberty: -Promote adolescent growth spurts -Epiphyseal plate closure ends growth Abnormal skeletal growth: caused by excesses/deficits of any hormone |
|

Bone Remodeling |
-Bone Deposit/Resorption on surface of periosteum & endosteum -5-7% bone mass recycled each week, Spongy-replaced 3-4 yrs, Compact replaced 10 yrs. -Remodeling Unit: Osteoblast/Osteoclast packets |
|

Bone Deposits |
-New bone matrix deposited by osteoblasts -deposit triggered by: mechanical signals, increased calcium/phosphate concentration (hydroxylapatites, matrix proteins), algalune phosphatase enzyme for mineralization |
|

Osteoid Seam & Calcification Front
|
Osteoid Seam: Band of unmineralized bone matrix = new matrix Calcification Front: Transtion zone between osteoid seam & old mineralized bone
|
|
Bone Resorption |
Osteoclast function: -Secrete lysosomal enzymes & protons (H+) that digest & phagocytize matrix -Osteoclasts activation involves PTH (parathyoid hormone) and immune T cell proteins -regulated by hormones & mechanical stress response |
|

1. Hormonal Control -Parathyroid Hormone (PTH) |
PTH: Low calcium level response by parathyroid gland -Stimulates osteoclasts to resorb bone, release calcium back to blood, controlled by homeostatic calcium levels. |
|
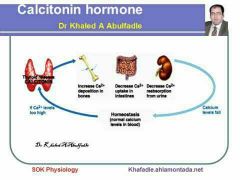
-Calcitonin
|
High calcium blood levels = Calcitonin release by parafollicular cells of thyroid gland -Causes bones to store calcium |
|
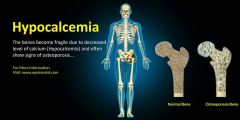
Hypocalcemia
|
Low levels of calcium cause hyperexcitablility, spasms |
|

Hypercalcemia |
High levels of calcium cause nonresponsiveness. Sustained High Blood Calcium Levels:
|
|
|
Serotonin & Leptin |
Leptin: Adipose tissue hormone, regulates bone density, inhibits osteoblasts Serotonin: -Neurotransmitter (made in gut after meal = eating regulates calcium stores) regulates mood & sleep, inhibits osteoblasts |
|
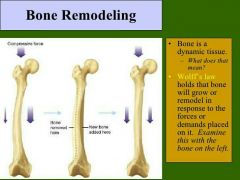
Wolf's law states |
Bones grow/remodel in response to demands, (stress bends & stretches bones, thickest where stress greatest) -Bone can be hollow because compression and tension cancel each other out in center of bone |
|
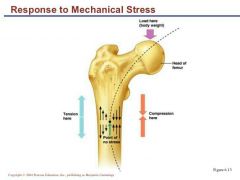
Wolf's law also explains: |
-Handedness= thicker/stronger bone in that limb -Curved bones thickest where most likely to buckle -Trabeculae form trusses along lines of stress. Large, bony projections= heavy, active muscle attach |
|

Cont. of control remodeling |
Remodeling control: -Mechanical stress -> remodeling w/ electric signals where deformations occur - Hormonal Control= If & When - Mechanical Stress= Where |
|
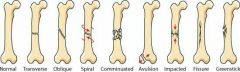
Fractures |
-Fractures = breaks -youth = physical trauma, old = bone thinning |
|
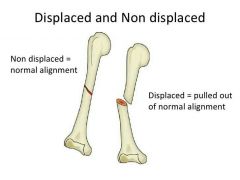
Three Fractures Classification: 1. Position of bone ends after fracture: |
-Nondisplaced: Ends retain normal position -Displaced: Ends are out of normal alignment |
|
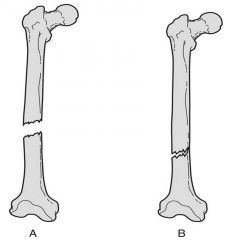
2. Completeness of break:
|
-Complete: Broken all the way through. -Incomplete: Not broken all the way through.
|
|
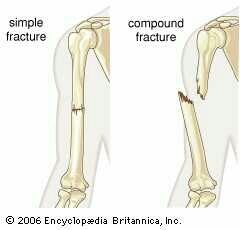
3. Whether skin is penetrated: |
-Open (compound): Skin is penetrated. -Closed (simple): Skin is not penetrated.
|
|
|
Fracture Tratment and repair
|
Treatment = reduction, realignment of broken ends -Closed reduction: physician manipulates to correct position -Open reduction: surgical pins or wires secure ends.
|
|

Immobilization
|
Bone immobilized by cast to heal -Time needed for repair depends on break severity, bone broken, and age of patient. |
|

Repair Involves four major stages
|
Fracture Repair: -Hematoma formation -Fibrocartilaginous callus formation -Bony callus formation -Bone remodeling |
|

1.Hematoma Formation:
|
-Torn blood vessels hemorrhage, forming mass of clotted blood called a Hematoma. -Site is swollen, painful, and inflamed.
|
|
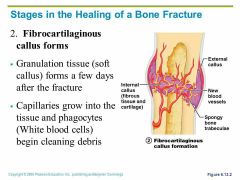
2.Fibrocartilaginous Callus formation |
|
|

