![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
64 Cards in this Set
- Front
- Back
|
What is the negative predictive value of a negative knee MRI?
|
MR has a very high negative predictive value; therefore, a normal MR knee examination is highly accurate in excluding an internal derangement
|
|
|
How is the knee positioned in the scanner?
|
The knee should be imaged using a dedicated knee coil and externally rotated about 5° to 10° (should not exceed 10°) to put the anterior cruciate ligament in the plane of imaging.
|
|
|
What do normal menisci look like?
|
-The normal meniscus is a fibrocartilaginous, C-shaped structure that is uniformly low in signal on both T1WIs and T2WIs.
-Many centers have found that the menisci are more easily examined if they fat-suppress the T1 or proton-density sequences. -With T2* sequences, the menisci will usually demonstrate some internal signal. -With T1WIs, any signal within the meniscus is abnormal, except in children, in whom some signal is normal and represents normal vascularity. |
|
|
What is meniscal degeneration? What does it look like on MR?
|
-Meniscal signal that does not disrupt an articular surface is representative of intrasubstance degeneration, which is myxoid degeneration of the fibrocartilage.
-It most likely represents aging and normal wear and tear. -It is not thought to be symptomatic and cannot be diagnosed clinically or with arthroscopy. -Some choose, therefore, not to mention intrasubstance degeneration in the radiology interpretation. |
|
|
Describe the grading system for abnormal meniscal signal:
|
A grading scale for meniscal signal that is widely used is the following:
-Grade 1, rounded or amorphous signal that does not disrupt an articular surface -Grade 2, linear signal that does not disrupt an articular surface -Grade 3, rounded or linear signal that disrupts an articular surface. -Grades 1 and 2 are intrasubstance degeneration and should not be reported as “grade 1 or 2 tears,” since the term “tear” can lead to unnecessary arthroscopy (arthroscopy is not indicated for intrasubstance degeneration). -Grade 3 is a meniscal tear. |
|
|
What do you need to see to call a meniscal tear?
|
-When high signal in a meniscus disrupts the superior or inferior articular surface, a meniscal tear is diagnosed
-In a small but significant percentage of cases, it can be virtually impossible to be certain whether meniscal high signal disrupts an articular surface. -In these cases it is recommended that the surgeon be advised that it is too close to call. -The surgeon can then rely on his or her clinical expertise to decide if arthroscopy is warranted, and if it is, the MR will guide the surgeon to the location of the questionable tear. -If these equivocal cases are excluded, the remaining cases will have an extremely high accuracy rate. |
|
|
In which setting does the sensitivity for detecting meniscal tears decrease?
|
-It has been shown that MR imaging sensitivity for meniscal tears decreases significantly when the anterior cruciate ligament (ACL) is torn.
-These frequently overlooked tears occur in the periphery of the meniscus and in the posterior horn of the lateral meniscus. -Hence, great care must be used in examining these areas of the menisci in patients with ACL tears. |
|
|
What is the most common configuration for a meniscal tear?
|
Meniscal tears have many different configurations and locations; an oblique tear extending to the inferior surface of the posterior horn of the medial meniscus is the most common type.
|
|
|
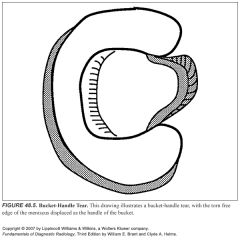
Describe a bucket handle meniscal tear: What does it look like on MR?
|
-This is a vertical longitudinal tear that can result in the inner free edge of the meniscus becoming displaced into the intercondylar notch.
-It is most easily recognized by observing on the sagittal images that only one image is present that has the bow-tie appearance of the body segment of the meniscus. -Normally, two contiguous sagittal images with a bow-tie shape are seen, because the normal meniscus is 9 to 12 mm wide and the sagittal images are 4 to 5 mm in thickness. -On the coronal images, a bucket-handle tear may reveal the meniscus to be shortened and truncated; however, the torn meniscus often remodels and truncation cannot be appreciated. -The displaced inner edge of the meniscus (the “handle” of the bucket) is often seen in the intercondylar notch on sagittal or coronal views -The handle of the bucket can form the "double PCL sign", so that it looks like two PCL's are present. |
