![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
|
What's the difference between osteoporosis and osteomalacia?
Can you tell the difference on plain films? |
-Osteoporosis is defined as diminished bone quantity in which the bone is otherwise normal.
-This contrasts to osteomalacia, in which the bone quantity is normal but the quality of the bone is abnormal in that it is not normally mineralized. -Osteomalacia results in excess nonmineralized osteoid. -It is not possible in most cases to distinguish between osteoporosis and osteomalacia on plain films; hence, many prefer the term “osteopenia” for the plain film finding of diminished mineralization. |
|
|
What are the different types of osteoporosis?
|
-There are myriad causes of osteoporosis, the most common of which is primary osteoporosis (so-called senile osteoporosis or osteoporosis of aging).
-This is seen most commonly in postmenopausal women and is a major health concern because of the increase in vertebral body and hip fractures in this patient population. -Secondary osteoporosis implies that an underlying disorder, such as thyrotoxicosis or renal disease, has caused the osteoporosis. -Only about 5% of osteoporosis cases are of the secondary type. -A type of osteoporosis that can be seen in a patient of any age is disuse osteoporosis. -It results from immobilization from any cause, most commonly following treatment of a fracture. -The radiographic appearance of disuse osteoporosis differs from that of primary osteoporosis in that it occurs somewhat more rapidly and gives the bone a patchy appearance -This is from osteoclastic resorption in the cortex, which causes intracortical holes. If the disuse were to continue, the bone would resemble any bone with marked osteoporosis, that is, severe cortical thinning. |
|
|
What are the radiographic findings in osteopenia? Where should you look for osteopenia?
|
-The main radiographic finding in osteoporosis is thinning of the cortex.
-Although this can be seen in any bone, it is most reliably demonstrated in the second metacarpal at the middiaphysis. -Normal metacarpal cortical thickening should be approximately one fourth to one third the thickness of the metacarpal. -In osteoporosis, this cortical thickness is decreased |
|
|
What does "aggressive osteoporosis" mean?
How can you tell the difference between a permeative lesion and a pseudopermeative lesion? Name some causes of pseudopermeative lesions: |
-Occasionally, aggressive osteoporosis from disuse can mimic a permeative lesion, such as a Ewing sarcoma or multiple myeloma, because of the multiple cortical holes that project over the medullary space, thus resembling a medullary permeative process
-The way to differentiate a true intramedullary permeative process from an intracortical process such as osteoporosis is to observe the cortex and see whether it is solid or riddled with holes -If the cortex is solid, one can assume the permeative process is emanating from the medullary space -If the cortex has multiple small holes, the clinician can assume the permeative pattern is from the cortical process. -I call a permeative appearance that is secondary to cortical holes a “pseudopermeative” process to distinguish it from a true permeative process. -Other causes for a pseudopermeative process include hemangioma and radiation. |
|
|
Explain how hemangiomas can cause the appearance of a permeative lesion:
|
A hemangioma can cause cortical holes in two ways: from focal hyperemia causing
focal osteoporosis, or by the blood vessels themselves tunneling through the cortex |
|
|
Explain how radiation therapy can cause the appearance of a permeative lesion in bone:
|
-Radiation can cause cortical holes in bone and mimic a permeative pattern because of the death of cortical osteocytes, which can result in large lacunae in the cortex.
-The cortical holes from radiation can be large, in which case they would not be confused with a true permeative process, but they can also be small and resemble an aggressive lesion. |
|
|
What's your differential for a permeative bone lesion in a young patient (<30 years)? What about an older patient?
What's your differential for a pseudopermeative lesion? |
-If a permeative lesion is found, the differential diagnosis is usually an aggressive process such as Ewing sarcoma, infection, or eosinophilic granuloma in a young person (<30 years of age) or multiple myeloma, metastatic carcinomatosis, or primary lymphoma of bone in an older patient.
-If, however, the permeative pattern is a result of cortical holes—that is, a pseudopermeative pattern—the differential diagnosis is considerably less sinister: aggressive osteoporosis, hemangioma, or radiation changes. This differential diagnosis does not arise often but is very useful when it does |
|
|
What is the most common cause of osteomalacia?
What are the radiographic findings of osteomalacia? |
-The most common cause is renal osteodystrophy.
-The plain radiographic findings are almost identical to those of osteoporosis (cortical thinning), and, for the most part, the two disorders are indistinguishable. -The only finding that is pathognomonic for osteomalacia is a Looser fracture, which is a fracture through large osteoid seams -They are extremely uncommon but tend to occur in the femur, pelvis, and scapula. |