3.Bony callus Formation |
|
|
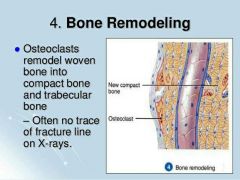
4. Bone Remodeling |
|
|
|
Bone Disorders
|
bone deposit/resorption imbalances -Osteomalacia and rickets -Osteoporosis -Paget's disease |
|

Osteomalacia |
-Bones are poorly mineralized -Osteoid is produced, but calcium salts not adequately deposited. -Result is soft, weak bones. -Pain upon bearing weight. |
|
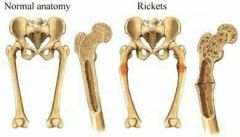
Rickets (Osteomalacia of children) |
-Results in bowed legs and other bone deformities because bones ends are enlarged and abnormally long. -Cause: Vitamin D deficiency or insufficient dietary calcium. |
|
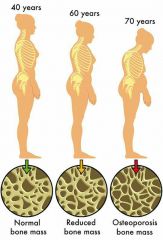
Osteoporosis |
-Is a group of diseases in which bone resorption exceeds deposits. -Matrix remains normal, but bone mass declines. -Spongy bone of spine and neck of femur most susceptible. (Vertebral and hip fractures common) |
|
|
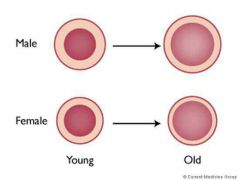
Osteoporosis risk factors |
-Most often aged, postmenopausal women. (Estrogen plays a role in bone density, so when levels drop at menopause, women run higher risk) - Men are less prone due to protection by the effects of testosterone. -Petite body form -Diet poor in calcium and protein. -Smoking -Insuficiente exercise to stress bone, |
|
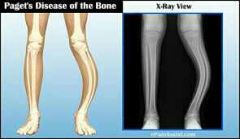
Paget's Disease (pagetic bone) |
-Excessive and haphazard bone deposits and resorption cause bone to be made fast and poorly. -Very high ratio of spongy to compact bone and reduced mineralization. -Usually occurs in spine, pelvis, fémur, and skull -Rarely occurs before age 40. -Treatment includes calcitonin and bisphosphonates. |
|
|
Developmental Aspects of Bone |
-Embryonic skeleton ossifies predictably, so fetal age is easily determined from X rays or sonograms. -most long bones begin ossifying by 8 weeks, with primary ossification centers developed by week 12 |
|
|
Developmental Aspects of Bone |
-Embryonic skeleton ossifies predictably, so fetal age is easily determined from X rays or sonograms. -Most long bones begin ossifying by 8 weeks, with primary ossification centers developed by week 12 |
|
|
Birth to Young Adulthood |
-At birth, most long bones ossified, except at epiphyses. -Epiphyseal plates persist through childhood and adolescence. -At ~ age 25, all bones are completely ossified, and skeletal growth ceases. |
|

Age-Related Changes in Bone |
-In children and adolescents, bones formation exceeds resorption. (Males tend to have greater mass than females) -In young adults, both are balanced. -In adults, bones resorption exceeds formation. |
|
Aged- Related Changes in Bone |
-Bone density changes over lifetime are largely determined by genetics. *Gene for vitamin D's cellular docking determines mass early in life and osteoporosis risk at old age. -Bone mass, mineralization, and healing ability decrease with age beginning in fourth decade. *Except bones of skull. *Bone loss is greater in whites and females. |
|
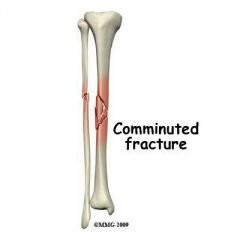
Fracture Types of Bones : 1. Comminuted |
-Bone fragments into three or more pieces. -Particularly common in the aged, whose bones are more brittle. |
|
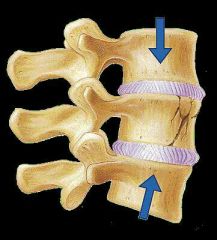
2. Compression |
-Bone is crushed. -Common in porous bones (i.e, osteoporotic bones) subjected to extreme trauma, as a fall. (Crushed vertebrae) |
|
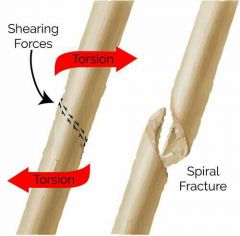
3. Spiral |
-Ragged break occurs when excessive twisting forces are applied to a bone. -Common sports fracture. |
|
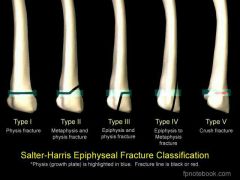
4. Epiphyseal |
-Epiphyseal separates from the diaphysis along the Epiphyseal plate. -Tends to occur where cartilage cells are dying and calcification of the matrix is occurring. |
|

5. Depressed |
-Broken bone portion is pressed inward. -Typical of skull fracture. |
|

6. Greenstick |
-Bone breaks incompletely, much in the way a green twig breaks. Only one side of the shaft breaks; the other side bends. -Common in children, whose bones have relatively more organic matrix and more flexible than those of adults. |