|
|
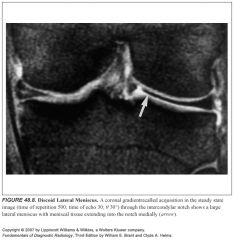
What is a discoid meniscus?
What is its significance? What does it look like on MR? |
-A discoid meniscus is thought to be more prone to tear than a normal meniscus, and it can be symptomatic even without being torn.
-A discoid meniscus is a large meniscus that can have many different shapes: lens-shaped, wedged, flat, and others. -Whether it is congenital or acquired is not known, but most are found in children and young adults. -It is seen laterally in up to 3% of the population, with a discoid medial meniscus being much less common. -Although they are easily identified on coronal images by noting extensions of meniscal tissue into the tibial spines at the intercondylar notch, they are most reliably diagnosed by noting more than two consecutive sagittal images that show the meniscus with a bow-tie appearance |
|
|
What is a meniscal cyst?
What is their significance? Which meniscus is more commonly affected? Why might you miss a meniscal cyst? |
-They are formed by insinuation of joint fluid through a meniscal tear into adjacent tissues.
-Almost always associated with a meniscal tear -A meniscal cyst will enlarge the meniscus and give it a swollen appearance unless it decompresses into the soft tissues (called a parameniscal cyst) or into the joint via a meniscal tear. -Most common in lateral meniscus -More common in discoid menisci -The intrameniscal portion of the cyst typically does not get as bright as fluid in signal on T2 sequences, which has misled many radiologists into discounting the presence of a cyst. |
|
|
Is a parameniscal cyst always associated with a meniscal tear?
|
No:
-Decompression of meniscal fluid into a parameniscal cyst does not always indicate a meniscal tear because a meniscal tear, by definition, has to disrupt the articular surface of the meniscus (not always present with a parameniscal cyst). |
|
|
What is the transverse ligament? What can it simulate?
|
-A ligament that connects the anterior horns of the medial and lateral menisci and runs through Hoffa's fat pad
-The lateral meniscus often has what appears to be a tear on the anterior horn near its upper margin, which is a pseudotear from the insertion of the transverse ligament. -This can easily be differentiated from a real tear by following it medially across the knee in Hoffa's fat-pad, where it inserts into the anterior horn of the medial meniscus. |
|
|
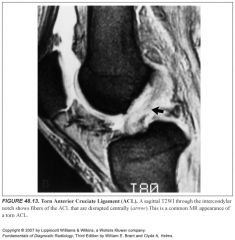
What does a normal ACL look like on MR?
What a torn ACL look like? What does an ACL sprain look like? |
-The normal ACL is seen in the intercondylar notch as a linear, predominantly low-signal structure on T1WIs; it often shows some linear striations near its insertion onto the medial tibial spine when viewed on sagittal images.
-When torn, the ACL is most often simply not visualized, although sometimes the actual disruption will be seen. -T2WIs are imperative for obtaining the highest accuracy in diagnosing ACL tears, because fluid and hemorrhage will often obscure the ligament on T1WIs. -Partial tears or sprains of the ACL are manifested by high signal within an otherwise intact ligament. -MR is highly accurate in diagnosing a torn ACL, with sensitivities reported in the literature approaching 100%. |
|
|
What does a torn PCL look like?
How is it managed? |
-It is infrequently torn and even less frequently repaired by surgeons.
-When torn, it takes on diffuse intermediate signal throughout -This increased signal usually does not get brighter with T2WIs and is therefore often overlooked. -Most orthopaedic surgeons do not even inspect the PCL at arthroscopy and do not repair it when torn, because it is rarely a cause of instability. |
|
|
What is a meniscofemoral ligament?
What does it simulate? |
-A low-signal, round structure that is often seen just anterior or posterior to the PCL, as seen in the sagittal views.
-A loose body or a free fragment of a piece of torn meniscus can have this appearance, but it is most commonly caused by a meniscofemoral ligament that extends obliquely across the knee from the medial femoral condyle to the posterior horn of the lateral meniscus. -If it passes in front of the PCL, it is called the ligament of Humphry, and if it passes behind the PCL, it is called the ligament of Wrisberg -Either one of these ligaments is present in up to 72% of all knees. -The insertion of the ligament of Humphry or Wrisberg onto the lateral meniscus can produce a pseudotear similar to that caused by the transverse ligament on the anterior horn of the lateral meniscus |