|
|
What is osteomalacia in children called?
What does it look like on radiographs? What are the most common causes? |
-In children, osteomalacia is called rickets.
-It causes the epiphyses to become flared and irregular and the long bones to undergo bending from the bone softening -As in adults, the most common cause is renal disease, although other causes such as biliary disease and dietary insufficiencies are occasionally seen. |
|
|
Explain the difference between primary and secondary hyperparathyroidism:
What's the most common cause of hyperparathyroidism? |
-Primary HPT is caused by parathyroid adenomas and hyperplasia.
-Up to 40% of patients with primary HPT will demonstrate skeletal abnormalities radiographically. -The most common cause of HPT is from renal disease, which leads to secondary HPT. -Secondary HPT is the result of the parathyroids secreting excess PTH in response to the hypocalcemia that occurs from chronic renal failure |
|
|
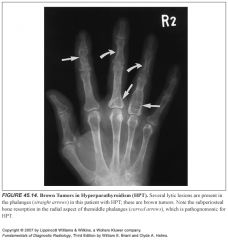
Describe the radiographic findings in hyperparathyroidism:
Where is the best place to look for these findings? |
-The radiographic sign that is pathognomonic for HPT is subperiosteal bone resorption.
-It is seen most commonly on the radial aspect of the middle phalanges of the hand, but it can be seen in any long bone in the body. -It is commonly seen on the medial aspect of the proximal tibia, at the sacroiliac joints and in the distal clavicle. -Other radiographic findings include osteosclerosis, which is usually diffuse but often involves the spine in a manner resembling the stripes on rugby jerseys, hence the name “rugger jersey spine” -Brown tumors are cystic lesions that are often expansile and aggressive in appearance -A brown tumor can have a variety of appearances, so its only unique characteristic is its association with subperiosteal bone resorption. |
|
|
Describe imaging findings in hypoparathyroidism:
|
-Few skeletal changes occur in hypoparathyroidism.
-The calvaria on occasion will show thickening, and calcification in the basal ganglia of the brain has been described. |
|
|
What is pseudohypoparathyroidism?
|
-Pseudohypoparathyroidism is caused by a congenital failure of tissues to respond to PTH.
-The parathyroid glands are normal in these cases. -Treatment of these patients with PTH is of no help because the problem lies in the end organs, not in the parathyroid glands. -A characteristic appearance is seen in these patients: obesity, round facies, short stature, and brachydactyly. -The tubular bones of the hands and feet are often all short. -Shortened fourth and fifth metacarpals are a frequent finding in this entity (knuckle knuckle dimple dimple--Turner's syndrome has blunting only of the 4th metascarpal "knuckle knuckle dimple knuckle") |
|
|
What is pseudopseudohypoparathyroidism?
|
-In pseudopseudohypoparathyroidism, there is no parathyroid abnormality and no end-organ problem; these patients merely resemble patients with pseudohypoparathyroidism.
|
|
|
What causes gigantism/acromegaly?
|
A secreting adenoma or hyperplasia of the anterior lobe of the pituitary gland will result in accelerated bone growth. If it occurs before the epiphyses close, it causes giantism. If it occurs after the epiphyses are closed, the result is acromegaly.
|
|
|
Describe radiographic manifestations of acromegaly:
|
-Acromegaly has several characteristic radiographic features in the skeletal system.
-The skull film invariably shows calvarial thickening, enlarged sinuses, and an enlarged sella turcica. -The jaw is prognathic. -The terminal tufts of the distal phalanges become hypertrophied and have a so-called spade appearance (an appearance not unlike a spade or shovel) -The joint spaces are occasionally minimally enlarged because of hypertrophy of the hyaline articular cartilage. -Early DJD ensues because the cartilage itself is abnormal. -The soft tissues also hypertrophy, with various measurements of soft tissue thickening used by some as an indicator for acromegaly. -For instance, thickening of the heel pad adjacent to the calcaneus has been used as a sign of acromegaly. |
|
|
Describe radiographic manifestations of hyperthyroidism:
|
-A rare manifestation of hyperthyroidism in adults is thyroid acropachy.
-This occurs only after prior thyroidectomy, and the cause is unknown. -A characteristic-appearing periostitis occurs in the metacarpals and phalanges of the hands and feet -It invariably involves the ulnar aspect of the fifth metacarpal, a useful differential point that can be used to tell thyroid acropachy from other causes of diffuse periostitis, such as hypertrophic pulmonary osteoarthropathy and pachydermoperiostitis, a rare form of idiopathic periostitis and skin thickening. |
|
|
Describe radiographic manifestations of congenital hypothyroidism (cretinism):
|
-Decreased thyroid secretion, or cretinism, results in delayed skeletal maturation in children.
-Delay in ossification of epiphyseal centers with occasional appearance of “stippled” epiphyses is seen. -A delay in epiphyseal closure also occurs, in some instances with failure of epiphyseal closure noted in the third and fourth decade. |