|
|
What are the ligaments of Humphrey and Wrisberg?
|
-Meniscofemoral ligaments that extend obliquely across the knee from the medial femoral condyle to the posterior horn of the lateral meniscus.
-If it passes in front of the PCL, it is called the ligament of Humphrey, and if it passes behind the PCL, it is called the ligament of Wrisberg -Either one of these ligaments is present in up to 72% of all knees. |
|
|
What should you stop and think about if you're about to call a tear in the superior aspect of the posterior horn of the lateral meniscus?
|
-The insertion of the ligament of Humphry or Wrisberg onto the lateral meniscus can produce a pseudotear similar to that caused by the transverse ligament on the anterior horn of the lateral meniscus.
-Prior to diagnosing a tear on the upper aspect of the posterior horn of the lateral meniscus, care must be taken to look for a meniscofemoral ligament to be certain it is not a pseudotear from the ligament's insertion. |
|
|
What should you stop and think about if you're about to call a tear in the anterior horn of the lateral meniscus?
|
-The lateral meniscus often has what appears to be a tear on the anterior horn near its upper margin, which is a pseudotear from the insertion of the transverse ligament.
-This can easily be differentiated from a real tear by following it medially across the knee in the Hoffa fat-pad, where it inserts into the anterior horn of the medial meniscus. |
|
|
What should you stop and think about if you're about to call a loose body near the PCL?
|
Prior to diagnosing a loose body in front of or behind the PCL, care must be taken to try to follow the structure across to the lateral meniscus to determine whether it is a meniscofemoral ligament.
|
|
|
Desribe the origin and insertion of the MCL:
|
-The medial collateral ligament (MCL) originates on the medial femoral condyle and inserts on the tibia.
-It is closely applied to the joint and is intimately associated with the medial joint capsule and the medial meniscus. |
|
|
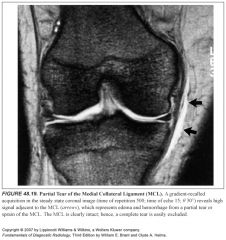
Describe the grading system of MCL tears:
|
-A grade 1 injury represents a mild sprain and is diagnosed on MR by the presence of fluid or hemorrhage in the soft tissues medial to the MCL.
-The ligament is otherwise normal. -A grade 2 injury is a partial tear and is seen as high signal in and around the MCL on T2 or T2* coronal sequences. -The ligament is intact, although the deep or superficial fibers may show minimal disruption -A grade 3 injury is a complete disruption of the MCL. -It is best appreciated on T2 or T2* images |
|
|
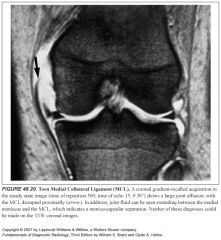
What is meniscocapsular separation?
Where does it usually occur? What does it look like on imaging? |
-A meniscocapsular separation occurs when the medial meniscus is torn from its attachment to the joint capsule.
-This occurs most commonly at the site of the MCL and often occurs concomitantly with an MCL injury. -It is easily recognized on a T2 or T2* coronal image by noting joint fluid extending between the medial meniscus and the capsule |
|
|
Describe the lateral collateral complex:
|
-The lateral collateral ligament (LCL) consists of three parts.
-The most posterior structure is the tendon of the biceps femoris, which inserts onto the head of the fibula. -Next, anterior to the biceps, is the true lateral collateral ligament, also called the fibular collateral ligament, which extends from the lateral femoral condyle to the head of the fibula. -The biceps and the fibular collateral ligament usually join and insert onto the head of the fibula in a conjoined fashion. -Anterior to the fibular collateral ligament is the iliotibial band, which extends into the fascia more anteriorly and blends into the lateral retinaculum on the patella. |
|
|
What forms the conjoined tendon?
|
-The biceps and the fibular collateral ligament (LCL) usually join and insert onto the head of the fibula in a conjoined fashion.
|
|
|
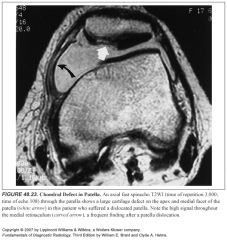
What is chondromalacia patellae?
What does it look like on imaging? What causes it? |
-The patellar cartilage commonly undergoes degeneration, causing exquisite pain and tenderness.