|
|
What's your differential for diffusely dense bones (osteosclerosis)?
|
“Regular Sex Makes Occasional Perversions Much More Pleasurable And Fantastic.”
Renal osteodystrophy Sickle cell disease Myelofibrosis Osteopetrosis Pyknodysostosis Metastatic carcinoma Mastocytosis Paget disease Athletes Fluorosis |
|
|
When should you consider renal osteodystrophy as a cause of osteosclerosis?
|
-Although the most common presentation of renal osteodystrophy is osteopenia, about 10% to 20% of patients with renal osteodystrophy will exhibit osteosclerosis, and the reasons for it are unknown.
-The sine qua non of renal osteodystrophy is subperiosteal bone resorption, seen earliest and most reliably at the radial aspect of the middle phalanges of the hands. -Without this finding, osteosclerosis caused by renal disease should not be entertained. |
|
|
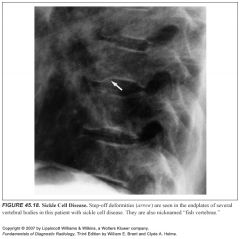
What are radiographic manifestations of sickle cell disease?
|
-As in renal osteodystrophy, the underlying cause of dense bones in sickle cell disease is unknown.
-It occurs in a small percentage of patients. -Additional signs to look for are bone infarcts and step-off deformities of the vertebral body endplates. -These are also called “fish” vertebrae because they resemble the vertebrae found in fish. -Avascular necrosis of the hip and humerus is frequently an accompanying finding. |
|
|
What findings should make you suspicious for myelofibrosis?
|
Whenever osteosclerosis is seen in a patient older than 50 years of age, a search should be made for a large spleen and extramedullary hematopoiesis characteristic of myelofibrosis
|
|
|
Describe radiographic manifestations of osteopetrosis:
|
-Osteopetrosis is a hereditary abnormality that results in extremely dense bones throughout the skeleton
-A characteristic finding is the so-called bone-in-bone appearance often seen in the vertebral bodies, in which the vertebrae have a small replica of the vertebral body inside the normal one. -Also characteristic are “sandwich vertebrae,” in which the endplates are densely sclerotic, giving the appearance of a sandwich -The sandwich vertebrae appearance resembles a rugger jersey spine but the pattern is much denser and more sharply defined. |
|
|
What's the difference between a rugger jersey spine and sandwich spine?
Which disorders are associated with each? |
-Rugger jersey spines are manifestations of the osteosclerosis related to hyperparathyroidism, most commonly seen with chronic renal disease.
-The upper and lower endplates of the verterbal bodies are dense, appearing like stripes on a rugby jersey. -Sandwich vertebrae occur with osteopetrosis -The sandwich vertebrae appearance resembles a rugger jersey spine but the pattern is much denser and more sharply defined. |
|
|
What is pyknodysostosis?
What are the radiographic manifestations? |
-These patients are typically short and have hypoplastic mandibles.
-The distinguishing radiographic finding that is essentially pathognomonic is acroosteolysis with sclerosis. -The distal phalanges often have the appearance of chalk that has been put into a pencil sharpener: they are pointed and dense, without distal tufts. -No other disease process has this appearance. -Another name for this disorder is Toulouse-Lautrec syndrome, named for the famous artist who was afflicted with pyknodysostosis. |
|
|
What is mastocytosis?
|
-Mastocytosis is another rare disorder that can cause uniformly increased bone density.
-Unfortunately, there are no other plain film findings that might help with the diagnosis. -Patients with this disease have thickened small bowel folds with nodules, but, of course, to see these, an upper GI contrast study must be performed -Urticaria pigmentosa is a characteristic skin lesion found in these patients (hives break out wherever the skin is scraped) |
|
|
Describe radiographic manifestations of Paget's dsiease:
|
-Paget disease classically causes bony enlargement and thickening
-It occurs most commonly in the pelvis where it has been said that the iliopectineal line on the pelvic brim is almost always thickened -Paget disease can occur in any bone in the body, including the smaller bones of the hands and feet. -Paget disease has three distinct phases that are visible radiographically: a lytic phase, a sclerotic phase, and a mixed lytic-sclerotic phase. -The lytic phase often has a sharp leading edge, called a flame-shaped or blade-of-grass leading edge -In a long bone, with the sole exception being the tibia, Paget disease always starts at the end of the bone; therefore, if a lesion is present in the middle of a long bone and does not extend to either end, one can safely exclude Paget disease. |
|
|
Describe radiographic manifestations of fluorosis:
|
-A radiographic finding that patients with fluorosis often have is ligamentous calcification.
-Calcification of the sacrotuberous ligament is said to be characteristic for fluorosis. |
|

|
1
|
|

|
2
|
|

|
3
|
|

|
4
|
|

|
5
|
|

|
6
|
|

|
7
|
|

|
8
|
|

|
9
|
|

|
10
|
|

|
11
|
|

|
12
|
|

|
13
|
|
|
14
|
|

|
15
|
|

|
16
|
|

|
17
|
|
|
18
|
|

|
19
|
|

|
20
|
|

|
21
|
|

|
22
|
|

|
23
|
|

|
24
|
|

|
25
|
|

|
26
|