-This is called chondromalacia patella. -It can be diagnosed on sagittal images but is more easily identified on axial images. -Because hyaline articular cartilage has the same signal intensity as joint fluid on T1W sequences, T2 or T2* sequences are necessary to diagnose chondromalacia patella in most instances. -Chondromalacia patella begins with focal swelling and degeneration of the cartilage. -This can be seen as low- or high-signal foci in the cartilage. -Its progression causes thinning and irregularity of the articular surface of the cartilage; finally, underlying bone is exposed. -This final stage occurs more commonly from trauma than from wear and tear. -A frequent cause of a patellar cartilage defect is dislocation of the patella, in which the patella strikes the lateral femoral condyle and displaces a piece of patellar articular cartilage. -The lateral femoral condyle invariably has a contusion following a dislocated patella. |
|
|
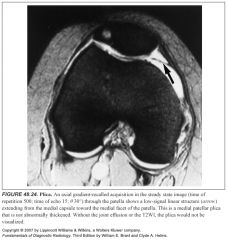
What is a patellar plica?
|
-A normal structure seen in over half of the population is the medial patellar plica.
-It is an embryologic remnant from when the knee was divided into three compartments. -It is a thin, fibrous band that extends from the medial capsule toward the medial facet of the patella -Suprapatellar and infrapatellar plicae also exist. -The medial patellar plica can, on rare occasions, thicken and cause clinical symptoms that are indistinguishable from those of a torn meniscus; this has been termed “plica syndrome.” -An abnormal plica can be removed arthroscopically quite easily. |
|
|
What is the thin fibrous band that extends from the medial capsule toward the medial facet of the patella?
|
Medial patellar plica
|
|
|
What is plica syndrome?
|
The medial patellar plica can, on rare occasions, thicken and cause clinical symptoms that are indistinguishable from those of a torn meniscus; this has been termed “plica syndrome.”
|
|
|
What is a bone contusion?
What does it look like on imaging? What is a potential complication? |
-A contusion represents microfractures from trauma.
-They are also called bone bruises. -They are easily identified on T1WIs as subarticular areas of inhomogeneous low signal. -With T2 weighting, a contusion will show increased signal for several weeks, depending on its severity -Contusions can progress to osteochondritis dissecans if they are not treated with decreased weight bearing; hence, an isolated bone contusion, with no other internal derangement, is a serious finding that requires protection. |
|
|
Which site of bony contusion is frequently associated with a torn ACL?
|
-A commonly seen contusion is one that occurs on the posterior part of the lateral tibial plateau
-It is invariably associated with a torn ACL. -Acute ACL tears have been reported to have this type of contusion in over 90% of cases |
|
|
What is a segond fracture?
What is it associated with? |
-A fracture that is almost always associated with an internal derangement is the Segond fracture.
-A small, bony fragment pulled off the posterior lateral tibial joint line by an avulsion of the lateral joint capsule, it is almost always associated with an ACL tear. |
|
|
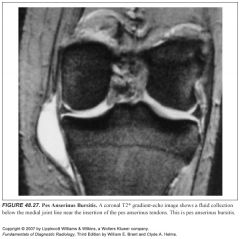
What structures make up the pes anserinus?
Where do they arise from and insert? Where is the pes anserinus bursa located? |
Three tendons—the sartorius, the gracilis, and the semitendinosus—insert onto the anteromedial aspect of the tibia in a fan-shaped manner that has been likened to a goose's foot, hence the name pes anserinus.
-A bursa lies beneath the insertion site, which can become inflamed and cause medial joint line or patellar pain; this can be confused with plica syndrome or a torn medial meniscus |
|
|
Name the two medial bursae of the knee?
|
-Pes anserinus bursa
-Semimembranosus tibial collateral ligament bursa |
|
|
Why is diagnosing medial bursitis particularly important?
|
Making the diagnosis of pes anserinus or semimembranosus tibial collateral ligament bursitis with MR imaging can prevent an unnecessary arthroscopy procedure—one in which the bursae would be overlooked, since they are extracapsular structures.
|
|
|
What does the semimembranosus tibial collateral ligament look like?
|
-It occurs at the medial joint line and often mimics a meniscal cyst.
-It has a characteristic comma shape as it drapes over the semimembranosus tendon |
|

|
1
|
|

|
2
|
|

|
3
|
|

|
4
|
|
|
5
|
|

|
6
|
|

|
7
|
|
|
8
|
|

|
9
|
|

|
10
|
|

|
11
|
|

|
12
|
|
|
13
|
|

|
14
|
|

|
15
|
|

|
16
|
|

|
17
|
|

|
18
|
|
|
19
|
|
|
20
|
|

|
21
|
|

|
22
|
|
|
23
|
|
|
24
|
|

|
25
|
|

|
26
|
|
|
27
|
|

|
28
|

